Obstetric and neonatal outcomes of spontaneous labor with a large fetus depending on the gestational age
Tysyachnyi O.V., Prikhodko A.M., Baev O.R.
Background: Fetuses that are large for gestational age pose a risk of macrosomia, particularly when excessive growth occurs at full-term gestational age. However, not all large-for-gestational-age fetuses are born with macrosomia, which can result from either earlier delivery or a decrease in growth rate over time. Existing studies on the outcomes of labor induction for fetal macrosomia typically focus on fetal body weight at the time of induction, with few considering gestational age. Investigating the outcomes of spontaneous labor in large-for-gestational-age fetuses can help to identify the most favorable gestational age for delivery and reduce the incidence of such cases.
Objective: To study obstetric and neonatal outcomes of spontaneous labor with a large fetus depending on gestational age.
Materials and methods: This retrospective cohort study included 571 healthy primiparous women who were divided into two groups based on ultrasound findings. The control group comprised pregnancies with fetal sizes ranging from the 10th to the 80th percentile (n=345), while the study group included pregnancies with large-for-gestational-age fetuses above the 90th percentile (n=226). Each group was further divided into four subgroups: subgroup 1 – gestational age 37 weeks, subgroup 2 – 38 weeks, subgroup 3 – 39 weeks, and subgroup 4 – 40 weeks.
Results: The overall rates of operative deliveries and cesarean sections were significantly higher in the study group – 23% versus 11.6% for operative deliveries (p=0.0004) and 21.2% versus 8.7% for cesarean sections (p<0.0001). Among women with large fetuses at 36–37 weeks of pregnancy, every third observation at 38–39 weeks resulted in the birth of a child with macrosomia, whereas this occurred every in second observation at 40 weeks. The lowest cesarean section rates and occurrence of large fetuses were noted at 38–39 weeks.
Conclusion: Pregnant women with an estimated fetal weight at the 90th percentile or higher, determined by ultrasound at 36–37 weeks, are at an increased risk of higher cesarean section rates and the birth of large fetuses. The optimal delivery window for these cases was between the end of the 37th week and the beginning of the 39th week, during which the lowest cesarean section rates were observed.
Authors’ contributions: Baev O.R. – conception and design of the study; Tysyachnyi O.V. – material collection and processing, drafting of the manuscript, statistical analysis; Prikhodko A.M. – editing of the manuscript.
Conflicts of interest: The authors have no conflicts of interest to declare.
Funding: There was no funding for this study.
Ethical Approval: The study was reviewed and approved by the Research Ethics Committee of the V.I. Kulakov NMRC for OG&P.
Patient Consent for Publication: All patients provided informed consent for the publication of their data.
Authors' Data Sharing Statement: The data supporting the findings of this study are available upon request from the corresponding author after approval from the principal investigator.
For citation: Tysyachnyi O.V., Prikhodko A.M., Baev O.R. Obstetric and neonatal outcomes of
spontaneous labor with a large fetus depending on the gestational age.
Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2025; (4): 44-50 (in Russian)
https://dx.doi.org/10.18565/aig.2025.36
Keywords
Currently, in obstetrics, the terms "large fetus" and "macrosomia" characterize the birth of a child weighing 4000 g or more, regardless of gestational age. Additionally, the term "large fetus for gestational age" qualifies a fetal body weight that exceeds the expected range for gestational age by more than the 90th percentile, as determined by ultrasound (US) examination. It follows that this group of fetuses represents a potential pool for the birth of a macrosomic infant, particularly if excessive growth continues until full-term gestational age [1, 2]. However, not all large-for-gestational-age fetuses are born with macrosomia; this can be attributed to factors such as earlier delivery and decreased growth rates over time. It is well established that the birth of a large fetus is associated with a heightened risk of adverse obstetric and neonatal outcomes [3, 4]. One method for preventing complications associated with macrosomia is labor induction [5, 6]. However, current data on the outcomes of labor induction in cases of fetal macrosomia typically focus only on the fetal body weight at the time of induction, with few studies considering gestational age [7].
Furthermore, examining the outcomes of spontaneous labor in cases of large-for-gestational age fetuses could help to identify the most favorable gestational age for delivery and reduce the percentage of large fetuses [8].
