Use of cervical elastography to assess the effectiveness of labor pre-induction with a dilation catheter
Pachuliia O.V., Kopteeva E.V., Milyutina Yu.P., Khalenko V.V., Mokhnachev A.V., Bespalova O.N.
Objective: To assess the possibility of cervical elastography (compression elastography) use as a method for evaluating the effectiveness of pre-induction of labor in full-term pregnancy using a dilation catheter (double balloon and single-balloon Foley catheter).
Materials and methods: The study comprised 58 patients with singleton pregnancies at ≥37 weeks' gestation. Pre-induction was performed using two types of dilatation catheters. Cervical elastography and palpation using the Bishop score were performed before and after the procedure.
Results: The number of patients with an "absolutely soft" cervix according to the Bishop scale increased from 12% to 83% (p<0.001) after pre-induction of labor with a balloon catheter. According to elastography data of the anterior cervical lip, the proportion of "soft" and "very soft" cervix increased from 9% to 91% (p<0.001). We found high comparability of elastography data of the anterior cervical lip with the palpation data according to Bishop score (AUC=0.850). The relative risk of achieving optimal cervical maturity was 1.48 times higher when using a double balloon catheter, and the time to delivery was significantly shorter than when using a single balloon Foley catheter (p=0.033), without the increase in the incidence of complications.
Conclusion: Compression elastography is a new noninvasive tool for adequate assessment of the birth canal maturity, equal to the Bishop score. A double-balloon catheter is an effective and safe method for pre-induction of labor, ensuring faster achievement of cervical maturity.
Authors’ contributions: Pachuliia O.V., Kopteeva E.V., Milyutina Yu.P., Khalenko V.V., Mokhnachev A.V., Bespalova O.N. – study concept and design, collection, processing and analysis of materials, text composition and editing. All authors made a significant contribution to the elaboration of the study concept, study conduction and manuscript processing; read and approved the final manuscript version before publication.
Conflicts of interest: The authors declare no conflicts of interest.
Funding: The study was carried out within the framework of the Fundamental Research No. 1024032800227-5-3.2.2 “Medical and biological matrices of healthy maternity and fetal antenatal programming” (2025–2027).
Ethical Approval: The study protocol was approved by the local bioethics committee of the D.O. Ott Research Institute of Obstetrics, Gynecology and Reproductology.
Patient Consent for Publication: The patients signed informed consent for the publication of their data.
Authors' Data Sharing Statement. The data supporting the findings of this study are available on request from the corresponding author after approval from the principal investigator.
For citation: Pachuliia O.V., Kopteeva E.V., Milyutina Yu.P., Khalenko V.V., Mokhnachev A.V., Bespalova O.N.
Use of cervical elastography to assess the effectiveness of labor pre-induction with a dilation catheter.
Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2025; (12): 64-73 (in Russian)
https://dx.doi.org/10.18565/aig.2025.208
Keywords
In recent decades, pre-induction of labor is becoming more and more important in obstetric practice. According to research data, the need for pre-induction of labor occurs in 25–30% of cases in developed countries [1], while in some regions it reaches 40% [2]. In order to reduce the frequency of cesarean deliveries, the concept of programmed delivery has been introduced, which means term pregnancy of 39 weeks and more, with a mature fetus and a prepared cervix, that can be delivered at a time optimal for the mother, fetus and the medical facility [3]. One of the most important conditions for the successful programmed labor is cervical maturity, which indicates the readiness of the soft birth canal for childbirth [4].
The use of a double balloon dilatation catheter and an off-label Foley catheter is one of the mechanical methods of preparing the birth canal for childbirth [5]. This method involves applying pressure to the internal and external cervical os, promoting dilation of the cervical canal. Physical stimulation of the cervix leads to the local release of endogenous prostaglandins and increased levels of interleukin-6, -8, matrix metalloproteinases, nitric oxide synthase, and hyaluronan synhtase (HAS-1), which accelerate the maturation of the cervix [5].
A distinctive feature of the double balloon dilation catheter is a tighter contact with the cervical tissue, a lower frequency of catheter expulsion and minimization of the risk of uterine hyperstimulation [6]. Pre-induction of labor using a balloon catheter is especially relevant for patients with an unfavorable prognosis for cervical maturation and the presence of contraindications to pharmacological pre-induction [7]. Safety of mechanical labor pre-induction methods is confirmed by the absence of data on an increased risk of uterine rupture during childbirth and the development of chorioamnionitis, and the absence of the impact on the composition of the vaginal microbiota [7].
To assess the effectiveness of labor pre-induction, palpation examination of cervical maturity using the Bishop scale is traditionally used [3]. However, this method greatly depends on the experience of the clinician, which determines the low intra- and interobserver reproducibility of the method [4]. The large number of vaginal examinations performed on a single patient during pre-induction, induction, and subsequent labor raises alertness. Therefore, the search for alternative methods for assessing the effectiveness of labor pre-induction is urgent. In this regard, the use of ultrasound cervical (compression) elastography, which has become very popular in recent years, may prove promising [8].
