Родовозбуждение (индукция родов) остается одной из самых частых процедур в акушерско-гинекологической практике, и, по данным ряда авторов, до трети родов в настоящее время являются индуцированными [1]. Подготовка шейки матки (преиндукция родов) имеет важное значение для повышения эффективности родовозбуждения [2]. Для подготовки шейки матки к родам применяют как механические, так и фармакологические средства, однако до сих пор не существует консенсуса относительно оптимального метода и средства для преиндукции и индукции родов [3].
Баллонные катетеры для подготовки шейки матки сопоставимы по эффективности с препаратами простагландинов, но при этом безопаснее, так как не приводят к маточной тахисистолии с последующим изменением частоты сердечных сокращений плода [4, 5].
В настоящее время появляется все больше работ, в которых авторы приходят к выводу, что частота неблагоприятных перинатальных и материнских исходов неуклонно возрастает с увеличением срока беременности после 39 недель [6–9]. Есть данные, что при выжидательной тактике (по сравнению с индукцией родов) чаще возникают гипертензивные расстройства и преэклампсия, а также необходимость в респираторной поддержке новорожденным. В свою очередь, благодаря элективной индукции родов, возможно снижение частоты кесарева сечения [10, 11].
Целью нашего исследования явилось сравнение эффективности индукции родов у пациенток в сроке беременности 284–285 дней («Full term») и 287 и более дней («Late term»).
Материалы и методы
Проспективное исследование эффективности индукции родов проведено в Национальном медицинском исследовательском центре акушерства, гинекологии и перинатологии им. В.И. Кулакова Минздрава России с сентября 2017 по сентябрь 2019 г. На исследование получено разрешение локального Этического комитета. Исследование проводили в соответствии с требованиями Хельсинкской декларации (1964, 2013). Все участницы подписали добровольное информированное согласие.
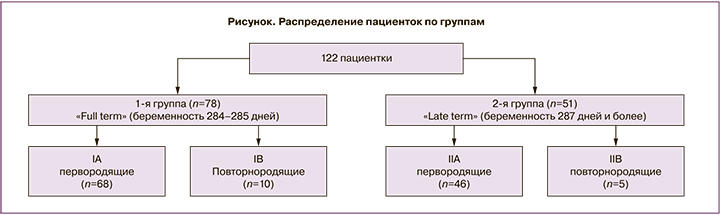
В исследование включены 129 беременных женщин, которые были разделены на две группы, в зависимости от срока беременности (рисунок).
Установление срока беременности и предполагаемой даты родов производили с учетом параметров менструального цикла (первый день последней менструации, регулярность/нерегулярность цикла и его продолжительность в днях) после сопоставления и подтверждения с помощью данных ультразвуковых исследований (УЗИ). Срок по дате менструации сопоставляли с результатом УЗИ в I триместре в 11–14 недель, так как этот метод признан наиболее точным в установлении срока беременности. Если различие между сроком по менструации и результатами УЗИ, проведенного в I триместре, составляет более 5 дней или более 10 дней во II триместре, то предполагаемую дату родов рассчитывали по результатам УЗИ. При наличии результатов УЗИ в I и II триместре срок рассчитывали по более раннему исследованию. При использовании вспомогательных репродуктивных технологий (ВРТ) расчет срока беременности и даты родов производили по дате переноса эмбриона с учетом его возраста в днях.
Критериями включения в исследование служили: возраст пациенток 18–45 лет; одноплодная беременность; головное предлежание плода; срок беременности 284 дней и более; неготовность родовых путей на момент включения в исследование (оценка по шкале Бишоп менее 8 баллов); наличие показаний к индукции родов; отсутствие противопоказаний к влагалищным родам и применению других препаратов для подготовки к родам (мифепристон, простагландин Е2, окситоцин); подписанное информированное согласие. Критериями невключения в исследование явились: миома или аномалии развития матки; количество родов в анамнезе более 3; предшествующее родоразрешение путем операции кесарева сечения; тяжелые заболевания сердца; артериальная гипертензия 160/100 мм рт. ст. и выше; выраженные нарушение функции печени, почек, надпочечников; тазовое предлежание плода; многоводие; предполагаемая масса плода менее 2000 г и более 4500 г; активная герпесвирусная инфекция; рак шейки матки; показатели кардиотокографии, указывающие на нарушение состояния плода; наличие показаний к плановому родоразрешению путем операции кесарева сечения; преждевременное излитие околоплодных вод.