This study aimed to investigate the obstetric and neonatal outcomes of spontaneous labor with a large fetus, depending on gestational age.
Materials and methods
We conducted a retrospective cohort study analyzing 2,721 birth histories from the electronic database of V.I. Kulakov NMRC for OG&P of the Ministry of Health of Russia from 2023 to 2024.
The inclusion criteria for the study were primiparous women aged 18–40 years, with spontaneously occurring singleton pregnancies, cephalic presentation of the fetus, full-term pregnancies, and estimated fetal weights at or above the 10th percentile according to ultrasound data. At 36–37 weeks of pregnancy, all women underwent an assessment of estimated fetal weight using ultrasound fetal biometry, followed by calculation using the Hadlock formula. After applying the inclusion criteria, 571 women were included in the study.
Exclusion criteria included severe somatic pathology (such as diabetes), complicated pregnancies (including preeclampsia, gestational arterial hypertension, and gestational diabetes mellitus), planned cesarean sections, induction/pre-induction of labor, uterine developmental abnormalities, fetal malformations, and abnormalities in fetal condition, as determined by functional research methods (cardiotocography and Doppler ultrasound).
The study involved an analysis of medical data related to women and their newborns, including clinical and anamnestic data, pregnancy and childbirth characteristics, and the condition of the children at birth and during their hospital stay. The source of clinical data was archival records of the history of childbirth and development of newborns.
After applying the inclusion criteria, the women were divided into two groups. The control group consisted of women with normal fetal sizes (between the 10th and 80th percentiles) (n=345). The study group included 226 women with fetuses classified as large for gestational age according to the ultrasound data (90th percentile and above). Observations with fetal body weights between the 81st and 89th percentiles were excluded from the study to reduce the likelihood of misclassification in the "large for term" category.
The primary outcome of the study was the incidence of cesarean section, and the secondary outcome was the assessment of neonatal outcomes.
The study was reviewed and approved by the Research Ethics Committee of V.I. Kulakov NMRC for OG&P.
Statistical analysis
Statistical analysis was performed using IBM SPSS Statistics version 22 for Windows. The normality of the distribution was tested using the Shapiro–Wilk criterion. Continuous variables with a normal distribution were described using arithmetic mean (M) and standard deviation (SD). The Mann–Whitney U-test was used to compare the two groups by continuous variables in the absence of a normal distribution. Fisher's test was applied to check for equality of variances before parametric statistical methods were used. When comparing two groups for continuous variables with a normal distribution and equal variances, the Student's t-test was used. For data lacking a normal distribution, quantitative data were described using the median (Me) and lower and upper quartiles (Q1; Q3). Categorical data were described using counts and percentages, and Pearson's chi-squared test was used for group comparisons. Relative risk (RR) was used as a measure of the effect size, and the level of statistical significance was set at p<0.05.
Results
Analysis of the age data showed no statistically significant differences between the groups. The mean age of women in the control group was 32.6 (1.9) years versus 32.1 (7.2) years in the study group (p=0.41). There were no significant differences in the mean body mass index of the women, which was 24.6 (5.1) kg/m2 versus 25 (1.1) kg/m2 (p=0.33).
