В связи с низкой рождаемостью в нашей стране остро стоит проблема борьбы с невынашиванием беременности как одной из главных составляющих репродуктивных потерь. Исследования многих авторов доказывают, что потеря беременности в I триместре может свидетельствовать об уже имеющихся нарушениях в репродуктивной системе, которые в дальнейшем могут усугубляться, приводя к привычному невынашиванию, внематочной беременности, хроническим воспалительным заболеваниям женских половых органов, в том числе к хроническому эндометриту [1–3].
Воспалительные заболевания репродуктивной системы занимают одно из первых мест среди причин репродуктивных нарушений. Важно отметить, что после свершившегося выкидыша развитию эндометрита могут способствовать не только облигатные, но и условно-патогенные микроорганизмы. Активация условно-патогенной микрофлоры зависит не только от концентрации микроорганизмов, но и от состояния иммунитета, что необходимо учитывать при проведении лекарственной терапии. Вместе с тем на фоне применения антибиотиков нередко возникает дисбиоз, отрицательное действие которого на здоровье женщин в настоящее время уже не требует доказательств. В литературе появляется все больше работ, посвященных восстановлению и поддержанию нормальной микробиоты, которая играет исключительно важную роль в нормализации иммунного статуса и профилактике гинекологических и экстрагенитальных заболеваний [3–5].
Помимо создания новых и более эффективных антибактериальных препаратов, продолжается поиск других методов противовоспалительного лечения, например, использование лазерного излучения, воздействие переменного магнитного поля на органы малого таза, а также инфузий озонированных растворов. Физиотерапию применяют для лечения многих заболеваний, включая и воспалительные заболевания женских половых органов. Лазерное излучение, магнитное поле, озонотерапия обладают не только противовоспалительным, но и иммуномодулирующим эффектом, улучшают регенеративные процессы и снижают сенсибилизацию, они могут быть применены у больных с аллергическими реакциями на антибиотики [1, 2].
Цель проведенного исследования – снижение риска воспалительных осложнений после самопроизвольного прерывания беременности в I триместре для полноценного восстановления репродуктивной функции путем применения антибактериальных, пробиотических средств и физиотерапии.
Материалы и методы
В исследование изначально были включены 117 женщин в возрасте от 17 до 35 лет после самопроизвольного прерывания беременности в сроке 6–12 недель. Всем пациенткам проведены вакуум-аспирация содержимого полости матки и всестороннее обследование, включающее микробиологическое исследование соскоба из цервикального канала и со стенки влагалища тестами «Инбиофлор» и «Фемофлор-16» в 1-е сутки после прерывания беременности и через 1 месяц. Данные тесты представляют собой полимеразную цепную реакцию с детекцией результатов в режиме реального времени. «Инбиофлор» позволяет диагностировать наличие в биопробе следующих безусловных патогенов: Chlamydia trachomatis, Neisseria gonorrhoeae, Trichomonas vaginalis, Mycoplasma genitalium. Используя «Фемофлор-16», можно выявить анаэробные микроорганизмы (облигатные и факультативные), грибы, уреа- и микоплазмы, сравнив с объемом бактериальной массы (ОБМ) нормофлоры, при этом также определяют качество взятия материала. Помимо микробиологических исследований, всем пациенткам определяли концентрации иммуноглобулинов (IgА, IgМ, IgG) в сыворотке крови и показатели гемостазиограммы в динамике. Всем пациенткам в динамике выполняли также ультразвуковое исследование органов малого таза.