Женщины, включенные в исследование, получали разъяснение от врача-исследователя о показаниях к индукции родов, последовательности проведения процедуры, возможных осложнениях, побочных эффектах и исходах. После подписания информированного согласия, сбора анамнеза, общего и акушерского обследования, оценки состояния плода в 19 ч вечера в шейку матки устанавливали двухбаллонный катетер для подготовки шейки матки к родам (Cook Cervical Ripening Balloon with Stylet Cook Medical) в соответствии с инструкцией производителя. Через 12 ч баллон удаляли и пациентку осматривали повторно. Если оценка зрелости по шкале Бишоп составляла 8 баллов и более – производили амниотомию и наблюдали за развитием родовой деятельности.
Началом родов считали появление регулярных маточных сокращений (2—3 за 10 минут и более) с прогрессирующим сглаживанием и открытием шейки матки. Активной фазой родов считали достижение полного сглаживания и открытия шейки матки более 4 см.
При отсутствии схваток в течение 4 ч после амниотомии приступали к родовозбуждению окситоцином в соответствии с протоколом нашего Центра. Тахисистолией считали частоту схваток более 5 за 10 минут в 30-минутном интервале.
Если родовозбуждение окситоцином в течение 4 ч не сопровождалось появлением схваток с адекватным раскрытием шейки матки, то результат расценивали как отсутствие эффекта от родовозбуждения.
Если после удаления баллона оценка по шкале Бишоп составляла менее 8 баллов, то для продолжения подготовки к родам использовали гель с динопростоном (0,5 мг), который вводили в цервикальный канал в соответствии с инструкцией производителя. По достижении степени зрелости шейки матки 8 баллов и более производили амниотомию. При отсутствии схваток через 4 ч начинали родовозбуждение окситоцином.
Если после использования геля с динопростоном оценка по шкале Бишоп составляла менее 6 баллов, результат расценивали как отсутствие эффекта от подготовки шейки матки к родам.
До и после установки баллона, его удаления и амниотомии, а также непрерывно во время инфузии окситоцином и во время родов проводили оценку состояния плода с помощью кардиотокографии.
Первичными оценками исхода являлись: изменение оценки по шкале Бишоп после удаления баллона; интервал от извлечения баллона до начала родов и интервал до родоразрешения (влагалищным путем); количество женщин, родивших влагалищным путем в течение 24 ч от введения баллона; частота отсутствия эффекта от подготовки к родам и родовозбуждения, частота родоразрешения путем операции кесарева сечения.
Вторичными оценками исхода являлись: частота и выраженность болезненных ощущений при проведении подготовки шейки матки к родам баллоном; метод родоразрешения; частота маточной тахисистолии; необходимость в родовозбуждении или родостимуляции окситоцином; продолжительность родов и безводного промежутка; исходы для новорожденных.
Статистическую обработку материала проводили с использованием статистических программ IBM SPSS Statistics v22 for Windows (США), MedCalc (США) и Microsoft Office Excel 2010.
Статистическую обработку полученных результатов проводили с помощью статистической программы IBM SPSS Statistics 22 for Windows. Проверку гипотезы о нормальном распределении осуществляли, используя критерий Шапиро–Уилка. При нормальном распределении рассчитывали среднее значение (М) и стандартное отклонение (SD), для сравнения данных использовали t-тест. При распределении признаков, отличных от нормального, для сравнения данных использовали тест Манна–Уитни, данные представляли в виде медианы и интерквартильного интервала. Для качественных данных рассчитывали частоты и использовали точный тест Фишера. Различия между сравниваемыми величинами признавали статистически значимыми при p<0,05.
Результаты
Как следует из данных, приведенных в табл. 1, группы пациенток оказались сопоставимы по среднему возрасту, массе тела и росту, но при этом отмечалась статистически значимая разница в значении индекса массы тела (25,59 (3,07)) кг/м² и (26,78 (3,48)) кг/м² соответственно (р=0,03) и количестве наблюдений, где беременность наступила в результате применения ВРТ (15,4 и 13,7% соответственно (р=0,03). Анализируя паритет женщин в исследовании, мы пришли к выводу, что в обеих группах подавляющее большинство были первобеременными/первородящими (70,5%/87,2% и 82,4%/90,2% соответственно).
