Birth outcomes in primiparous women diagnosed with fetal macrosomia and managed with active surveillance and watch-and-wait approach
Aim: To compare specific features of delivery in primiparous women diagnosed with fetal macrosomia and managed with the watch-and-wait approach. Materials and methods: The study included 328 primiparous women, who had no carbohydrate metabolism disorders in pregnancy and delivered infants with birth weight 4000—4999 g at 390— 416 weeks of gestation: the active surveillance (pre-induction of labor) was applied to 38 patients at 390-6 weeks of pregnancy; and the watch- and-wait approach (spontaneous delivery and medical indications for induced labor)was applied to 290 patients at 400-6 and 410-6 weeks of pregnancy. Results: The rate of cesarean section was significantly high, when active surveillance was used at 390-6 weeks of pregnancy versus the watch-and-wait approach at 400-6 weeks of pregnancy (55.3% versus 26.8%, p=0.001). Moreover, in the group of women with pre-induction of labor at 390-6 weeks of pregnancy, premature rupture of membranes and low amniotic fluid for a long time (for more than 12 hours) increased the risk of infectious complications, andprophilactic antimicrobial therapy was used to prevent them (p<0,05). The watch-and-wait approach after 41 weeks of pregnancy contributed to increased incidence of chronic fetal hypoxia (p<0.05). Conclusion: The watch-and wait approach used in primiparous women, who had no carbohydrate metabolism disorders and diagnosed with fetal macrosomia before 400-6 weeks of pregnancy allows to decrease the rate of cesarean section and does not increase the incidence of adverse maternal outcomes (perineal trauma, hypotonic bleeding, endometritis) and perinatal outcomes (clavicle fracture, cephalohematoma, neonatal jaundice).Odinokova V.A., Shmakov R.G.
Keywords
Currently, there is no generally accepted term for “fetal macrosomia”, due to this, the babies weighing more than 4000 g at birth [1] are considered large regardless of their gestational age. The term "large for gestational age" (LGA) is used in the practice of neonatologists and pediatricians for the babies with birthweights greater than the 90th percentile for their gestational age [2]. It is important to study this issue due to increased incidence of LGA newborns by 5–20%, and this is one of the reasons for the increased cesarean section rates, vacuum extraction of the fetus, birth traumas for the mother and newborn [3–6].
The existing range of recommendations for management of patients with fetal macrosomia include expectant management, elective labor induction and elective cesarean section in term pregnancies. Nowadays, the issue of the term of pregnancy for labor and management options for these patients remains open.
Elective cesarean section made it possible to avoid complications in vaginal delivery among women with LGA babies. However, in the world practice this option is used in cases when the estimated fetal weight is more than 4500 g in women with diabetes or more than 5000 g in women without diabetes [7]. The complexity of this problem is due to the high error rate in the diagnosis of fetal macrosomia in the antenatal period that does not allow to consider this condition to be an absolute indication for elective caesarean section among this group of patients. For these reasons, the doctors have a dilemma expectant, either to use the active management (pre-induction/induction of labor) or expectant management (waiting for spontaneous labor and/or labor induction for medical reasons).
Proponents of active management argue that readiness of cervix for labor before the suggested date of delivery in term pregnancy can serve as an alternative to weight loss at birth, and as a result, decrease the risk of cesarean section due to clinically narrow pelvis, as well as perineal injuries, shoulder dystocia, and birth trauma of the newborn [8, 9]. Nevertheless, there are controversial data on the rates of cesarean section and labor complications, when active management is used. Some authors showed in their studies that pre-induction/induction of labor in patients with fetal macrosomia increased the risk of caesarean section and did not reduce the incidence of shoulder dystocia [10–12], the others reported on reduction of the risk [8] and no influence on the rate of abdominal surgical delivery [13].
When making a decision whether pre-induction or induction of labor should be carried out, the optimal gestational age is of great importance. Pre-induction/induction of labor before 39 weeks of pregnancy has been shown to cause fetal respiratory distress syndrome [14]. Due to this, it is not recommended to carry out pre-induction /induction of labor before 390-6 weeks of pregnancy in cases when the fetus is estimated to be “large for gestational age” in the absence of other medical indications [15].
