The frequency of caesarean section and neonatal outcomes depending on management strategy for large‑for‑gestational‑age pregnancy
Fetal macrosomia is a risk factor for adverse obstetric outcomes, such as operative vaginal delivery, cesarean section and shoulder dystocia. With fetal macrosomia, the effectiveness of reducing the frequency of operative delivery is still a matter of debate. More promising is to study a possibility of early-term delivery in women with large-for gestational-age (LGA) fetuses, who have not yet reached the criteria for defining macrosomia.Tysyachnyi O.V., Baev O.R., Prikhodko A.M., Kepsha M.A.
Objective: To evaluate the frequency of operative delivery in pregnant women with LGA fetuses, depending on management strategy (pre-induction/ induction of labor or expectant management) and gestational age.
Materials and methods: A retrospective cohort study included 478 healthy primiparous women with delivery of large-for-gestational age fetuses according to ultrasound data. The women were divided into two groups. The comparison group was expectant management (n=195) and the main group was induction of labor (n=283). Both groups were divided into three subgroups depending on gestational age: subgroup 1 included women who were 38 weeks pregnant, subgroup 2 – 39 weeks, subgroup 3 – 40 weeks.
Results: The frequency of cesarean section in the group of women with spontaneous onset of labor at 38 and 39 weeks was 33.3% and 20.5% versus 22.2% and 17.1% in the induction group (p>0.05). At the same time, the frequency of cesarean section at 40 weeks was significantly lower in the expectant management group, 21.8% versus 36.9%, p=0.02. There were no differences between the rates of vaginal delivery, fetal shoulder dystocia, and perinatal outcomes. However, in the expectant management group at 39 weeks, there were significantly more newborns with Apgar score of 7 or less, 12.8% versus 4.04% in the induction group, p=0.04.
Conclusion: In most cases, the formation of macrosomia was between 39–40 weeks, and induction of labor as a method for preventing complications associated with macrosomia was ineffective. It is apparent that, the optimal gestational age for delivery was 39 weeks for ultrasound-estimated fetal weight equal to the 90th percentile, 38 weeks for the 95th percentile, and 37–38 weeks for the 97th percentile.
Authors’ contributions: Tysyachnyi O.V. – statistical data processing, article writing, Baev O.R. – article editing, Prikhodko A.M. – design of the study, Kepsha M.A. – material collection and processing.
Conflicts of interest: The authors declare that they have no conflicts of interest.
Funding: The study was carried out without any sponsorship.
Ethical Approval: The study was approved by the local Ethics Committee of the National Medical Research Center for Obstetrics, Gynecology and Perinatology named after Academician V.I. Kulakov of the Ministry of Health of the Russian Federation.
Patients’ Consent for Publication: The patients have signed informed consent for publication of their data.
Authors' Data Sharing Statement: The data supporting the findings of this study are available on request from the corresponding author after approval from the principal investigator.
For citation: Tysyachnyi O.V., Baev O.R., Prikhodko A.M., Kepsha M.A. The frequency of caesarean section and neonatal outcomes depending on management strategy for large-for-gestational-age pregnancy.
Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2023; (5): 29-36 (in Russian)
https://dx.doi.org/10.18565/aig.2023.33
Keywords
It is known that fetal macrosomia is a risk factor for adverse obstetric outcomes, such as operative vaginal delivery, cesarean section and shoulder dystocia [1, 2]. Currently, there is a clear trend towards the increased average birthweight and the incidence of fetal macrosomia. The studies showed that from 1986 to 2012 the birthweight increased on average by 44 g [3].
In modern clinical practice, there are two terms applicable for excessive fetal weight – “fetal macrosomia” and “lage for gestational age”. The term “macrosomia” is used, when birth weight is equal to 4.0 kg or over, despite the length of pregnancy [4]. At the same time, the term “lage for gestational age” refers to fetal weight equal to the 90th percentile or larger for a given gestational age, that is defined by diagnostic ultrasound [5].
