Comparative evaluation of mechanical methods for preparing the cervix for induction of labor in pregnant women with extragenital pathologies
Objective. To evaluate the effectiveness of mechanical (osmotic) dilators Dilapan-S and laminaria tents in preparing the cervix for term programmed labor in patients with extragenital pathologies.Shaposhnikova E.V., Dikke G.B., Bazina M.I., Tskhai V.B., Egorova A.T., Mentsik M.M., Tsaryuk E.P., Zhirova N.V.
Materials and methods. Fifty-seven pregnant women at 380-6 to 390-4 weeks of gestation were divided into two groups: group 1 (main) included 32 patients who underwent Dilapan-S induction and group 2 (control) enrolled 25 women using laminaria tents. The condition of the cervix was assessed with the Bishop score before placing and after extracting the dilators. The condition of the fetus during cervical preparation was monitored using cardiotocography.
Results. According to the Bishop score, when the action of Dilapan-S finished the degree of cervical ripening increased from Me 3 (Q1 2; Q3 4) to Me 8.5 (Q1 8; Q3 9) points (+5.5; p=0.001) and it was higher than in group 2, Me 8 (Q1 7; Q3 8) points (+5; p=0.01). The women had vaginal delivery in 75% (24/32) of cases in group 1 versus 68% (17/25) in group 2 (р=0.77). Spontaneous onset of labor was observed in 46.9% (15/32) versus 20% (5/25) of cases, (RR = 2.3; 95% CI: 0.99–5.57; p=0.07), respectively. Side effects of both Dilapan-S and laminaria tents were noted rarely and were insignificant.
Conclusion. Dilapan-S facilitates cervical ripening more effectively than laminaria tents. There is no statistically significant difference in labor induction rate and its outcomes. Dilapan-S has a good safety profile.
Keywords
Extragenital pathologies that complicate the course of pregnancy, childbirth and the postpartum period have proven to be a serious public health problem being the leading cause of maternal mortality. The most frequent of them are anemia (34% of pregnant women in 2017), diseases of the circulatory system (8%) and endocrine system (8%). Their incidence has remained relatively stable over the past decade with minor annual fluctuations in the range of 2–3% [1].
Managing pregnant women, choosing the time and mode of delivery for the patients with comorbid conditions are associated with difficulties due to the adverse influence of chronic diseases and pregnancy, as well as the use of medications, taking into account the ratio of benefits and risks for the mother and fetus. The presence of concomitant pathology that complicates the course of pregnancy contributes to an induced labor till 38–39 weeks [2].
It has been proved that successful course and outcome of labor depend on how a woman’s body is prepared for childbirth, both in spontaneous delivery and planned labor [3].
Nowadays, the methods used for preparing the cervix for delivery in full-term pregnancy are divided into mechanical (Foley catheter, two-balloon catheter, osmotic dilators) and pharmacological (mifepristone, prostaglandin E2) ones [4, 5]. However, the use of medications in pregnant women with extragenital diseases is not always safe and can be limited due to contraindications or side effects of the medication.
From this point of view, mechanical methods for preparing the cervix for childbirth are relevant [4–7].
The objective of the study is to evaluate the effectiveness of mechanical (osmotic) dilators Dilapan-S and laminaria tents in preparing the cervix for term programmed labor in patients with extragenital pathologies.
Materials and Methods
Design: prospective uncontrolled open-label comparative study in parallel groups.
Study subjects: the study included 57 pregnant women who were hospitalized prenatally in High Risk Pregnancy Department of Krasnoyarsk Interdistrict Clinical Hospital No. 20 named after I.S. Berzon and Krasnoyarsk Interdistrict Maternity Hospital No. 2 from September 2018 to March 2019.
Inclusion criteria were gestational age from 380-6 to 390-4 weeks, the absence of severe extragenital pathology requiring operative delivery, the absence of contraindications for using the method, unripe cervix or insufficiently ripe cervix (according to the Bishop score), informed patient’s consent to participate in the study.