Proponents of expectant management are not categorically against active tactics, but they believe that pregnant women without diabetes mellitus and with large fetuses should wait for spontaneous delivery, at least up to 40 weeks of pregnancy [1]. Moreover, according to the recommendations of the world societies of obstetricians and gynecologists (the Royal College of Obstetricians and Gynecologists, the National Institute of Health and Care Excellence, the Society of Obstetricians and Gynecologists of Canada, the World Health Organization), the patients without impairement of carbohydrate metabolism and with suspected fetal macrosomia should not undergo pre-induction/induction of labor before 41 weeks of pregnancy [16–19].
The aim of this study was to compare characteristics of labor in primiparous women with fetal macrosomia, who underwent active and expectant management of labor.
Materials and methods
The retrospective cohort study included 328 primiparous women, who gave birth to infants with birthweights above 4000 g in the National Medical Research Center for Obstetrics, Gynecology and Perinatology named after Academician V.I. Kulakov in the period from 2016 to 2019.
Inclusion criteria were the women aged 18–45 years, cephalic presentation of the fetus, the first birth, 390–416 weeks of gestation, babies with birthweights above 4000 g, spontaneous labor or pre-induction/induction of labor in patients, who have signed informed written consent form.
Exclusion criteria were scars on the uterus after cesarean section and myomectomy, contraindications for vaginal delivery and the use of medications for pre-induction of labor, premature rupture of membranes prior to pre-induction of labor, any type of diabetes mellitus, somatic diseases at the stage of decompensation, Rh-sensitization, fetal malformation.
Clinical and anamnestic characteristics, anamnestic features of the course of pregnancy and delivery in women included in the study, the condition of newborns after birth and during the stay in hospital were analyzed. Clinical data on the course of pregnancies and condition of newborns were obtained from the archival records of birth histories and anamnestic features of newborns.
The examined pregnant women were divided into 2 groups. The first group included 38 patients at 390-6 weeks of pregnancy, and the active management was used. They underwent preparation of the cervix due to suspected fetal macrosomia and unripe cervix (cervical status assessment showed <8 points). Group 2 (expectant management group) included 290 patients at 400–416 weeks of pregnancy. These women had spontaneous onset of labor, or pre-induction of labor was carried out in women with diagnosed fetal macrosomia or in those, who are more likely to have prolonged pregnancy (410-6 weeks), when the cervix was not ready for labor. The patients who underwent expectant management were divided into 2 subgroups depending on the term of pregnancy at the time of regular contractions or the start of pre-induction of labor. The subgroup 1 included 239 patients at 400-6 weeks of pregnancy. The subgroup 2 included 51 patients at 410-6 weeks of pregnancy.
Ultrasound scans were performed for diagnosis of fetal macrosomia, and Hadlock's formula was used to estimate fetal weight in all patients before elective pre-induction of labor.
Modified Bishop score was used to assess the cervix in all patients [20]. In all cases, when pre-induction of labor was carried out, assessment of the cervix showed that the cervix was not ready for labor, i.e. the cervix was unripe and cervical ripening was insufficient. For the unripe cervix (≤ 5 points according to the Bishop scoring system), usually mifepristone was used as a primary drug for cervical ripening. In some cases, non-drug methods were initially used to prepare the cervix for labor, such as cervical dilators (cervical catheters or hygroscopic dilators), or they were used in combination with mifepristone. When the cervical ripening was insufficient (the Bishop score of 6–7 points), pre-induction of labor was carried out using prostaglandin-containing gel. In the absence of regular contractions with ripe cervix after pre-induction (the Bishop score of ≥8 points), labor induction (amniotomy and/or administration of oxytocin by intravenous infusion) was performed.
Statistical analysis
Microsoft Exel spreadsheet software program and software package SPSS Statistics 21.0 for Windows (USA) were used for statistical data processing. The Kolmogorov–Smirnov test was used to check the compliance of quantitative data with the normal distribution. The quantitative data were presented as mean values and standard deviation M (SD) for the parameters of normal distribution, and as median and interquartile range (Q1;Q3) when distribution differed from normal. The Student's paired t-test was used to compare quantitative data in different groups for a normal distribution, and the Mann–Whitney test was used to compare the differences between the quantitative data, when they were not normally distributed. Qualitative data were presented as absolute values and absolute frequency was determined as abs. (%). Comparison of categorical data and assessment of reliability of intergroup differences was carried out using the Chi-square (χ2) test with Yates' correction and Fisher's exact test using contingency tables. The p-value threshold for statistical significance was 0.05. The Bonferroni correction was used for multiple comparisons, and the p-value threshold for statistical significance was 0.017.
Results
590 birth histories in the period from 2016 to 2019 were analyzed. After selection of patients according to inclusion and exclusion criteria, the remaining 328 women and their newborns participated in the study.