One of the methods for prevention of obstetric complications is labor induction [6]. However, with fetal macrosomia, the effectiveness of reducing the frequency of operative delivery is still a matter of debate. More promising is to study a possibility of early-term delivery in women with large-for gestational-age (LGA) fetuses, who have not yet reached the criteria for defining macrosomia.
The purpose of the study was to evaluate the frequency of operative delivery in pregnant women with LGA fetuses, depending on management strategy (pre-induction/ induction of labor or expectant management) and gestational age.
Materials and methods
A retrospective cohort study including the analysis of 26 386 bith histories from electronic database in the period from 2020 to 2022 was conducted in the National Medical Research Center for Obstetrics, Gynecology and Perinatology named after Academician V.I. Kulakov of the Ministry of Health of the Russian Federation.
Inclusion criteria were: primiparous women aged 18–40 years, spontaneous conception and singleton pregnancy, cephalic presentation of the fetus, full-term pregnancy, fetuses large for gestational age according to diagnostic ultrasound (ultrasound) (estimated fetal weight equal to the 90 percentile or over) [7].
Exclusion criteria were: severe somatic disorders, pregnancy complications (preeclampsia, gestational hypertension, gestational diabetes mellitus), elective cesarian section, uterine anomalies, fetal malformations, fetal disorders according to the techniques used to monitor the condition of the fetus (cardiotocography, dopplerometry).
The clinical and anamnestic data, the course of pregnancy and delivery in women under study, the condition of their babies at birth and during stay in hospital were analyzed. The clinical data on pregnant women and their newborns were obtained from the archival records of delivery histories and medical histories of the newborns. Sonographic diagnosis of the large for gestational age fetuses using ultrasound scanner was determined in all patients, and fetal weight was estimated using Hadlocks formula. 478 women with LGA fetuses according to diagnostic ultrasound сonformed to inclusion criteria.
After undergoing medical examination, these women were divided into two groups. The expectant management was in the comparison group (n=195), and induction of labor was in the main group (n=283).
Both groups were divided into three subgroups depending on gestational age: subgroup 1 included women who were 38 weeks pregnant (n=30 in the comparison group and n=27 in the main group), subgroup 2 – 39 weeks pregnant (n=78 and n= 99), subgroup 3 – 40 weeks pregnant and over (n=87 and n=157).
The comparison group included pregnant women with full-term pregnancy, and songraphically diagnosed LGA fetuses, but they were not offered labor pre-induction or induction (expectant management). In women in the main group with diagnosed LGA, indication for labor induction in full-term pregnancy was unreadiness of the birth canal.
Labor pre-induction was performed according to the clinical recommendations “Failed attempt of labor induction (cervical ripening and labor induction), 2021” [8].
In the induction group, the Bishop score for assessment of the readiness of the cervix for induction of labor was initially 1–4 points, and on average was 4 (2,3) points. The reasons for inducing labor was when the Bishop score riched 8 points and higher, and it was possible to perform amniotomy. Four hours after amniotomy, labor induction with oxytocin was performed in 10.6% of cases (30 women) in the absence of contractions. Labor induction with oxytocin was interrupted when the active phase of labor was reached.
The percentage of caesarean sections in groups under study were considered as the primary outcomes to be studied. The percentage of vaginal deliveries and perinatal outcomes were considered as the secondary outcomes to be studied.
The study was approved by the local Ethics Committee of the Academician V.I. Kulakov National Medical Research Center for Obstetrics, Gynecology and Perinatology, Ministry of Health of the Russian Federation.
