Possibilities for predicting recurrent uterine myoma by plasma lipidomic analysis
Objective. To predict recurrent uterine fibroids (UFs) by direct mass spectrometry.Tonoyan N.M., Tokareva A.O., Chagovets V.V., Starodubtseva N.L., Kozachenko I.F., Adamyan L.V., Frankevich V.E.
Subjects and methods. A plasma lipidomic analysis was carried out in 81 patients treated at the V.I. Kulakov National Medical Research Center of Obstetrics, Gynecology, and Perinatology, including 35 patients with newly diagnosed UFs, 31 patients diagnosed with recurrent UFs (RUFs), and 15 comparison group patients who underwent surgical treatment for infertility, intrauterine septum. Semi-quantitation of blood lipid levels was performed by high performance liquid chromatography-mass spectrometry (HPLC-MS/MS). Mass spectrometric data were processed using the orthogonal projection to latent structure discriminant analysis (OPLS-DA) to build a statistical model for classifying samples and identifying potential biomarkers. The lipids were identified by their exact mass and characteristic tandem mass spectra (MS/MS).
Results. The presented patient groups differed in the lipid composition of blood plasma by the presence and level of phospholipids, sphingomyelins, cholesterol esters, and triglycerides. The created statistical models made it possible to identify lipids, potential biomarkers of both the disease itself and its recurrences.
Conclusion. This investigation confirms the implication of phospholipids and sphingolipids in the pathogenesis of UFs and opens up new possibilities for predicting RUFs.
Keywords
Uterine fibroids (UF) are one of the most common benign tumors of the female genital tract that occur in every third woman of reproductive age [1–3].
For many reasons, women postpone their motherhood to a later date, which leads to an increase in the quantity of gynecological pathologies including UF. Therefore, indications for reconstructive surgery should be expanded [4].
Organ-preserving operations are associated with the possibility of recurrence of the disease, which in some cases can lead to repeated surgery. Doridot V. et al. [5] identify the recurrence of UF on the basis of the combination of the following facts: the presence of a myoma during ultrasound examination and the appearance of a clinical picture of the disease similar to that before surgery.
In most studies on the recurrence of leiomyomas, the risk of relapse is associated with the genetic aspect (MED 12 gene), the presence of a familial history of this disease, the age of patients (30–40 years), a large number of myomas (more than three), rapid growth of UF before surgery, and large sizes of the submucous tumor with its incomplete resection, as well as with morphological and histological types of tumors [6, 7]. According to many authors, the recurrence of UF is mainly a measure of the accuracy and qualification of the surgeon in finding and trying to remove all small myomas, and additional hormonal treatment only corrects the symptoms of the disease; this treatment is symptomatic and only extends the time of pregnancy.
Despite the huge number of studies on various aspects of UF, the etiology and pathogenesis of this disease are not fully understood, there are not any methods for its early diagnosis and determining the prognosis of relapse in the future. Changes in lipid metabolism in UF are manifested in a decrease in blood levels of high density lipoproteins and an increase in the level of low density lipoproteins and oxylipoproteins [8], as well as a decrease in the level of malondialdehyde [9]. Targeted blood tests of patients with UF revealed significant differences in the level of certain proteins. A correlation has been demonstrated between the level of dioxin in the blood and the risk of UF [10]. A group of J. Wong and E. Gold [11] proposed a method for assessing the risk of UF or its recurrence by the level of sex hormones in the blood.
Thus, the development of modern principles for the early diagnosis of UF as well as its recurrence using highly informative modern methods (in particular, chromatography-mass spectrometry) with minimal invasion is of great importance.
In this study, we analyzed the lipid content in the blood plasma of patients with UF taken before surgery and the potential use of plasma lipidoma for the diagnosis of UF. The advantage of using blood plasma for diagnosing UF and its relapse is minimally invasive and simple blood sampling.
Materials and methods
The study included 35 women with newly diagnosed UF and 31 patients with the diagnosis of recurrent UF (RUF); they were examined and operated on at Gynecology Department of the National Medical Research Center for Obstetrics, Gynecology and Perinatology, Moscow, Russia. The comparison group consisted of 15 patients operated on for infertility and the intrauterine septum. All patients signed an informed consent to participate in the study, approved by the Ethics Committee of the National Medical Research Center for Obstetrics, Gynecology and Perinatology.
UF was diagnosed with a vaginal examination, ultrasound, confirmed by laparoscopy, finally confirmed by histological examination. Inclusion criteria for the UF and RUF groups were the presence of uterine fibroids, reproductive age of patients (18–45 years), patient’s interest in maintaining reproductive function, lack of hormone therapy for 6 months or more before surgery. Exclusion criteria were contraindications for surgical treatment, cancerous tumors, sexually transmitted infections, acute infectious diseases, pelvic inflammatory diseases, systemic autoimmune diseases, severe somatic pathology.
The main complaints of patients who presented for surgical treatment were pain during intercourse; menstrual disorders, namely painful, heavy, irregular menstruation; intermenstrual discharge; dysfunction of adjacent organs: constipation, frequent urination, infertility, miscarriage.
All patients were reproductive-aged women. The average age of patients with UF was 37.9 ± 5.5 years, and patients with RUF were 40.0 ± 5.2 years. When analyzing the age indicator, it was found that the incidence of RUF is higher in the group of women over 40 years old, while the first myomectomy is performed at the age of 30–40 years.
The body mass index (BMI) in patients with UF and RUF was 24.05 and 24.7, respectively. There was a statistically significant (p <0.05) excess of BMI in patients with RUF compared with that in patients with UF. When analyzing the UF relapse group, it was revealed that repeated myomectomy was performed on average in 5.7 ± 4.4 years.