Comparison of the studied groups showed no statistically significant differences in the mean values of age, including the patients aged over 35 years, body mass index, as well as the frequency of clinical narrow pelvis (Table 1). Specific features of pregnancy course in the studied groups are presented in Table 1. It is shown, that the incidence rates of somatic diseases and pregnancy complications that could influence the term of pregnancy for labor were comparable between the groups. Among pregnancy complications, premature rupture of membranes and low amniotic fluid for a long time (for more than 12 hours) occurred statistically most often at 390-6 weeks of pregnancy when active management was used versus expectant management at 400-6 weeks of pregnancy (21/38 (55.3%) versus 34/239 (142%)) and at 410-6 weeks of pregnancy (21/38 (55.3%) versus 4/51 (7.8%)). After 41 weeks of pregnancy the women were most often diagnosed with oligohydramnios and increased incidence of chronic fetal hypoxia that was defined by meconium stained amniotic fluid.
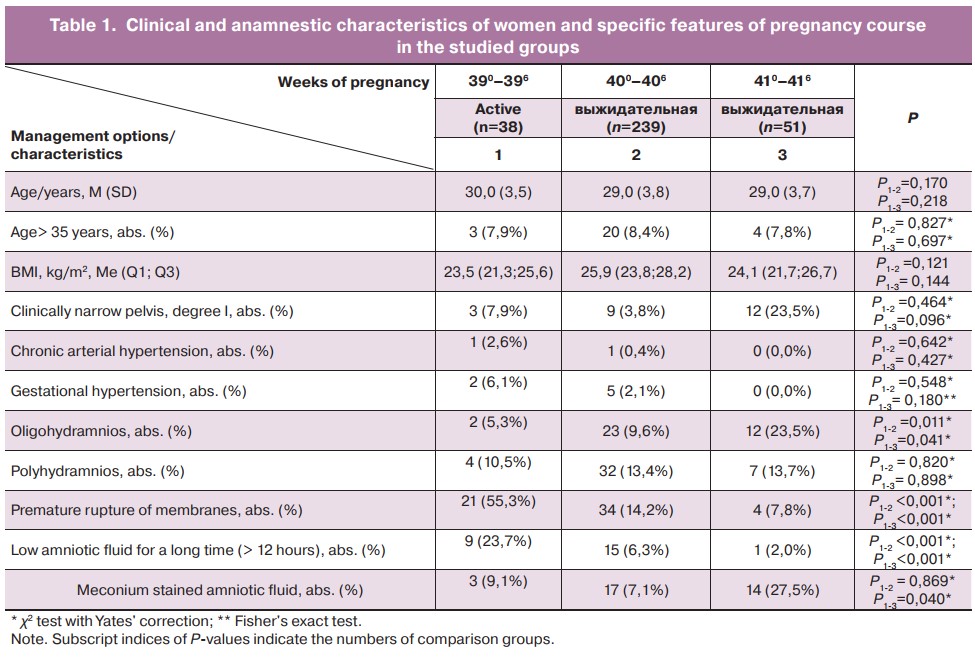
Pre-induction of labor was carried out in women using active and expectant management, when the cervix was not ready for labor (Table 2). 30/38 (78.9%) patients in group 1 had unripe cervix at 390-6 weeks of pregnancy, 41/50 (82.0%) patients in group 2 (subgroup 1) at 400-6 weeks, and 22/27 (81.5%) patients in group 2 (subgroup 2) at 410-6 weeks of pregnancy; 8/38 (21.1%) patients had insufficient cervical ripening at 390-6 weeks of pregnancy, 9/50 (18.0%) patients at 400-6 weeks, and 5/27 (18.5%) patients at 410-6 weeks. Statistically significant differences between the groups were not found.