Compression elastography is a method of color mapping of the “stiffness” of various tissue areas [9]. Despite the fact that this is an experienced-based method of visual assessment of the color elastography, there are various approaches aimed at standardizing the assessment. The scale of Gazhonova V.E. et al. (2008), used in gynecological practice, allows for the verification of 7 types of elastographic images based on a comparison of the number of pixels of a certain color [10]. A number of modern ultrasound devices also make it possible to quantitatively evaluate the elastography: E-cervixTM software automatically calculates quantitative indicators of cervical stiffness [11]. However, the widespread implementation of high-tech equipment is associated with economic burden, need for qualified specialists, and methods standardization.
Objective of the study: to assess the possibility of cervical elastography (compression elastography) use as a method for evaluating the effectiveness of pre-induction of labor in full-term pregnancy using a dilation catheter (double balloon and single-balloon Foley catheter).
Materials and methods
Study design
A single-center prospective cohort study was conducted at the D.O. Ott Research Institute for Obstetrics, Gynecology and Reproductology. The cohort included patients with singleton pregnancies at ≥37 weeks of gestation, cephalic presentation, an estimated fetal weight of less than 4,500 g based on ultrasound data, and a soft birth canal with a Bishop score of ≤6. Exclusion criteria included premature rupture of membranes and past cervical surgery. Indications for mechanical pre-induction of labor using a dilation catheter were regulated by relevant clinical guidelines. All patients signed informed consent to participate in the study. The study protocol was approved by the local bioethics committee. As a result, 62 patients were included in the study. Four patients were subsequently excluded from the study due to premature rupture of membranes or the inability to undergo compression elastography after labor pre-induction. The 58 patients included in the study underwent birth canal preparation with cervical dilatation catheters: a double balloon catheter (n=36) or a single balloon Foley catheter (n=22).
The following data were assessed before and after labor pre-induction: cervical maturity (using the Bishop scale), cervical length (using ultrasound cervicometry), and elastometry of the anterior and posterior cervical lips. All procedures were performed by a single specialist.
Procedure description
Labor pre-induction included the birth canal preparation using a cervical dilation balloon catheter (single or double balloon) in the pregnancy pathology department according to standard procedures. The double balloon dilation catheter design features two balloons positioned sequentially at one end, each filled with fluid (saline) up to 80 ml. The distal balloon is positioned in the lower uterine segment of the internal os, while the proximal balloon is positioned in the vaginal side of the external os. A single-balloon catheter was inserted beyond the internal os and filled with 80 ml of fluid. The catheter was inserted until it spontaneously prolapsed, with the exposure time not exceeding 24 hours. A longer exposure time is considered to be optimal.
All patients underwent vaginal microbiome examination before and after catheter placement.
A palpatory examination to assess cervical maturity was performed before catheter placement and after its removal or spontaneous expulsion. A modified Bishop scale (1966) with 5 parameters was used. The Bishop scores were transformed and distributed into the following categories: 0 to 2 points – "absolutely dense," 3 to 5 – "relatively dense," 6 and 7 – "relatively soft," 8 and above – "absolutely soft.".
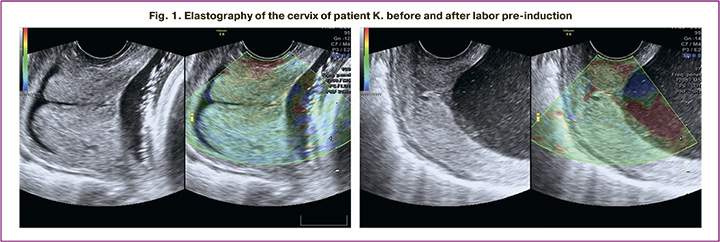
Before and after pre-induction of labor, a cervical ultrasound was performed using a Voluson E6 (General Electric) multifrequency pelvic transducer. The examination was performed using B-mode cervical ultrasound assessment (cervicometry) under the empty bladder, and compression elastography of the anterior and posterior labial cervix (Figure 1).
Elastometry interpretation
In accordance with classical elastography all obtained images of the cervix were colored in red – softer areas, green – areas of medium density, and blue – dense areas. Based on the ratio of color pixels, the results of the elastography study were ranked into 4 categories in accordance with the modified scale by Gazhonova V.E. [10]: 1 – “very dense cervix” (corresponds to category 3), 2 – “dense cervix” (corresponds to category 2a), 3 – “soft cervix” (corresponds to category 2b), 4 – “very soft cervix” (corresponds to category 2c). The anterior and posterior cervical lips were assessed separately.
Major outcomes
The primary outcome demonstrated the impact of the dilatation catheter on labor pre-induction effectiveness and a change in the degree of cervical maturity, which is achieving of optimal readiness of the birth canal for childbirth (8 or more points on the Bishop scale).
Secondary outcomes were presented with spontaneous onset of labor after pre-induction with a dilation catheter; onset of labor within 24 hours after placement of a dilation catheter; and vaginal delivery.
Statistical analysis
Statistical analysis was performed with Statistica software (version 10, Statsoft, USA).