All patients underwent laparoscopic surgery. Indications for surgical treatment were heavy menstruation leading to anemia, severe pain, lack of effect from previously performed conservative therapy, absence of pregnancy in the women of reproductive age.
In the RUF group, the number of removed myomas was statistically significantly higher than that in the UF group (UF - 3-4 nodes, RUF - 5-6 nodes), but the size of the removed nodes prevailed in the UF group (UF - 8.1 cm, RUF - 6.3 cm).
Blood sampling was performed on an empty stomach shortly before surgery. Blood was collected in a sterile vacuum tube with EDTA - sodium (0.5 ml of a 1.5% solution per 10 ml of blood) and centrifuged for 10 min at 2500 rpm to obtain plasma. A cryo tube with blood plasma in liquid nitrogen was transported to a biobank, where it was stored in a freezer at a temperature of -80 ° C until analysis.
Lipid extracts were obtained in accordance with the modified Folch method [12]. In the course of this study, 480 ml of a chloroform-methanol mixture (2:1) was added to a 40 ml plasma sample, the mixture was subjected to ultrasound for 10 min, after which 150 ml of H2O were added to the mixture and passed through Vortex for 10 sec. The mixture was centrifuged for 5 minutes at 15,000 rpm at ambient temperature. The organic layer containing lipids was taken, vacuum dried, then redissolved in a mixture of 100 ml of isopropanol and 100 ml of acetonitrile for subsequent mass spectrometric analysis.
The samples were analyzed on a Dionex Ultimate 3000 liquid chromatograph (ThermoScientific, Bremen, Germany) coupled to a Maxis Impact qTOF mass spectrometer (Bruker Daltonics, Bremen, Germany). Lipid extracts were separated on a Zorbax SB-C18 column (0.5x150 mm, sorbent 5 μm, Agilent), injected sample volume 3 μl, flow rate 40 μl/min, column temperature 50°C, mobile phase gradient: 0 - 0.5 min, 70% A + 30% B, 20.5 - 30.5 min, 1% A + 99% B, 31 - 33 min, 70% A + 30% B; where A is 10 mmol/L ammonium formate solution and 0.1% solution of formic acid in acetonitrile / H2O (60/40), B is 10 mmol/L solution of ammonium formate and 0.1% solution of formic acid in isopropanol/acetonitrile/H2O (90/8/2). Mass spectra were obtained in the mode of positive ions in the range of m/z 400-1000 with the following settings: voltage at the capillary 4.1 kV, pressure of the spraying gas 0.7 bar, flow rate of the drying gas 6 L/min, temperature of the drying gas 200°С [13, 14].
For preliminary processing of chromatographic-mass spectrometric data, the free msConvert programs from Proteowizard 3.0.9987 were used to convert .d files to MzXml files and MzMine to extract mass chromatographic peaks, normalize to the full ion current and create a table containing peak information - mass of ion, exit time, peak area.
For statistical processing of the obtained numerical data, we used scripts written in the R language version 3.3.3 [15] and the RStudio 1.1.383 program under the GNU General Public License [16].
Lipids were identified using the Lipid Match R script [17] for the exact mass using the Lipid Maps database [18] and for the characteristic tandem mass spectra (MS/MS). Statistical analysis to determine lipids, potential UF markers, was performed using a nonparametric two-way Mann – Whitney test. The intensities of the peaks related to lipids were described as the median (Me) and quartiles Q1 and Q3 in the format Me (Q1; Q3). The value of the critical significance level p was taken equal to 0.05. The search for potential lipid markers was carried out through the analysis of the diagnosis and lipid levels with a significant difference in levels using the method of discriminant analysis with orthogonal projection onto latent structures (OPLS-DA) with cross-validation by seven-fold partitioning. Due to this fact it was possible to construct a statistical model on the basis of some sample, the membership of each sample to a particular group was known and lipids responsible for differences in groups could be assessed. Potential lipid markers included lipids whose importance of the independent variable for projection (VIP) for the discriminant model exceeded 1 [19].
The lipids (VIP>1, p <0.05) were selected for each pair of clinical groups and for pair the control group / combined group: newly diagnosed fibroids and recurrent fibroids were analyzed in terms of their use as diagnostic markers by constructing multivariate logistic regression using levels of lipid markers as predictor variables and diagnosis as a response variable and cross-validation of the diagnostic model for individual objects. A potential diagnostic model of logistic regression was built on the basis of an N - 1 object with a subsequent test of an object not participating in the construction of the regression, where N is the number of objects in a pair of clinical groups for which a diagnostic model is built.
Results and Discussion
In the last decade, postgenomic methods of analysis are increasingly used to search for markers of various diseases. Among them the leading positions are occupied by metabolic and proteomic technologies, which make it possible to determine the molecular composition of any biological sample with high accuracy [20]. Lipids and fatty acids are involved in all processes occurring in the body: they are a structural element of cell membranes, perform a transport function for hydrophobic and amphiphilic substances and are involved in the regulation of cell proliferation, migration, extracellular and intracellular signal transmission [21].
In this study, a lipid analysis of the blood of patients with UF and RUF was performed. The comparison group consisted of patients without UF, its absence was confirmed by ultrasound and laparoscopy. A total of 81 patients participated in the study.
