Features of karyotypes in married couples with reproductive functional problems in Kazakhstan
Objective. To investigate the frequency and spectrum of chromosomal abnormality and chromosomal polymorphism in married couples with reproductive functional problems to determine the etiology of infertility, treatment policy, and prognosis in offspring.Khoroshilova I.G., Lokshin V.N., Begimbaeva A.A., Sarsenbaeva Zh.K., Valiev R.K., Rybina A.N., Karibaeva Sh.K., Kim A.V., Semenova N.Yu.
Subjects and methods. A cytogenetic study of peripheral blood lymphocytes was performed in 1524 patients (672 married couples with infertility and miscarriage, 90 men and 90 women without reproductive problems)
at the PERSONA International Clinical Center of Reproductology in 2017 to 2018.
Results. The chances of detecting chromosomal polymorphism in patients with infertility and burdened obstetric history (BOH) were higher than in those with normal reproduction (OR = 28.896, 95% CI, 11.799–70.765
for women; OR = 29.000, 95% CI, 9.081–92.611 for men; p < 0.05).
Conclusion. Our data allow us to recommend that genetic studies must be included in the diagnostic algorithms and clinical protocols for assisted reproductive treatment for patients with reproductive functional problems in the Republic of Kazakhstan.
Keywords
Married couples with a genetic pathology have a high risk of transmitting hereditary diseases to their offspring. Implantation with an abnormal embryo leads to impaired reproductive function: miscarriage, infertility, reduced treatment effectiveness with assisted reproductive technologies (ART) and the birth of children with chromosomal abnormalities and congenital malformations (CM) [1–4].
The study of chromosomes in couples allows us to determine the processes of maturation of gametes - their quantity and quality [5, 6]. In the Republic of Kazakhstan (RK), the use of cytogenetic, molecular genetics and molecular cytogenetic research methods has not been included in the list of the obligatory study before ART yet. There are no publications on the frequency of chromosomal pathology in patients with infertility and miscarriage in Kazakhstan.
Improving the diagnostic algorithms and clinical protocols for the treatment of infertility with ART using a genetic examination in Kazakhstan will prevent ineffective in vitro fertilization (IVF) programs, as well as prevent the transmission of chromosomal abnormalities to offspring and the birth of children with congenital malformations.
Materials and Methods
A cytogenetic study of peripheral blood lymphocytes was performed in 1524 patients (672 married couples with infertility and miscarriage, 90 men and 90 women without reproductive problems) at the PERSONA International Clinical Center of Reproductive Medicine in 2017 to 2018. All patients were divided into three groups: the 1st group included 456 married couples with primary female infertility, primary male infertility, combined infertility (the average age of women in this group was 28.9 ± 4.4 years, for men - 34.3 ± 6.7 years); the 2nd group included 216 couples with a burdened obstetric history (BOH), who had two or more miscarriages and missed abortions up to 12 weeks (68%), two or more ineffective IVF programs (21%), cases of giving birth to children with congenital malformations (11%) (the average age of men included in the 2nd group was 40.9 ± 8.9 years, women - 36.1 ± 5.0 years). The 3rd (control) group enrolled 90 female and 90 male donors of oocytes and spermatozoa, aged 18 to 35 years old, somatically healthy, with normal reproduction, and one or more healthy children.
Cases of infertility due to inflammatory or infectious diseases of the genital area were excluded.
The research material was chromosomal preparations obtained from peripheral blood lymphocytes by the standard method and stained using differential G-staining. The results of a cytogenetic study (RCS) are presented in accordance with the International System for Human Cytogenetic Nomenclature (ISCN, 2016). Statistical analysis of the data was carried out using the calculator of the free version of the program EPI InfoTM version 7.2. Data are presented as mean ± standard deviation for continuous variables, and values for qualitative categorical variables are presented as the number of subjects (n) and percentage (%). The distribution of symptoms was abnormal. Differences between groups were evaluated using the Pearson chi-squared test. Odds ratios (OR) with a confidence interval of 95% (95% CI) were used to determine the statistical significance of the relationship between factor and outcome.