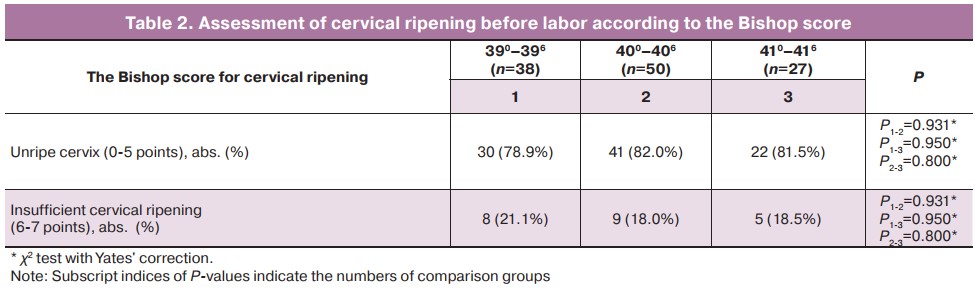
In pre-induction/induction of labor, regular contractions began at 390-6 weeks of pregnancy in 33/38 (86.8%) patients, at 400-6 weeks in 43/50 (86.0%) patients and at 410-6 weeks in 24/27 (88.9%) patients. We noted that, the time period from pre-induction of labor to delivery of babies in women with unripe cervix was 2–3 days (Me – 2 days, Q1–Q3: 0.9–3.0), and with insufficient ripening of the cervix – 1–2 days (Me – 1 day, Q1–Q3: 0.5–2.0).
Table 3 presents specific features of pregnancy course in women in the studied groups. The average length of pregnancy at the time of pre-induction of labor was 39.3 (0.4) weeks in group 1, 40.3 (0.1) weeks in group 2 (subgroup 1), and 41.0 (0.3) weeks in group 2 (subgroup 2).
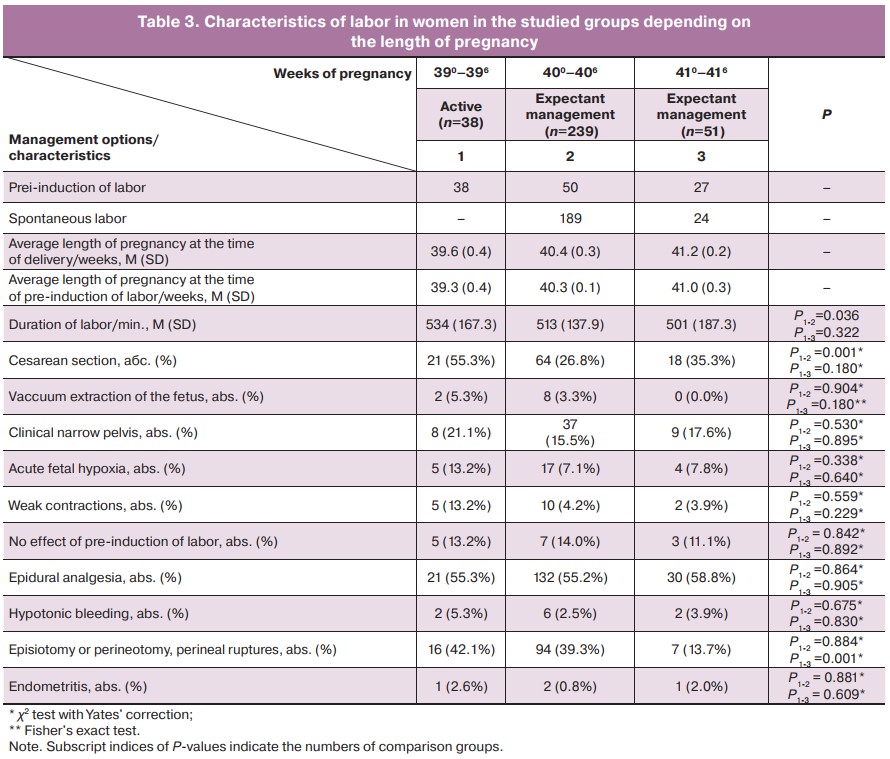
The comparative analysis of delivery methods in primiparous women showed the increased rates of cesarean delivery with active management of labor at 390-6 weeks versus expectant management at 400-6 weeks of pregnancy (21/38 (55.3%) versus 64/239 (26.8%). At the same time, the incidence of complications during labor (clinically narrow pelvis, acute fetal hypoxia, weak contractions), that were the indications for caesarean delivery, had no significant differences between the groups. Nevertheless, it should be noted that clinical narrow pelvis was the most common complication of delivery at any term of pregnancy.
The frequency of surgical vacuum-assisted vaginal delivery was comparable between the groups at all terms of pregnancy in the study. Weak uterine contractions and acute fetal hypoxia were the main indications for vaccum extraction of the fetus.
It is notable that active management resulted in significant increase in perineal ruptures and in performance of episiotomy or perineotomy at 390-6 weeks of pregnancy versus expectant management at 410-6 weeks – 16/38 (42.1%) versus 7/51 (3.7%).
The incidence of hypotonic bleeding and postpartum endometritis had no statistically significant difference between the groups.