Statistical analysis
Statistical analysis of the obtained results was performed using software IBM SPSS Statistics 22 for Windows. Shapiro–Wilk hypothesis test was used to check normal distribution of variables. Quantitative variables with normal distribution were described using atithmetic mean (M) and standard deviation (SD), with 95 confidence interval (95% CI). Normal distribution of quantitavie data was described using median (Me) and the lower and upper quartiles (Q1and Q3). The quantitative variables in the groups were compared using Mann–Whitney U-test in the absence of normal distribution. Fisher’s test was used to check the equality of dispersion in the groups before using statistical parametric methods. In case of equal dispertion, quantitative variables with notmal distribution were compared between the groups using Student’s t-test. The categorical data were described in absolute vlues and percentage (%). The qualitative variables were presented in absolute values and percentage (%). Pearson's chi-square (χ2) test was used for comparisons between the groups. To measure relative effect, risk ratio was used with 95% CI. The differences were considered to be statistically significant at p<0,05.
Results
Comparison between the groups showed that there were no age differences. The mean age of women in the control group was 31.4 (2.7) years versus 31.8 (5.1) in the main group, respectively (p=0.35). Also, there were no differences between the mean levels of body mass index 26.7 (4.7) kg/m2 versus 27 (5.3) kg/м2, respectively (р=0.41).
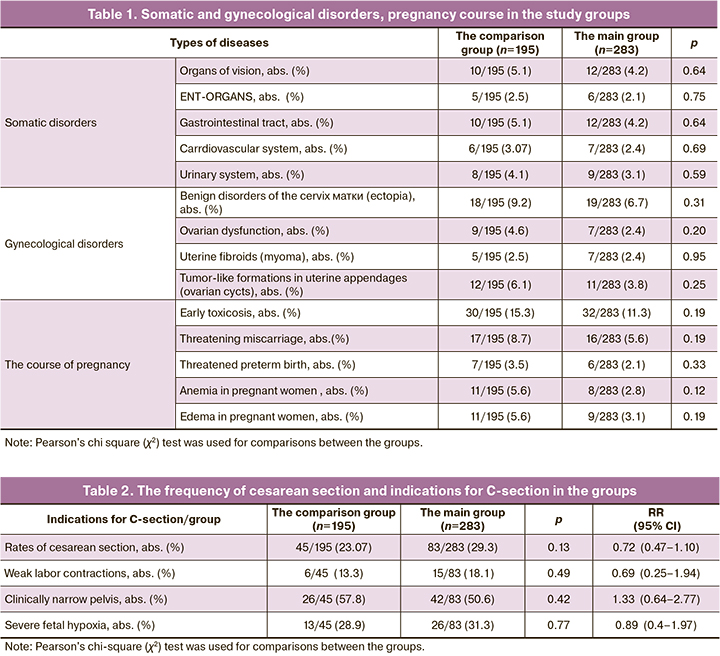
No differences between the groups were found in the frequency and the structure of somatic disorders, in the anamnestic data and the course of pregnancy. The data are presented in Table 1.
At the time of childbirth, the length of pregnancy was 279.9 (4.39) days – 39 weeks and 6 days in the comparison group versus 277.9 (4.37) days – 39 weeks and 4 days in the main group (р=0.0001).
The data obtained in the study showed that the frequency of cesarean section in the expectant management group was 45/195 (23.07%) versus 83/283 (29.3%) in the induction group. However the differences were not statistically significant. At the same time, there were no differences in the structure of indications for abdominal delivery (Table 2). Comparison in the groups showed that indication for each second cesarean section was “clinically narrow pelvis”, and “fetal hypoxia” for each third C-section, and “weak labor contractions and ineffectiveness of conservative management” was less often.
