Remodeling of the endometrial cavity in patients experiencing infertility and pregnancy loss
Makiyan Z.N., Adamyan L.V., Gus A.I., Omarova A.R.
Relevance: Uterine abnormalities occur in 35% of infertile patients and in approximately 63% of cases of pregnancy loss. Early detection of congenital uterine abnormalities and timely surgical correction are crucial.
Objective: To evaluate the effectiveness of surgical remodeling of the endometrial cavity in patients with reproductive dysfunction and various types of intrauterine septa.
Materials and methods: Between 2024 and 2025, 325 patients with various types of intrauterine septa underwent surgery at the Department of Operative Gynecology at V.I. Kulakov NMRC for OG&P, Ministry of Health of Russia. All patients underwent pelvic examination using three-dimensional ultrasound scanning. The extent of surgical treatment was determined by the anatomical form of the intrauterine septum and the presence of concomitant gynecological pathologies. Reproductive outcomes were studied in 135 patients over two years following the recovery phase.
Results: The mean age of the patients was 33.6±3.5 years. Based on the anatomical characteristics of the uterus, we classified the intrauterine septa into three categories: complete intrauterine septum (n=22), incomplete intrauterine septum (n=183), and T-shaped narrowing of the uterine cavity (n=120). Hysteroresectoscopy was performed in 245 cases, whereas laparoscopy was combined with hysteroresectoscopy in 80 cases. Three-dimensional surgical remodeling of the endometrial cavity was performed by making a transverse incision in the subendometrial layer of the myometrium using a monopolar hysteroscopic loop at the fundus of the uterine cavity between the openings of the fallopian tubes. Areas of fibrous myometrium at the fundus were excised to a depth of 4–6 mm and a length of 25–30 mm in the transverse direction. Subsequently, a longitudinal excision of the subendometrial layer of the fibrous myometrium was performed along the lateral walls of the uterus from the openings of the fallopian tubes to the internal os, measuring 30–35 mm in length, 4–5 mm deep, and 6–8 mm wide. Pregnancy occurred in 34.8% of patients: 27 achieved pregnancy in a natural cycle, and 20 through IVF and embryo transfer. Thirty-six (26.7%) patients participated in the oocyte donation and pre-pregnancy preparation programs.
Conclusion: Three-dimensional surgical remodeling of the endometrial cavity is recommended for patients with congenital (intrauterine septum) or acquired narrowing (synechiae) of the uterine cavity. It also aims to enhance reproductive outcomes in cases of ineffective embryo transfer attempts during IVF and in older reproductive age groups as part of preimplantation preparation.
Authors' contributions: Makiyan Z.N., Adamyan L.V., Gus A.I., Omarova A.R. – diagnostics, operations, conception and design of the study, data collection on the stated topic, analysis of the results, drafting and editing of the manuscript.
Conflicts of interest: The authors declare no conflicts of interest.
Funding: This study received no funding.
Ethical Approval: The study was reviewed and approved by the Research Ethics Committee of the V.I. Kulakov NMRC for OG&P (Ref. No: 6 of December 24, 2023).
Patient Consent for Publication: All patients provided informed consent for the publication of their data.
Authors' Data Sharing Statement: The data supporting the findings of this study are available upon request from the corresponding author after approval from the principal investigator.
For citation: Makiyan Z.N., Adamyan L.V., Gus A.I., Omarova A.R. Remodeling of
the endometrial cavity in patients experiencing infertility and pregnancy loss.
Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2025; (11): 95-100 (in Russian)
https://dx.doi.org/10.18565/aig.2025.217
Keywords
Over the past 20 years, fertility has declined globally across all populations [1]. According to the WHO (2023), infertility is recognized as the most common chronic disease among people of reproductive age, affecting approximately 17.5% of the adult population (with an incidence of primary infertility of 9.6% and secondary infertility of 6.5%). Additionally, the frequency of spontaneous loss of desired pregnancies is approximately 10–15%. More than 10% of all newborns are conceived through in vitro fertilization (IVF). The reasons for failure to conceive in 80% of couples examined, including during embryo transfer in artificial insemination cycles, remain unknown [1, 2].
Uterine abnormalities occur in 35% of patients with infertility and in approximately 63% of cases involving miscarriage [2–11]. Many women experience recurrent pregnancy loss, prolonged infertility, and unsuccessful IVF attempts, which significantly worsen the prognosis for restoring reproductive function [6–11]. Therefore, early detection of congenital uterine anomalies and timely surgical correction are crucial [2–5].
This study aimed to evaluate the effectiveness of surgical remodeling of the endometrial cavity in patients with reproductive dysfunction and various types of intrauterine septa.