Exclusion criteria were severe preeclampsia, multiple pregnancy, fetal distress, decompensated extragenital pathologies, acute inflammatory diseases of the genital tract at the time of the study, and ripe cervix.
Participants and group distribution: 76 pregnant women were selected to participate in the study; however, 19 patients did not meet the inclusion/exclusion criteria and were not included. Thus, a total of 57 pregnant women took part in the study, of which 32 patients were randomly included in group 1 (main) and 25 women were enrolled in group 2 (control). The random sequence of distribution was provided by a researcher using envelopes with numbers and was not overt until the administration of interventions.
Methods of examination: the condition of the cervix was assessed with the Bishop score before placing and after extracting the dilators; the condition of the fetus during cervical preparation and labor was monitored using cardiotocography.
Methods of treatment: patients of group 1 were treated with three Dilapan-S dilators (4×55 mm), patients of group 2 were administered three laminaria tents according to the instructions for their medical use. Before placing dilators, the vagina and cervix were cleansed with an antiseptic solution. Dilapan-S dilator rods were wetted with saline solution before placement.
Testable hypothesis: Dilapan-S dilators are more effective than laminaria tents in preparing the cervix for labor using the criterion of the Bishop score.
The evaluation of the effectiveness of preparing cervix for labor was based on the primary results, namely the degree of the cervix ripening according to the Bishop score after extracting the dilators. Secondary outcomes included the period of time from the moment of extracting the dilator till the onset of labor, duration of labor, the course of labor (vaginal/operative), the condition of the newborn at one and five minutes after the baby was born using the Apgar scale, side effects when using the dilators (local discomfort/pain when placing the dilators, bleeding from the cervical canal, signs of chorioamnionitis and intraamniotic infection of the fetus, uterine hyperstimulation with/without signs of fetal distress according to cardiotocography). To increase the accuracy of the assessment, the researchers were trained to evaluate clinical outcomes.
Statistical data processing was performed using the Statistica 6.0 software package. When analyzing quantitative parameters, the normal distribution was checked, and the arithmetic mean (M) and standard deviation (SD) were calculated. The statistical significance of the differences between the two average indicators was assessed using the Student’s t-test. For quantitative (ordinal) parameters, the median value (Me) and interquartile range (Q1 : Q3) were calculated. The statistical significance of differences between the two median values was assessed using the Mann-Whitney test for intergroup comparison, the difference during the observation within the group was assessed using the Wilcoxon test. The differences were considered statistically significant at the level of p≤0.05. When evaluating qualitative indicators, the actual and percentage frequency of observations were calculated (abs., %). The study of correlation between pairs of qualitative parameters was carried out by analyzing binary contingency tables with the calculation of the Pearson criterion (χ2). Yates continuity correction was applied for contingency tables with low frequencies (less than 10). The relative risk (RR) was defined as the probability of a positive event that could occur in individuals who were exposed to a treatment factor in the study group, in relation to the comparison group. If the RR values exceeded 1, the factor was considered to increase the frequency of positive outcomes (direct correlation); if the RR values were less than 1, it decreased (feedback). If the confidence interval (CI) did not include 1, the differences between the groups according to the studied binary parameter were considered statistically significant with an error probability of p<0.05.
Results
The average age of patients was 27.6 (5.5) and 29.1 (5.2) years in groups 1 and 2, respectively (p=0.84).