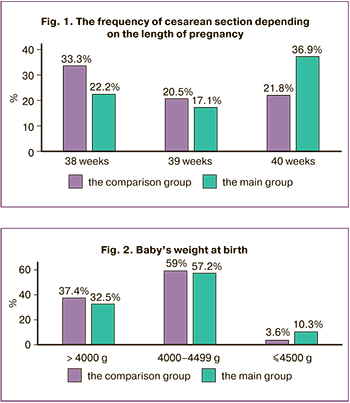
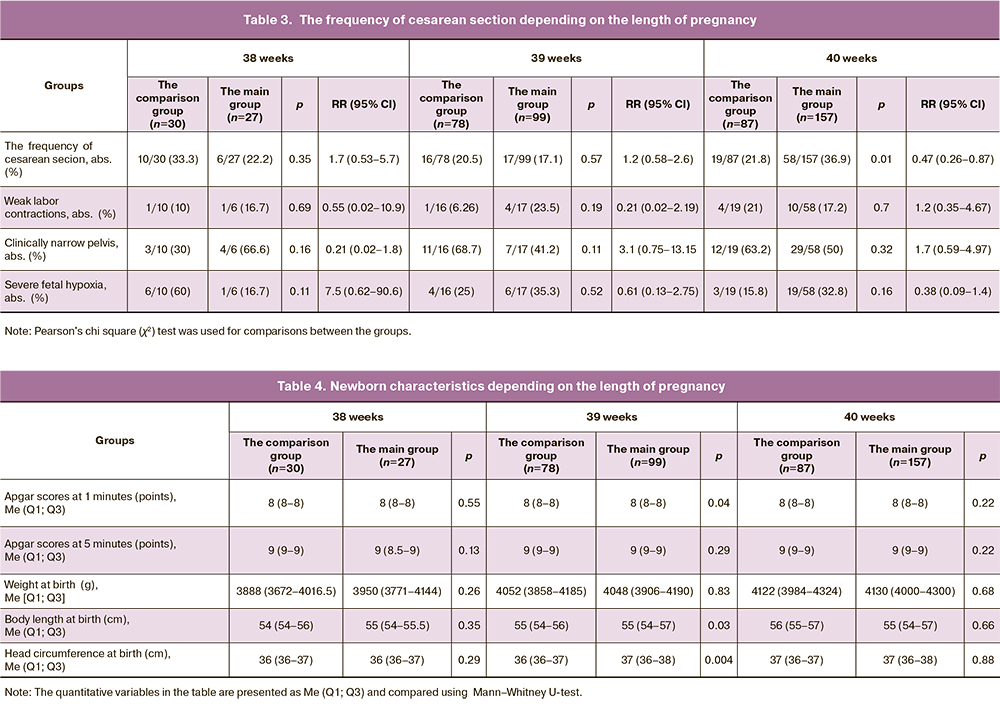
The analysis of the frequency of C-section depending of the length of pregnancy on the day of delivery showed that the percentage of C-sections at 38 and 39 weeks was higher in the groups of spontaneous onset of labor – 33.3% versus 22.2% and 20.5% versus 17.1%. However, the differences were not statistically significant (р=0.35 and 0.57, respectively) (Fig. 1). At the same time, at 40 weeks of pregnancy, the situation changed, and the frequency of cesarean section was significantly lower in the expectant management group – 21.8% versus 36.9%, p=0.02. The comparative analysis of labor and delivery complications that were indications for operative delivery are shown in Table 3.
Operative vaginal delivery due to severe fetal hypoxia was more often in the expectant management group. However, the difference between the groups was not statistically significant – 4/195 (2.05%) versus 2/283 (0.7%), respectively, р=0,21.
In all observations, pregnancies ended in live birth. There were no significant differences in Apgar scores at 1 minute – 7.91 (0.15) points in the comparison group versus 7.88 (0.21) points in the main group, р=0.79. Also, there were no differences between the groups at 5 minutes – 8.8 (0.31) points versus 8.8 (0.32) points, р=0.49.
There was no difference between the groups in the frequency of childbirth with Apgar scores less than or equal to 7 points at 1 minute – 15/195 (7.69%) in the comparison group versus 20/283 (7.06%) in the main group, р=0.79 and at 5 minutes – 5/195 (2.56%) versus 4/283 (1.41%), р=0.36.
Anthropometric assessment in newborns showed that there were no differences between the groups. The data are shown in Fig.2. The average weight at birth was 4048.4 (214.9) g in the comparison group versus 4100.2 (229.7) in the main group, respectively, p=0.13. Baby’s weight less than 4000 g was in 73/195 (37.4%) cases in the comparison group versus 92/283 (32.5%) in the main group, р=0.26. Baby’s weight between 4000–4499 g was in 115/195 (59%) cases versus 162/283 (57.2%), р=0,7, and baby’s weight greater than or equal to 4500 g was in 7/195 (3,6%) cases versus 29/283 (10.3%), respectively, р=0.009.