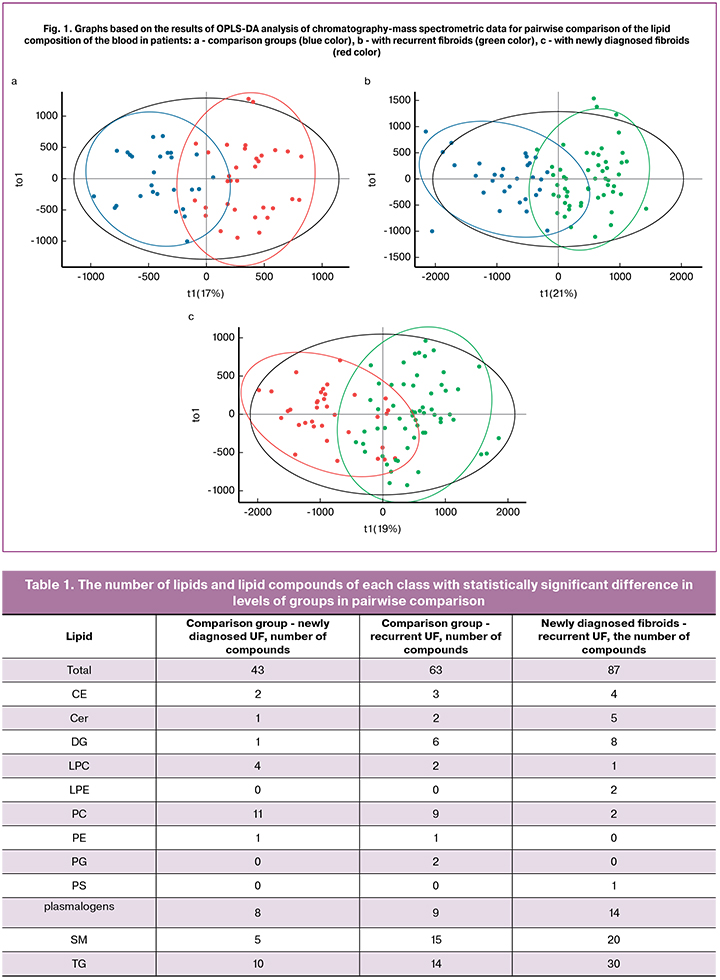
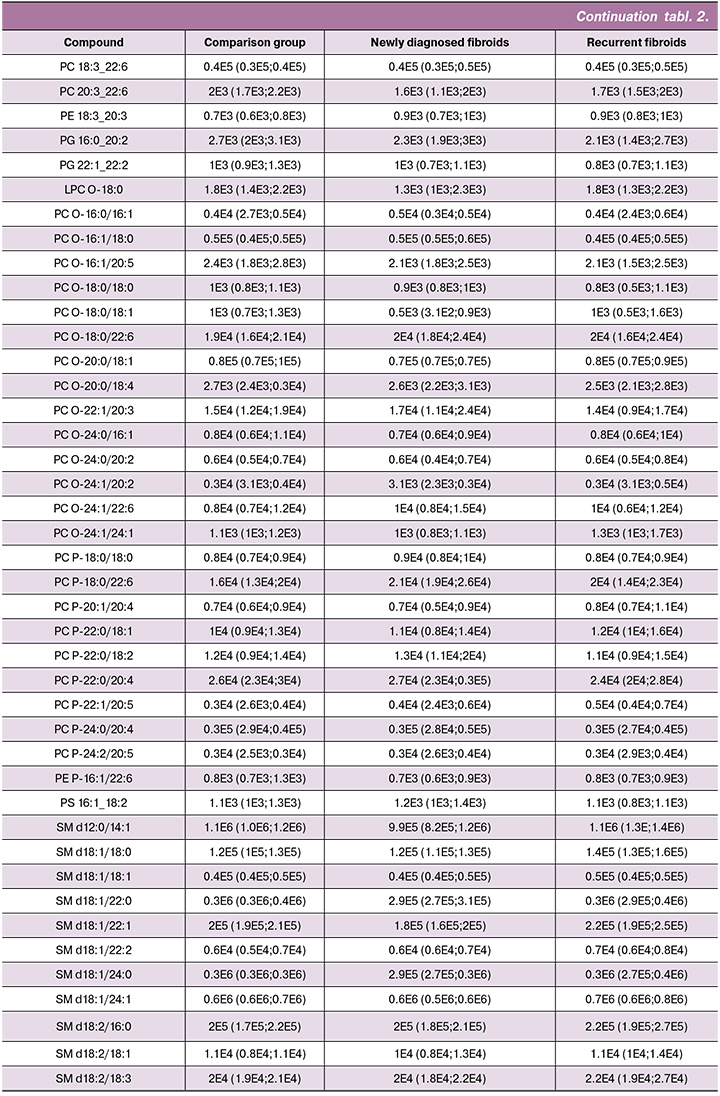
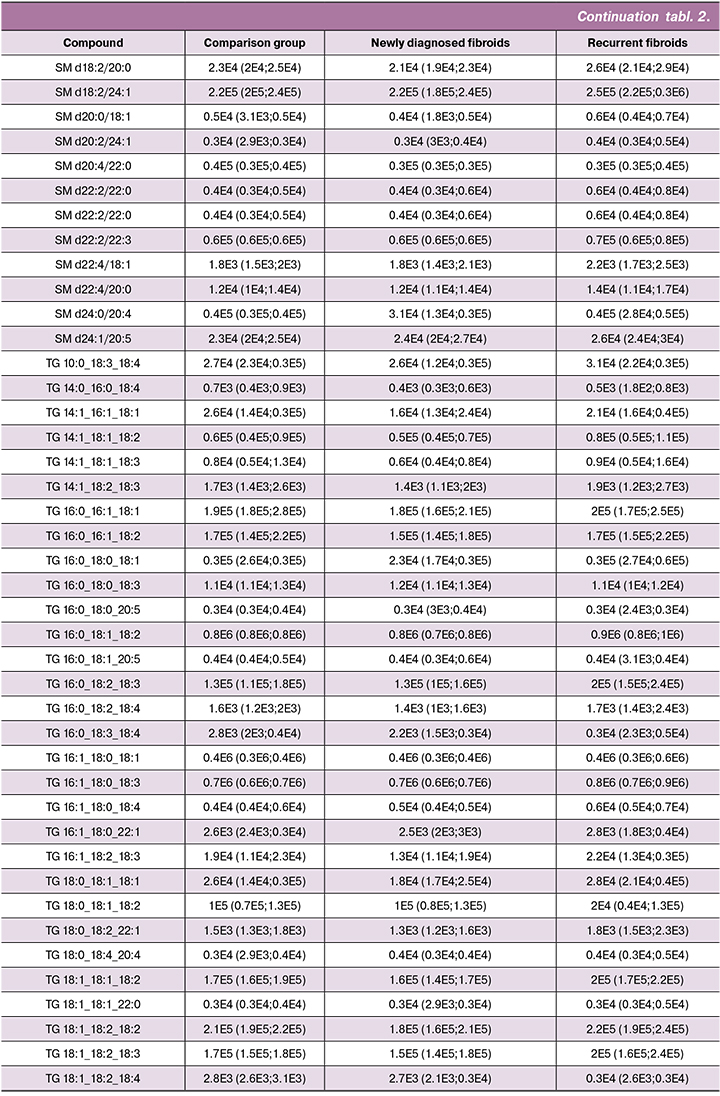
In plasma samples, 267 lipid compounds were identified. To search for potential lipid markers, lipid levels were tested for the Mann – Whitney test in pairs control group / newly diagnosed fibroid, control group / recurrent fibroid and newly diagnosed fibroid / recurrent fibroid. Statistically significant differences were found in the first case in 43 lipids, the differences were found in the second case in 64 lipids, and in the group of patients with newly diagnosed fibroid and recurrence statistically significant differences were revealed in 87 lipids (Tables 1–2).