Results
The study allowed us to establish chromosomal abnormalities (CA) in 46 patients, which amounted to 4.2%, including 11 (0.5%) numerical and 35 (3.7%) structural (Table 1). Full forms of CA (45, X0, 47, XXY) in the group of primary infertility were clinically manifested by underdevelopment of the genitals, an abnormality in the development of gonads in women and azoospermia in men. Mosaic forms of monosomy – X0 (45, X0 [10]/46, XX [90]) were manifested by miscarriages up to 6 weeks.
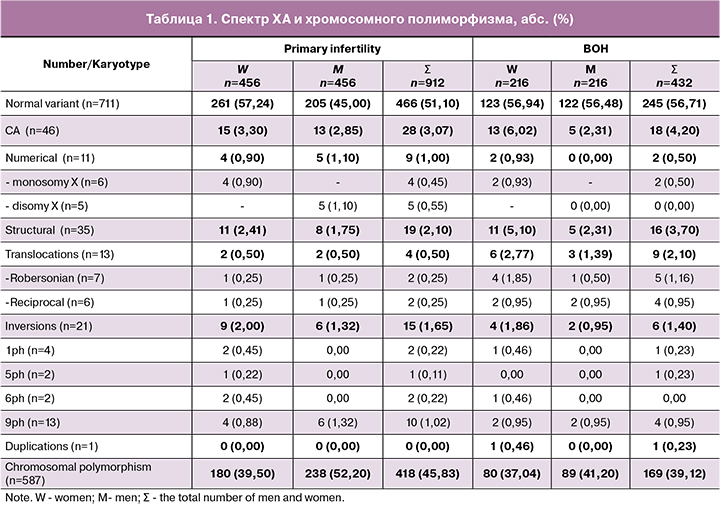
The proportion of Robertsonian translocations in women in the group of couples with BOH prevailed compared to the proportion of women with primary infertility (1.85 and 0.25%, respectively). In the formation of the derivative of Robertsonian translocations, chromosome 14 was noted, three of them were of the “centric fusion” type of chromosomes pairs 13 and 14 (45, XX, der (13; 14) (q10; q10)), which is consistent with data from other studies [7, 8]. Reciprocal translocations occurred identically in men and women with reproductive problems in general, and manifested in oligoteratozoospermia in two cases.
Pericentric inversions of heterochromatin were found in pairs of chromosomes 1, 5, 6, and 9 both in groups with infertility and BOH (1.65 and 1.39%, respectively). Their manifestations were LUF syndrome, endometriosis, low AMH and polycystic ovaries in women, as well as cases of miscarriage, premature birth, antenatal death, and malformations in the fetus [9–12].
Chromosomal polymorphism (Table 2), associated with an increase in heterochromatin regions of chromosomes (qh +) and an increase in the size of short shoulders of acrocentric chromosomes (ps +), was found in 587 patients with reproductive function problems and in 5 patients with normal reproduction (45.20 and 2.77%), which is consistent with many studies [13–15].
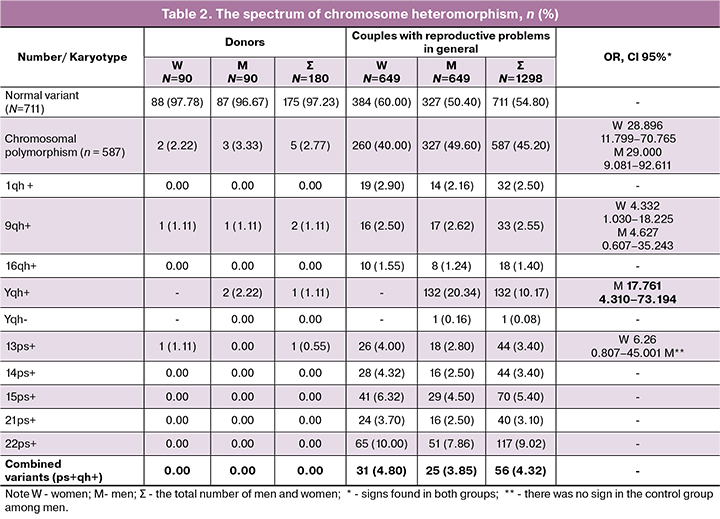
Variant 9qh+ was found equally in couples with normal and impaired reproduction (1.11 and 2.55%), which is consistent with other studies [14, 15]. Variants 15ps+ and 22ps+ were manifested as asthenozoospermia, cases of congenital malformations (cystic hygroma) and fetal monosomy-X in 28.8% of carriers from this group.
