Evaluation of the course of clinical symptoms and reproductive outcomes after laser drilling of the uterus with a holmium laser in patients of reproductive age
Ishchenko A.I., Ishchenko A.A., Zuev V.M., Gadaeva I.V., Malyuta E.G., Dzhibladze T.A., Isaev M.P., Obosyan L.B., Khokhlova I.D., Minashkina E.V., Tevlina E.V., Verbitsky M.V.
Adenomyosis is a medical and social problem associated not only with a deterioration in the quality of life of reproductive and perimenopausal women, but is also one of the causes of infertility and miscarriage in young patients.
Objective: To evaluate the course of clinical symptoms and reproductive outcomes after laser drilling of the uterus with a holmium laser in patients of reproductive age.
Materials and methods: The study included 470 patients with uterine factor infertility due to diffuse and/or nodular adenomyosis Grade 2 and Grade 2–3 (MUSA 2022), treated during the period of 2000–2024. The patients underwent laser drilling of the uterus with a holmium laser using a laparoscopic approach.
Results: During the follow-up period after organ-preserving surgery, clinical symptoms and reproductive outcomes were assessed. Ultrasound and MRI were used to objectify the data. Six months after surgery most patients demonstrated a significant reduction in the severity of dysmenorrhea (from 8.10 to 2.0 according to the NRS scale). Menstrual blood loss also markedly decreased from 153.1 (80) ml to 67.0 ml. Pregnancy occurred in 127/337 patients under the follow-up. No intra- or postoperative complications were noted.
Conclusion: The obtained data demonstrate a significant improvement in clinical symptoms (decrease in the severity of dysmenorrhea, menstrual blood loss, and uterine size) in patients with adenomyosis. Reproductive outcomes also improved, which did not show statistical significance after Bonferroni correction, therefore requiring further confirmation with control groups.
Authors’ contributions: Ishchenko A.I., Zuev V.M., Isaev M.P. – study concept and design; Dzhibladze T.A., Ishchenko A.A., Obosyan L.B., Malyuta E.G., Minashkina E.V., Gadaeva I.V. – material collection and processing; Obosyan L.B., Tevlina E.V., Verbitsky M.V. – statistical data processing; Obosyan L.B., Gadaeva I.V., Dzhibladze T.A. – text composition; Khokhlova I.D., Gadaeva I.V. – text editing.
Conflicts of interest: The authors declare no conflicts of interest.
Funding: The study had no sponsorship.
Ethical Approval: The study was reviewed and approved by the Ethics Committee of the I.M. Sechenov First Moscow State Medical University, Ministry of Health of Russia (Sechenov University).
Patient Consent for Publication: All patients provided informed consent for the publication of their data.
Authors' Data Sharing Statement: The data supporting the findings of this study are available on request from the corresponding author after approval from the principal investigator.
For citation: Ishchenko A.I., Ishchenko A.A., Zuev V.M., Gadaeva I.V., Malyuta E.G., Dzhibladze T.A., Isaev M.P., Obosyan L.B., Khokhlova I.D., Minashkina E.V., Tevlina E.V., Verbitsky M.V. Evaluation
of the course of clinical symptoms and reproductive outcomes after laser drilling of
the uterus with a holmium laser in patients of reproductive age.
Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2025; (10): 107-116 (in Russian)
https://dx.doi.org/10.18565/aig.2025.195
Keywords
Adenomyosis remains one of the significant medical and social problems, especially in women with preserved menstrual function, negatively affecting fertility, which often requires the use of assisted reproductive technologies (ART) [1–5]. Despite the advances achieved in the study of etiopathogenetic mechanisms, including molecular genetic aspects, the treatment of adenomyosis remains controversial for women of reproductive age and needs further research [6].
The most informative diagnostic methods for adenomyosis include transvaginal ultrasound (TVUS), magnetic resonance imaging (MRI), and hysteroscopy followed by histological examination of biopsy specimens. The widespread adoption of modern diagnostic methods allows for the more frequent detection of adenomyosis in women of reproductive age, including patients with abnormal uterine bleeding, infertility, pelvic pain, as well as in asymptomatic women [6–9].
This pathological process is considered a specific component in the PALM-COEIN FIGO classification, used to reveal the causes of abnormal uterine bleeding [10]. According to the results of many studies, adenomyosis reduces endometrial receptivity, which, in turn, leads to infertility and an increased risk of spontaneous miscarriages [2, 11–14]. Medical treatment is usually temporary and symptomatic and is recommended for patients who wish to preserve their uterus and are not planning pregnancy. Hysterectomy is considered to be a standard surgical treatment for adenomyosis, but it does not preserve fertility [15, 16]. Organ-preserving surgery is a promising treatment option for adenomyosis to preserve and restore fertility, but there are currently insufficient well-designed clinical trials evaluating the impact of such surgeries on reproductive outcomes.