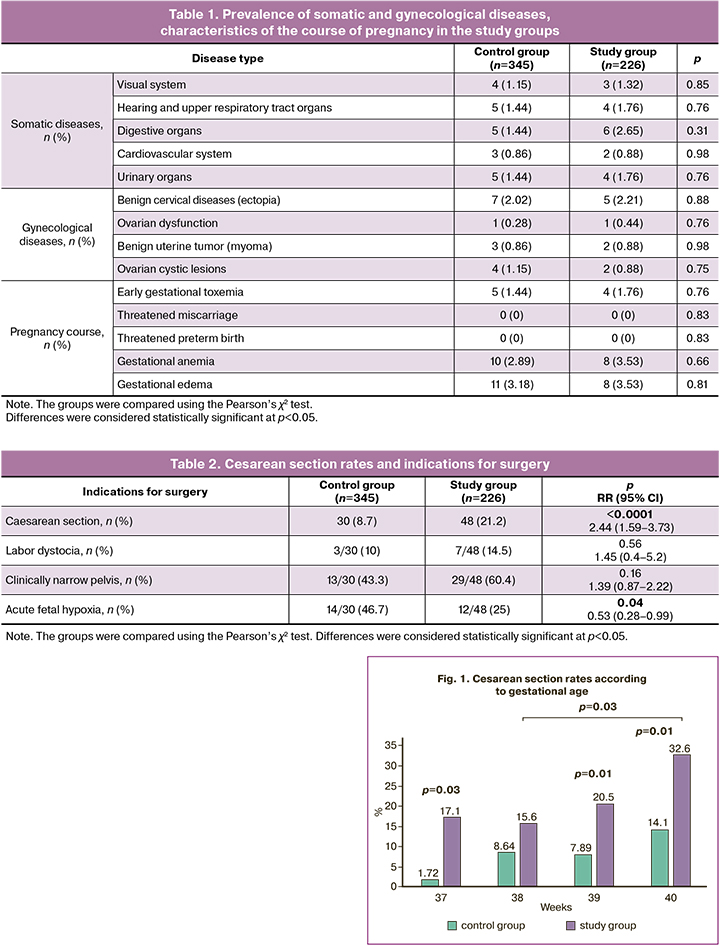
After comparing the groups, no significant differences were found in the frequency and structure of somatic diseases, gynecological history, or course of pregnancy, as shown in Table 1.
In the study group, the overall operative delivery rate was 1.9 times higher and was 52/226 (23%) versus 40/345 (11.6%) in the control group (p=0.0004). The delivery rate by vacuum extraction in the compared groups did not differ and was 4/226 (1.7%) and 10/345 (2.9%), respectively. In all cases, the indication for vacuum extraction was acute fetal hypoxia.
The incidence of cesarean section in the study group was 2.4 times higher and amounting to 48/226 (21.2%) versus 30/345 (8.7%) in the control group (p<0.0001) (Table 2).
In order to study the incidence of cesarean section depending on the gestational age at the time of spontaneous labor, the women were divided into 4 groups: 37 weeks, study group (n=35), control group (n=58); 38 weeks, study group (n=64), control group (n=81); 39 weeks, study group (n=78), control group (n=114); 40 weeks, the study group (n=49), the control group (n=92), which is presented in Table 3. The analysis showed that at 37, 39, and 40 weeks, the incidence of cesarean section in women with a large-for-gestational-age fetus was significantly higher than that in the control group: 6/35 (17.1%) versus 1/58 (1.72%) (p=0.03), 16/78 (20.5%) versus 9/114 (7.89%) (p=0.01), and 16/49 (32.6%) versus 13/92 (14.1%) (p=0.01), respectively (Fig. 1). When analyzing the incidence of cesarean sections in the control groups by gestational age, no differences were found (p>0.05). In the study group, at 38 weeks, the frequency of cesarean section was significantly lower than that at 40 weeks (10/64 (15.6%) versus 16/49 (32.6%) (p=0.03).
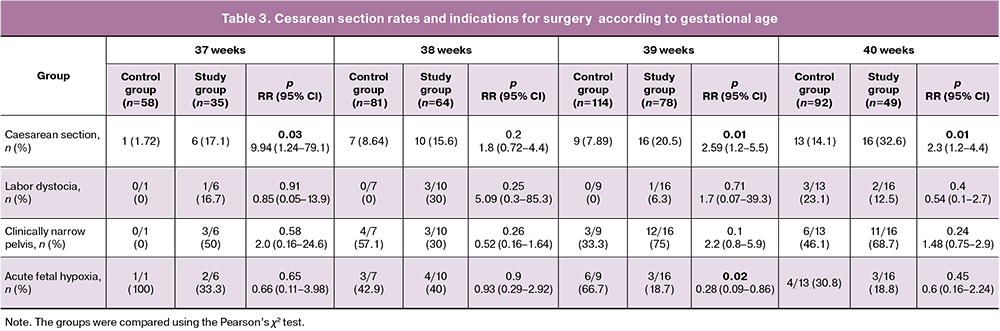
When comparing the structure of the indications for cesarean delivery, acute fetal hypoxia was found to be significantly more common in the control group at 39 weeks; no differences were found for other indications.