Materials and methods
Between 2024 and 2025, 325 patients with various types of intrauterine septa underwent surgery at the Department of Operative Gynecology at V.I. Kulakov NMRC for OG&P, Ministry of Health of Russia, representing 14% of the total number of patients operated on.
All patients underwent pelvic organ examination (three-dimensional ultrasound of uterus and appendages). Ultrasound examination was conducted in the ultrasound and functional diagnostics department using GE Voluson E10 (USA) devices equipped with a 9.0 MHz transvaginal sensor.
This prospective cohort study was reviewed and approved by the Research Ethics Committee of V.I. Kulakov NMRC for OG&P (Ref. No: 6 of December 24, 2023).
Results
Surgical treatment was performed based on patient complaints, including failure to conceive in a natural cycle with a normal spermogram in 16% (52/325) of cases, failure to conceive during embryo transfer in the IVF program in 12% (39/325), miscarriage after IVF in 9% (29/325), and miscarriage after conception in a natural cycle in 63% (205/325).
Variants of the intrauterine septum were identified in 325 patients aged 21 to 45 years, with an average age of 33.6±3.5 years at the time of diagnosis of the congenital uterine anomaly. The duration of infertility ranged from 5 to 16 years, and patients with a history of pregnancy loss experienced 2 to 11 spontaneous miscarriages.
A study of the outcomes of desired pregnancies revealed that 82% of spontaneous miscarriages occurred before 12 weeks of gestation, whereas 8.7% of pregnancy losses occurred between 13 and 28 weeks. Premature births (between 28 and 37 weeks) were observed in 6.1% of patients, and full-term live births occurred in 3.2% of patients.
Three-dimensional ultrasound scanning was performed to clarify the shape of the uterine cavity (Figs. 1–3). The most informative images were obtained from the endometrial cavity in the frontal plane, which demonstrated a pronounced change in anatomical shape, including narrowing of the uterine cavity at the fundus and the lateral walls.
Based on the anatomical characteristics of the uterus, three variants of the intrauterine septum were identified: a complete intrauterine septum with bifurcation of the cervical canal, an incomplete intrauterine septum, and a saddle-shaped intrauterine septum combined with T-shaped narrowing of the uterine cavity.
The extent of surgical treatment was determined by the anatomical form of the intrauterine septum and the presence of concomitant gynecological pathologies. Hysteroresectoscopy was performed in 245 patients, and laparoscopy was combined with hysteroresectoscopy in 80 patients.
A complete intrauterine septum was detected in 22 patients (Fig. 1), characterized by a normal external contour of the uterus and complete separation by the intrauterine septum, forming two symmetrical endometrial cavities and two cervical canals. Fourteen patients had a single cervix divided by a septum into two cervical canals, while eight patients had a double cervix, two cervical canals, and a double vagina.

Surgical treatment aimed to dissect the intrauterine septum and create a single endometrial cavity. Surgery was performed under laparoscopic guidance.
Description of hysteroresectoscopy
The cervix was fixed with bullet forceps, and the cervical canal was dilated to Hegar No. 8. A hysteroresectoscope was inserted into the cervical canal of one hemipole. Using a monopolar loop, the intrauterine septum was incised at the level of the internal os, followed by excision of the fibrous tissue in the fundus area, forming a uterine cavity of normal shape and size.
A 5% glucose solution was used as the medium. The fluid was introduced and its outflow was controlled using a Karl Stortz hysteroscopic pump. The volume of fluid introduced ranged from 1.0 to 2.0 liters, the fluid delivery rate was 150–400 ml per minute, and the average pressure in the uterine cavity was 60–80 mm Hg. A monopolar electrode in the cutting mode with a current power of 60 W was used to dissect the intrauterine septum. Hemostasis was performed in the coagulation mode in cases of bleeding in the area of septum dissection.
The anatomical features of the cervix are important: when the width between the cervical canals is more than 6 mm, the cervix is preserved and divided into two cervical canals. When the width between the cervical canals of the uterus was less than 6 mm, the septum in the cervical canal was incised, and a single cervical canal was formed (in four patients).
An incomplete intrauterine septum was detected in 183 patients (Fig. 2a), and the uterine cavity was divided by a longitudinal septum of varying lengths (from the internal os and proximally), while the cervical canal remained intact. While a complete intrauterine septum divides the uterine cavity and cervical canal, an incomplete intrauterine septum begins directly at the level of the internal os or higher, and continues to the bottom of the uterus.
Surgical treatment: Hysteroresectoscopy (using the method described above) was performed, the intrauterine septum was incised, fibrous tissue in the area of the longitudinal-lateral walls was excised, and an endometrial biopsy was performed.