A common variant of chromosomal pathology in men was Yqh + (132 - 10.17%), of which 84 (63.5%) were accompanied by azoospermia and oligoastenozoospermia, аnd in 21 (16.2%) patients there were malformations of the reproductive system (microorchia and testicular aplasia). The molecular genetic study in patients with established chromosomal pathology revealed 6 (12.7%) cases of carriage of CFTR gene mutations (2 – IVS8-5T, 2 – IVS8-7T, 1 – IVS8-9T, 1 – delF508) and 4 (10.6%) carriers of microdeletion in the subregion AZFс Y-chromosome and 1 (2.1%) in subregions of AZFb+c, which is consistent with other studies [14–16]. In the case of Yqh- with testicular hypoplasia and asthenozoospermia, microdeletions were found in the AZFa+c subregions, which requires further study [17, 18]. In men with a normal reproductive history, clinical manifestations of Yqh+ were not detected.
The efficacy of IVF + ICSI in male carriers of Yqh+ was 82.0%, and preimplantation screening (PGS) using the a-CGH method for 13 patients with translocation was effective in 61.5%, which is consistent with another study [19].
Conclusion
There was no statistical relationship between the frequency of detected cases of chromosomal abnormality and chromosomal polymorphism and primary infertility or BOH at a significance level of p > 0.05.
The chance of detecting chromosomal polymorphism in patients with infertility and BOH was higher than in patients with normal reproduction (in women OR=28.896, CI 95% 11.799–70.765; in men 29.000, CI 95% 9.081–92.611, р<0.05). The foregoing indicates the need for mandatory cytogenetic and molecular genetic studies in patients with impaired reproductive function. It is recommended to include these studies in the diagnostic algorithms and clinical protocols for the treatment of infertility with ART methods in order to increase their effectiveness and prevent the transmission of a chromosomal abnormality to offspring and the birth of children with congenital malformations.
References
- Локшин В.Н., Джусубалиева Т.М., ред. Клиническая практика в репродуктивной медицине. Алматы: MedMedia Казахстан, 2015. 464 с. [Lokshin V.N., Dzhusubalieva T.M., ed. Clinical practice in reproductive medicine. Almaty: MedMedia Kazakhstan, 2015.446 s. (in Russian)]. ISBN 978-601-80151-6-82015.
- Сидельникова В.М., Сухих Г.Т. Невынашивание беременности. М.: МИА; 2010. 536 с. [Sidelnikova V.M., Sukhikh G.T. Unintention of pregnancy. M.: MIA; 2010. 536 p. (in Russian)]
- Локшин В.Н., Хорошилова И.Г., Куандыков Е.У. Персонифицированный подход при генетическом скрининге супружеских пар в программах ВРТ (Обзор литературы). Доклады Национальной Академии наук Республики Казахстан. 2018; 1: 37–41. [Lokshin V.N., Khoroshilova I.G., Kuandykov E.U. Personified approach to genetic screening of infertility couples in ART programs (literature review). Natsional’noy Akademii nauk Respubliki Kazakhstan. 2018; 1: 37–41. (In Russian)]. ISSN 2518-1483.
- Гончарова Н.Н., Мартышкина Е.Ю., Казначеева Т.В., Арсланян К.Н., Адамян Л.В., Курило Л.Ф., Сорокина Т.М., Черных В.Б. Медико-генетические аспекты бесплодия. Акушерство. Гинекология. Репродукция. 2012; 6(2): 35–40. [Goncharova N.N., Martyshkina E.Yu., Kaznacheyeva T.V., Arslanyan K.N., Adamyan L.V., Kurilo L.F., Sorokina T.M., Chernykh V.B.Medicogenetic aspects of infertility. Obstetrics. Gynecology. Reproduction. 2012; 6(2): 35–40. (in Russian)]. eLIBRARY ID: 17901152
- Баранов В.С., Кузнецова Т.В. Цитогенетика эмбрионального развития человека. СПб.: Н-Л; 2006. 640 с.[Baranov V.S., Kuznetsova T.V. Cytogenetics of human embryonic development. SPb.: N-L; 2006. 640 s.(in Russian)]
- Фетисова И.Н., Дюжев Ж.А., Конева Т.Г., Липин М.А. Цитогенетические факторы первичного бесплодия и привычной потери беременности. Вестник новых медицинских технологий. 2008; 15(1): 43–4. [Fetisova I.N., Dyuzhev J.A., Koneva T.G., Lipin M.A. Cytogenetic Factors of Primary Infertility and Recurrent Pregnancy Loss. Vestnik novykh meditsinskikh tekhnologiy. 2008; 15(1): 43–4. (in Russian)].