Advances in laser technology and fiber optics have enabled a fundamentally new approach to treating adenomyosis in reproductive patients. Therefore, the improvement and implementation of new high-tech treatment methods remain relevant. We have strengthened the technique for performing interstitial laser-induced destruction (ILID) of adenomyosis using a Ho:YAG laser system and a fiber-optic catheter with a cylindrical scattering tip. The holmium laser (Ho:YAG – Holmium:yttrium-aluminum-garnet – an abbreviation for the active medium yttrium-aluminum-garnet activated by holmium ions) is a solid-state pulsed laser (ULHK-03 unit, TRIPLE-X series) with a wavelength of 2.09 μm (2088 nm) and a peak power of up to 10 kW, which, due to the pulsed mode, causes evaporation (ablation) of biological tissue [17]. Thanks to the minimal penetration depth (0.4 mm), the Ho:YAG laser affects precisely the point of application, without damaging the surrounding tissue [18].
The evidence base for laser drilling of the adenomyotic uterus remains limited. Existing studies are uncontrolled observational case series, which precludes drawing conclusions on the effectiveness of this intervention compared to other methods.
The present study aims to evaluate the effect of laser destruction of pathological foci of adenomyosis in improving reproductive parameters in patients with infertility, as well as in reducing the severity of clinical manifestations such as dysmenorrhea and abnormal uterine bleeding, while maintaining the integrity of the endometrium and unaffected areas of the myometrium.
The objective is to evaluate the course of clinical symptoms and reproductive outcomes after laser drilling of the uterus with a holmium laser in patients of reproductive age.
Materials and methods
Study design, participants and sampling size
This retrospective uncontrolled interventional single-group study (before-after type) was conducted at the Department of Obstetrics and Gynecology No. 1 of the N.V. Sklifosovsky Institute of Cardiology, at the V.F. Snegirev Clinic of Obstetrics and Gynecology of Sechenov University and the Gynecology Department of the National Medical Research Center for Treatment and Rehabilitation. The study included 470 patients with uterine factor infertility due to the diffuse and/or nodular adenomyosis Grade 2 and Grade 2–3 (MUSA 2022), treated during the period of 2000-2024. The diagnosis was proved based on complaints, a gynecological examination, pelvic ultrasound results, and, in some cases, MRI. We considered TVUS as an initial instrumental, minimally invasive diagnostic method. The signs of adenomyosis were determined according to the MUSA 2022 Consensus: a zone of increased echogenicity of a round or oval shape, the presence of anechoic areas or cystic cavities with a fine-dispersed suspension solids in the myometrium, hyperechoic islands, fan-shaped shadows, echogenic subendometrial lines/rudiments, an increase in the anteroposterior size of the uterus, asymmetric thickening of the uterine walls, an interrupted and irregular transition zone, and a round-shaped uterus [19]. All patients underwent ultrasound examination of the pelvic organs, during which the adenomyosis was confirmed, and to clarify the stage of the disease MRI was required in 30 patients.
The patients' age ranged 35–48 years, with an average of 42 years.
Data collection
All information was extracted from archives of medical and birth histories; we also used electronic medical record databases. Social and demographic data, including age, were recorded. Inclusion criteria for the study: proven diagnosis of primary or secondary infertility; abnormal uterine bleeding; severe dysmenorrhea (Pain Score on Numerical Rating Scale [NRS] ≥ 6) that negatively impacts quality of life; patients with adenomyosis as the primary cause of implantation failure following more than two attempts of fresh/cryo embryo transfer after in vitro fertilization (IVF). Exclusion criteria: patients with combined pathology of the uterus and its adnexa; somatically burdened patients other than iron deficiency anemia; women with failure to conceive after treatment with gonadotropin-releasing hormone agonists.
The primary endpoints were: changes in the intensity of dysmenorrhea (based on the NRS scale) and changes in the volume of menstrual blood loss. Secondary endpoints included: the confirmed pregnancy occurred during the observation period (verified by the beta-hCG test, as well as by ultrasound data confirming the presence of one or more yolk sacs, or by final clinical signs of pregnancy), the presence/absence of intra- and postoperative complications.
Surgical technique
Uterine laser drilling using a holmium laser (Ho:YAG) for the treatment of adenomyosis is performed laparoscopically. After inserting the laparoscope and necessary instruments, the affected areas of the uterus are identified both by eye and using intraoperative ultrasound. Uterine drilling was performed using a Ho:YAG laser with an average power of 20 W, model “ULHK-04 Compact” (OOO MedOptoTech, Russia). Laser radiation was conducted by a flexible quartz light guide with a free outlet and a diameter of 400 μm. The light guide was passed through the working channel of the aquapurator and applied directly to the pathological lesion. The holmium laser has a wavelength of 2.09 µm and an absorption coefficient of 40 cm-1 in water. The holmium laser has a pulsed operating mode: the pulse duration is 300–600 μs, the pulse repetition frequency is in the range from 5 to 15 Hz, the energy of the output radiation was 1.5–3.0 J, the depth of surgical exposure for the diffuse form of adenomyosis of grade 2 was no more than 1–2 cm, and for the nodular form – 0.2–0.4 mm. 10 to 20 channels were formed in a focused manner in the fundus, along the anterior and posterior walls of the uterus using a Ho:YAG laser under ultrasound control, depending on the location of the foci and nodes of adenomyosis, and the myometrium was irradiated with laser radiation through each channel for 15–30 s (Fig. 1).