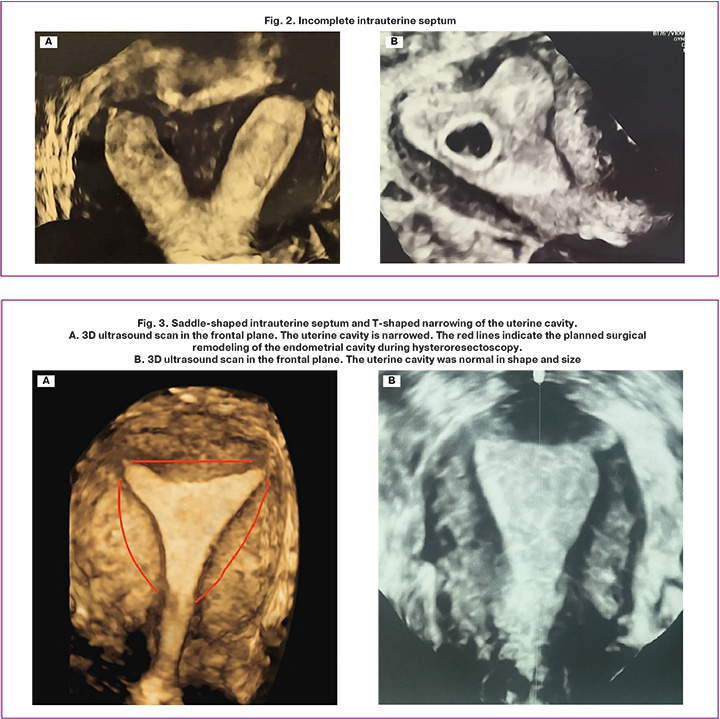
On the control 3D ultrasound scan (Fig. 2b), the uterine cavity was normal in shape and size. A fetal egg with a diameter of 8 mm was detected in the uterine cavity, corresponding to a gestation period of six weeks. The chorion is ring shaped and adheres to the lateral wall of the uterine cavity in the area of fibrous tissue excision.
A saddle-shaped intrauterine septum was detected in 120 patients (Fig. 3), with a length of approximately 10–12 mm on a wide base between the openings of the fallopian tubes. Combined T-shaped narrowing of the uterine cavity was detected in 92 patients.
Surgical treatment included remodeling of the endometrial cavity using hysteroresectoscopy, excision of the fibrous intrauterine septum, longitudinal-lateral excision of fibrous tissue, and endometrial biopsy.
With a T-shaped uterus, remodeling of the endometrial cavity was performed, including longitudinal-lateral incisions of the uterine cavity walls and excision of fibrous tissue. In the frontal image, the red lines mark the contours of the upcoming surgical remodeling of the endometrial cavity (Fig. 3a).
Remodeling of the endometrial cavity
Hysteroresectoscopy was performed using a previously described technique. The uterine cavity was narrowed at the lateral walls and bottom owing to internal thickening of the myometrium, while the openings of the fallopian tubes were clear. The endometrium appeared unremarkable, with no visible pathology. A monopolar loop of the hysteroresectoscope was used to make a transverse incision in the subendometrial layer of the myometrium at the bottom of the uterine cavity between the openings of the fallopian tubes to a depth of 4–6 mm. Areas of fibrous myometrium in the fundal region were excised using a straight monopolar loop, creating an oval shape measuring 25–30 mm in length (transversely), 4–5 mm in depth, and 12–16 mm in width, resulting in an oval basal surface of the myometrium in the fundus. Longitudinal-lateral excisions were performed in the lateral folds of the myometrium with a curved monopolar loop, extending from the fallopian tube openings to the internal os on both sides, measuring 30–35 mm in length, 4–5 mm in depth, and 6–8 mm in width. The volume of uterine cavity was enlarged.
Histological examination of the excised fragments of the intrauterine septum and fibrous-muscular tissue revealed chaotically arranged bundles of smooth muscle cells with sclerosed and sharply narrowed vascular lumens. A marked decrease in the total capillary lumen area (Kernogan index) indicated impaired capillary perfusion in excised fibrous tissue. These features hinder adequate blood circulation in the subendometrial layers, which can adversely affect normal implantation and placentation, contributing to the risk of intrauterine fetal death.
After excision of fibrous tissue, the endometrium regenerates on the resected surface within 2–3 menstrual cycles.
Three months after the surgical treatment, the effectiveness of the intervention was assessed using ultrasound examination. The criteria for effective remodeling included a triangular endometrial cavity and an optimal endometrial thickness of at least 8 mm during the conception cycle.