Quantitative indicators were assessed for normal distribution using the Kolmogorov–Smirnov test. Normally distributed indicators were compared using the t-test for independent samples and described using arithmetic means (M) and standard deviations (SD). For distributions other than normal, quantitative data were compared using the Mann–Whitney test and described featuring the median, upper and lower quartiles – Me (Q1–Q3). Categorical data were showed using absolute values and percentages. When comparing indicators measured on a nominal or ordinal scale, we took the Pearson's χ2 test, while for small samples this criterion was calculated with Yates's correction, or a two-tailed Fisher's exact test. The Friedman test was used to compare related rank variables (cervical compression elastography and Bishop scale scores). The Bland–Altman comparison of methods helped to compare the comparability of the compression elastography method with the palpatory assessment of the cervix using the Bishop scale. To confirm the prognosis for cervix maturity (based on Bishop) with the elastography assessment, a logistic regression method was used with the construction of ROC-curve. The normality of the residual distribution was analyzed using the Shapiro–Wilk test of standardized residuals. Outliers were analyzed using the Cook's distance estimator. To assess the risk of the primary outcomes, a relative risk (RR) calculation was performed with a 95% CI.
Results
Clinical characteristics of the study groups
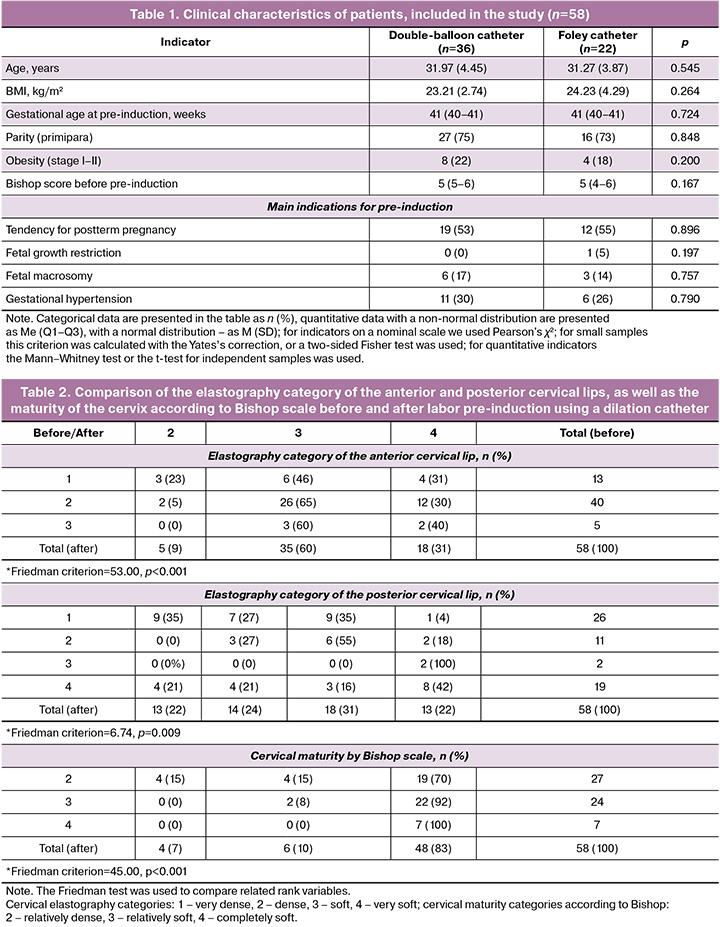
Table 1 represents the clinical characteristics of the patients included in the study. The comparison groups were matched for age, BMI, parity, gestational age at pre-induction, and indications for pre-induction (p>0.05). In more than half of the cases the indication for pre-induction was a tendency toward postterm pregnancy. In one-third of cases, the indication for labor pre-induction was hypertensive disorders during pregnancy. The median Bishop score was 5 for both groups.
Cervical elastography
To assess the comparability of cervical compression elastography and Bishop score results, we analyzed data in all study groups. Before labor pre-induction, most anterior cervical lip elastography images described the cervix as “dense” and “very dense” – 53/58 (91%), whereas after labor pre-induction, 53/58 (91%) elastography data showed “soft” and “very soft” cervix (Friedman criterion=53.00, p<0.001, Table 2). When analyzing the elastography images of the posterior cervical lip before pre-induction of labor, 37/58 (64%) cases were assessed as “very dense” and “dense”. After pre-induction of labor, 13/58 (22%) elastography data were also classified as “very dense” and 14/58 (24%) as “dense”. At the same time, the number of elastography images that demonstrated "soft" cervix increased up to 18/58 (31%) (Friedman criterion=6.74, p=0.009).
No patients in the study had an absolutely dense cervix (category 1) according to the Bishop scale (0 to 2 points), and therefore this category was excluded from the analysis. The majority of patients – 27/58 (47%) – had a “relatively dense” cervix (3–5 points at Bishop scale) before labor pre-induction, while 24/58 (41%) had a “relatively soft” cervix (6–7 points at Bishop scale). Whereas after labor pre-induction, 48/58 (83%) patients had an “absolutely soft” cervix (8 points or more) (Friedman criterion=45.00, p<0.001). The median Bishop score accounted for 5 before labor pre-induction and 10 points after labor pre-induction (p<0.001).
To compare the comparability of the compression elastography with the palpatory cervical assessment using the Bishop scale, we used a Bland–Altman plot. This analysis demonstrated an acceptable degree of comparability of the palpatory examination and elastography data for the anterior cervical lip (Fig. 2a) and a low degree of data comparability for the posterior cervical lip (Fig. 2b). After analyzing the comparability data of the posterior cervical lip, we observed values exceeding the threshold of ±1.96 SD.