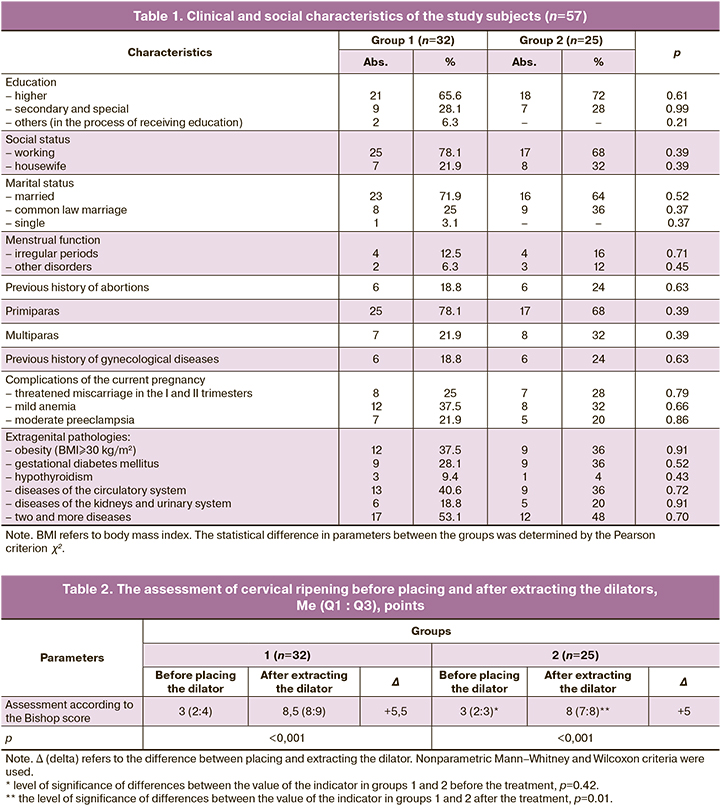
When the patients were included in the study, the gestational age was 38.4 (0.67) and 38.8 (0.58) weeks (p=0.65), respectively. The groups did not show statistically significant differences in age, education, social status, marital status, obstetric and gynecological history, somatic diseases, and body mass index (Table 1).
Among the patients with extragenital diseases, endocrinopathy was observed most frequently: 75 and 76% (24/32 and 19/25), as well as the diseases of the circulatory system 40.6 and 36% (13/32 and 9/25), respectively, which were the indications for induction of labor at 38-39 weeks.
The initial condition of the cervix in patients of both groups was comparable and did not have a statistically significant difference between them (Table 2).
The duration of the dilators placement period in situ was 22.3 (3.6) hours in group 1 and 24.3 (4.6) hours in group 2 (p=0.73).
When the action of Dilapan-S dilator finished, the degree of cervical ripening according to the Bishop score (Table 2) reached a median value of 8.5 (Q1 8 : Q3 9) points, which was statistically significantly higher than the initial level (p<0.001) and it was statistically significantly higher than in group 2 (p=0.01), where the median value of the indicator was noted at the level of Me 8 (Q1 7 : Q3 8) points after the dilators.
The number of patients who used Dilapan-S dilator and reached cervical ripening according to the Bishop score (≥8 points) [3] did not have a statistically significant difference in comparison with those who used laminaria tents and was 87.5% (28/32) versus 64% (16/25), respectively (RR=1.6; 95% CI: 1.08-2.27; p=0.08 using the Pearson criterion χ2 with the Yates correction).
The use of Dilapan-S dilator contributed to the onset of spontaneous labor in 46.9% (15/32) of patients, which was 2.4 times higher than in the control group, where the onset of spontaneous labor was observed only in 20% (5/25) of patients, but the difference was not statistically significant (RR=2.3; 95% CI: 0.99-5.57; p=0.07).
The duration of labor was 12 hours from the moment of dilator extraction in 18.8% (6/32) of patients in group 1 and 4% (1/25) of patients in group 2 (RR=4.7; 95% CI: 0.6-36.5; p=0.12) and it was 12–48 hours in 28.1% (9/32) and 16% (4/25) of patients, respectively (RR=1.76; 95% CI: 0.61-5.05; p=0.35). After extracting the dilator, it was possible to follow wait-and-see strategy within 24–48 hours due to the compensation for extragenital pathology and the absence of patients with obstetric complications (severe preeclampsia, fetal distress) requiring active tactics (transition to the second stage of preinduction).