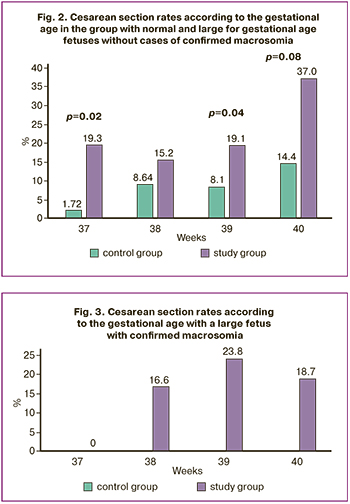
Next, we analyzed the cesarean section rate according to the gestational age and fetal birth weight. For this purpose, each group was divided into two subgroups: 1st – without fetal macrosomia, 2nd – with fetal macrosomia. The results showed that in the subgroups without fetal macrosomia, the cesarean section rate increased with increasing gestational age. At the same time, a significantly higher frequency of cesarean sections was observed at 37, 39, and 40 weeks in the study group (Fig. 2). Analysis of the subgroup with confirmed fetal macrosomia also showed an increase in cesarean section rates with increasing gestational age, but no differences were found between the groups (Fig. 3).
No cases of fetal shoulder dystocia were observed during the study.
The main data on the newborns and the results of their observations are presented in Table 4. Apgar scores at the 1st and 5th minutes were comparable in both groups. The number of newborns who had an Apgar score of 7 or less in the 1st minute did not differ between the groups; at the 5th minute, an Apgar score of 7 or less was more common in the study group (1.76% versus 0.28 %), but the differences were not significant.
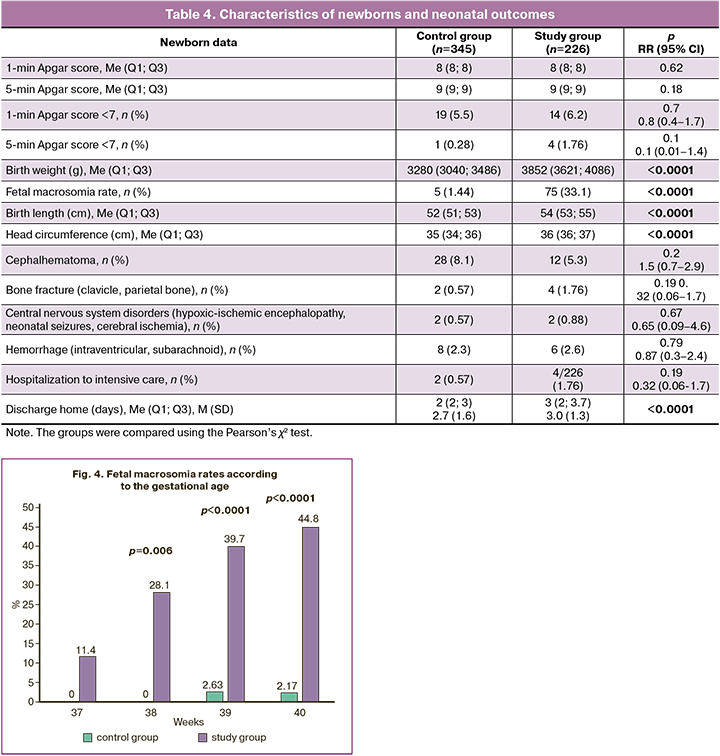
Evaluation of the anthropometric data of newborns showed significantly higher birth weight, birth length, and head circumference in the study group (p < 0.0001). All the children were born alive. The number of newborns with macrosomia was 5/345 (1.44%) in the control group and 75/226 (33.1%) in the study group (p<0.0001). Analysis of the frequency of large fetuses according to gestational age showed that starting from the 38th week of pregnancy, there were significant differences (Fig. 4). When analyzing the outcomes for newborns, it should be noted that, despite the significantly higher weight of newborns in the study group, cephalohematomas in this group were 1.5 times less common than in the control group; however, the number of newborns with bone fractures (clavicle and parietal bone) and hospitalization in the intensive care unit were three times more common in the study group, although the differences in these indicators were not significant. Due to the higher frequency of birth trauma, newborns in the study group stayed in the hospital longer and were discharged home later: 3 days versus 2 days (p<0.0001). No differences were found between the groups for the other parameters studied.