The average baby’s body length at birth in the group of expectant management was 55.09 (1.3) cm versus 55.43 (1.5) cm in the induction group, р=0,07. The average newborn head circumference was 36.5 (0.77) cm versus 36.8 (0.82) cm, respectively, р=0.01. This result was possible due to higher number of newborns with birth weight greater than or equal to 4500 g in the induction group.
The characteristics of newborn babies in the groups depending on the length of pregnancy are shown in table 4.
Analysis of neonatal outcomes in the groups at 38 and 40 weeks gestation showed no differences between the average Apgar scores at 1 and 5 minutes, and anthropometric data. However, the number of infants born at 39 weeks and having Apgars scores less or equal to 7 (10/78 (12.8%) versus 4/99 (4.04%), р=0.04) was significantly higher in the expectant management group. Interestingly, that despite the absence of differences in the average fetal weight, longer body length and larger head circumference was in newborns in the induction group (р=0.03 and р=0.004, respectively).
Discussion
Currently, induction of labor for fetal macrosomia is a matter of debate. Previously conducted observational and retrospective studies found no evidence of reduced frequency of cesarean section in women with labor induction versus expectant management strategy [9, 10]. However, these studies had a number of limitations, such as small sample size, accurate prediction of macrosomia [11, 12].
In this study, we investigated the frequency of operative delivery in pregnant women with large-for gestational-age fetuses depending on management strategy and pregnancy length.
The recent analysis of 4 randomized control trials that included 1190 women without disorders of carbohydrate metabolism and with suspected fetal macrosomiam, who had spontaneous and induced labor, showed that there were no differences in the frequency of cesarean section – 26.6% versus 29.4%; RR 0.91 (95% CI 0.76–1.09), operative vaginal delivery – 13% versus 15.2%; RR 0.86 (95% CI 0.65–1.13), shoulder dystocia – 2.4% versus 4.2%; RR 0.57 (95% CI 0.30–1.08) [13]. Randomized trial by Boulvain M. et al. showed that labor induction for LGA fetuses between 37 weeks and 38 weeks +6 days did not significantly reduce the frequency of cesarian section compared to expectant management strategy (28% versus 32%; RR 0.89 (0.72–1.09), but significantly reduced macrosomia and related complications [14].
The data obtained by us showed that there were no differences in the frequency of cesarean section in women with LGA fetuses at 38–41 weeks with spontaneous onset of labor and induced labor. At the same time, the analysis considering the certain length of pregnancy showed, that the trend of cesarean section was higher at 38 and 39 weeks with expectant management at 38 and 39 weeks. In contrast, at 40 weeks, abor induction was associated with increased rate of operative delivery (21.8% in expectant management versus 36.9% in labor induction, р=0.02).
The analysis of perinatal outcomes showed that newborn’s body weight 4500 g was 3 times more often in the group of labor induction (3.6% versus 10.3%, respectively, p=0.009). Moreover, the average head circumference at birth was significantly larger (p=0.01). Therefore, despite no difference in the average body weight, the prognosis for outcome was less favourable in the induction group due to a higher frequency of babies with large body weight and length at birth. This could be a factor that influenced the frequency of operative delivery.
At 39 weeks, assessment of newborns showed that Apgar score less than or equal to 7 ponts at 1 minute was 3 times more often in the expectant management group (12.8% versus 4.04%, p=0.04). In the absence of significant differences in the frequency of caesarean section, it is evidenced in favor of labor induction.