The procedure was monitored in real time with intraoperative ultrasound navigation, allowing for precise adjustment of the depth and width of the laser beam, minimizing damage to surrounding healthy tissue. Upon completion of the procedure, the operative time, bleeding volume, and possible complications were recorded.
Relief from menorrhagia and dysmenorrhea symptoms was assessed clinically and using the NRS scale, respectively. Ultrasound and/or MRI were used to confirm adenomyosis remission.
Participants could try to conceive 6–9 months after the intervention. The method for achieving pregnancy was chosen by the patient, including both natural and ART methods.
Statistical analysis
All collected data were systematized and analyzed using statistical methods to identify possible relationships and patterns. Statistical analysis was done using StatTech v. 4.8.1 software (StatTech LLC, Russia). Quantitative indicators were assessed for compliance with a normal distribution with the use of the Kolmogorov–Smirnov test. Quantitative indicators with a normal sample distribution were described using arithmetic means (M) and standard deviations (SD). Results are presented in M (SD) format.
To analyze changes in pre-post variables, a paired t-test (for normal distribution) or a Wilcoxon test (for non-normal distribution) were used. Additionally, the variation (Δ = post – pre), 95% confidence interval (CI) of Δ, p-value, and effect size (Cohen's dz or r) were calculated. When comparing more than two independent groups based on categorical characteristics, the Pearson χ² test was used. To clarify differences between groups, pairwise comparisons were performed with a Bonferroni correction; a new critical significance level was identified by dividing 0.05 by the number of comparisons (e.g., for three groups, p<0.017).
In cases where normal distribution was not observed, quantitative data were described using the median (Me) and lower and upper quartiles (Q1–Q3). Categorical data were described using absolute values and percentages. 95% CI for percentages was calculated using the Clopper–Pearson interval.
Ethics Committee and data confidentiality
The study was approved by the local ethics committee of the I.M. Sechenov First Moscow State Medical University, Ministry of Health of Russia (Sechenov University). Written informed consent was obtained from all participants.
Results
Clinical and surgical outcomes
In this retrospective study we analyzed the treatment outcomes of 470 patients who underwent interstitial laser-induced destruction (ILID) using holmium laser. The clinical data of the patients are presented in Table 1. The mean patient age was 42 years, and the mean duration of infertility accounted for 67.0 (95% CI 31.00–101.00) months. Postoperative complications were not recorded in any case.
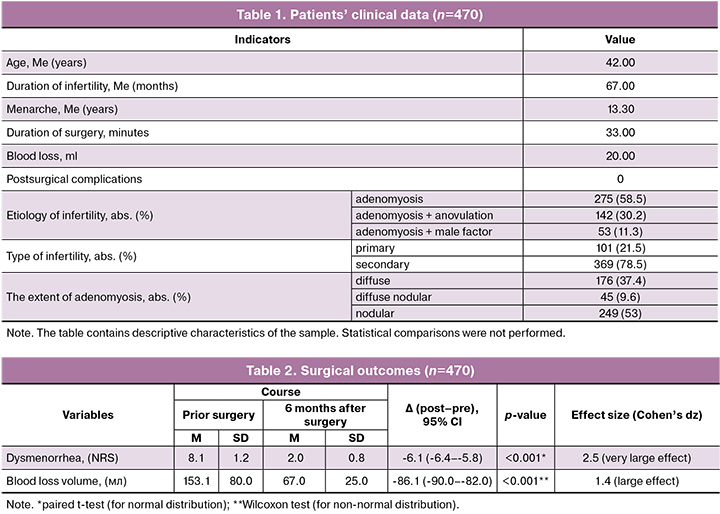
Six months after surgery most patients experienced a significant reduction in the severity of dysmenorrhea. NRS scores decreased from 8.1 (1.2) to 2.0 (0.8); Δ=-6.1 (95% CI -6.4–-5.8), p<0.001, Cohen’s dz=2.5 (very large effect) (Table 2).
The volume of menstrual blood loss also significantly decreased: from 153.1 (80.0) ml to 67.0 (25.0) ml; Δ=-86.1 (95% CI -90.0–-82.0), p<0.001, Cohen’s dz=1.4 (large effect) (Table 2).
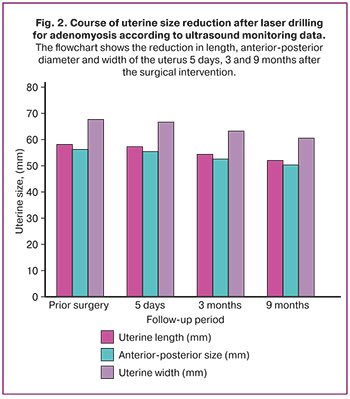
Series of ultrasound scan of uterine size revealed a significant trend toward its reduction, indicating a positive effect of the intervention. The studies were conducted during the period of 9 months after surgery (Table 3, Fig. 2). Figure 3 shows ultrasound images before and after laser drilling, demonstrating regression of pathological changes.
The presented data confirm the effectiveness of ILID and its impact on the improvement of uterine anatomical parameters, which, in turn, contributed to improved clinical outcomes in patients. The obtained results demonstrate the high clinical efficacy of this technique in reducing the severity of adenomyosis symptoms and normalizing menstrual function.