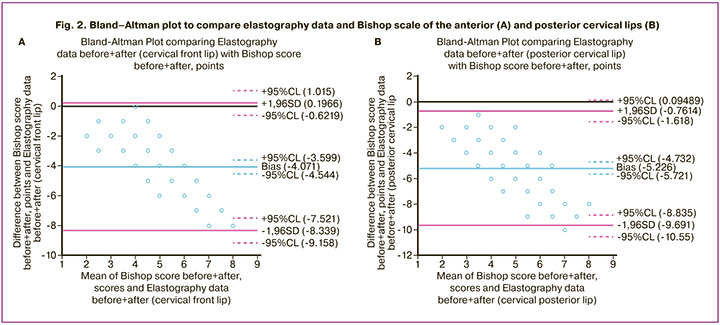
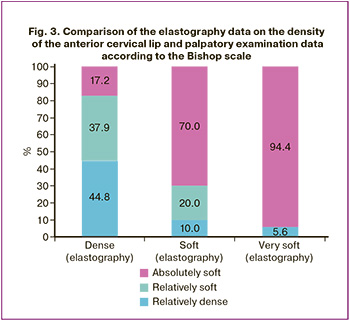
Figure 3 illustrates three Bishop score categories: relatively dense (n=31), relatively soft (n=30), and absolutely soft (n=55) cervix, and three elastography levels of cervical density: dense (n=58), soft (n=40), and very soft (n=18). It is important to note that the most prognostically significant elastography finding is a “very soft” cervix, as it largely coincides with the Bishop classification (94.4%). It was also noted that as cervical “softness” increases, as demonstrated by elastography of the anterior cervical lip, the number of cases identified as “completely soft cervix” according to the Bishop scale also grows.
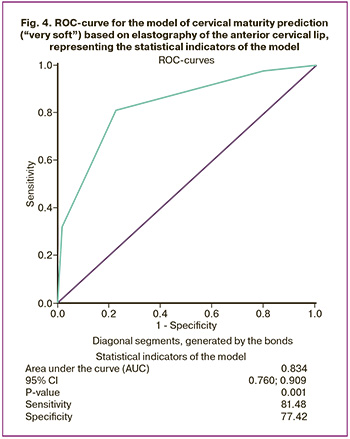
Based on the comparison of the obtained data from palpation and ultrasound examination of the cervix (Bland–Altman analysis) in pregnant women before and after labor pre-induction, a prognostic model was elaborated to assess the achievement of optimal cervical maturity (the “soft” and “very soft” cervix according to Bishop score) according to the anterior labial elastography. A formula was derived to calculate the predicted probability: p = 1/(1+e-z),
where: p is the predicted probability of achieving optimal cervical maturity; at p<0.66 – the cervix is “solid”, at p>0.66 – the maturity tends to be optimal; e – base of natural logarithm 2,71; z – logistic regression equation:
z = -5,221+1,976×elastography category.
The threshold chosen was the predicted probability value is p=0.66, which corresponds to the elastography category 3.
The logistic regression model had the following characteristics: intercept Wald – 28.870, p<0.001; elastography assessment Wald – 29.281, p<0.001, Exp(B) = 7.215 [3.527; 14.761]. No outliers were detected, the residuals were normally distributed.
Based on the obtained predicted probability of cervical maturity, a ROC-curve was constructed using the logistic regression method (Fig. 4).
Evaluation of the effectiveness of labor pre-induction with a double balloon catheter and a Foley catheter
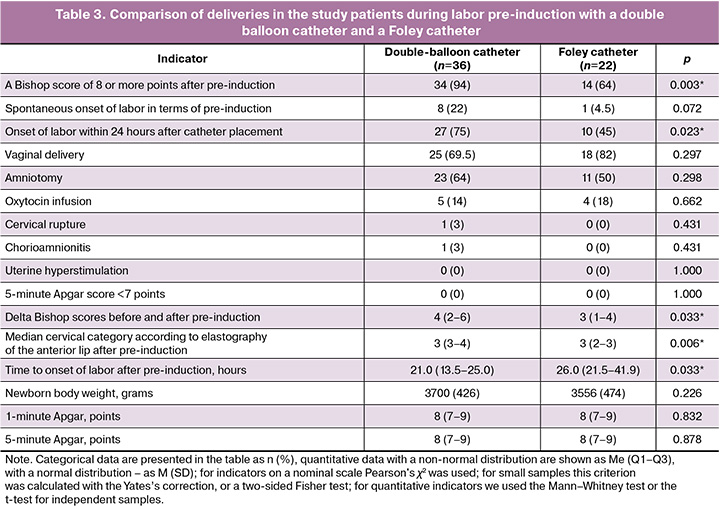
A Bishop score of 8 or more points after labor pre-induction was achieved in 34/36 (94%) patients who received pre-induction with a double balloon catheter, compared with 14/22 (64%) in the Foley catheter group (p=0.003). When using a double balloon catheter, the delta Bishop scores before and after labor pre-induction was higher (Me – 4 points) compared to a Foley catheter (Me – 3 points, p=0.033). The same tendency described the median of the cervix according to elastography of the anterior lip after pre-induction (p=0.006). The analysis showed that the rates of amniotomy and induction of labor when using oxytocin did not differ significantly between the groups (p>0.05). A trend toward an increased rate of spontaneous labor was noted in the double-balloon catheter group (22% versus 4.5% in the Foley catheter group, p=0.072).