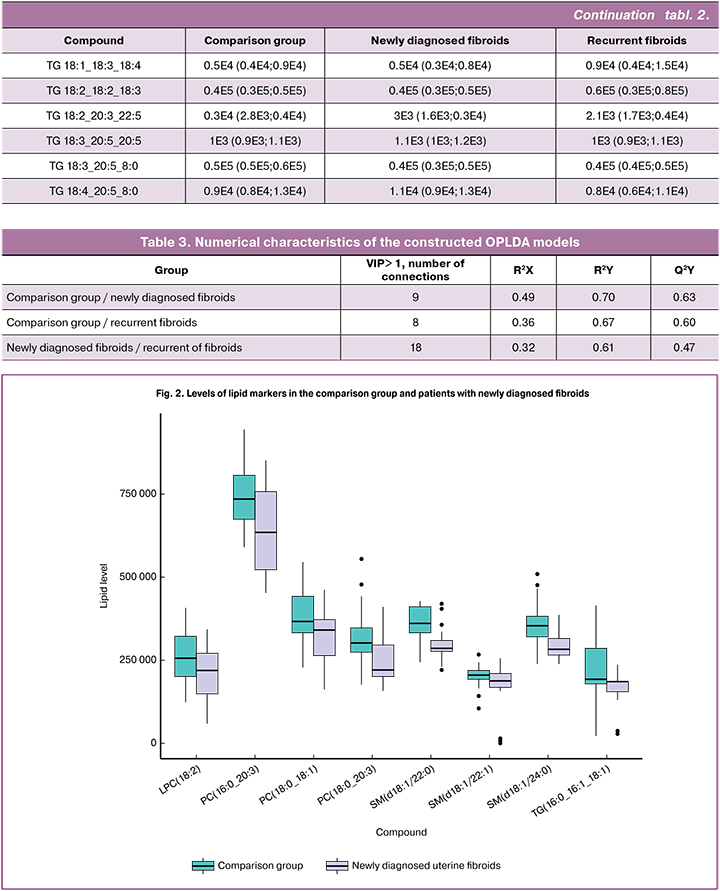
Based on the data on the level of potential lipid markers in blood plasma, OPLS-DA models were constructed for classifying patients from the comparison group, patients with newly diagnosed fibroid and patients with recurrent fibroid (Fig. 1). For the classification, the comparison group / fibroid, the proportion of data included in the model (R2Y) was 70 and 67% for the newly diagnosed fibroid, respectively, and the expected classification accuracy when adding new ones (Q2Y) in cross-validation was 63 and 60%. For the classification newly diagnosed fibroid/recurrence, these values were 61 and 47% (Table 3).