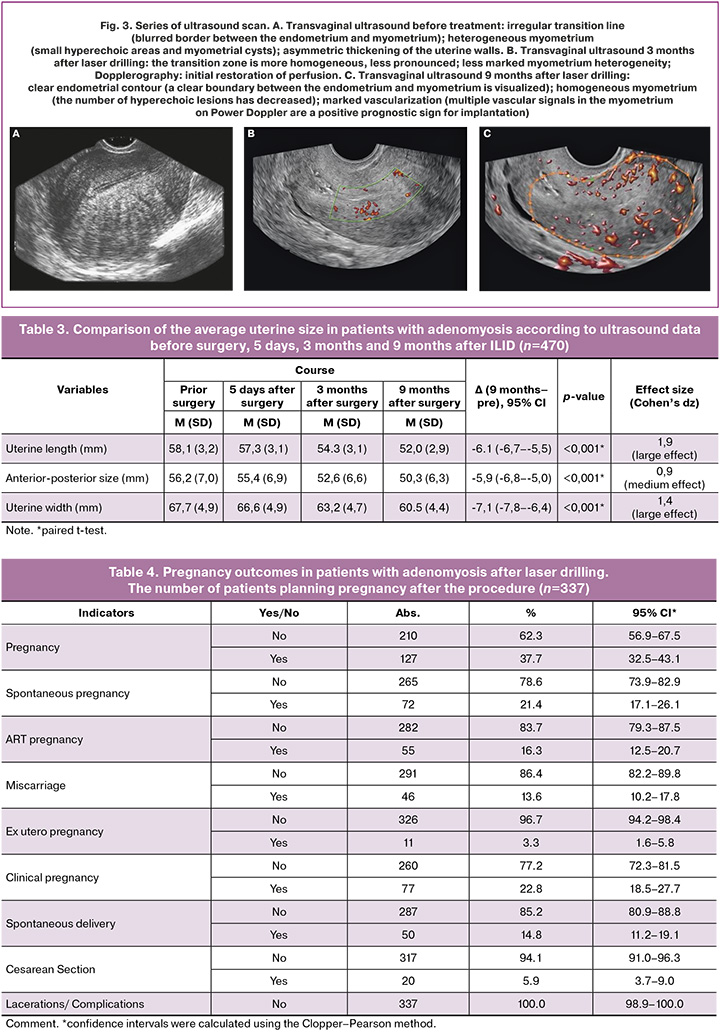
Reproductive outcomes
Data on reproductive status were available for 337 patients, while the same data for 133 patients were lost. Among patients with available information, pregnancy was recorded in 127/337 (37.7%). Pregnancy occurred both spontaneously (n=72) and using ART (n=55). The spontaneous abortion rate accounted for 13.6%, and the ectopic pregnancy rate was 3.3%. Clinical pregnancy was confirmed in 77 patients (22.8%), all of whom delivered in term. Spontaneous deliveries were recorded in 50 patients (14.8%), and cesarean sections for obstetric indications were performed in 20 women (5.9%). The course of pregnancy, childbirth, and the postpartum period were uneventful in all patients. Pregnancy outcomes are presented in Table 4. Second and third pregnancies were registered in 97 women throughout the follow-up period.
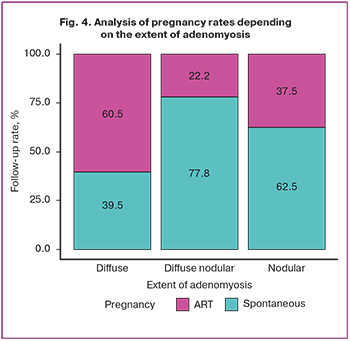
The analysis of the relationship between the pregnancy rate in 127 patients and the degree of adenomyosis spread after treatment was conducted in a group of patients with infertility associated only with adenomyosis (Table 5, Fig. 4). Among the patients who achieved spontaneous pregnancy, 50 had the nodular form of Grade 2 adenomyosis, 15 had the diffuse form of the same degree, and 7 patients had the diffuse-nodular form of Grades 2–3 adenomyosis. The remaining 55 patients became pregnant with the help of ART methods, of which 30 had the nodular form of Grade 2 adenomyosis, 23 had diffuse form, and only 2 had the diffuse nodular form of Grades 2–3 adenomyosis.
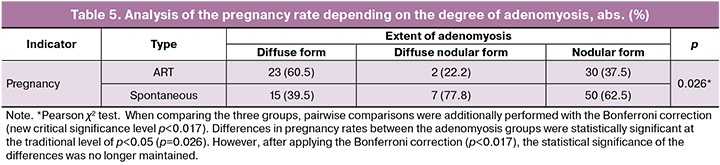
ILID using a Ho:YAG laser is associated with improved clinical parameters (pain reduction, blood loss, and uterine size). Regarding reproductive outcomes, differences between adenomyosis groups had no statistical significance after Bonferroni correction, requiring further studies on larger samples to clarify the factors influencing conception success and reducing pregnancy risks.