Discussion
A large randomized controlled trial on the management of pregnant women with fetal macrosomia demonstrated that labor induction significantly reduces the incidence of severe fetal shoulder dystocia, with a risk ratio of 0.32 (0.12–0.85) [9, 10]. However, the use of labor induction as a preventative strategy for complications associated with macrosomia remains contentious [11]. A notable limitation in resolving this issue is the insufficient data on obstetric and neonatal outcomes of spontaneous labor among pregnant women with a large-for-gestational-age fetus.
In this context, our study examined obstetric and neonatal outcomes of labor in pregnant women with a large-for-gestational-age fetus stratified by gestational age. For each gestational age, a control group of women with normal-sized fetuses was established. Our results indicated that the proportion of operative deliveries and the incidence of cesarean sections were significantly higher in the study group (23% vs. 11.6%, p=0.0004) and 21.2% compared with 8.7% (p<0.0001), respectively. At 37, 39, and 40 weeks of pregnancy, the rate of cesarean section was notably elevated in the study group.
Analysis of cesarean section rates based on gestational age and fetal weight revealed a similar trend in both the normal fetal size and large-for-gestational-age groups.
Analysis of perinatal outcomes showed that the birth weight, birth length of newborns, head circumference, and number of large fetuses in the study group were significantly higher (p<0.0001). Furthermore, an analysis of fetal macrosomia incidence by gestational age revealed that among women with a large-for-gestational-age fetus, as indicated by ultrasound at 36–37 weeks, one in three births at 38–39 weeks resulted in macrosomia, whereas this ratio increased to one in two at 40 weeks.
The frequency of births with an Apgar score of 7 or less at the 5th minute was more common in the study group (1.76 %) than in the control group (0.28 %). Additionally, the occurrence of bone fractures and the need for hospitalization in the intensive care unit were three times more frequent in the study group; however, the differences did not reach statistical significance, likely due to the limited number of observations.
The literature indicates a direct correlation between the timing of delivery and frequency of complications. For instance, Hong et al. demonstrated that with fetal macrosomia and expectant management of pregnancy, complications increase from 3.8 per 10,000 live births at 38 weeks to 3.2 by 40 weeks, with a minimum of 0.7 at 39 weeks [8]. We identified an optimal ratio between the cesarean section rate and the birth of a large fetus at 38–39 weeks.
Conclusion
Our study findings suggest that pregnant women whose estimated fetal weight is determined by ultrasound to be at least the 90th percentile at 36–37 weeks are at high risk for cesarean section and the birth of a large fetus. The optimal timing for delivery in these cases appears to be between the end of the 37th week and the beginning of the 39th week, when the lowest cesarean section rate was observed. Given these insights, further research into the effectiveness of labor induction for women with a large-for-gestational-age fetus, starting at 38 weeks of gestation, is warranted to potentially reduce the incidence of cesarean sections and complications associated with fetal macrosomia.
References
- Bair C.A., Cate J., Chu A., Kuller J.A., Dotters-Katz S.K. Nondiabetic fetal macrosomia: causes, outcomes, and clinical management. Obstet. Gynecol. Surv. 2024; 79(11): 653-64. https://dx.doi/org/10.1097/OGX.0000000000001326.
- Chandrasekaran N. Induction of labor for a suspected large-for-gestational-age/macrosomic fetus. Best Pract. Res. Clin. Obstet. Gynaecol. 2021; 77: 110-8. https://dx.doi/org/10.1016/j.bpobgyn.2021.09.005.
- Rezaiee M., Aghaei M., Mohammadbeigi A., Farhadifar F., Zadeh Ns., Mohammadsalehi N. Fetal macrosomia: risk factors, maternal, and perinatal outcome. Ann. Med. Health Sci. Res. 2013; 3(4): 546. https://dx.doi/org/10.4103/2141-9248.122098.
- Одинокова В.А., Шмаков Р.Г. Исходы родов у первородящих с фетальной макросомией при активной и выжидательной тактике. Акушерство и гинекология. 2022; 1: 72-9. [Odinokova V.A., Shmakov R.G. Birth outcomes in primiparous women diagnosed with fetal macrosomia and managed with active surveillance and watch-and-wait approach. Obstetrics and Gynecology. 2022; (1): 72-9 (in Russian)]. https://dx.doi.org/10.18565/aig.2022.1.72-79.