Table 4 presents the condition of newborns in the studied groups. All infants were born alive. The Apgar scores at 1 and 5 minutes after birth, birth weights and body lengths had no significant differences between the groups. Median weights of babies at birth had no significant differences in the groups – 4180 g at 390-6 weeks, 4110 g at 400-6 weeks, and 4145 g at 410-6 weeks’ gestation. In some cases, the birth weights of newborns were over 4500 g at all studied lengths of gestation.
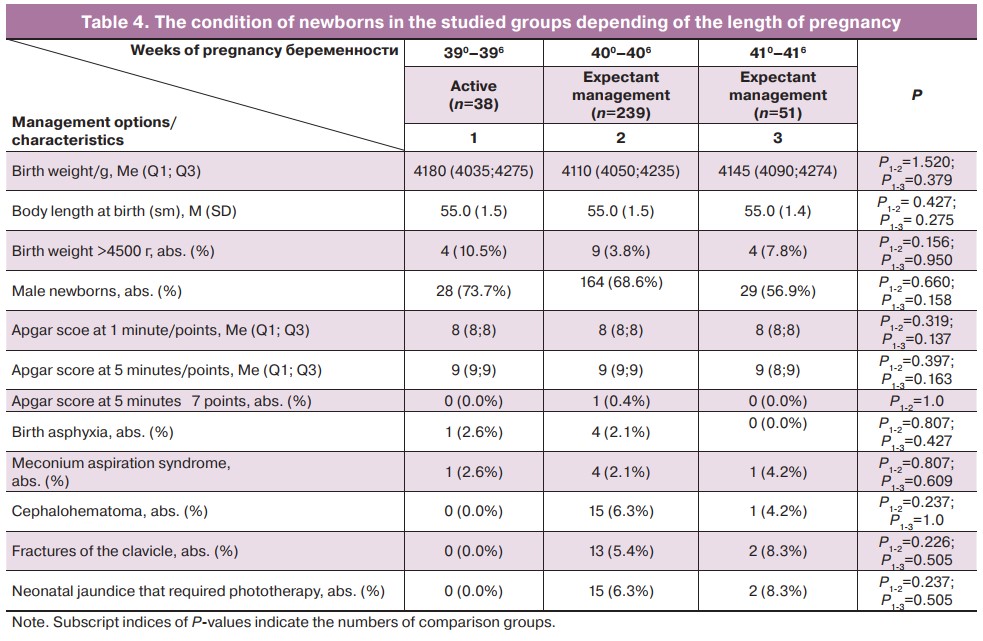
The incidence of fractures of the clavicle, cephalohematoma, neonatal jaundice that required phototherapy for newborns had not statistically significant differences between the groups at all studied lengths of gestation.
It should be noted that labor complications, such as shoulder dystocia and brachial plexus injury did not occur in newborns in our study.
Discussion
In this study we compared maternal and neonatal outcomes in primiparous women with fetal macrosomia, who had no impairment of carbohydrate metabolism in pregnancy and underwent active and expectant management at 390–416 weeks of pregnancy. The obtained results were as follows: 1) Active management at 390-6 weeks of pregnancy significantly increased the frequency of cesarean section, premature rupture of membranes and low amniotic fluid for a long time (˃12 hours), that required antibiotic prophylaxis; 2) expectant management after 400-6 weeks of pregnancy reduced significantly and at 410-6 weeks decreased the rates of cesarean section and did not increase the rates of adverse maternal and perinatal complications; 3) expectant management before 410-6 weeks of pregnancy increased the incidence of chronic fetal hyhpoxia and had no effect on newborns’ condition (low Apgar score, incidence of meconium aspiration syndrome and birth asphyxia).
Pre-induction of labor (active management) is an unavoidable measure for obstetrician-gynecologist due to the fact that prolongation of pregnancy and waiting for spontaneous labor is a high risk both for the mother and fetus. According to contemporary clinical practice guidelines of foreign authors, suspected fetal macrosomia is not an indication for pre-induction of labor in women without diabetes before 40–41 weeks of pregnancy [1, 16–19]. Meanwhile, the attempts are being undertaken to study labor outcomes in women with fetal macrosomia, who underwent earlier pre-induction/induction of labor in term pregnancy. It should be noted that the results of studies regarding the outcomes of labor and the suggested term for pre-induction of labor are controversial [8, 9, 13, 21–24]. It seems, that one of the reasons for these controversies is different design of studies and patients sampling. Thus, many researchers include in the expectant management group only those patients, who have spontaneous labor contractions. However, the notion “expectant management" implies waiting for spontaneous labor contractions before the indicated term of pregnancy with subsequent pre-induction of labor in the absence of the expected result or occurrence of other medical indications. Due to this, we included in expectant management group the patients, who had both spontaneous labor contractions and those, who underwent pre-induction of labor in cases of diagnosed fetal macrosomia or prolonged pregnancy.