The data obtained by us, did not fully conform with the results of randomized trial by Boulvain M. et al. (2015), that showed decreased frequency of macrosomia in the group of labor induction. In our study, the average birth weight at 39 and 40 weeks did not exceed 4000 g in all groups. At 38 weeks, the median body weight was about 3900 g. Nevertheless, even in this group, there were newborns weighing over 4000 g. Thus, despite the objective to study the frequency of cesarean section in women with LGA fetuses, the obtained results showed the frequency of cesarean section when macrosomia was already formed. In 2018, Nicolaides et al. published estimated birth weight charts according to ultrasound data [15]. The results of their study showed that firstly, the weight at birth was larger that estimated birth weight according to US. The 90th percentile birthweigh of a newborn at 38 weeks is 3754 g, at 39 weeks – 3944 g, at 40 weeks – 4103 g. Thus, at 39–40 weeks, the 90the percentile of sonographic estimated fetal weight predicts neonatal weight of 4000 g and larger. Due to this fact, labor induction at these terms as a method for prevention of macrosomia and associated complication is meaningless and ineffective. It seems that the optimal term for delivery of babies having the 90th percentile according to sonographic estimated weight, is 39 weeks. At the 95th percentile, the term for delivery can be 38 weeks, at the 97th percentile – 37–38 weeks. However, with less gestation, labor induction is less effective due to “immaturity” of mechanisms to trigger the onset of labor.
Conclusion
Thus, the issue of reducing the frequency of operative delivery and prevention of complications of fetal macrosomia requests further study. Prevention of macrosomia during pregnancy and timely diagnosis before full-term pregnancy is important. Labor induction can be a promising method, when in addition to estimated fetal weight, the length of pregnancy will be taken into account, and the readiness of woman’ body for childbirth will be achieved. Apparently, the optimal term for delivery of babies with sonographic estimated birth weight at the 90th percentile, is 39 weeks, at the 95th percentile – 38 weeks and at the 97th percentile – 37–38 weeks.
References
1. Rezaiee M., Aghaei M., Mohammadbeigi A., Farhadifar F., Zadeh Ns., Mohammadsalehi N. Fetal macrosomia: risk factors, maternal, and perinatal outcome. Ann. Med. Health Sci. Res. 2013; 3(4): 546‑50. https://dx.doi.org/10.4103/2141‑9248.122098.
2. Одинокова В.А., Шмаков Р.Г. Исходы родов у первородящих с фетальной макросомией при активной и выжидательной тактике. Акушерство и гинекология. 2022; 1: 72‑9. [Odinokova V.A., Shmakov R.G. Birth outcomes in primiparous women diagnosed with fetal macrosomia and managed with active surveillance and watch‑and‑wait approach. Obstetrics and Gynecology. 2022; (1): 72‑9. (in Russian)]. https://dx.doi.org/10.18565/ aig.2022.1.72‑79.
3. Ghosh R.E., Berild J.D., Sterrantino A.F., Toledano M.B., Hansell A.L. Birth weight trends in England and Wales (1986‑2012): babies are getting heavier. Arch. Dis. Child. Fetal Neonatal Ed. 2018; 103(3): F264‑F270. https://dx.doi.org/10.1136/archdischild‑2016‑311790.
4. Macrosomia: ACOG Practice Bulletin Summary, Number 216. Obstet. Gynecol. 2020; 135(1): 246‑8. https://dx.doi.org/10.1097/AOG.0000000000003607.
5. Ye J., Zhang L., Chen Y., Fang F., Luo Z., Zhang J. Searching for the definition of macrosomia through an outcome‑based approach. PLoS One. 2014; 9(6): e100192. https://dx.doi.org/10.1371/journal.pone.0100192.
6. Akanmode A.M., Mahdy H. Macrosomia. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan. 2022 Sep. 6.
7. The American College of Obstetricians and Gynecologists. Women’s health care physicians. Obstet. Gynecol. 2016; 128(5). https://dx.doi.org/10.1097/ AOG.0000000000001767.