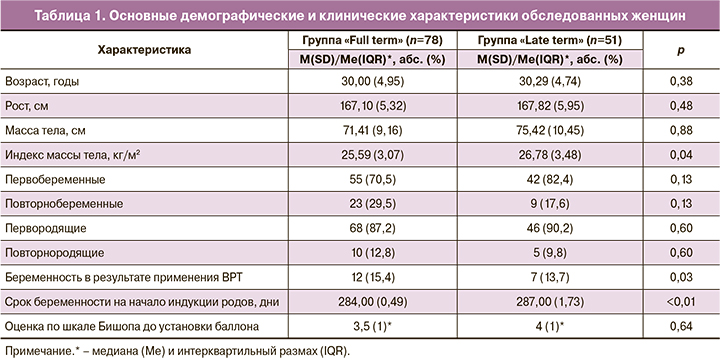
До установки двухбаллонного катетера 13 (16,67%) пациенткам группы «Full term» и 25 (49,02%) пациенткам группы «Late term» был назначен пероральным прием 200 мг мифепристона с целью подготовки шейки матки (ШМ) к родам.
Основным показанием к подготовке ШМ к родам и родовозбуждению в обеих группах послужила неготовность родовых путей в сроке 284 дня и более, свидетельствующая о тенденции к перенашиванию беременности, – 70 (89,7%) и 46 (90,2%) наблюдений соответственно (р=0,93); крупный плод – 2 (6,3%) и 4 (7,8%) (р=0,19). В группе «Full term» анатомическое сужение таза послужило показанием в 5,1% наблюдений, а осложненное течение беременности в 2,6% и 2% наблюдений группы «Late term».
В 13 наблюдениях пациенткам группы «Full term» и в 25 группы «Late term» до установки двухбаллонного катетера был назначен пероральный прием 200 мг мифепристона с целью подготовки ШМ к родам. Как показали полученные результаты (табл. 2), после удаления баллонного катетера прирост оценки по шкале Бишопа в группах не различался (составила 3 (2)* и 2 (3)* балла соответственно (р=0,47)). Медиана оценки по шкале Бишопа составила 7 (1,5)* и 6 (2,25)* баллов соответственно (р=0,29).
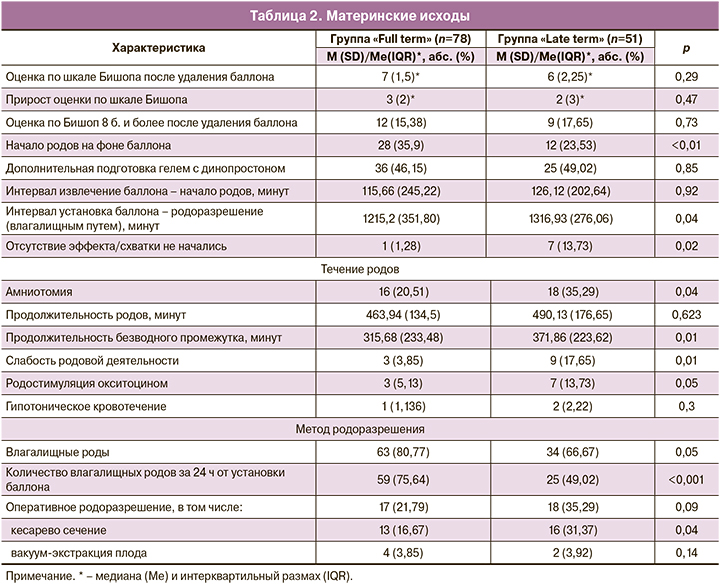
В 35,9% и 23,53% наблюдений роды начались до извлечения баллона (значительно чаще у пациенток группы «Full term (р<0,01)).
При недостаточно зрелой ШМ после извлечения двухбаллонного катетера дополнительную подготовку гелем с динопростоном 0,5 г №1 провели в 36 (46,15%) наблюдениях группы «Full term» и в 25 (49,02%) наблюдениях пациенток группы «Late term» (р=0,85); 16 (20,51%) пациенткам группы «Full term» и 18 (35,29%) пациенткам группы «Late term» с целью родовозбуждения была произведена амниотомия (р=0,04), из них повторнородящими были только по 1 женщине в каждой группе.
Мероприятия по подготовке ШМ к родовозбуждению обеспечили развитие родовой деятельности у 77 (98,72%) пациенток группы «Full term» и 44 (86,27%) из группы «Late term» (р=0,02).