An important advantage of using a double balloon catheter included the significantly faster onset of labor – an average of 21 hours versus 26 hours in the Foley catheter group (p=0.033).
The rates of operative delivery, cervical rupture, as well as neonatal body weight, and Apgar score were comparable between the study groups (p>0.05). The incidence of complications, such as chorioamnionitis and uterine hyperstimulation, was minimal and did not differ between the study groups (Table 3).
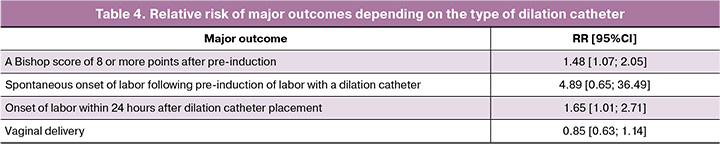
The relative risk (RR) of achieving a Bishop score of 8 or more (RR=1.48) points and the onset of labor within 24 hours after catheter placement (RR=1.65) was higher in the double balloon catheter group (Table 4). The RR of spontaneous onset of labor and vaginal delivery did not differ significantly between the groups.
Discussion
The achieved results demonstrated that elastography of the anterior cervical lip can be used to assess the cervical maturity before and after labor pre-induction and is comparable to palpatory assessment with the Bishop scale. The purpose of using ultrasound cervical elastography is to reduce the number of vaginal examinations, as well as to increase the objectivity of assessing the maturity of cervix. The use of a double balloon catheter for labor pre-induction raises the likelihood of cervical maturation by 1.5 times and ensures a faster onset of labor, compared with a Foley catheter, without increasing the risk of complications.
The process of cervical maturation or remodeling is an integral part of the pathophysiology of labor. Current methods for assessing cervical function during pregnancy include ultrasound cervicometry, the Bishop score, and biochemical tests (IGFBP-1, PAMG-1, fetal fibronectin). However, all of these methods have limitations and low predictive value for the effectiveness of labor preinduction.
Ultrasound cervical elastography is a promising non-invasive and safe method for assessing the effectiveness of labor pre-induction [12]. In this context, elastography is more informative than traditional methods, as it reflects the degree of softening (maturity) of the cervix [13].
Previous studies assessed the potential role of various elastography methods in predicting the effect of the pharmacological labor induction [14–18]. Swiatkowska-Freund M. et al. (2011) and Preis K. et al. (2010) were the first to show that elastography predicts the results of labor induction with oxytocin better than palpatory assessment according to the Bishop scale [14, 15]. The results of Wozniak S. et al. (2015) demonstrate that using elastography index assessment, it is possible to predict successful labor induction with a Foley catheter [8]. In the studies by Hee L. et al. (2014) and Fruscalzo A. et al. (2015), it was demonstrated that quantitative elastography is superior to the Bishop score and cervical length assessment in predicting the time of cervical maturation and the risk of prolonged labor induction when using prostaglandins [17, 18]. Brega E.S. et al. (2019) found a strong correlation between the Bishop score and the Strain Ratio (obtained by performing compression elastography) before cervical preparation for labor using combined methods [19]. High intra- and interobserver reproducibility was demonstrated when using various cervical elastography techniques [16, 18].
It's worth noting that the main limitations of this method are associated with the visual assessment of the elastography color map and the subjectivity of this approach. Some modern software (e.g., E-cervix, Samsung Medison) can quantify elastography parameters, but the lack of reference values also indicates the need for further development in this area [11].
An important feature of the study is the high comparability of elastography results with the Bishop score. Furthermore, we demonstrated the high prognostic value of ultrasound elastography in predicting “absolutely soft” cervix comparing to the Bishop score (more than 8 points). In our study, the best results of elastography conssitency with the Bishop score were obtained for the anterior cervical lip, located as close as possible to the sensor, which is associated with the peculiarities of the propagation of ultrasound waves in tissues.
The condition of the cervix before labor pre-induction can be a decisive factor for successful vaginal delivery. For example, a study by Fruscalzo A. et al. (2015) demonstrated that in women with cervical stiffness above 30 kPa, the probability of unsuccessful induction accounted for 70% [18]. Hwang H.S. et al. (2013) reported that high elastography index values in women with successful pre-induction correlated with better delivery outcomes [16]. This work highlights that elastography values before pre-induction may become prognostic markers of labor success, providing clinicians with additional information for decision-making [16].
The application of mechanical methods of labor pre-induction using a double-balloon catheter and a Foley catheter demonstrated comparable high efficacy of both techniques. We found that a double-balloon catheter makes it significantly shorter till the onset of labor compared to a Foley catheter. The study did not reveal any complications during pre-induction and the delivery process, which indicates the safety of this method.
A unique feature of the double-balloon catheter is that the mechanical exposure is provided by two balloons by the side of the internal and external os, thereby creating a tighter contact with the cervical tissues and increasing the stretching pressure on the lower uterine segment [1].
According to Baev O.R. et al. (2019) [20], the use of a double balloon catheter is associated with an increase in the Bishop score by an average of 3 points; in 60% of cases vaginal delivery occurred, which is comparable with the results obtained.