Discussion
Laser destruction of adenomyosis lesions demonstrated its effectiveness in reducing such severe symptoms as dysmenorrhea and abnormal uterine bleeding. This aspect of treatment is important, as a marked improvement in patients' quality of life can serve as a key indicator of the success of the procedure. However, for a more accurate assessment, it is necessary to consider many factors, such as patient's age, extent of pathological process and presence of comorbidities.
There are studies dedicated to other organ-sparing methods in patients with adenomyosis, for example, uterine artery embolization. However, when analyzing the results obtained, in most cases they were limited only to the relief of menstrual symptoms. Uterine artery embolization is considered to be an effective treatment for heavy menstrual bleeding and pain associated with adenomyosis. This treatment is typical for patients who are not planning pregnancy anymore and wish to preserve their uterus. Non-invasive thermal ablation procedures such as high-intensity focused ultrasound, radiofrequency ablation and percutaneous microwave ablation can be used as treatment options for symptomatic adenomyosis, but are quite time-consuming and expensive. In addition, they cause certain complications (severe pain, burns of underlying tissues and organs) [20], since there is no precise anatomical navigation and certain application points. Adenomyomectomy (Osada procedure) is an effective treatment option for symptomatic adenomyosis, although it should be noted that this procedure can lead to significant perioperative complications, such as uterine rupture during pregnancy [21, 22]. The relationship between surgery for adenomyosis and fertility and pregnancy outcomes in diffuse adenomyosis is still not completely investigated [23, 24]. Several prospective studies have recently reported varying pregnancy rates after adenomyosis excision: 14.3% (2/14), 2.3% (2/86), 30% (21/70), and 40.8% (56/137) [25–28]. The results of a recent meta-analysis by Jiang L. et al. [29] demonstrated that excisional therapy may be an effective treatment option for patients with symptomatic adenomyosis and infertility for several years or repeated ART failures, while non-excisional methods (high-intensity ultrasound, microwave ablation, radiofrequency ablation) can probably become specific for the treatment of infertility associated with adenomyosis: pregnancy, miscarriage, and live birth rates were 40% (95% CI 29–52), 21% (95% CI 16–27), and 70% (95% CI 64–76), respectively, after excisional therapy; for non-excisional therapy, these rates were 51% (95% CI 42–60), 22% (95% CI 13–34), and 71% (95% CI 57–83). Differences between methods were not statistically significant.
In our study pregnancy was documented in 37.7% (127/337) of patients after intraoperative laser thermal destruction using a holmium laser. However, this pregnancy rate should be interpreted solely as a descriptive characteristic of the sample. Given the lack of a control group and randomization, we cannot rule out the fact that a similar rate could have been observed without the procedure or with other treatment methods.
During our study no complications were recorded, either in the intra- or postoperative periods or during pregnancy, childbirth, or the postpartum period. In a systematic review conducted by Tan J. et al. [30], uterine rupture was detected in 6.8% of pregnant women with diffuse adenomyosis after surgery.
A retrospective analysis of our study showed that laser destruction of adenomyosis lesions is highly accurate, therefore minimizing the risk of damage to healthy uterine tissue. This is achieved through the strong absorption of 2.09 µm wavelength radiation in biological tissue, ensuring maximum absorption in water. The shallow penetration depth (0.4 mm) allows for precise control of the depth and extent of thermal damage. Its hemostatic effect involves "twisting" vessels up to 0.5 mm, which eliminates the risk of thrombus detachment and reduces the likelihood of microembolism and delayed hemorrhages. This is confirmed by the results of our study, with no complications such as thrombosis, thromboembolism, or bleeding in the intra- and postoperative periods.
In addition, the holmium laser has a number of additional advantages that make it a better choice for various surgical interventions. The 2-micron beam of the holmium laser is safe for the eyes, which is especially significant in hospital settings, where the protection of patients and medical staff is of primary importance. Low operating costs significantly reduce treatment expenses, making the technology more accessible to a wider range of patients. Finally, its compact and portable design, along with the absence of fiber burning, ensures ease of use and high treatment efficiency.
Thus, the holmium laser combines safety, cost-effectiveness and utility, making it a preferable tool in modern medicine.
Despite the encouraging results, potential limitations of this study should be taken into account: data loss during follow-up (133 patients, 28.3%) and the retrospective nature of the analysis. This is a single-group “before-after” study without a control group, which significantly limits the ability to draw causal conclusions and may introduce systematic error.
To improve the accuracy and reliability of the conclusion, it is important to conduct further studies aimed at comparing different methods of treating adenomyosis, assessing the risk of recurrence of the disease, and identifying factors that may influence the success of laser destruction.
Conclusion
Our retrospective study, aimed at assessing the course of symptoms and reproductive outcomes after laser destruction of adenomyosis lesions, demonstrated a positive result of the proposed method in reducing the symptoms of the disease. Laser destruction of pathological lesions is a safe and potentially promising treatment for infertility associated with adenomyosis, as it preserves the integrity of the endometrium and unaffected areas of the myometrium, which plays a key role in maintaining reproductive function and increasing the chances of successful conception.