Intrauterine adhesions in the area of fibrous tissue resection were detected in 8.9% of the patients, necessitating repeat hysteroresectoscopy and fibrous tissue resection.
Reproductive outcomes were studied in 135 patients over two years following the recovery period (three months).
Pregnancy in the natural cycle occurred in 27/135 patients, whereas pregnancy after IVF and embryo transfer was observed in 20/135 patients, resulting in a total pregnancy rate of 34.8% among the patients. Additionally, 26.7% (36/135) of patients participated in the oocyte donation and pre-pregnancy preparation program.
Discussion
Given the global decline in fertility, restoring reproductive function in patients suffering from infertility or pregnancy loss could increase birth rates in our country. Patients with congenital uterine anomalies are highly motivated to have children; to achieve reproductive success, they often require surgical correction and assisted reproductive technology.
Analysis of pregnancy losses prior to surgical treatment indicates that more than 80% of spontaneous miscarriages occur in early pregnancy (6–8 weeks), when the fertilized egg occupies the entire uterine cavity. During this period, the chorion is supplied with blood through the entire surface of the villous membrane, continuing up to 12 weeks when the placenta forms. From 12 to 16 weeks of gestation, part of the chorion develops into the placenta, and the prognosis for the progression of pregnancy and fetal development depends on this process.
The proposed method of surgical remodeling of the endometrial cavity aims to excise (eliminate) avascular fibrous tissue and expand the volume and perimeter of the effective blood supply in the newly formed subendometrial layer.
Three-dimensional surgical remodeling of the endometrial cavity is advisable in the following cases:
- Patients with congenital uterine anomalies or acquired narrowing (intrauterine synechiae) of the uterine cavity
- To improve reproductive outcomes in patients with ineffective embryo transfer attempts in IVF programs
- In patients of advanced reproductive age, as preimplantation preparation.
In patients with a history of multiple intrauterine interventions following spontaneous abortions, the presence of intrauterine synechiae, and issues with a “thin” endometrium, the postoperative recovery period is critical.
The most relevant and understudied issue to date remains the mechanism of endometrial regeneration on the newly formed surface of the myometrium as a result of remodeling after the procedure. Is the process of endometrial repair the result of regeneration of the existing intact endometrium in areas of the original (native) uterine cavity, or does metaplasia of the cambial layer occur from pluripotent cells embedded in the myometrium, similar to those found in the uterine rudiments [12, 13]?
Conclusion
The proposed method of surgical remodeling of the endometrial cavity is designed to excise (eliminate) avascular fibrous tissue and expand the volume and perimeter of the effective blood supply in the newly formed subendometrial layer. It is advisable to use this approach not only in patients with congenital (intrauterine septum) or acquired narrowing (synechiae) of the uterine cavity but also to improve reproductive outcomes in cases of ineffective embryo transfer in IVF programs and in older reproductive age as preimplantation preparation.
References
- Fauser B.C.J.M., Adamson G.D., Boivin J., Chambers G.M., de Geyter C., Dyer S. et al. Declining global fertility rates and the implications for family planning and family building: an IFFS consensus document based on a narrative review of the literature. Hum. Reprod. Update. 2024; 30(2): 153-73. https://dx.doi.org/10.1093/humupd/dmad028
- Makiyan Z. Systematization for female genital anatomic variations. Clin. Anat. 2021; 34(3): 420-30. https://dx.doi.org/10.1002/ca.23668
- Noventa M., Spagnol G., Marchetti M., Saccardi C., Bonaldo G., Laganà A.S. et al. Uterine septum with or without hysteroscopic metroplasty: impact on fertility and obstetrical outcomes – a systematic review and meta-analysis of observational research. J. Clin. Med. 2022; 11(12): 3290. https://dx.doi.org/10.3390/jcm11123290
- Prior M., Richardson A., Asif S., Polanski L., Parris‐Larkin M., Chandler J. et al. Outcome of assisted reproduction in women with congenital uterine anomalies: a prospective observational study. Ultrasound Obstet. Gynecol. 2018; 51(1):110-7. https://dx.doi.org/10.1002/uog.18935