The results of the cervical assessment obtained during the study indicated that the number of patients who needed amniotomy (due to the ripe cervix) did not differ between the groups and amounted to 40.6% (13/32) and 44% (11/25), respectively (RR=0.9; 95% CI: 0.5–1.7; p=0.99).
Cervical ripening was unsuccessful in group 1 in 12.5% (4/32) of patients compared to group 2 with 36% (9/25) of patients (RR=0.4; 95% CI: 0.14–1.16; p=0.08). These patients were subsequently treated with medications for preparing the cervix or performed operative delivery (Table 3).
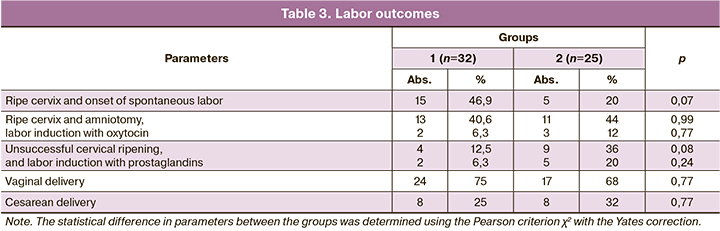
The duration of labor for more than 24 hours was not observed in any group. The average duration of labor in patients of groups 1 and 2 was 483.6±58.4 and 529.8±44.5 minutes, respectively (p=0.53).
Among the patients with spontaneous onset of labor, vaginal delivery was noted in 86.7% (13/15) of cases in group 1 and in 80% (4/5) of patients in group 2 (RR=1.1; 95% CI: 0.67–1.75; p=0.72). Poor progress in labor was observed in 13.3% (2/15) and 20% (1/5) of patients, respectively; they were performed operative delivery (p=0.72). Amniotomy was done in 76.5% (13/17) and 55% (11/20) of cases, respectively, due to the absence of spontaneous onset labor and the presence of the ripe cervix (p=0.31). After performing amniotomy, 84.6% (11/13) of patients had spontaneous labor, and 15.4% (2/13) of women underwent induction of labor with oxytocin in group 1; these indicators were 72.7% (8/11) and 27.3% (3/11), respectively, in group 2 (p=0.83).
Operative delivery was performed in 50% (2/4) of patients with unripe cervix in group 1, and the second stage of preinduction of labor with prostaglandins was done in the remaining 50% (2/4) of cases. In group 2, the corresponding indicators were 44.4% (4/9) (p=0.68) and 55.6% (5/9) (p=0.68).
The data obtained during the study showed that most women in group 1 had vaginal delivery, namely 75% (24/32) (Table 3). Cesarean section was performed in 25% (8/32) of cases in group 1, while in group 2 the frequency of operative delivery was 1.3 times higher and was 32% (8/25, p=0.77).
The probability of vaginal delivery in the group of patients treated with Dilapan-S compared to those who used laminaria was the same (RR=1.1; 95% CI: 0.79–1.54; p=0.77), as well as the risk of operative delivery (RR=0.8; 95% CI: 0.34–1.79; p=0.77).
The indications for cesarean section included abnormalities of labor in 6.25% (2/32) of cases in group 1 versus 4% (1/25, p=0.83) of cases in group 2, fetal hypoxia in 9.4% (3/32) versus 8% (2/25, p=0.77) of cases, cephalopelvic disproportion in 3.2% (1/32) versus 4% (1/25, р=0.56) of cases, unsuccessful cervical ripening in 6.3% (2/32) versus 16.0% (4/25, p=0.45), respectively.
The average weight of newborns in mothers of groups 1 and 2 was 3483.3 (321.2) and 3545.1 (386.4) g, respectively (p=0.9). The Apgar score at the first minute of life was Me 8 (Q1 7 : Q3 8) points, at the fifth minute - Me 9 (Q1 8 : Q3 9) points in group 1 and Me 8 (Q1 8 : Q3 8) and Me 9 (Q1 8 : Q3 9) points – in group 2, respectively (p=0.32; p=0.82).