The method we proposed showed beneficial results in reducing the severity of dysmenorrhea and abnormal uterine bleeding, which directly contributes to improving the quality of life of patients.
However, further large-scale, well-controlled prospective studies are needed to better understand the long-term effects and potential complications of laser destruction.
References
- Mavrelos D., Holland T.K., O'Donovan O., Khalil M., Ploumpidis G., Jurkovic D. et al. The impact of adenomyosis on the outcome of IVF-embryo transfer. Reprod. Biomed. Online. 2017; 35(5): 549-54. https://dx.doi.org/10.1016/j.rbmo.2017.06.026
- Dueholm M. Uterine adenomyosis and infertility, review of reproductive outcome after in vitro fertilization and surgery. Acta Obstet. Gynecol. Scand. 2017; 96(6): 715-26. https://dx.doi.org/10.1111/aogs.13158
- Vercellini P., Consonni D., Dridi D., Bracco B., Frattaruolo M.P., Somigliana E. Uterine adenomyosis and in vitro fertilization outcome: a systematic review and meta-analysis. Hum. Reprod. 2014; 29(5): 964-77. https://dx.doi.org/10.1093/humrep/deu041
- Wang P.H., Liu W.M., Fuh J.L., Cheng M.H., Chao H.T. Comparison of surgery alone and combined surgical-medical treatment in the management of symptomatic uterine adenomyoma. Fertil. Steril. 2009; 92(3): 876-85. https://dx.doi.org/10.1016/j.fertnstert.2008.07.1744
- Bourdon M., Santulli P., Oliveira J., Marcellin L., Maignien C., Melka L. et al. Focal adenomyosis is associated with primary infertility. Fertil. Steril. 2020; 114(6): 1271-7. https://dx.doi.org/10.1016/j.fertnstert.2020.06.018
- Chapron C., Vannuccini S., Santulli P., Abrão M.S., Carmona F., Fraser I.S. et al. Diagnosing adenomyosis: an integrated clinical and imaging approach. Hum. Reprod. Update. 2020; 26(3): 392-411. https://dx.doi.org/10.1093/humupd/dmz049
- Bergeron C., Amant F., Ferenczy A. Pathology and physiopathology of adenomyosis. Best Pract. Res. Clin. Obstet. Gynaecol. 2006; 20(4): 511-21. https://dx.doi.org/10.1016/j.bpobgyn.2006.01.016
- Dueholm M., Lundorf E., Hansen E.S., Sørensen J.S., Ledertoug S., Olesen F. Magnetic resonance imaging and transvaginal ultrasonography for the diagnosis of adenomyosis. Fertil. Steril. 2001; 76(3): 588-94. https://dx.doi.org/10.1016/s0015-0282(01)01962-8
- Pinzauti S., Lazzeri L., Tosti C., Centini G., Orlandini C., Luisi S. et al. Transvaginal sonographic features of diffuse adenomyosis in 18-30-year-old nulligravid women without endometriosis: association with symptoms. Ultrasound Obstet. Gynecol. 2015; 46(6): 730-6. https://dx.doi.org/10.1002/uog.14834
- Munro M.G., Critchley H.O.D., Broder M.S., Fraser I.S., FIGO Working Group on Menstrual Disorders. FIGO classification system (PALM-COEIN) for causes of abnormal uterine bleeding in nongravid women of reproductive age. Int. J. Gynaecol. Obstet. 2011; 113(1): 3-13. https://dx.doi.org/10.1016/j.ijgo.2010.11.011
- Cozzolino M., Cosentino M., Loiudice L., Martire F.G., Galliano D., Pellicer A. et al. Impact of adenomyosis on in vitro fertilization outcomes in women undergoing donor oocyte transfers: a prospective observational study. Fertil. Steril. 2024; 121(3): 480-8. https://dx.doi.org/10.1016/j.fertnstert.2023.11.034
- Cozzolino M., Tartaglia S., Pellegrini L., Troiano G., Rizzo G., Petraglia F. The effect of uterine adenomyosis on IVF outcomes: a systematic review and meta-analysis. Reprod. Sci. 2022; 29(11): 3177-93. https://dx.doi.org/10.1007/s43032-021-00818-6
- Li Y.T., Chen S.F., Chang W.H., Wang P.H. Pregnancy outcome in women with type I adenomyosis undergoing adenomyomectomy. Taiwan. J. Obstet. Gynecol. 2021; 60(3): 399-400. https://dx.doi.org/10.1016/j.tjog.2021.03.003
- Juárez-Barber E., Cozzolino M., Corachán A., Alecsandru D., Pellicer N., Pellicer A. et al. Adjustment of progesterone administration after endometrial transcriptomic analysis does not improve reproductive outcomes in women with adenomyosis. Reprod. Biomed. Online. 2023; 46(1): 99-106. https://dx.doi.org/10.1016/j.rbmo.2022.09.007