Пациентки с выявленной тестом «Инбиофлор» безусловно-патогенной микрофлорой (n=25) исключены из исследования, в дальнейшем им проводили необходимое лечение с последующим контролем излеченности. Оставшихся 92 пациенток разделили на 2 группы (1-я группа – 45 человек, 2-я – 47 человек), в зависимости от состава комплексной противовоспалительной терапии. Всем пациенткам проведена антибактериальная терапия (доксициклина гидрохлорид 100 мг/сут) в течение 7 дней. При наличии в микробиологических исследованиях элементов гриба рода Candida пациентки получали однократно интравагинально суппозиторий, содержащий 300 мг сертаконазола. Кроме того, начиная с первого дня антибактериальной терапии, всем назначали перорально пробиотик – капсулы, содержащие Lactobacillus rhamnosus и Lactobacillus reuteri, для восстановления микробиоты влагалища. Пациенткам 1-й группы в стационаре и амбулаторно дополнительно проводили физиотерапию: магнитно-лазерное облучение малого таза (интравагинально и трансабдоминально, на курс 6–8 процедур) и озонотерапию (внутривенная инфузия озонированного физраствора, на курс 6–8 процедур). Пациентки 2-й группы в связи с занятостью на работе и/или учебе от физиотерапии отказались.
Статистический анализ
Все полученные цифровые результаты клинико-лабораторных исследований обрабатывали методами вариационной статистики. Вычисляли среднюю статистическую величину, среднее квадратичное отклонение, ошибку средней, критерий Стьюдента. Различие расценивали как значимое, если «уровень значимости» (p) был меньше 0,05.
Результаты и обсуждение
При обследовании пациенток обеих групп методом «Фемофлор-16» в 1-е сутки после самопроизвольного выкидыша нормобиота влагалища не была зарегистрирована ни в одном наблюдении. Количество лактобацилл в биопробах было снижено, варьировало от 30 до 55% (в норме превышает 70% от ОБМ) и в среднем составило 42,5±8,2%. Показатели условно-патогенной микрофлоры в норме должны быть не более 103–104 КОЕ/мл, что составляет 0,01% ОБМ. У всех обследованных больных относительные показатели условно-патогенной микрофлоры были умеренно повышены, в пределах от 2 до 10% от ОБМ. Наиболее часто повышение относительного показателя отмечено в отношении стафилококка, стрептококка, энтеробактерий (факультативные и облигатные анаэробы), грибов рода Candida, мико- и уреаплазм (рис. 1).
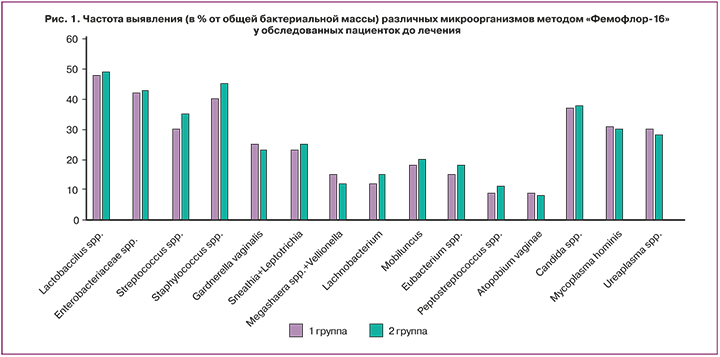
Условно-патогенные микроорганизмы, как известно, в определенных условиях, например, при повышенном их количестве и снижении локального иммунитета, могут вызвать воспалительный процесс (неспецифические воспалительные заболевания женских половых органов), поэтому назначение антибиотика широкого спектра действия было оправданным. Антимикотик сертаконазол назначали пациенткам с выявленным в отделяемом из половых путей мицелием гриба: 15 (33,3%) и 17 (36,2%) пациенткам 1-й и 2-й групп соответственно. Сертаконазол является производным бензотиофена и имидазола, обладает тройным механизмом действия: фунгицидным, фунгистатическим, а также ингибирует диморфную трансформацию (переход гриба из непатогенной формы в патогенную), назначается однократно. Согласно данным литературы, препарат воздействует на резистентные формы грибов, включая Candida non-albicans, при этом отсутствует перекрестная резистентность грибов к сертаконазолу, обладает антибактериальной активностью в отношении стафилококков и стрептококков, не оказывая действия на лактобациллы [6–8].