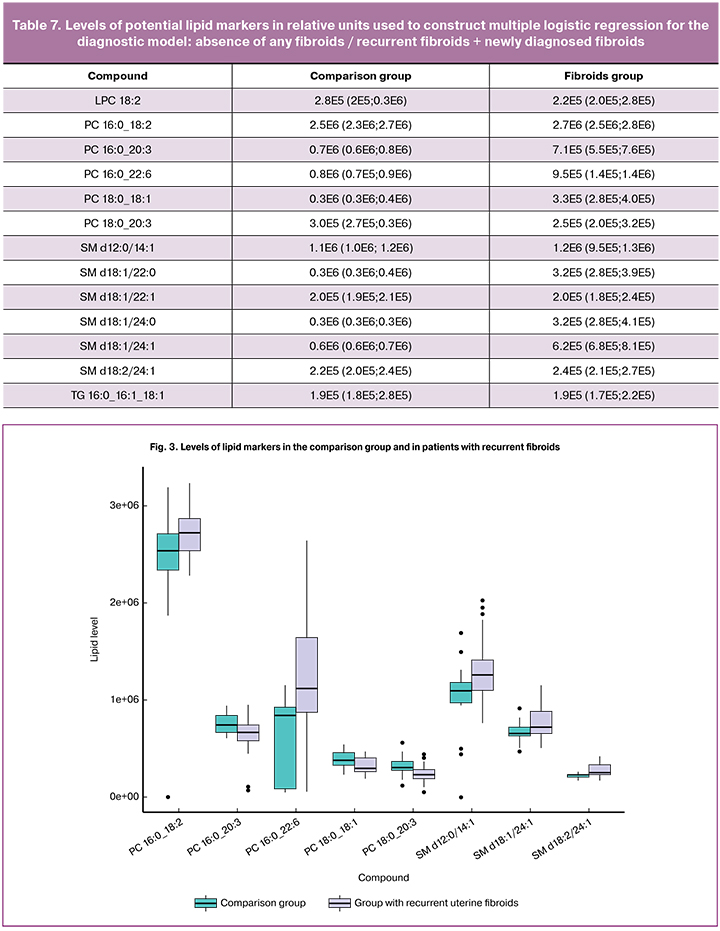
Phosphotidylcholines (LPC 18:2, PC 16:0_20:3, PC 18:0_18:1, PC 18:0_20:32 in case of newly diagnosed fibroid, and PC 16:0_22:6, PC 16:0_18:2, PC 16:0_20:3, PC 18:0_20:3, PC 18:0_18:1 in case of recurrence) and sphingomyelins (SM d18:1/22:0, SM d18:1/22:1, SM d18:1/24:0 in case of newly diagnosed fibroid, and SM d18:1/24:1, SM d18:2/24:1 in case of recurrence) were of great importance for the classification model (VIP>1) comparison group / fibroid (Fig. 2-3). Cholesterol esters (CE 18:2, CE 20:4), phosphotidylcholines (PC 18:0_18:2, PC 16:0_22:6), sphingomyelins (SM d12:0/14:1, SM d18:1/22:0, SM d18:1/22:1, SM d18:1/24:0, SM d18:1/24:1, SM d18:2/16:0, SM d18:2/24:1) and triglycerides (TG 14:1_18:1_18:2, TG 16:0_16:1_18:2, TG 16:0_18:1_18:2, TG 16:0_18:2_18:3, TG 16:1_18:0_18:1, TG 16:1_18:0_18:3, TG 18:1_18:2_18:3) had the most significant influence on the classification model newly diagnosed fibroid / recurrent fibroid (Fig. 4). In some cases, lipids, which are potential markers of newly diagnosed fibroid, are not the markers of recurrent fibroid or the level of lipids changes in comparison with the control group (Fig. 5).
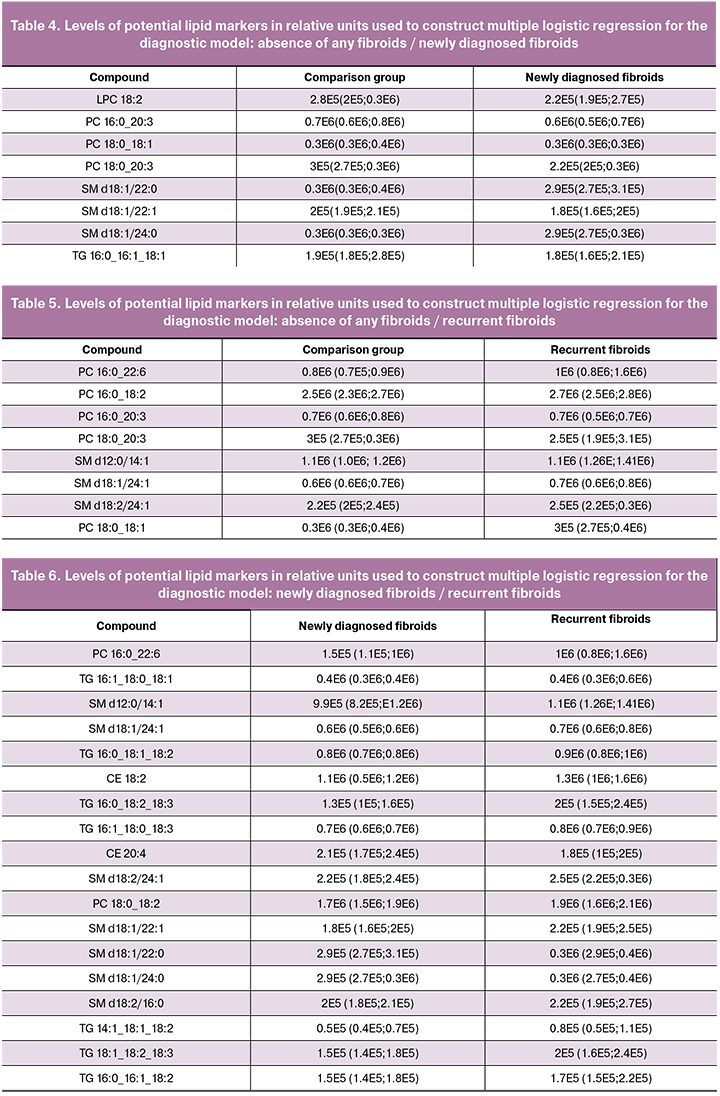
The analysis of multiple logistic regressions using relative lipid intensities as predictors previously identified as potential lipid markers (Tables 4–7) showed a statistically significant relationship between lipid levels SM d18: 1/22: 0 (p = 0.009) and SM d18: 1/22: 1 (p = 0.049) and the presence of newly diagnosed fibroid / absence of any fibroid (Table 8). In the logistic regression, which describes the differences between the comparison group and the group with recurrent fibroids, the relationship between the diagnosis and the levels of phosphotidylcholines PC 16: 0_22: 6 (p = 0.023), PC 16: 0_18: 2 (p = 0.020), PC 18:0_18:1 (p = 0.017) and sphingomyelins SM d12: 0/14: 1 (p = 0.008) and SM d18:2/24: 1 (p = 0.046) can be considered statistically significant (Table 9). When comparing newly diagnosed fibroids and recurrent fibroids, a statistically significant relationship was found only in SM d18: 2/24: 1 (p = 0.049) (Table 10). The analysis of the logistic regression constructed to diagnose the presence / absence of fibroids showed a statistically significant relationship between the diagnosis and levels of PC 16: 0_18: 2 (p = 0.012) and PC 18: 0_18: 1 (p = 0.014) (Table 11).