- Kovaleva N.V. Examination of Rates and Spectrums of Robertsonian Translocations in the General Population and in Patients with Reproductive Disorders. Rus J Genet. 2018; 54(4): 489–93. doi:10.1134/S1022795418040099
- Scriven P.N., Flinter F.A., Braude P. R., Mackie Ogilvie C. Robertsonian translocations--reproductive risks and indications for preimplantation genetic diagnosis. Hum Reprod. 2001; 16(11): 2267–73. doi:10.1093/humrep/16.11.2267
- Uehara S., Akai Y., Takeyama Y., Takabayashi T., Okamura K., Yajima A. Pericentric Inversion of Chromosome 9 in Prenatal Diagnosis and Infertility. J Exp Med. 1992; 166(4): 417–27. doi: 10.1620/tjem.166.417
- Sahin F.I., Yi lmaz Z., Yuregir O.O., Bulakbasi T., Ozer O., Zeyneloglu H.B. Chromosome heteromorphisms: an impact on infertility. J Assist Reprod Gen. 2008; 25(5):191-5. doi: 10.1007/s10815-008-9216-3
- Caglayan A.O., Ozyazgan I., Demiryilmaz F., Ozgun M.T. Are heterochromatin polymorphisms associated with recurrent miscarriage? J Obstet Gynecol Res. 2010; 36(4): 774–6. doi: 10.1111/j.1447-0756.2010.01207.x
- Madon P.F., Athalye A.S., Parikh F.R. Pоlymorphic variants on chromosomes probably play a significant role in infertility. Reprod Biomed Online. 2005; 11(6): 726–32. doi:10.1016/S1472-6483(10)61691-4
- Minocherhomji S., Athalye A.S., Madon P.F., Kulkarni D., Uttamchandani S.A., Parikh F.R. A case-control study identifying chromosomal polymorphic variations as forms of epigenetic alterations associated with the infertility phenotype. Fertil Steril. 2009; 92(1): 88–95. doi: 10.1016/j.fertnstert.2008.05.071
- Li L.L., Peng D., Wang R.X., Zhu H.B., Wang W.J., Liu R.Z. Correlation between chromosomal polymorphisms and male infertility in a Northeast Chinese population. Genet. Mol. Res. 2015; 14 (4): 15435–5443. doi: 10.4238/2015.November.30.21
- Cheng R., Ma Y., Nie Y., Qiao X., Yang Z., Zeng R., Xu L..Chromosomal polymorphisms are associated with female infertility and adverse reproductive outcomes after infertility treatment: a 7-year retrospective study. Reprod Biomed Online. 2017; 35(1): 72–80. doi: 10.1016/j.rbmo.2017.03.022.