8. Российское общество акушеров‑гинекологов (РОАГ). Клинические рекомендации «Неудачная попытка стимуляции родов (подготовка шейки матки к родам и родовозбуждение)». 2021. [Russian Society of Obstetricians and Gynecologists (RSOG). Clinical guidelines "Unsuccessful attempted induction of labor (cervical preparation and labor induction)". 2021. (in Russian)]. Available at: https://roag‑portal.ru/recommendations_obstetrics
9. Combs C.A., Singh N.B., Khoury J.C. Elective induction versus spontaneous labor after sonographic diagnosis of fetal macrosomia. Obstet. Gynecol. 1993; 81(4): 492‑6.
10. Leaphart W.L., Meyer M.C., Capeless E.L. Labor induction with a prenatal diagnosis of fetal macrosomia. J. Matern. Fetal Med. 1997; 6(2): 99‑102. https://dx.doi.org/10.1002/(SICI)1520‑6661(199703/04)6:2<99::AID‑ MFM7>3.0.CO;2‑K.
11. Henriksen T. The macrosomic fetus: a challenge in current obstetrics. Acta Obstet. Gynecol. Scand. 2008; 87(2): 134‑45. https://dx.doi.org/10.1080/00016340801899289.
12. Zhang X., Decker A., Platt R.W., Kramer M.S. How big is too big? The perinatal consequences of fetal macrosomia. Am. J. Obstet. Gynecol. 2008; 198(5): 517. e1‑6. https://dx.doi.org/10.1016/j.ajog.2007.12.005.
13. Boulvain M., Irion O., Thornton J.G. Induction of labour at or near term for suspected fetal macrosomia. Cochrane Database Syst. Rev. 2016; 2016(5): CD000938. https://dx.doi.org/10.1002/ 14651858.CD000938.pub2.
14. Boulvain M., Senat M.-V., Perrotin F., Winer N., Beucher G., Subtil D. et al. Induction of labour versus expectant management for large‑for‑date fetuses: a randomised controlled trial. Lancet. 2015; 385(9987): 2600‑5. https://dx.doi.org/10.1016/S0140‑6736(14)61904‑8.
15. Nicolaides K.H., Wright D., Syngelaki A., Wright A., Akolekar R. Fetal medicine foundation fetal and neonatal population weight charts. Ultrasound Obstet. Gynecol. 2018; 52(1): 44‑51. https://dx.doi.org/10.1002/ uog.19073.
Received 07.02.2023
Accepted 04.04.2023
About the Authors
Oleg V. Tysyachnyi, Ph.D, Junior Researcher at the 1st Maternity Department, Academician V.I. Kulakov National Medical Research Center for Obstetrics, Gynecology and Perinatology, Ministry of Health of Russia, o_tysyachny@oparina4.ru, https://orcid.org/0000-0001-9282-9817, 117997, Russia, Moscow, Oparina str., 4.Oleg R. Baev, Dr. Med. Sci., Professor, Head of the 1st Maternity Department, Academician V.I. Kulakov National Medical Research Center for Obstetrics, Gynecology and Perinatology, Ministry of Health of Russia; Professor at the Department of Obstetrics, Gynecology, Perinatology and Reproductology, I.M. Sechenov First MSMU, Ministry of Health of Russia (Sechenov University), +7(495)438-11-88, o_baev@oparina4.ru, https://orcid.org/0000-0001-8572-1971, 117997, Russia, Moscow, Ac. Oparina str., 4.
Andrey M. Prikhodko, Dr. Med. Sci, doctor at the 1st Maternity Department, Academician V.I. Kulakov National Medical Research Center for Obstetrics, Gynecology and Perinatology, Ministry of Health of Russia, +7(495)438-11-88, a_prikhodko@oparina4.ru, https://orcid.org/0000-0002-66-15-2360, 117997, Russia, Moscow, Oparina str., 4. Maria A. Kepsha, clinical intern, Academician V.I. Kulakov National Medical Research Center for Obstetrics, Gynecology and Perinatology, Ministry of Health of Russia, +7(495)438-11-88, a_prikhodko@oparina4.ru, 117997, Russia, Moscow, Oparina str., 4.