The sampling of patients may also have effect on the results of studies. In most cases, the authors analyze the outcomes and labor complications in women, who gave birth to LGA newborns. Moreover their weights at birth are less than 4000 g. The question arises, as to whether it is clinically appropriate to carry out pre-induction of labor at earlier terms, if the fetus is not large. It has been proven, that the risk of maternal and perinatal complications depends on the absolute weight of the fetus at birth, and based on this, the grading system for fetal macrosomia has been suggested [25]. Accordingly, our comparative analysis of labor outcomes using active and expectant management was based on assessment of large infants (weighing >4000g), but not “large for gestagional age” at birth (above the 90th percentile).
Therefore, the aim of our study was comparison of the course of labor in primiparous women with fetal macrosomia (4000–4999 g) using active management at 390 weeks of pregnancy, and expectant management at 400-6 and 410-6 weeks of pregnancy. The obtained data showed that the rate of cesarean section was higher after pre-induction of labor at 390-6 weeks of pregnancy versus expectant management at 400-6 weeks (p=0.002). The main indications for emergency C-section were: clinically narrow pelvis, acute fetal hypoxia, weak contractions and no effect of cervical ripening. The rates of cesarean section were comparable between the groups. It should be noted that with active management, premature rupture of membranes and low amniotic fluid for a long time (for more than 12 hours) occurred most often at 390-6 weeks of pregnancy. Due to this, prophilactic antibiotic treatment was used (p<0.001).
We did not find association between pre-induction of labor and surgical vacuum-assisted vaginal delivery. Similar results were obtained by Magro-Malosso E.R. et al. (2017) in the large randomized study [22].
According to a number of authors, one of the advantages of pre-induction of labor in women with fetal macrosomia is reduction of neonatal morbidity. The results of randomized study by Boulvain M. et al. (2015) showed reduction of birth traumas (shoulder dystocia, clavicle fracture, brachial plexus injury and perinatal mortality) in infants born to mothers after pre-induction/induction of labor (OR =0.34; 95% CI: 0,16–0.71) [26]. At the same time, other researchers did not demonstrate the differences between the rates of shoulder dystocia using active and expectant management of labor [8, 9, 12, 21–23]. Сheng Y.W. et. al. (2012) reported similar results. They did not reveal significant differences between the rates of birth traumas in newborns with birth weights more than 4000 g [8]. Perhaps, the absence of life-threatening complications, such as shoulder dystocia and brachial plexus paralysis in newborns can be explained by the fact, that patients with impaired carbohydrate metabolism were excluded from the study, since large infants born to mothers with and without diabetes have different risks for birth traumas [27].
Thus, the data obtained by us correlate with the results reported by a number of other researchers. According to them, expectant management of labor and timely diagnosis of intrapartum complications is an optimal option for fetal macrosomia [28], and pre-induction of labor in women, who are more likely to have prolonged pregnancy, does not contribute to high rates of cesarean section and adverse perinatal outcomes [29].
Conclusion
Expectant tactics in primiparous women with fetal macrosomia before 40 weeks of pregnancy who have no impaired carbohydrate metabolism reduces the rates of C-section and does not contribute the incidence rates of adverse maternal (perineal trauma, hypotonic bleeding, endometritis) and perinatal outcomes (clavicle fracture, cephalohematoma, neonatal jaundice). The optimal term for pre-induction of labor in primiparous women with fetal macrosomia should be 400-6 weeks of pregnancy adjusted for cervical ripening.
References
- Macrosomia: ACOG Practice Bulletin, Number 216. Obstet. Gynecol. 2020; 135(1): e18-e35. https://dx.doi.org/10.1097/AOG.0000000000003606.
- Ye J., Torloni M.R., Ota , Jayaratne K., Pileggi-Castro C., Ortiz-Panozo E. et al. Searching for the definition of macrosomia through an outcome-based approach in low- and middle-income countries: a secondary analysis of the WHO Global Survey in Africa, Asia and Latin America. BMC Pregnancy Childbirth. 2015; 15: 324. https://dx.doi.org/10.1186/s12884-015-0765-z.