Side effects were rare and manifested as local discomfort during the dilator placement in 3.1% (1/32) and 8% (2/25, p=0.83) of patients in groups 1 and 2, respectively (no pain was observed in any of the patients), and mild spotting in 3.1% (1/32) and 4% (1/25, p=0.56) of patients, respectively. According to cardiotocography, there were no cases of bleeding from the cervical canal, chorionamnionitis and intraamniotic infection of the fetus, hyperstimulation of the uterus with/without fetal distress.
Thus, according to the Bishop score, the effectiveness of Dilapan-S dilators in preinduction and induction of term programmed labor in patients with extragenital pathologies was higher in comparison with the use of laminaria tents if there was no statistically significant difference in secondary outcomes.
Discussion
The mechanism of action of osmotic dilators after their placement in the cervical canal consists in swelling and increasing their diameter due to the hydrophilic properties of the material and moisture absorption, while the rods exert radial pressure on the walls of the canal, resulting in an evenly expanded cervix. At the same time, endogenous prostaglandin is released, which leads to softening and ripening of the cervix [4, 8, 9]. In addition to the mechanisms of cervical ripening described above, the neuroendocrine (Ferguson) reflex contributes to the spontaneous onset of contractions [4].
According to foreign studies, Dilapan-S swells faster up to 3–4 times the original diameter in situ in comparison with laminaria tents and allows you to achieve the dilation of the cervical canal in a shorter time. In this study, there was no difference in the duration of the position in situ of Dilapan-S dilators compared to laminaria tents (p=0.73).
According to the study by Maier J. T. et al., the average period of time from cervical ripening to labor was less than 36 hours when Dilapan-S was used [7], and the data are consistent with the results of our study.
Indicator dynamics of the degree of cervical ripening using the Bishop score in the period between placement and extraction of the dilator was comparable to +3.6 and +5.5 points in the literature and in the present study, respectively; the average duration of Dilapan-S position in situ was 15.4 versus 22.3 hours, as well as the need for induction of labor with prostaglandins was 7 and 6.3%, respectively [6]. Similar indicators on the Bishop score for 12-hour Dilapan-S in situ in the study of O.R. Baev were +3.1 points (in nulliparous women), and in the study of O.G. Pekarev they were +6.7 points [10, 11].
According to some studies, the frequency of vaginal delivery is 60.2% (in multiparous women it is 82.6%) [7], 69.8% [6], 74.6% [12], which is slightly lower or equal to 75% in our study. At the same time, the frequency of spontaneous onset of labor in these studies was 5–10% versus 46.9%, respectively. This may be explained by the difference in gestational age (37–42 versus 38–40 weeks, respectively), the age of participants (29–32.7 versus 27.6 years, respectively), the frequency of cesarean section in the history (9–10 versus 0%, respectively), and the indicators of cervical ripening before the placement of dilators (2 versus 3 points, respectively). The results similar to the present study were obtained in the work of Saad A.F. et al. where the authors noted vaginal delivery in 82.4% (155/188) of patients, while spontaneous delivery was observed in 77.7% (146/188) of patients [13]. At the same time, the initial indicators of participants in the above-mentioned study were close to our study: the age of 25 years, gestational age of 39.0 weeks, and the Bishop score of 3.0; thus, these indicators may correlate to the obtained results.
The results of the present study for the corresponding indicators were also consistent with the results obtained by N.Yu. Katkova et al. [14]. Thus, the researchers noted that when using Dilapan-S, after 24 hours the indicator of cervical ripening was 9.4 points (initially 2.3 points; +7.1), which was significantly higher than one after the use of laminaria tents, which was 6.7 points (initially 2.1; +4.6 points; p=0.04). Spontaneous labor was observed in 39.1% of patients versus 17.9%, respectively (p=0.001). Dilapan-S was effective in 91.2% of patients, including 84.8% of women who had vaginal delivery; however, labor preinduction turned out to be ineffective in every fourth patient who used laminaria tents, and the frequency of vaginal delivery was lower, namely, 60.7% of patients (p=0.001).