- Harada T., Taniguchi F., Guo S.W., Choi Y.M., Biberoglu K.O., Tsai S.J.S. et al. The Asian society of endometriosis and adenomyosis guidelines for managing adenomyosis. Reprod. Med. Biol. 2023; 22(1): e12535. https://dx.doi.org/10.1002/rmb2.12535
- Benetti-Pinto C.L., Mira T.A.A. de, Yela D.A., Teatin-Juliato C.R., Brito L.G.O. Pharmacological treatment for symptomatic adenomyosis: a systematic review. Rev. Bras. Ginecol. Obstet. 2019; 41(9): 564-74. https://dx.doi.org/10.1055/s-0039-1695737
- Socarrás M.R., del Álamo J.F., Sancha F.G. Long live holmium! Eur. Urol. Open Sci. 2022; 48: 28-30. https://dx.doi.org/10.1016/j.euros.2022.07.012
- Bhatta N., Isaacson K., Bhatta K.M., Anderson R.R., Schiff I. Comparative study of different laser systems. Fertil. Steril. 1994; 61(4): 581-91. https://dx.doi.org/10.1016/s0015-0282(16)56629-1
- Harmsen M.J., Van den Bosch T., de Leeuw R.A., Dueholm M., Exacoustos C., Valentin L. et al. Consensus on revised definitions of morphological uterus sonographic assessment (MUSA) features of adenomyosis: results of modified Delphi procedure. Ultrasound Obstet. Gynecol. 2022; 60(1): 118-31. https://dx.doi.org/10.1002/uog.24786
- Ищенко А.И., Жуманова Е.Н., Ищенко А.А., Горбенко О.Ю., Чунаева Е.А., Агаджанян Э.С., Савельева Я.С. Современные подходы в диагностике и органосохраняющем лечении аденомиоза. Акушерство, гинекология и репродукция. 2013; 7(3): 30-4. [Ishchenko A.I., Zhumanova E.N., Ishchenko A.A., Gorbenko O.Yu., Chunaeva E.A., Aghajanyan E.S., Savelieva Yа.S. Modern approaches in the diagnosis and conserving therapy of adenomyosis. Obstetrics, Gynecology and Reproduction. 2013; 7(3): 30-4 (in Russian)].
- Dason E.S., Maxim M., Sanders A., Papillon-Smith J., Ng D., Chan C. et al. Guideline No. 437: Diagnosis and Management of Adenomyosis. J. Obstet. Gynaecol. Can. 2023; 45(6): 417-29.e1. https://dx.doi.org/10.1016/j.jogc.2023.04.008
- Selntigia A., Molinaro P., Tartaglia S., Pellicer A., Galliano D., Cozzolino M. Adenomyosis: an update concerning diagnosis, treatment, and fertility. J. Clin. Med. 2024; 13(17): 5224. https://dx.doi.org/10.3390/jcm13175224
- Kim J.K., Shin C.S., Ko Y.B., Nam S.Y., Yim H.S., Lee K.H. Laparoscopic assisted adenomyomectomy using double flap method. Obstet. Gynecol. Sci. 2014; 57(2): 128-35. https://dx.doi.org/10.5468/ogs.2014.57.2.128
- Fujishita A., Masuzaki H., Khan K.N., Kitajima M., Ishimaru T. Modified reduction surgery for adenomyosis. A preliminary report of the transverse H incision technique. Gynecol. Obstet. Invest. 2004; 57(3): 132-8. https://dx.doi.org/10.1159/000075830
- Dai Z., Feng X., Gao L., Huang M. Local excision of uterine adenomyomas: a report of 86 cases with follow-up analyses. Eur. J. Obstet. Gynecol. Reprod. Biol. 2012; 161(1): 84-7. https://dx.doi.org/10.1016/j.ejogrb.2011.11.028
- Saremi A., Bahrami H., Salehian P., Hakak N., Pooladi A. Treatment of adenomyomectomy in women with severe uterine adenomyosis using a novel technique. Reprod. Biomed. Online. 2014; 28(6): 753-60. https://dx.doi.org/10.1016/j.rbmo.2014.02.008
- Takeuchi H., Kitade M., Kikuchi I., Shimanuki H., Kumakiri J., Kitano T. et al. Laparoscopic adenomyomectomy and hysteroplasty: a novel method. J. Minim. Invasive Gynecol. 2006; 13(2): 150-4. https://dx.doi.org/10.1016/j.jmig.2005.12.004
- Zhou Y., Shen L., Wang Y., Yang M., Chen Z., Zhang X. Long-term pregnancy outcomes of patients with diffuse adenomyosis after double-flap adenomyomectomy. J. Clin. Med. 2022; 11(12): 3489. https://dx.doi.org/10.3390/jcm11123489
- Jiang L., Han Y., Song Z., Li Y. Pregnancy outcomes after uterus-sparing operative treatment for adenomyosis: a systematic review and meta-analysis. J. Minim. Invasive Gynecol. 2023; 30(7): 543-54. https://dx.doi.org/10.1016/j.jmig.2023.03.015
- Tan J., Moriarty S., Taskin O., Allaire C., Williams C., Yong P. et al. Reproductive outcomes after fertility-sparing surgery for focal and diffuse adenomyosis: a systematic review. J. Minim. Invasive Gynecol. 2018; 25(4): 608-21. https://dx.doi.org/10.1016/j.jmig.2017.12.020
Received 17.07.2025
Accepted 21.10.2025
About the Authors