- Cherepnina A.L., Panina O.B., Oleshkovich L.N. Management of pregnancy and labor with large fetus. Issues of gynecology, obstetrics and perinatology. 2005; 1: 15-9. (in Russian).
- Luhete P.K., Mukuku O., Kiopin P.M., Tambwe A.M., Kayamba P.K. Fetal macrosomia in Lubumbashi: risk factors and maternal and perinatal prognosis. Pan. Afr. Med. J. 2016; 23: 166. https://dx.doi.org/10.11604/pamj.2016.23.166.7362.
- García-De la Torre J.I., Rodríguez-Valdez A., Delgado-Rosas A. Risk factors for fetal macrosomia in patients without gestational diabetes mellitus. Ginecol. Obstet. Mex. 2016; 84(3): 164-71.
- Wassimi S., Wilkins R., Mchugh N.G., Xiao L., Simonet F., Luo Z.C. Association of macrosomia with perinatal and postneonatal mortality among First Nations people in Quebec. CMAJ. 2011; 183(3): 322-6. https://dx.doi.org/10.1503/cmaj.100837.
- Sokol R.J., Blackwell S.C.; American College of Obstetricians and Gynecologists. Committee on Practice Bulletins-Gynecology. ACOG practice bulletin: Shoulder dystocia. Number 40, November 2002. (Replaces practice pattern number, October 1997). Int. J. Gynaecol. Obstet. 2003; 80(1): 87-92. https://dx.doi.org/10.1016/s0020-7292(02)90001-9.
-
Cheng Y.W., Sparks T.N., Laros R.K. Jr, Nicholson J.M., Caughey B. Impending macrosomia: will induction of labour modify the risk of caesarean delivery? BJOG. 2012(4); 119: 402-9. https://dx.doi.org/10.1111/
j.1471-0528.2011.03248.x.
- Sanchez-Ramos L., Bernstein S., Kaunitz A.M. Expectant management versus labor induction for suspected fetal macrosomia: a systematic review. Obstet. Gynecol. 2002; 100(5, Pt. 1): 997-1002.
- Combs C.A., Singh N.B., Khoury J.C. Elective induction versus spontaneous labor after sonographic diagnosis of fetal macrosomia. Obstet. Gynecol. 1993; 81(4): 492-6.
- Friesen C.D., Miller A.M., Rayburn W.F. Influence of spontaneous or induced labor on delivering the macrosomic fetus. Am. J. Perinatol. 1995; 12(1): 63-6. https://dx.doi.org/10.1055/s-2007-994404.
-
Leaphart W.L., Meyer M.C., Capeless E.L. Labor induction with a prenatal diagnosis of fetal macrosomia. J. Matern. Fetal. Med. 1997; 6(2): 99-102. https://dx.doi.org/10.1002/(SICI)1520-6661(199703/04)6:2<99::
AID-MFM7>3.0.CO;2-K.
- Vendittelli F., Riviere O., Neveu B., Lemery D.; Audipog Sentinel Network. Does induction of labor for constitutionally large-for-gestational-age fetuses identified in utero reduce maternal morbidity? BMC Pregnancy Childbirth. 2014; 14: 156. https://dx.doi.org/10.1186/1471-2393-14-156.
- Boulvain M., Marcoux S., Bureau M., Fortier M., Fraser W. Risks of induction of labour in uncomplicated term pregnancies. Paediatr. Perinat. Epidemiol. 2001; 15(2): 131-8. https://dx.doi.org/10.1046/j.1365-3016.2001.00337.x.
- Caughey A.B. Should pregnancies be induced for impending macrosomia? Lancet. 2015; 385(9987): 2557-9. https://dx.doi.org/10.1016/S0140-6736(14)62302-3.
- Royal College of Obstetricians and Gynaecologists (RCOG). Shoulder Dystocia. Green-top Guideline No. 42. London: RCOG; 2005 (update 2017).
- National Institute for Health and Care Excellence. NICE Guidence: induction of labour. Evidence Update July 2013. Evidence. 2013; 44: 1-124.
- Clinical Practice Obstetrics Committee, Society of Obsetricians and Gynaecologists of Canada. Induction of labour. SOGC Clinical Practice Guideline No. 296, September 2013.
- WHO recommendations: induction of labour at or beyond term. Geneva: World Health Organization; 2018.