The studies confirm that Dilapan-S has a minimal potential for developing abnormalities of labor, including the cases a history of cesarean section, as well as a low rate of side effects [6, 7]; rare side effects were also noted in this study. Similar data are presented in a new review of the Cochrane database (113 studies, 22,373 women) comparing mechanical dilators with pharmacological ones [15]. It has been shown that the use of a mechanical device is more effective than oxytocin induction in women with unripe cervix; mechanical device is equally effective compared to prostaglandins, but has a lower risk of hyperstimulation and other serious complications, both for the mother and the fetus; and it is also preferable from an economic point of view.
Conclusion
The use of osmotic dilators for preinduction and induction of term programmed labor in patients with extragenital pathologies is a preferable method for preparing the cervix for labor. Dilapan-S facilitates cervical ripening more effectively than laminaria tents (p=0.01) in 87.5% of patients and has a good safety profile (it does not affect the condition of the mother, fetus and newborn) in the absence of a statistically significant difference in the rates of induction of labor and its outcomes.
References
- Основные показатели здоровья матери и ребенка, деятельность службы охраны детства и родовспоможения в Российской Федерации. М.: Минздрав РФ, Центральный научно-исследовательский институт организации и информатизации здравоохранения Минздрава РФ; 2019. 169 с. [The main indicators of maternal and child health, the activities of the child welfare and obstetric care service in the Russian Federation / Ministry of Health of the Russian Federation, Central Research Institute of Organization and Informatization of Health of the Ministry of Health of the Russian Federation. Moscow, 2019. 169 p. (in Russian)].
- Савельева Г.М., Сухих Г.Т., Серов В.Н., Радзинский В.Е., ред. Акушерство. Национальное руководство. 2-е изд. М.: ГЭОТАР-Медиа; 2015. 1080 с. [Savelyeva G.M., Sukhikh G.T., Serov V.N., Radzinsky V.E., Ed. Obstetrics: national leadership / 2nd edition, revised. and add. GEOTAR-Media, 2015. 1080 p. (in Russian)].
- Серов В.Н., Шмаков Р.Г., Баев О.Р., Румянцева В.П., Долгушина Н.В., Клименченко Н.И., Ходжаева З.С., Тетруашвили Н.К., Кан Н.Е., Тютюнник В.Л., Краснопольский В.И., Логутова Л.С., Петрухин В.А., Коваленко Т.С., Башмакова Н.В., Мальгина Г.Б., Ерофеев Е.Н., Зазерская И.Е., Осипова Н.А., Михайлова М.В. и др. Медикаментозная подготовка шейки матки к родам и родовозбуждение. Клинические рекомендации. Акушерство и гинекология. 2015; Приложение 5: 1–14. [Serov V.N., Shmakov R.G., Baev O.R., Rumyantseva V.P., Dolgushina N.V., Klimenchenko N.I., Khojaeva Z.S., Tetruashvili N.K., Kan N.E., Tyutyunnik V.L. et al. Drug preparation of the cervix for childbirth and labor excitement. Clinical recommendations. Akusherstvo i ginekologiya / Obstetrics and gynecology. 2015; 5: 1–14. (in Russian)].
- Дикке Г.Б. Сравнительная оценка современных методов подготовки шейки матки к хирургическому аборту и индукции родов. Акушерство и гинекология. 2017; 9: 12–9. [Dikke G.B. Comparative evaluation of moden methods of preparing the cervix for surgical abortion and induction of labor. Akusherstvo i ginekologiya / Obstetrics and gynecology. 2017; 9: 12–9. (in Russian)]. https://dx.doi.org/10.18565/aig.2017.9.12-9.