According to the research data, there are a sufficient number of foreign randomized clinical trials comparing the Foley catheter and the double balloon catheter in terms of the effectiveness of labor pre-induction and its safety for the mother and fetus [1]. However, the results of these studies are contradictory. Some authors demonstrated the comparability of the effectiveness and safety of these methods [21–25]. Xing Y. et al. (2019) and Hoppe K.K. et al. (2016) obtained better results when using a double balloon catheter [24, 26], while other authors used a Foley catheter [27, 28].
Previous meta-analyses showcased comparable safety of these methods both for maternal (uterine hyperstimulation, chorioamnionitis, etc.) and perinatal (Apgar score <7 at 5 minutes) outcomes [29–31]. The key factor to achieve the positive results in mechanical labor pre-induction is a unified mechanism of pathogenetic impact on the cervix maturation, promoting dilation of the cervical canal and local release of prostaglandins. Therefore, single- and double-balloon catheters are expected to have comparable safety profiles [1].
It is important to understand that the use of balloon catheters is the most controllable method of labor pre-induction, which allows the clinician to monitor and adjust the course of the procedure depending on the individual patient's responses [32]. A study by De Bonrostro Torralba C. et al. (2017) on mechanical induction of labor in women with a history of cesarean section showed that after the use of a double balloon catheter, 61% of women achieved optimal cervical maturity, with 51.4% of vaginal deliveries [33]. The incidence of adverse events was low, which makes this a better choice in patients with a history of cesarean section [33].
Conclusion
To sum up, compression elastography can be used to assess cervical maturity based on certain cervical elastography category, and its integration into the labor preparation process will reduce the number of vaginal examinations and predict the effectiveness of pre-induction. However, we need further studies on a larger sample of patients to assess the impact of elastography thresholds on pre-induction outcomes.
References
- Hamza A., Radosa J., Gerlinger C., Solomayer E.F., Ströder R., Meyberg-Solomayer G. Cervical and lower uterine parameter ultrasound and elastographic parameters for the prediction of a successful induction of labor. Ultraschall Med. 2021; 42(5): 520-8. https://dx.doi.org/10.1055/a-1131-7736
- Cheuk Q.K., Lo T.K., Lee C.P., Yeung A.P. Double balloon catheter for induction of labour in Chinese women with previous caesarean section: one-year experience and literature review. Hong Kong Med. J. 2015; 21(3): 243-50. https://dx.doi.org/10.12809/hkmj144404
- Ткаченко Л.В., Веровская Т.А., Костенко Т.И., Складановская Т.В., Свиридова Н.И., Бабаева Л.К. Применение классификации робсона для поиска путей снижения частоты операций кесарева сечения. Вестник ВолгГМУ. 2020; 2(74): 87-90. [Tkachenko L.V., Verovsky T.A., Kostenko T.I., Skladanowsky T.V., Sviridova N.I., Babayeva L.K. Applying the robson classification to find ways to reduce the frequency of cesarean section operations. Journal of Volgograd State Medical University. 2020; 2(74): 87-90 (in Russian)]. https://dx.doi.org/10.19163/1994-9480-2020-2(74)-87-90
- Ma K., Yang M., Feng X., Liu L., Li L., Li Y. Predictors of vaginal delivery following balloon catheter for labor induction in women with one previous cesarean. BMC Pregnancy Childbirth. 2023; 23(1): 417. https://dx.doi.org/10.1186/s12884-023-05734-y
- Solt I., Frank Wolf M., Ben-Haroush S., Kaminskyi S., Ophir E., Bornstein J. Foley catheter versus cervical double balloon for labor induction: a prospective randomized study. J. Matern. Fetal Neonatal. Med. 2021; 34(7): 1034-41. https://dx.doi.org/10.1080/14767058.2019.1623776
- Ten Eikelder M.L., Mast K., van der Velden A., Bloemenkamp K.W., Mol B.W. Induction of labor using a Foley catheter or misoprostol: a systematic review and meta-analysis. Obstet. Gynecol. Surv. 2016; 71(10): 620-30. https://dx.doi.org/10.1097/OGX.0000000000000361
- Kehl S., Weiss C., Rath W. Balloon catheters for induction of labor at term after previous cesarean section: a systematic review. Eur. J. Obstet. Gynecol. Reprod. Biol. 2016; 204: 44-50. https://dx.doi.org/10.1016/j.ejogrb.2016.07.505
- Wozniak S., Czuczwar P., Szkodziak P., Paszkowski T. Usefulness of elastography in predicting the outcome of Foley catheter labour induction. Aust. N. Z. J. Obstet. Gynaecol. 2015; 55(3): 245-50. https://dx.doi.org/10.1111/ajo.12331
- Diaz A., Aedo S., Burky D., Catalan A., Aguirre C., Acevedo M. et al. Sonographic cervical length predicts vaginal delivery after previous cesarean section in women with low Bishop score induced with a double-balloon catheter. J. Matern. Fetal Neonatal. Med. 2022; 35(24): 4830-6. https://dx.doi.org/10.1080/14767058.2020.1868430
- Гажонова В.Е., Чуркина С.О., Хохлова Е.А., Панфилова Е.А., Лукьянова Е.С., Андрияничева Е.Н., Зубарев А.В. Клиническое применение нового метода соноэластографии в гинекологии. Кремлевская медицина. Клинический вестник. 2008; 2; 18-23. [Gazhonova V.E., Churkina S.O., Khokhlova E.A., Panfilova E.A., Lukyanova E.S., Andrianicheva E.N., Zubarev A.V. Clinical application of the new method of sonoelastography in gynecology. Kremlin Medicine. Clinical Bulletin. 2008; 2; 18-23 (in Russian)].