Anatoly I. Ishchenko, Dr. Med. Sci., Professor, Professor at the Department of Obstetrics and Gynecology No. 1, Sklifosovsky Institute of Clinical Medicine,I.M. Sechenov First Moscow State Medical University, Ministry of Health of Russia (Sechenov University), 119048, Russia, Moscow, Trubetskaya str., 8, bld. 2,
+7(499)248-69-56, 7205502@mail.ru, https://orcid.org/0000-0003-3338-1113
Anton A. Ishchenko, PhD, Head of the Center for Gynecology and Reproductive Technologies, National Medical Research Center for Treatment and Rehabilitation,
Ministry of Health of Russia, 125367, Russia, Moscow, Ivankovskoye Shosse, 3, +7(499)450-03-93, ra2001_2001@mail.ru, https://orcid.org/0000-0002-4476-4972
Vladimir M. Zuev, Dr. Med. Sci., Professor, Professor at the Department of Obstetrics and Gynecology No. 1, Sklifosovsky Institute of Clinical Medicine,
I.M. Sechenov First Moscow State Medical University, Ministry of Health of Russia (Sechenov University), 119048, Russia, Moscow, Trubetskaya str., 8, bld. 2,
+7(499)248-69-56, vlzuev@bk.ru, https ://orcid.org/0000-0001-8715-2020
Irina V. Gadaeva, PhD, Associate Professor at the Department of Obstetrics and Gynecology No. 1, Sklifosovsky Institute of Clinical Medicine, I.M. Sechenov First Moscow State Medical University, Ministry of Health of Russia (Sechenov University), 119048, Russia, Moscow, Trubetskaya str., 8, bld. 2, +7(499)248-69-56, irina090765@gmail.com, https://orcid.org/0000-0003-0144-4984
Elena G. Malyuta, PhD, Head of Gynecological Department, National Medical Research Center for Treatment and Rehabilitation, Ministry of Health of Russia, 125367, Russia, Moscow, Ivankovskoye Shosse, 3, +7(495)730-98-89, egma@list.ru, https://orcid.org/0000-0003-0098-0830
Tea A. Dzhibladze, Dr. Med. Sci., Professor, Professor at the Department of Obstetrics and Gynecology No. 1, Sklifosovsky Institute of Clinical Medicine, I.M. Sechenov
First Moscow State Medical University, Ministry of Health of Russia (Sechenov University), 119048, Moscow, Trubetskaya str., 8, bld. 2, +7(499)248-69-56, djiba@bk.ru, https://orcid.org/0000-0003-1540-5628
Mikhail P. Isaev, PhD, General Director, MedOptoTech LLC, 117342, Russia, Moscow, Butlerova str., 17B, office 334, +7(925)748-95-68, medoptotec@yandex.ru,
https://orcid.org/0009-0009-6995-7381
Lilia B. Obosyan, Resident at the Department of Obstetrics and Gynecology No. 1, Sklifosovsky Institute of Clinical Medicine, I.M. Sechenov First Moscow State Medical University, Ministry of Health of Russia (Sechenov University), 119048, Russia, Moscow, Trubetskaya str., 8, bld. 2, +7(925)196-17-78, lilia070500@mail.ru,
https://orcid.org/0000-0002-1316-6291
Irina D. Khokhlova, PhD, Associate Professor at the Department of Obstetrics and Gynecology No. 1, Sklifosovsky Institute of Clinical Medicine, I.M. Sechenov First Moscow State Medical University, Ministry of Health of Russia (Sechenov University), 119048, Russia, Moscow, Trubetskaya str., 8, bld. 2, +7(499)248-69-56, irhohlova5@gmail.com, https://orcid.org/0000-0001-8547-6750
Elena V. Minashkina, Doctor at the Ultrasound Diagnostics Department of the Obstetrics and Gynecology Clinic of the Sechenov Center for Motherhood and Childhood, I.M. Sechenov First Moscow State Medical University, Ministry of Health of Russia (Sechenov University), 119048, Russia, Moscow, Elansky str., 2, bld. 1, +7(916)600-11-99, as1199@list.ru, https://orcid.org/0009-0004-3448-7944
Ekaterina V. Tevlina, Teaching Assistant at the Department of Obstetrics and Gynecology No. 1, Sklifosovsky Institute of Clinical Medicine, I.M. Sechenov First Moscow State Medical University, Ministry of Health of Russia (Sechenov University), 119048, Russia, Moscow, Trubetskaya str., 8, bld. 2, +7(903)689-67-39, tevlina.ekaterina@gmail.com, https://orcid.org/0009-0003-5235-1814
Maxim V. Verbitsky, Clinical Resident at the Department of Obstetrics and Gynecology No. 1, Sklifosovsky Institute of Clinical Medicine, I.M. Sechenov First Moscow State Medical University, Ministry of Health of Russia (Sechenov University), 119048, Russia, Moscow, Trubetskaya str., 8, bld. 2, 7(909)167-88-81, MVS-7-99@yandex.ru, https://orcid.org/0009-0006-0749-5538
Corresponding author: Tea A. Dzhibladze, djiba@bk.ru