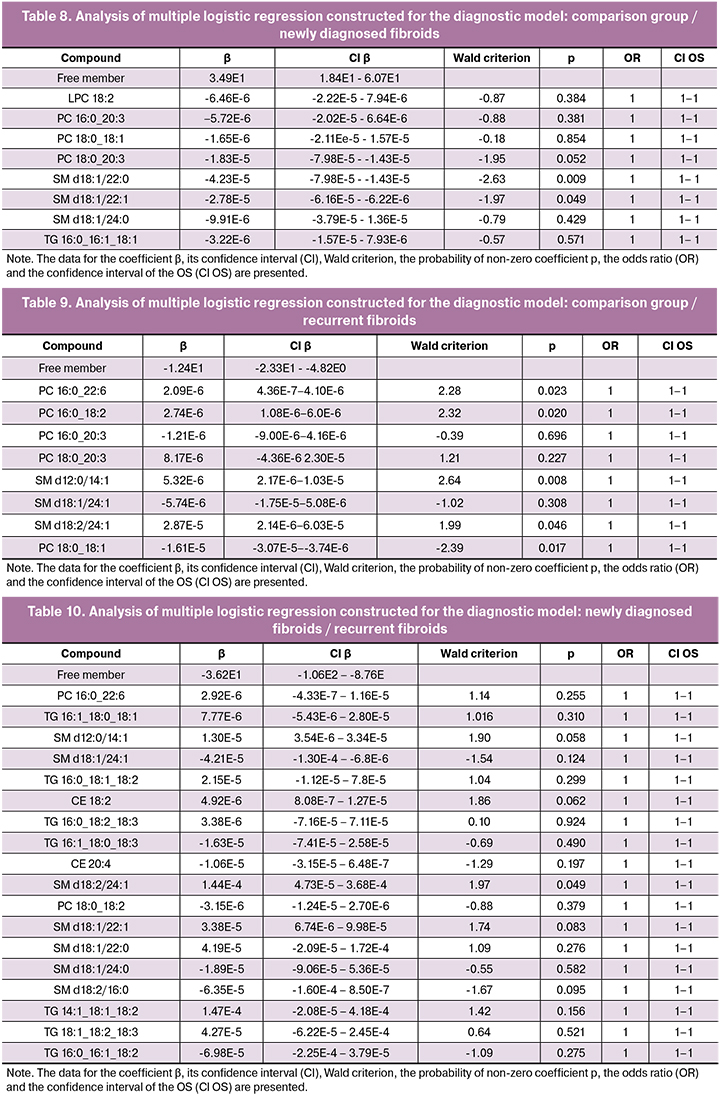
Equality to the unit of odds ratio (OR) relating to all studied predictors in all logistic regressions was due to the fact that in the applied system of units a single change in lipid level is too insignificant in terms of accuracy we use.
The analysis of diagnostic models which were constructed using logistic regression on the basis of selected lipid markers specific for each pair of clinical groups demonstrated high sensitivity and predictability of a positive result of models (Table 12) and significant specificity and predictability of a negative result, which allows us to talk about the relationship between plasma lipidoma and the development of UF, as well as the relationship of blood plasma lipidoma and recurrent UF. The high sensitivity of the diagnostic model based on the group of lipid markers made up of each pair of clinical groups suggests the potential effectiveness of UF diagnosis by the lipid profile of blood plasma.

The analysis of the error curve (ROC – curve) (Fig. 6, Table 12) for the constructed models shows the good quality of the diagnostic models (area under the curve ≥0.9) for all analyzed pairs.
The first study on metabolic profiling of blood plasma in patients with UF and recurrent UF is presented. Lipids, which are potential markers of newly diagnosed UF, are not markers of the recurrent UF. These are completely different lipids.

The researchers of the National Medical Research Center for Obstetrics, Gynecology and Perinatology in Moscow conducted studies on the recurrence of endometriosis, which made it possible to reveal identical lipids both in the recurrence of endometriosis and in the newly diagnosed endometriosis. In the case of UF, the recurrence of this disease at the molecular level is a different process.
Therefore, further studies are needed to study the pathogenetic features of UF recurrence and the creation of prognostic methods; on their basis it is necessary to develop new diagnostic criteria using non-invasive or minimally invasive examination methods to predict possible recurrence and growth rate of fibroids.