Одновременно с началом антибактериальной терапии всем больным назначали перорально пробиотик – капсулы, содержащие Lactobacillus rhamnosus GR-1 и Lactobacillus reuteri RC-14, которые являются представителями нормальной вагинальной микрофлоры, для восстановления нормобиоты влагалища. После перорального приема капсула проходит через желудок и растворяется в кишечнике с освобождением лактобацилл, которые проходят через кишечник, а далее, в связи с анатомической близостью ануса и преддверия влагалища, колонизируют влагалище. Научно доказана способность данных лактобацилл продуцировать перекись водорода и молочную кислоту, нормализовать pH влагалища, при этом подавляя рост патогенов [9–13]. Результаты исследования методом «Фемофлор-16», выполненные через 1 месяц после проведенного лечения, представлены на рисунке 2.

В результате повторного исследования установлено, что количество лактобацилл у большинства обследованных пациенток после проведенного лечения достоверно увеличилось (p<0,05) и достигло нормальных значений, без статистически значимых различий между группами (72,5±8,1% и 80,1±7,5% ОБМ). А количество условно-патогенной микрофлоры достоверно уменьшилось (p<0,05) по сравнению с первым обследованием (до лечения). Так, относительный показатель по Enterobacteriaceae spp., Streptococcus spp., Staphylococcus spp., Sneathia+Leptotrichia, Megashaera spp.+Vellionella, Lachnobacterium, Eubacterium spp. снизился в 1,5–2 раза по сравнению с первым обследованием и не превышал 10% от ОБМ у пациенток обеих групп, что соответствует умеренной концентрации условно-патогенных микроорганизмов. Вместе с тем выявлены и достоверные различия между группами при обследовании пациенток после проведенного лечения: относительный показатель по анаэробной микрофлоре (Gardnerella vaginalis, Mobiluncus, Peptostreptococcus, Atopobium vaginae) у пациенток 2-й группы, не получавших физиотерапию, был более 10% от ОБМ, что соответствует высокой концентрации данных условно-патогенных микроорганизмов, отмечается при бактериальном вагинозе, трудно поддающемся лекарственной терапии, на фоне которого может развиться анаэробный вагинит. В то же время у пациенток 1-й группы, получавших физиотерапию, относительный показатель по анаэробной микрофлоре соответствовал умеренной концентрации данных микроорганизмов, так как был менее 10% от ОБМ. То есть эффект антибактериальной терапии на фоне магнитно-лазерной и озонотерапии повышался, что минимизировало риск возникновения дисбиоза и воспалительного процесса.
Заслуживают внимания результаты повторного обследования, касающиеся гриба рода Candida. Количество пациенток, у которых были выявлены грибы рода Candida, достоверно уменьшилось, элементы гриба обнаружены всего в 2 случаях: у 1 (2,2%) и 1 (2,1%) пациенток обеих групп, тогда как до лечения элементы гриба были обнаружены у 14 (31,1%) и 13 (27,6%) пациенток из 1-й и 2-й групп (p<0,05). Полученные результаты свидетельствуют об эффективности однократного интравагинального применения сертаконазола, эффективность которого отмечена и в других исследованиях [6–8].
 Физические факторы в лечении острого воспаления уже были исследованы и обоснованы как необходимый фактор в восстановлении функции органов малого таза [14–17]. Наше исследование проведено для уточнения эффективности физиотерапии в профилактике воспалительных осложнений после самопроизвольного выкидыша. Большинство пациенток 1-й группы, получавших магнитно-лазерную и озонотерапию, отмечали болеутоляющий и седативный эффект после проводимых физиопроцедур.
Физические факторы в лечении острого воспаления уже были исследованы и обоснованы как необходимый фактор в восстановлении функции органов малого таза [14–17]. Наше исследование проведено для уточнения эффективности физиотерапии в профилактике воспалительных осложнений после самопроизвольного выкидыша. Большинство пациенток 1-й группы, получавших магнитно-лазерную и озонотерапию, отмечали болеутоляющий и седативный эффект после проводимых физиопроцедур.