- Wormer K.C., Bauer A., Williford A.E. Bishop Score. In: StatPearls. Treasure Island, FL: StatPearls Publishing. 2021.
- Gonen O., Rosen D.J., Dolfin Z., Tepper R., Markov S., Fejgin M.D. Induction of labor versus expectant management in macrosomia: a randomized study. Obstet. Gynecol. 1997;89(6):913-7.https://dx.doi.org/10.1016/s0029-7844(97)00149-x.
- Magro-Malosso E.R., Saccone G., Chen M., Navathe R., Di Tommaso M., Berghella V. Induction of labour for suspected macrosomia at term in non-diabetic women: a systematic review and metaanalysis of randomized controlled trials. BJOG. 2017; 124(3): 414-21. https://dx.doi.org/10.1111/1471-0528.14435.
- Tey A., Eriksen N.L., Blanco J.D. A prospective randomized trial of induction versus expectant management in nondiabetec pregnancies with fetal macrosomia. Am. Obstet. Gynecol. 1995; 172(1): 203. https://dx.doi.org/10.1016/0002-9378(95)90803-x.
- Vitner D., Bleicher I., Kadour-Peero E., Borenstein-Levin L., Kugelman A., Sagi S., Gonen R. Induction of labor versus expectant management among women with macrosomic neonates. A retrospective study. J. Matern. Fetal Neonatal Med. 2020; 33(11): 1831-9. https://dx.doi.org/10.1080/2018.1531121.
- Boulet S.L., Alexander G.R., Salihu H.M., Pass M. Macrosomic births in the United States: Determinants, outcomes and prposed grades of risk. J. Obstet. Gynecol. 2003; 188(5): 1372-8. https://dx.doi.org/10.1067/mob.2003.302.
-
Boulvain M., Senat M.V., Perrotin F., Winer N., Beucher G., Subtil D. et al. Induction of labour versus expectant management for large-for-date fetuses: a randomised controlled trial. Lancet. 2015; 385(9987): 2600-5.
https://dx.doi.org/10.1016/S0140-6736(14)61904-8.
- Sinclair B.A., Rowan J.A., Hainsworth O.T. Macrosomic infants are not all equal. Aust. N.Z.J. Obstet. Gynaecol. 2007; 47(2): 101-5. https://dx.doi.org/10.1111/j.1479-828X.2007.00694.x.
-
Baeva I.Yu., Konstantinova O.D. Big fetus: Labor management tactics. Russian Bulletin of Obstetrician-Gynecologist. 2015; 15(3): 44-7. (in Russian).
https://dx.doi.org/10.17116/rosakush201515344-47.
- Tysyachny O.V., Baev O.R, Krechetova L.V. The course and outcomes of labor in relation to management tactics during prolonged pregnancy. Obstetrics and Gynecology. 2016; 7: 28-33. (in Russian)]. https://dx.doi.org/10.18565/aig.2016.7.28-33.
Received 25.11.2021
Accepted 16.12.2021
About the Authors
Victoria A. Odinokova, postgraduate student, Academician V.I. Kulakov National Medical Research Center for Obstetrics, Gynecology and Perinatology, Ministry of Health of Russia, +7(905)724-02-64, v_odinokova@oparina4ru, 117997, Russian Federation, Moscow, Oparin str., 4.Roman G. Shmakov, Dr. Med. Sci., Professor of the RAS, Academician V.I. Kulakov National Medical Research Center for Obstetrics, Gynecology and Perinatology, Ministry of Health of Russia, +7(495)438-72-00, r_shmakov@oparina4.ru, 117997 Russian Federation, Moscow, Oparin str., 4.
Authors’ contributions: Odinokova V.A., Shmakov R.G. - the concept and design of the study; Odinokova V.A. - material collection, statistical data processing, writing the article; Shmakov R.G. - editing the article.
Conflicts of interest: The authors declare that they have no conflicts of interest.
Funding: The study was carried out without any additional financial support.
Patient Consent for Publication: All patients provided informed consent for the publication of their data.
Authors' Data Sharing Statement: The data supporting the findings of this study are available on request from the corresponding author after approval from the principal investigator.
For citation: Odinokova V.A., Shmakov R.G. Birth outcomes in primiparous women diagnosed with fetal macrosomia and managed with active surveillance and watch-and-wait approach.
Akusherstvo i Gynecologia/Obstetrics and Gynecology. 2022; 1: 72-79 (in Russian)
https://dx.doi.org/10.18565/aig.2022.1.72-79