- Халенко В.В., Коптеева Е.В., Беспалова О.Н., Пачулия О.В., Корнюшина Е.А., Коган И.Ю. Пилотное исследование CELASTO (Сervical ELASTOgraphy): цервикометрия с использованием соноэластографии при беременности. Журнал акушерства и женских болезней. 2024; 73(2): 89-98. [Khalenko V.V., Kopteeva E.V., Bespalova O.N., Pachulia O.V., Kornyushina E.A., Kogan I.Yu. CELASTO (Сervical ELASTOgraphy) pilot study: cervicometry using sonoelastography in pregnancy. Journal of Obstetrics and Women's Diseases. 2024; 73(2): 89-98 (in Russian)]. https://dx.doi.org/10.17816/JOWD623593
- Londero A.P., Schmitz R., Bertozzi S., Driul L., Fruscalzo A. Diagnostic accuracy of cervical elastography in predicting labor induction success: a systematic review and meta-analysis. J. Perinat. Med. 2016; 44(2): 167-78. https://dx.doi.org/10.1515/jpm-2015-0035
- Kim H., Hwang H.S. Elastographic measurement of the cervix during pregnancy: Current status and future challenges. Obstet. Gynecol. Sci. 2017; 60(1): 1-7. https://dx.doi.org/10.5468/ogs.2017.60.1.1
- Swiatkowska-Freund M., Preis K. Elastography of the uterine cervix: implications for success of induction of labor. Ultrasound Obstet. Gynecol. 2011; 38(1): 52-6. https://dx.doi.org/10.1002/uog.9021
- Preis K., Swiatkowska-Freund M., Pankrac Z. [Elastography in the examination of the uterine cervix before labor induction]. Ginekol. Pol. 2010; 81(10): 757-61. [Article in Polish].
- Hwang H.S., Sohn I.S., Kwon H.S. Imaging analysis of cervical elastography for prediction of successful induction of labor at term. J. Ultrasound Med. 2013; 32(6): 937-46. https://dx.doi.org/10.7863/ultra.32.6.937
- Hee L., Rasmussen C.K., Schlütter J.M., Sandager P., Uldbjerg N. Quantitative sonoelastography of the uterine cervix prior to induction of labor as a predictor of cervical dilation time. Acta Obstet. Gynecol. Scand. 2014; 93(7): 684-90. https://dx.doi.org/10.1111/aogs.12389
- Fruscalzo A., Londero A.P., Fröhlich C., Meyer-Wittkopf M., Schmitz R. Quantitative elastography of the cervix for predicting labor induction success. Ultraschall Med. 2015; 36(1): 65-73. https://dx.doi.org/10.1055/s-0033-1355572
- Брега Е.С., Пекарев О.Г., Гус А.И., Луньков С.С. Клинико-эластографическая оценка вариантов подготовки «незрелой» шейки матки. Акушерство и гинекология. 2019; 10: 81-91. [Brega E.S., Pekarev O.G., Gus A.I., Lun’kov S.S. Clinical and elastographic evaluation of methods for ripening an unripe cervix. Obstetrics and Gynecology. 2019; (10): 81-91 (in Russian)]. https://dx.doi.org/10.18565/aig.2019.10.81-91
- Баев О.Р., Бабич Д.А., Шмаков Р.Г., Полушкина Е.С., Николаева А.В. Опыт применения двухбаллонного катетера для подготовки к родам. Акушерство и гинекология. 2019; 3: 64-71. [Baev O.R., Babich D.A., Shmakov R.G., Polushkina E.S., Nikolaeva A.V. Experience of using a double balloon catheter for cervical ripening in the induction of labor. Obstetrics and Gynecology. 2019; (3): 64-71 (in Russian)]. https://dx.doi.org/10.18565/aig.2019.3.64-71
- Peel M.D., Croll D.M.R., Kessler J., Haugland B., Pennell C.E., Dickinson J.E. et al. Double-vs single-balloon catheter for induction of labor: systematic review and individual participant data meta-analysis. Acta Obstet. Gynecol. Scand. 2023; 102(11): 1440-9. https://dx.doi.org/10.1111/aogs.14626
- Obut M., Balsak D., Sarsmaz K., Tolunay H.E., Varlı E.N., Şahin D. et al. Double Foley catheter for labor induction: an alternative method. Int. J. Gynaecol. Obstet. 2021; 155(3): 496-504. https://dx.doi.org/10.1002/ijgo.13807
- Salim R., Zafran N., Nachum Z., Garmi G., Kraiem N., Shalev E. Single-balloon compared with double-balloon catheters for induction of labor: a randomized controlled trial. Obstet. Gynecol. 2011; 118(1): 79-86. https://dx.doi.org/10.1097/AOG.0b013e318220e4b7
- Xing Y., Li N., Ji Q., Hong L., Wang X., Xing B. Double-balloon catheter compared with single-balloon catheter for induction of labor with a scarred uterus. Eur. J. Obstet. Gynecol. Reprod. Biol. 2019; 243: 139-43. https://dx.doi.org/10.1016/j.ejogrb.2019.10.041
- de Los Reyes S.X., Sheffield J.S., Eke A.C. Single versus double-balloon transcervical catheter for labor induction: a systematic review and meta-analysis. Am. J. Perinatol. 2019; 36(8): 790-7. https://dx.doi.org/10.1055/s-0038-1675206