Средняя продолжительность интервала от извлечения двухбаллонного катетера до начала схваток не различалась (табл. 2). Однако от момента установки катетера до рождения ребенка в группе «Full term» проходило меньше времени (1215,19 (351,80) мин) по сравнению с группой «Late term» (1316,93±276,06 мин) (р=0,04). Из этого следовало, что в группе «Full term» чаще происходило родоразрешение через естественные родовые пути в течение 24 ч от момента установки двухбаллонного катетера в ШМ: 59 (75,64%) наблюдений по сравнению с группой «Late term» – 25 (49,02%) наблюдений (р<0,01).
Частота неуспешной индукции родов была выше в группе «Late term» – 7 (13,73%) наблюдений по сравнению с группой «Full term» – всего 1 (1,28%) наблюдение (р=0,02).
Ни в одном наблюдении у пациенток группы «Full term» не потребовалось проводить родовозбуждение окситоцином. В группе «Late term» у 3 (5,88%) роды начались только после внутривенного капельного введения окситоцина по схеме родовозбуждения.
У пациенток группы «Late term» чаще возникала слабость родовой деятельности – в 9 (17,65%) наблюдениях, тогда как в группе «Full term» это осложнение возникло только в 3 (3,85%) наблюдениях (р=0,01), причем все пациентки были первородящими. Родостимуляцию окситоцином производили чаще в группе «Late term» – 7 (13,73%) пациенток и 3 (5,13%) пациенток группы «Full term» (р=0,05), а еще в двух наблюдениях было решено отказаться от родостимуляции окситоцином и произвести операцию КС.
В 63 (80,77%) наблюдениях группы «Full term» и 34 (66,67%) наблюдениях группы «Late term» родоразрешение произошло через естественные родовые пути (р=0,05) (из них 4 пациенткам группы «Full term» и 2 пациенткам группы «Late term» была произведена операция вакуум-экстракции плода (р=0,14)).
Средняя продолжительность родов в группах не различалась (см. табл. 2). При этом средняя длительность безводного промежутка была короче в группе «Full term», чем в группе «Late term» – 315,68 (233,48) минут и 371,86 (223,62) минут соответственно (р=0,01).
Не было различий в частоте эпидуральной аналгезии, разрыва промежности и эпизиотомии, гипотонического кровотечения (см. табл. 2).
В 13 (16,67%) наблюдениях в группе «Full term» и в 16 (31,37%) наблюдениях группы «Late term» возникла необходимость в завершении родов путем операции кесарева сечения (р=0,04). Наиболее частыми показаниями являлась гипоксия плода (38,46 и 18,75%, р>0,05), слабость родовой деятельности (23,07 и 37,5%, р>0,05). В 7,69 и 43,75% случаев показанием явилось отсутствие эффекта от родовозбуждения (р=0,05). Не было ни одного наблюдения, где возникли маточная тахисистолия, инфекционные осложнения и существенные побочные эффекты.
Все дети от пациенток, включенных в исследование, родились живыми (табл. 3).
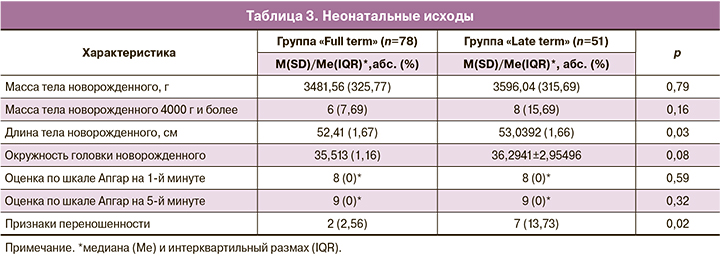
Не было различий в оценке состояния новорожденных детей по шкале Апгар в двух группах на 1-й и 5-й минутах жизни (см. табл. 3). Не было зарегистрировано ни одного наблюдения, где ребенок получил оценку по шкале Апгар менее 7 баллов к 5-й минуте жизни. Средняя масса тела новорожденных, по результатам исследования, не различалась. Средняя длина тела оказалась несколько выше в группе «Late term». Также в этой группе значимо чаще рождались дети с признаками переношенности (см. табл. 3), причем преобладали первородящие пациентки (р=0,02).
Обсуждение
В этом исследовании проведено сравнение эффективности родовозбуждения у пациенток в сроке беременности 284–285 дней («Full term») и 287 и более дней («Late term»).