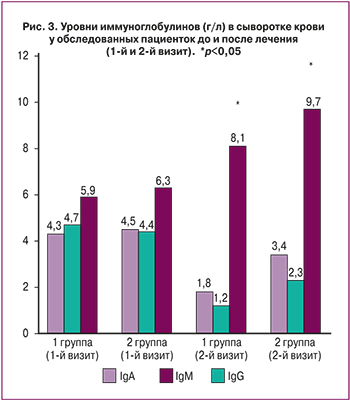
С целью изучения состояния иммунной системы и изменения ее показателей под влиянием включенных в комплекс лечения современных методов физиотерапии проведено исследование уровня иммуноглобулинов IgА, IgМ, IgG в сыворотке крови. Как известно, наличие острой воспалительной реакции характеризуется повышением концентрации иммуноглобулинов IgА и IgG, а содержание IgМ повышается при первом контакте с инфекционным агентом и свидетельствует об активности противоинфекционной защиты [3]. При сравнении уровня иммуноглобулинов в крови пациенток 1-й и 2-й групп в 1-е сутки отмечены повышенные уровни иммуноглобулинов IgA и IgG в обеих группах пациенток, что свидетельствует об активизации иммунной системы в борьбе с воспалением. Так, уровень IgA у пациенток 1-й группы составил 4,3±0,1 г/л, во 2-й группе – 4,5±0,2 г/л (в норме: 0,7–4,0 г/л), уровень IgM у пациенток 1-й группы – 4,7±0,3 г/л, у пациенток 2-й группы – 4,4±0,1 г/л (в норме: 0,4–2,3 г/л). После лечения отмечено снижение уровня IgА до 1,8±0,1 г/л и 3,4±0,2 г/л (в 1-й и 2-й группах соответственно), а уровня IgМ – до 1,2±0,1 г/л и 2,3±0,2 г/л (в 1-й и 2-й группах соответственно) с достоверным повышением уровня IgG от 5,9±0,4 г/л до 8,1±0,5 г/л у пациенток 1-й группы и от 6,3±0,5 г/л до 9,7±0,4 г/л – во 2-й группе (норма: 7–16 г/л). Проведенная комплексная терапия с использованием магнитно-лазерной и озонотерапии способствовала более быстрому снижению уровня иммуноглобулинов IgА и IgМ у пациенток 1-й группы, хотя статистически значимых различий между группами не констатировано (рис. 3).
Нами изучены также показатели гемостазиограммы до и после проведенного лечения у пациенток после самопроизвольного выкидыша. Результаты представлены в таблицах 1 и 2.
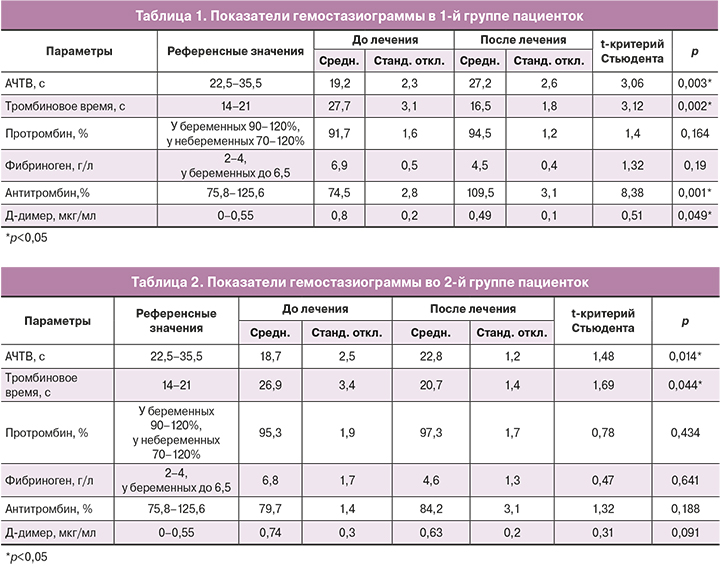
Данные гемостазиограммы свидетельствуют о наличии гиперкоагуляции у большинства обследованных в 1-е сутки после выкидыша. Так, в 1-й группе пациенток показатель АЧТВ составил 19,2±2,3 с, во 2-й группе – 18,7±2,5 с (референсные значения: 22,5–35,5 с) (р>0,05). Через 1 месяц отмечена нормализация АЧТВ: у пациенток 1-й группы – 24,2±2,6 с (р=0,003), у пациенток 2-й группы – 22,8±2,7 с (р=0,014).