- Durie D., Lawal A., Zegelbone P. Other mechanical methods for pre-induction cervical ripening. Semin. Perinatol. 2015; 39(6): 444–9.https://dx.doi.org/10.1053/j.semperi.2015.07.006.
- Gupta J., Chodankar R., Baev O., Bahlmann F., Brega E., Gala A. et al. Synthetic osmotic dilators in the induction of labor – An International Multicentre Observational Study. Eur. J. Obstet. Gynecol. Reprod. Biol. 2018; 229: 70–5. https://dx.doi.org/10.1016/j.ejogrb.2018.08.004.
- Maier J.T., Schalinski E., Gauger U., Hellmeyer L. Cervical ripening with an osmotic dilator (Dilapan-S) in term pregnancies – An Observational Study. J. Gynecol. Neonatal Biol. 2015; 1(2): 55–60. 10.15436/2380-5595.15.015.
- Mahendroo M. Cervical remodeling in term and preterm birth: insights from an animal model. Reproduction. 2012; 143(4): 429–38. https://dx.doi.org/10.1530/REP-11-0466.
- Package Labeling: Dilapan-S™ Hygroscopic Cervical Dilator: Indications for Use. JCECCo. (KendallPark, NJ, UnitedStates); 2012.
- Baev O.R., Babich D.A., Prikhodko A.M., Tysyachniy O.V., Sukhikh G.T. A comparison between labor induction with only Dilapan-S and a combination of mifepristone and Dilapan-S in nulliparous women: a prospective pilot study. J. Matern. Fetal Neonatal Med. 2019; Oct. 1: 1–6. Online ahead of print. https://dx.doi.org/10.1080/14767058.2019.1671340.
- Пекарев О.Г., Брега Е.С., Луньков С.С., Гус А.И. Клинико-эластографическая оценка вариантов подготовки незрелой шейки матки к родам. Доктор.Ру. 2019; 11: 22–8. [Pekarev O.G., Brega E.S., Lun’kov S.S., Gus A.I. Clinical and Elastographic evaluation of methods for ripening an unripe cervix. Doctor.ru. 2019; 11: 22–8. [in Russian]. https://dx.doi.org/10.31550/1727-2378-2019-166-11-22-28.
- Shindo R., Aoki S., Yonemoto N., Yamamoto Y., Kasai J., Kasai M., Miyagi E. Hygroscopic dilators vs balloon catheter ripening of the cervix for induction of labor in nulliparous women at term: Retrospective study. PLoS One. 2017; 12(12): e0189665. https://dx.doi.org/10.1371/journal.pone.0189665.
- Saad A.F., Villarreal J., Eid J., Spencer N., Ellis V., Hankins G.D., Saade G.R. A randomized controlled trial of Dilapan-S vs Foley balloon for preinduction cervical ripening (DILAFOL trial). Am. J. Obstet. Gynecol. 2019; 220: 275. e1-9. https://dx.doi.org/10.1016/j.ajog.2019.01.008.
- Каткова Н.Ю., Бодрикова О.И., Шевалдина С.А., Покусаева К.Б., Безрукова И.М., Лебедева Н.В., Рыжова Н.К. Подготовка шейки матки к родам: кому, когда, чем. Эффективная фармакотерапия. 2017; 26: 26–31. [Katkova N.Yu., Bodrikova O.I., Shevaldina S.A., Pokusaeva K.B., Bezrukova I.M., Lebedeva N.V., Ryzhova N.K. Preparation of the cervix for childbirth: to whom, when, what. Effektivnaya farmakoterapiya / Effective pharmacotherapy. 2017; 26: 26–31 (in Russian)].
- de Vaan M.D., Ten Eikelder M.L., Jozwiak M., Palmer K.R., Davies-Tuck M., Bloemenkamp K.W. et al. Mechanical methods for induction of labor. Cochrane Database Syst. Rev. 2019; (10): CD001233. https://dx.doi.org/10.1002/14651858.CD001233.pub3.