- Caballero Campo M., Pérez Milán F., Carrera Roig M., Moratalla Bartolomé E., Domínguez Arroyo J.A., Alcázar Zambrano J.L. et al. Impact of congenital uterine anomalies on obstetric and perinatal outcomes: systematic review and meta-analysis. Facts Views Vis Obgyn. 2024; 16(1): 9-22. https://dx.doi.org/10.52054/FVVO.16.1.004
- Omoto A., Ishikawa H., Inoue M., Morimoto S., Koga K., Shozu M. Metroplasty increases the take-home baby rate by reducing pregnancy loss without changing the chance of conception in women with septate uterus: a retrospective, single-center, observational study. BMC Pregnancy Childbirth. 2023; 23(1): 860. https://dx.doi.org/10.1186/s12884-023-06191-3
- Joshi B., Kaushal A., Suri V., Gainder S., Choudhary N., Jamwal S. et al. Prevalence and pregnancy outcome of Mullerian anomalies in infertile women: a retrospective study. J. Hum. Reprod. Sci. 2021; 14(4): 431-5. https://dx.doi.org/10.4103/jhrs.jhrs_3_21
- Practice Committee of the American Society for Reproductive Medicine. Evidence-based diagnosis and treatment for uterine septum: a guideline. Fertil. Steril. 2024; 122(2): 251-65. https://dx.doi.org/10.1016/j.fertnstert.2024.02.033
- Al-Husban N., Odeh O., AlRamahi M., Qadri S., Al-Husban H. Fertility-enhancing hysteroscopic surgery; multi-center retrospective cohort study of reproductive outcome. BMC Womens Health. 2023; 23(1): 459. https://dx.doi.org/10.1186/s12905-023-02562-2
- Kalaitzopoulos D.R., Themeli M.Z., Grigoriadis G., Alterio M.D., Vitale S.G., Angioni S. et al. Fertility, pregnancy and perioperative outcomes after operative hysteroscopy for uterine septum: a network meta-analysis. Arch. Gynecol. Obstet. 2023; 309(3): 731-44. https://dx.doi.org/10.1007/s00404-023-07109-2
- Rikken J.F.W., Kowalik C.R., Emanuel M.H., Bongers M.Y., Spinder T., Jansen F.W. et al. Septum resection versus expectant management in women with a septate uterus: an international multicentre open-label randomized controlled trial. Hum. Reprod. 2021; 36(5): 1260-7. https://dx.doi.org/10.1093/humrep/deab037
- Макиян З.Н., Адамян Л.В., Асатурова А.В., Ярыгина Н.К. Маточные рудименты: клинико-морфологические варианты и оптимизация хирургического лечения. Акушерство и гинекология. 2019; 12: 126-32. [Makiyan Z.N., Adamyan L.V., Asaturova A.V., Yarygina N.K. Uterine rudiments: clinical and morphological options of surgical treatment and its optimization. Obstetrics and Gynecology. 2019; (12): 126-32 (in Russian)]. https://dx.doi.org/10.18565/aig.2019.12.126-132
- Burunova V.V., Gisina A.M., Yarygina N.K., Sukhinich K.K., Makiyan Z.N., Yarygin K.N. Isolation of a population of cells co-expressing markers of embryonic stem cells and mesenchymal stem cells from the rudimentary uterine horn of a patient with uterine aplasia. Bull. Exp. Biol. Med. 2023; 174(4):549-55. https://dx.doi.org/10.1007/s10517-023-05746-w
Received 14.08.2025
Accepted 11.11.2025
About the Authors
Zograb N. Makiyan, Dr. Med. Sci., Leading Researcher at the Department of Operative Gynecology, Academician V.I. Kulakov National Medical Research Center for Obstetrics, Gynecology and Perinatology, Ministry of Health of Russia, 4, Oparin str., Moscow, 117997, Russia, makiyan@mail.ru, https://orcid.org/0000-0002-0463-1913Leyla V. Adamyan, Dr. Med. Sci., Professor, Academician of the Russian Academy of Sciences, Head of the Gynecological Department, Academician V.I. Kulakov
National Medical Research Center for Obstetrics, Gynecology and Perinatology, Ministry of Health of Russia, 4, Oparin str., Moscow,
117997, Russia, adamyanleila@gmai.com, https://orcid.org/0000-0002-3253-4512
Aleksandr I. Gus, Dr. Med. Sci., Professor, Chief Researcher at the Department of Ultrasound and Functional Diagnostics, Academician V.I. Kulakov National Medical Research Center for Obstetrics, Gynecology and Perinatology, Ministry of Health of Russia, 4, Oparin str., Moscow, 117997, Russia, aleksandr_gus@mail.ru,
https://orcid.org/0000-0003-1377-3128
Ayna R. Omarova, PhD student at the Department of Operative Gynecology, Academician V.I. Kulakov National Medical Research Center for Obstetrics, Gynecology and Perinatology, Ministry of Health of Russia, 4, Oparin str., Moscow, 117997, Russia, a_omarova@oparina4.ru, https://orcid.org/0009-0000-8655-6306
Corresponding author: Zograb N. Makiyan, makiyan@mail.ru