При исследовании тромбинового времени у пациенток после самопроизвольного выкидыша отмечено повышение данного показателя: в 1-й группе – 27,7±3,1 с; во 2-й группе – 26,9±3,4 с (референсные значения: 14–21 с; р>0,05). После проведенного лечения данный показатель достоверно снизился и достиг нормальных значений: у пациенток 1-й группы тромбиновое время составило 16,5±1,8 с (р=0,002), во 2-й группе – 20,7±1,4 с (р=0,044). Концентрация фибриногена у всех обследованных после самопроизвольного выкидыша была достоверно выше нормы, что, по-видимому, связано с воспалительной реакцией. После проведенного антибактериального лечения концентрация фибриногена практически вернулась к верхней границе нормальных значений у большинства обследованных пациенток. Состояние антикоагулянтного звена гемостаза было оценено по уровню антитромбина. При первом определении средний уровень антитромбина соответствовал 74,5±2,8% и 75,7±1,4% в 1-й и 2-й группах (норма: 75,8–125,6%; р>0,05). Через 1 месяц после выкидыша отмечено достоверное увеличение уровня антитромбина у пациенток 1-й группы – до 109,5±3,1% (p=0,001), тогда как у пациенток 2-й группы уровень антитромбина III составил всего 84,2±3,1%, без значимых различий по сравнению со значением до лечения (р=0,188). Статистически значимые различия (109,5±3,1% и 84,2±3,1%; р<0,05) при повторном определении уровня антитромбина III между двумя группами пациенток можно связать с положительным эффектом физиотерапии, которую получали пациентки 1-й группы.
Заслуживают обсуждения также значения Д-димера. Выявлено повышение показателей Д-димера у всех пациенток в 1-е сутки после самопроизвольного выкидыша: в 1-й группе среднее значение составило 0,8±0,2 мкг/мл с последующим снижением после лечения до 0,49±0,1 мкг/мл (референсные значения: 0–0,55 мкг/мл; р=0,049); во 2-й группе до лечения средний уровень Д-димера соответствовал 0,74±0,3 мкг/мл, а после лечения снизился до 0,63±0,2 мкг/мл, не достигнув нормальных значений (р=0,91). Полученные нами данные свидетельствуют о благоприятном влиянии физиотерапии на состояние свертывающей системы крови, что подтверждают и результаты других исследований [18, 19].
С целью контроля эффективности проводимой терапии всем больным проводили в динамике трансвагинальную эхографию с оценкой размеров матки, величины М-эха, наличия или отсутствия расширения полости матки. У пациенток 1-й группы не было выявлено изменений, характерных для воспалительного процесса, в то время как у пациенток 2-й группы, не получавших физиотерапию, через 10 дней после выкидыша в 5 (10,6%) случаях отмечено расширение полости матки с неоднородным содержимым (p<0,05), что потребовало назначения дополнительной терапии, так как может служить предпосылкой для развития воспалительного процесса с возможным формированием в дальнейшем хронического эндометрита [1, 2, 19, 20].
Заключение
Таким образом, проведенные нами исследования подтверждают необходимость включения в обследование пациенток после самопроизвольного выкидыша таких современных методов, как «Инбиофлор» и «Фемофлор», для оценки состояния микробиоты влагалища. Всем пациенткам после самопроизвольного выкидыша показано комплексное лечение с включением физиотерапии для профилактики воспалительных осложнений и восстановления репродуктивной функции.