- Hoppe K.K., Schiff M.A., Peterson S.E., Gravett M.G. 30 mL single - versus 80 mL double-balloon catheter for pre-induction cervical ripening: a randomized controlled trial. J. Matern. Fetal Neonatal. Med. 2016; 29(12): 1919-25. https://dx.doi.org/10.3109/14767058.2015.1067297
- Sayed Ahmed W.A., Ibrahim Z.M., Ashor O.E., Mohamed M.L., Ahmed M.R., Elshahat A.M. Use of the Foley catheter versus a double balloon cervical ripening catheter in pre-induction cervical ripening in postdate primigravidae. J. Obstet. Gynaecol. Res. 2016; 42(11): 1489-94. https://dx.doi.org/10.1111/jog.13086
- Pennell C.E., Henderson J.J., O'Neill M.J., McChlery S., Doherty D.A., Dickinson J.E. Induction of labour in nulliparous women with an unfavourable cervix: a randomised controlled trial comparing double and single balloon catheters and PGE2 gel. BJOG. 2009; 116(11): 1443-52. https://dx.doi.org/10.1111/j.1471-0528.2009.02279.x
- de Vaan M.D., Ten Eikelder M.L., Jozwiak M., Palmer K.R., Davies-Tuck M., Bloemenkamp K.W. et al. Mechanical methods for induction of labour. Cochrane Database Syst. Rev. 2019; 10(10): CD001233. https://dx.doi.org/10.1002/14651858.CD001233.pub3
- Salim R., Schwartz N., Zafran N., Zuarez-Easton S., Garmi G., Romano S. Comparison of single- and double-balloon catheters for labor induction: a systematic review and meta-analysis of randomized controlled trials. J. Perinatol. 2018; 38(3): 217-25. https://dx.doi.org/10.1038/s41372-017-0005-7
- Liu X., Wang Y., Zhang F., Zhong X., Ou R., Luo X. et al. Double- versus single-balloon catheters for labour induction and cervical ripening: a meta-analysis. BMC Pregnancy Childbirth. 2019; 19(1): 358. https://dx.doi.org/10.1186/s12884-019-2491-4
- Bleicher I., Dikopoltsev E., Kadour-Ferro E., Sammour R., Gonen R., Sagi S. et al. Double-balloon device for 6 compared with 12 hours for cervical ripening: a randomized controlled trial. Obstet. Gynecol. 2020; 135(5): 1153-60. https://dx.doi.org/10.1097/AOG.0000000000003804
- De Bonrostro Torralba C., Tejero Cabrejas E.L., Marti Gamboa S., Lapresta Moros M., Campillos Maza J.M., Castán Mateo S. Double-balloon catheter for induction of labour in women with a previous cesarean section, could it be the best choice? Arch. Gynecol. Obstet. 2017; 295(5): 1135-43. https://dx.doi.org/10.1007/s00404-017-4343-7
Received 04.08.2025
Accepted 27.11.2025
About the Authors
Olga V. Pachuliia, PhD, Senior Researcher at the Department of Obstetrics and Perinatology, D.O. Ott Research Institute of Obstetrics, Gynecology and Reproductology, 199034, Russia, St. Petersburg, Mendeleevskaya line, 3, for.olga.kosyakova@gmail.com, https://orcid.org/0000-0003-4116-0222Ekaterina V. Kopteeva, PhD, Scientific Secretary, D.O. Ott Research Institute of Obstetrics, Gynecology and Reproductology, 199034, Russia, St. Petersburg,
Mendeleevskaya line, 3, +7(911)218-86-69, ekaterina_kopteeva@bk.ru, https://orcid.org/0000-0002-9328-8909
Yulia P. Milyutina, Dr. Bio. Sci., Leading Researcher at the Laboratory of Biochemistry of Reproduction and Medical and Environmental Problems, D.O. Ott Research Institute of Obstetrics, Gynecology and Reproductology, 199034, Russia, St. Petersburg, Mendeleevskaya line, 3, milyutina1010@mail.ru, https://orcid.org/0000-0003-1951-8312
Vladislava V. Khalenko, Junior Researcher at the Department of Reproductology, D.O. Ott Research Institute of Obstetrics, Gynecology and Reproductology,
199034, Russia, St. Petersburg, Mendeleevskaya line, 3, vkhalenko@gmail.com, https://orcid.org/0000-0001-5313-2259
Alexander V. Mokhnachev, PhD student, D.O. Ott Research Institute of Obstetrics, Gynecology and Reproductology, 199034, Russia, St. Petersburg, Mendeleevskaya line, 3, mokhnachev.alexander@yandex.ru, https://orcid.org/0000-0002-6929-3396
Olesya N. Bespalova, Dr. Med. Sci., Deputy Director for Science, D.O. Ott Research Institute of Obstetrics, Gynecology and Reproductology,
199034, Russia, St. Petersburg, Mendeleevskaya line, 3, shiggerra@mail.ru, https://orcid.org/0000-0002-6542-5953
Corresponding author: Ekaterina V. Kopteeva, ekaterina_kopteeva@bk.ru