- Овчинников Р.И., Гамидов С.И., Попова А.Ю., Ушакова И.В., Голубева О.Н. Привычное невынашивание беременности – что зависит от мужчины? Акушерство и гинекология. 2016; 12: 15–23. [Ovchinnikov R.I., Gamidov S.I., Popova A.Yu., Ushakova I.V., Golubeva O.N. Recurrent miscarriage: What depends on a male partner? Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2016; (12): 15–23. (in Russian)]. http://dx.doi.org/10.18565/aig.2016.12.15-23
- Yakin K., Balaban B., Urman B. Is there a possible correlation between chromosomal variants and spermato-genesis? Int J Urol. 2005; 12(11): 984–9. doi: 10.1111/j.1442-2042.2005.01185.x
- Saran N., Kumar B., Kumar A. Chromosomal Heteromorphisms and Karyotype Abnormalities in Humans. Int J Curr Microbiol App Sci. 2017; 6(5): 2940–53 https://doi.org/10.20546/ijcmas.2017.605.333
- Morales R., Liedo B., Ortiz J., Ten J., Llacer J., Bernabeu R. Chromosomal polymorphic variants increase aneuploidies in male gametes and embryos. Syst Biol Reprod Med. 2016; 62(5): 317–24. doi: 10.1080/19396368.2016.1212949
Received 17.07.2019
Accepted 04.10.2019
About the Authors
Irina G. Khoroshilova, MD, student PhD, Center for Obstetrics, Gynecology and Perinatology, Almaty. Phone: +7 7013390169.E-mail: ira_horoshilova @ mail.ru; ORCID: https://orcid.org/0000-0001-9088-48477 050020, Republic of Kazakhstan, Almaty, Dostyk Ave,125.
Vyacheslav N. Lokshin , MD, professor, corresponding member NAS RK, President of the Kazakhstan Association of Reproductive Medicine, President of the International Academy of Reproductology, General Director of the International Clinical Center for Reproductology «PERSONA». Almaty. Phone: +7 7017558209.
E-mail:v_lokshin@persona-ivf.kz; ORCID: https://orcid.org/0000-0002-4792-53807 050060, Republic of Kazakhstan, Almaty, Utepova, 32A.
Aymira A. Begimbayeva, cytogenetics doctor, International Clinical Center for Reproductology «PERSONA». Phone: +7 7023302201.
E-mail: aimira.begimbayeva@mail.ru ORCID: https://orcid.org/0000-0002-7686-38287 050060, Republic of Kazakhstan, Almaty, st. Utepova, 32A.
Zhadyra K. Sarsenbayeva, doctor of cytogenetics, International Clinical Center for Reproductology «PERSONA». E-mail: zhadyradada@gmail.com;
ORCID: https://orcid.org/0000-0001-9808-72877 050060, Republic of Kazakhstan, Almaty, st. Utepova 32A.
Ravil K. Valiev, PhD, associate professor, head physician of the International Clinical Center for Reproductology “PERSONA Phone: + 7 7772258189.
E-mail:rvaliev75@mail.ru; ORCID: https://orcid.org/0000-0003-2526-42917 050060, Republic of Kazakhstan, Almaty, st. Utepova, 32A.
Anastassiya N. Rybina, MPh, reproductologist, International Clinical Center for Reproductology «PERSONA». Phone: +7 7772636715. E-mail:oedema@mail.ru;
ORCID: https://orcid.org/0000-0002-9368-66837 050060, Republic of Kazakhstan, Almaty, st. Utepova, 32A.
Sholpan K. Karibayeva, PhD, associate professor, deputy general director of the International Clinical Center for Reproductology «PERSONA».
Phone:+7 7017550675. E-mail:sh.karibaeva@gmail.com; ORCID: https://orcid.org/my-orcid7 050060, Republic of Kazakhstan, Almaty, ul. Utepova, 32A.
Alyena V. Kim, student of the Faculty of Biology and Biotechnology, Al-Farabi Kazakh National University, Republic of Kazakhstan, Almaty.
E-mail:alyena982401@gmail.com; ORCID: https://orcid.org/0000-0002-4504-85997 050040, Republic of Kazakhstan, Almaty, al-Farabi Ave, 71.
Nadezhda Yu. Semyonova, student of the Department of Biology and Biotechnology, Al-Farabi Kazakh National University, Republic of Kazakhstan,
Almaty. E-mail:grebenchshikova.nadezhda@gmail.com7 050040, Republic of Kazakhstan, Almaty, al-Farabi Ave, 71.
For citation: Khoroshilova I.G., Lokshin V.N., Begimbaeva A.A., Sarsenbaeva Zh.K., Valiev R.K., Rybina A.N., Karibaeva Sh.K., Kim A.V., Semenova N.Yu. Features of karyotypes in married couples with reproductive functional problems in Kazakhstan.
Akusherstvo i Ginekologiya/ Obstetrics and gynecology. 2020;1: 141-45. (In Russian).
https://dx.doi.org/10.18565/aig.2020.1.141-145