Анализ полученных результатов показал, что наиболее часто подготовку шейки матки к родам и родовозбуждение в сроке беременности 284 дня и более проводят первородящим женщинам, а наиболее частым показанием является тенденция к перенашиванию беременности, что соответствует данным мировой литературы [12, 13].
После преиндукции двухбаллонным катетером прирост оценки зрелости ШМ по шкале Бишоп составил в среднем 3 балла, что совпадает с данными других авторов [14, 15].
В 46 и 49% наблюдений при недостаточной зрелости ШМ после удаления баллона нами были использованы препараты простагландинов Е2 (р=0,85), а по данным Hoppe К. и соавт. [15], частота дополнительной фармакологической подготовки потребовалась в каждом пятом наблюдении. По данным Policiano С. и соавт. [13], необходимость в дополнительной подготовке ШМ простагландинами имела место в 53% наблюдений.
В проведенном исследовании родовозбуждение и родостимуляция окситоцином не являлись рутинной частью протокола и были применены в 5,88% наблюдений (р=0,06) (преобладали пациентки со сроком беременности более 287 дней – группа «Late term»), тогда как, по данным других авторов, частота применения окситоцина достигает 75–88% [16]. Все вышеуказанное свидетельствует о высокой эффективности подготовки ШМ к родам в сроке беременности 284–285 дней – группа «Full term».
Важным параметром, отражающим эффективность мероприятий по подготовке ШМ к родам, является частота родоразрешения в течение 24 ч от момента начала индукции до рождения ребенка. В нашей работе данный параметр был достоверно выше у пациенток группы «Full term» (75,64%), чем в группе «Late term» (49,02%) (р<0,01), и это лучше результатов Cheuk Q.K. и соавт. (2015), Brown J. и соавт. (2017) [16, 17].
Интервал от момента установки катетера до момента рождения ребенка через естественные родовые пути в двух группах составил 1215,19±351,80 минут и 1316,93±276,06 минут соответственно (р=0,04), что больше аналогичного показателя в работах Sayed Ahmed W.A. и соавт., Mei-Dan E. и соавт. [14, 18] и меньше, чем в исследовании Hoppe K. и соавт. [15]. Это можно объяснить разной тактикой ведения родов и, в частности, подходом к назначению окситоцина.
По данным литературы, при индукции родов частота влагалищного родоразрешения колеблется в пределах 60–85% [19–22]. В нашем исследовании подготовка ШМ и родовозбуждение завершились родами через естественные родовые пути в 80,77 и 66,67% наблюдений (р=0,05), при этом чаще влагалищным путем рожали пациентки группы «Full term». Частота кесарева сечения в нашей работе составила 16,67 и 31,37% (р=0,04) (чаще абдоминальное родоразрешение вынуждены были проводить у пациенток группы «Late term»). По данным Solt I. и соавт., этот показатель равен 12,9% [23], в работе Sayed Ahmed W.A. и соавт. – 21,6% [14], в исследованиях Brown J. и соавт. [17] и Hoppe K. и соавт. [15] частота КС была 28,1 и 28% соответственно, у Policiano C. и соавт. [13] – 37%.
В настоящее время в литературе не существует единого определения успеха/неуспеха индукции родов. Наиболее часто для определения этих понятий используют частоту влагалищных родов, спонтанных влагалищных родов, родоразрешения в первые 24 ч от начала мероприятий [24]. Частота неуспеха индукции составила, по нашим данным, 6,2%, что соответствует данным литературы [15]. При этом частота неудачи при индукции родов в группе «Full term» была в 10 раз ниже таковой в группе «Late term».
Следует отметить, что в нашей работе не было ни одного наблюдения с маточной тахисистолией, тогда как в других исследованиях ее частота достигала 5% [4, 17].
Заключение
Индукция родов более эффективна в сроке беременности 284–285 дней (в группе «Full term»), чем в сроке беременности 287 дней и более (группа «Late term»), так как реже наблюдается отсутствие эффекта от подготовки ШМ и индукции родов; реже возникает слабость родовой деятельности и потребность в назначения окситоцина для ее медикаментозной коррекции; короче интервал от момента установки двухбаллонного катетера до рождения ребенка через естественные родовые пути и безводный промежуток; реже рождаются дети с признаками переношенности; ниже частота кесарева сечения. Полученные результаты подтверждают современные данные литературы о безопасности и эффективности родовозбуждения с целью улучшения материнских и перинатальных исходов в сроке до 41 недели (287 дней).