Conclusion
The analysis of the lipid composition of blood plasma in patients with UF, RUF and patients without UF revealed a number of phospholipids, sphingomyelins, cholesterol esters and triglycerides, the levels of which differ significantly in blood plasma in women with UF, RUF and the control group.
A comparative study of mass spectrometric profiles of blood plasma will reveal new molecular markers for diagnosing the course of the disease. In the future, the results of these studies can be used to determine the optimal treatment tactics for patients with uterine fibroid and to create new prognostic strategies and treatment methods.
References
- Duhan N. Current and emerging treatments for uterine myoma – an update. International Journal of Women’s Health. 2011; 3: 231-241. http://dx.doi.org/10.2147/IJWH.S15710
- Donnez J., Tatarchuk T.F., Bouchard P., Puscasiu L., Zakharenko N.F., Ivanova T., Ugocsai G., Mara M., Jilla M. P., Bestel E., Terrill P., Osterloh I., Loumaye E. Ulipristal Acetate versus Placebo for Fibroid Treatment before Surgery. The New England Journal of Medicine. 2012; 366: 409-20. DOI: 10.1056/NEJMoa1103182
- Bourdel N., Bonnefoy C., Jardon K., Da Ines D., Tognazza E., Rabischong B., Botchorisvili R., Pouly J.-L., Canis M., Mage G. Myomectomie hystéroscopique: récidive et enquête de satisfaction à court et long terme. Journal de Gyne ́cologie Obste ́trique et Biologie de la Reproduction. 2011:40, 116–122. [Bourdel N., Bonnefoy C., Jardon K., Da Ines D., Tognazza E., Rabischong B., Botchorisvili R., Pouly J.-L., Canis M., Mage G. Hysteroscopic myomectomy: Recurrence and satisfaction survey at short- and long-term. Journal de Gyne ́cologie Obste ́trique et Biologie de la Reproduction. 2011:40, 116–122. (In French).] doi:10.1016/j.jgyn.2011.01.003
- Тоноян Н.М., Козаченко И.Ф., Франкевич В.Е., Чаговец В.В., Адамян Л.В. Рецидивы миомы матки. Современный взгляд на проблемы диагностики, лечения и прогнозирования. Акушерство и гинекология. 2019; 3: 32-38. [Tonoyan N.M., Kozachenko I.F., Frankevich V.E., Chagovets V.V., Adamyan L.V. Recurrences of uterine fibroids. The modern view on the problems of diagnosis, treatment, and prognosis. Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2019; (3): 32-8. (in Russian)].https://dx.doi.org/10.18565/aig.2019.3.32-38
- Doridot V., Dubuisson J.B.., Chapron C., Fauconnier A., Babaki-Fard K. Recurrence of leiomyomata after laparoscopic myomectomy. J Am Assoc Gynecol Laparosc. 2001; 8 (4): 495-500. DOI: 10.1016/s1074-3804 (05)60610-x
- Согоян Н.С., Кузнецова М.В., Асатурова А.В., Адамян Л.В., Трофимов Д.Ю. Соматические мутации в экзоне 2 гена MED12 у женщин с одиночной и множественной миомой матки. Акушерство и гинекология. 2018; (12): 63-70. [Sogoyan N.S., Kuznetsova M.V., Asaturova A.V., Adamyan L.V., Trofimov D.Yu. Somatic mutations in MED12 gene exon 2 in women with a single uterine fibroid or multiple ones. Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2018; (12): 63-70. (in Russian)]. http://dx.doi.org/10.18565/aig.2018.12.63–70
- Караваев Ю.Е., Аскольская С.И., Коган Е.А., Арсланян К.Н., Бурыкина П.Н. Прогностические критерии рецидива лейомиомы матки после реконструктивно-пластических операций. Акушерство и гинекология. 2013; (5): 54-57. [Karavayev Yu.E., Askolskaya S.I., Kogan E.A., Arslanyan K.N., Burykina P.N. Prognostic criteria for recurrent uterine leiomyoma after reconstructive plastic surgeries. Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2013; (5): 54-57. (In Russ.)].
- Aksoy Y., Sivri N. Carotid intima-media thickness: a new marker of patients with uterine leiomyoma. Eur J Obstet Gynecol Reprod Biol. 2014; 175: 54-7. doi: 10.1016/j.ejogrb.2014.01.005
- Caglayan A., Katlan D., et al. Assessment of oxidant-antioxidant status alterations with tumor biomarkers and reproductive system hormones in uterine myomas. Eur J Obst Gyn Repr Biol. 2018; 229: 1-7. https://doi.org/10.1016/j.ejogrb.2018.07.031
- Eskenazi B., Warner M., Mocarelli P., Samuels S., Needham L.L., Patterson D.G. Jr., Lippman S., Vercellini P., Gerthoux P.M., Brambilla P., Olive D. Serum dioxin concentrations and menstrual cycle characteristics. Am J Epidemiol. 2002; 156 (4): 383-92. DOI: 10.1093/aje/kwf046
- Wong J., Gold E. Circulating Sex Hormones and Risk of Uterine Fibroids: Study of Women’s Health Across the Nation (SWAN). J Clin Endocrinol Metab. 2016; 101 (1): 123-30. doi: 10.1210/jc.2015-2935
- Folch J., Lees M., Sloane Stanley G.H. A simple method for the isolation and purification of total lipides from animal tissues. J. Biol. Chem. 1957; 226 (1): 497-509. PMID: 13428781
- Chagovets V., Wang Z., Kononikhin A., Starodubtseva N., Borisova A., Salimova D., Popov I., Kozachenko A., Chingin K., Chen H., Frankevich V., Adamyan L., Sukhikh G. A Comparison of Tissue Spray and Lipid Extract Direct Injection Electrospray Ionization Mass Spectrometry for the Differentiation of Eutopic and Ectopic Endometrial Tissues. J Am Soc Mass Spectrom. 2018; 29 (2): 323-30. doi: 10.1007/s13361-017-1792-y
- Chagovets V.V., Wang Z., Kononikhin A.S., Starodubtseva N.L., Borisova A., Salimova D., Popov I.A., Kozachenko A.V., Chingin K., Chen H., Frankevich V.E., Adamyan L.V., Sukhikh G.T. Endometriosis foci differentiation by rapid lipid profiling using tissue spray ionization and high resolution mass spectrometry. Sci Rep. 2017; 7 (1): 2546. doi: 10.1038/s41598-017-02708-x
- R Core Team (2018). R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. URL https://www.R-project.org/
- RStudio Team (2016). RStudio: Integrated Development for R. RStudio, Inc., Boston, MA URL http://www.rstudio.com/.