- Giouleka S., Tsakiridis I., Ralli E., Mamopoulos A., Kalogiannidis I., Athanasiadis A. et al. Diagnosis and management of macrosomia and shoulder dystocia: A comprehensive review of major guidelines. Obstet. Gynecol. Surv. 2024; 79(4): 233-41. https://dx.doi/org/10.1097/OGX.0000000000001253.
- Boulvain M., Irion O., Dowswell T., Thornton J.G. Induction of labour at or near term for suspected fetal macrosomia. Cochrane Database Syst. Rev. 2016; 2016(5): CD000938. https://dx.doi/org/10.1002/14651858.CD000938.pub2.
- Badr D.A., Carlin A., Kadji C., Kang X., Cannie M.M., Jani J.C. Timing of induction of labor in suspected macrosomia: retrospective cohort study, systematic review and meta‐analysis. Ultrasound Obstet. Gynecol. 2024; 64(4): 443-52. https://dx.doi/org/10.1002/uog.27643.
- Hong J., Crawford K., Odibo A.O., Kumar S. Risks of stillbirth, neonatal mortality, and severe neonatal morbidity by birthweight centiles associated with expectant management at term. Am. J. Obstet. Gynecol. 2023; 229(4) :451.e1-451.e15. https://dx.doi/org/10.1016/j.ajog.2023.04.044.
- Boulvain M., Senat M.V., Perrotin F., Winer N., Beucher G., Subtil D. et al.; Groupe de Recherche en Obstétrique et Gynécologie (GROG). Induction of labour versus expectant management for large-for-date fetuses: a randomised controlled trial. Lancet. 2015; 385(9987): 2600-5. https://dx.doi/org/10.1016/S0140-6736(14)61904-8.
- Капустин Р.В., Коптеева Е.В., Алексеенкова Е.Н., Цыбук Е.М., Аржанова О.Н., Коган И.Ю. Анализ факторов риска дистоции плечиков плода в родах у женщин с сахарным диабетом. Акушерство и гинекология. 2022; 9: 54-63. [Kapustin R.V., Kopteeva E.V., Alekseenkova E.N., Tsybuk E.M., Arzhanova O.N., Kogan I.Yu. Risk factors for shoulder dystocia during labor in women with diabetes mellitus. Obstetrics and Gynegology. 2022; (9): 54-63. (in Russian)]. https://dx.doi/org/10.18565/aig.2022.9.54-63.
- Boulvain M., Thornton J.G. Induction of labour at or near term for suspected fetal macrosomia. Cochrane Database Syst. Rev. 2023; 3(3): CD000938. https://dx.doi/org/10.1002/14651858.CD000938.pub3.
Received 19.02.2025
Accepted 24.03.2025
About the Authors
Oleg V. Tysyachnyi, PhD, Researcher at the 1st Maternity Department, V.I. Kulakov National Medical Research Center for Obstetrics, Gynecology and Perinatology,Ministry of Health of Russia, 117997, Russia, Moscow, Oparin str., 4, o_tysyachny@oparina4.ru, https://orcid.org/0000-0001-9282-9817
Oleg R. Baev, Dr. Med. Sci., Professor, Head of the 1st Maternity Department, V.I. Kulakov National Medical Research Center for Obstetrics, Gynecology and Perinatology, Ministry of Health of Russia, 117997, Russia, Moscow, Oparin str., 4; Professor at the Department of Obstetrics, Gynecology, Perinatology, and Reproductology,
I.M. Sechenov First Moscow State Medical University, Ministry of Health of Russia (Sechenov University), 119991, Russia, Moscow, Trubetskaya str., 8-2, +7(495)438-11-88, o_baev@oparina4.ru, https://orcid.org/0000-0001-8572-1971
Andrey M. Prikhodko, Dr. Med. Sci., doctor at the 1st Maternity Department, V.I. Kulakov National Medical Research Center for Obstetrics, Gynecology and Perinatology, Ministry of Health of Russia, 117997, Russia, Moscow, Oparin str., 4, +7(495)438-11-88, a_prikhodko@oparina4.ru, https://orcid.org/0000-0002-6615-2360