Received 18.05.2020
Accepted 24.07.2020
About the Authors
Ekaterina V. Shaposhnikova, PhD, Associate Professors Department of Obstetrics and Gynaecology of FPK and PPS Krasnoyarsk State Medical University prof. V.F. Voyno-Yasenetsky, Krasnoyarsk. Tel: +7(391)264-29-83. E-mail: catrinaek@yandex.ru. ORCID: 0000-0001-8068-0699. 660022, Russia, Krasnoyarsk, Partizana Zeleznyaka str., 1.Galina B. Dikke, MD, Associate professor, Professor of the Department of Obstetrics and Gynecology with a course of reproductive medicine. Academy of Medical Education named F.I. Inozemtsev, St. Petersburg. Tel.: +7(812)334-76-50. E-mail: galadikke@yandex.ru. ORCID: 0000-0001-9524-8962 190013.
190013, Russia, St. Petersburg, Moscow Ave., 22, letter M.
Marina I. Bazina, MD, Associate Professors, the head of the Department of Obstetrics and Gynaecology of FPK and PPS Krasnoyarsk State Medical University
prof. V.F. Voyno-Yasenetsky, Krasnoyarsk. Tel: +7(391)264-29-83. E-mail: sonya189@mail.ru. ORCID: 0000-0002-1971-632X.
660022, Russia, Krasnoyarsk, Partizana Zeleznyaka str., 1.
Vitalii B. Tskhay, MD, The head of the Department of Perinatology, Obstetrics and Gynaecology of Krasnoyarsk State Medical University prof. V.F. Voyno-Yasenetsky, Krasnoyarsk. Tel: +7(391)265-35-84. E-mail: tchai@yandex.ru. ORCID: 0000-0003-2228-3884. 660022, Russia, Krasnoyarsk, Partizana Zeleznyaka str., 1.
Antonina T. Egorova, MD, Professors of the Department of Obstetrics and Gynaecology of FPK and PPS Krasnoyarsk State Medical University prof. V.F. Voyno-Yasenetsky, Krasnoyarsk. Tel: +7(391)236-06-21. E-mail: sledopyt.tonya@gmail.com. ORCID: 0000-0002-0160-8857. 660022, Russia, Krasnoyarsk, Partizana Zeleznyaka str., 1.
Marina M. Mentsik, the Head of the maternity hospital of Krasnoyarsk interdistrict city hospital №20 named after I.S. Berzona, Krasnoyarsk.
Tel: +7(391)264-29-57. E-mail: roddomgkb20@mail.ru. 660123, Russia, Krasnoyarsk, Instrumentalnya str., 12.
Elena P. Tsaryuk, the Head of the Krasnoyarsk Interdistrict Maternity Hospital No. 2, Krasnoyarsk. Tel.: +7(391)236-36-32. E-mail: KMRD2@yandex.ru.
660093, Russia, Krasnoyarsk, Krasnoyarskiy Rabochiy Ave., 170.
Natalia V. Zirova, PhD, Associate Professors Department of Obstetrics and Gynaecology of FPK and PPS Krasnoyarsk State Medical University prof. V.F. Voyno-Yasenetsky, Krasnoyarsk. Tel: +7(391)236-06-21. E-mail: meduniver10@mail.ru. ORCID: 0000-0002-9501-8179. 660022, Russia, Krasnoyarsk, Partizana Zeleznyaka str., 1.
For citation: Shaposhnikova E.V., Dikke G.B., Bazina M.I., Tskhai V.B., Egorova A.T., Mentsik M.M., Tsaryuk E.P., Zhirova N.V. Comparative evaluation of mechanical methods for preparing the cervix for induction of labor in pregnant women with extragenital pathologies.
Akusherstvo i Ginekologiya / Obstetrics and gynecology. 2020; 8: 88-94 (in Russian)
https://dx.doi.org/10.18565/aig.2020.8.88-94