- Koelmel J.P., Kroeger N.M., Ulmer C.Z. et al. LipidMatch: an automated workflow for rule-based lipid identification using untargeted high-resolution tandem mass spectrometry data. BMC Bioinformatics. 2017; 18: 331. doi:10.1186/s12859-017-1744-3
- Sud M., Fahy E., Cotter D., Brown A., Dennis E.A., Glass C.K., et al. LMSD: LIPID MAPS structure database. Nucleic Acid Res. 2007; 35 (Database issue): D527-32. DOI: 10.1093/nar/gkl838
- Wold S., Sjöström M., Eriksson L. PLS-regression: a basic tool of chemometrics. Chemometrics and Intelligent Laboratory Systems. 2001; 58 (2): 109-130. https://doi.org/10.1016/S0169-7439 (01)00155-1
- Лисица А.В., Пономаренко Е.А., Лохов П.Г. Постгеномная медицина: альтернатива биомаркерам. Вестник Российской Академии медицинских наук. 2016; 3: 255-60. [Lisica A.V., Ponomarenko E.A., Lohov P.G. Post-genomic medicine: an alternative to biomarkers. Vestnik Rossijskoj Akademii medicinskih nauk. 2016; 3:255–60. (In Russ.)].
- Борисова А.В., Чаговец В.В., Козаченко А.В., Стародубцева Н.Л., Кононихин А.С., Салимова Д.Ф., Коган Е.А., Адамян Л.В., Франкевич В.Е., Сухих Г.Т. Сравнительный анализ липидного состава перитонеальной жидкости и плазмы крови у пациенток с наружным генитальным эндометриозом и миомой матки. Акушерство и гинекология. 2017; 6: 74-82. [Borisova A.V., Chagovets V.V., Kozachenko A.V., Starodubtseva N.L., Kononikhin A.S., Salimova D.F., Kogan E.A., Adamyan L.V., Frankevich V.E., Sukhikh G.T. Comparative analysis of the lipid composition of peritoneal fluid and blood plasma in patients with external genital endometriosis and uterine myoma.Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2017; 6: 74-82. (in Russian)]. http://dx.doi.org/10.18565/aig.2017.6.74–82
Received 25.05.2019
Accepted 21.06.2019
About the Authors
About the authors:Narine M. Tonoyan, postgraduate student of the Department of Operative Gynecology, National Medical Reseach Center for Obstetrics, Gynecology and Perinatology named after Academician V.I.Kulakov of the Ministry of Healthcare of Russian Federation. Tel. +79133933113. E-mail: tonnar.13@bk.ru
117997, Russia, Moscow, Ac.Oparina str.4.
117997, Russia, Moscow, Ac.Oparina str.4.
Alisa O. Tokareva, a graduate student of the Moscow Institute of Physics and Technology. Tel.: +7 (965) 1286886. e-mail: alisa.tokareva@phystech.edu
141700, Russia, Moscow Region, Dolgoprudny, Institutsky Lane, 9.
Vitaliy V. Chagovets, PhD, Senior Researcher of the Laboratory of Proteomics and Metabolomics in Human Reproduction at the Department of Systems Biology in Reproduction, National Medical Reseach Center for Obstetrics, Gynecology and Perinatology named after Academician V.I.Kulakov of the Ministry of Healthcare of Russian Federation. Tel. +79265626590. E-mail: vvchagovets@gmail.com.
117997, Russia, Moscow, Ac.Oparina str.4.
Nataliia L.Starodubtseva, PhD, Head of Laboratory of Proteomics of Human Reproduction, National Medical Reseach Center for Obstetrics, Gynecology and Perinatology named after Academician V.I.Kulakov of the Ministry of Healthcare of Russian Federation. Tel. +79164639867. E-mail: n_starodubtseva@oparina4.ru
Irena F. Kozachenko, PhD., Senior Researcher of the Department of Operative Gynecology, National Medical Reseach Center for Obstetrics, Gynecology and Perinatology named after Academician V.I.Kulakov of the Ministry of Healthcare of Russian Federation.
117997, Russia, Moscow, Ac.Oparina str.4.
Leyla V. Adamyan, MD, professor, head of the Department of Operative Gynecology, National Medical Reseach Center for Obstetrics, Gynecology and Perinatology named after Academician V.I.Kulakov of the Ministry of Healthcare of Russian Federation. Tel. +74952223737. E-mail: adamyanleila@gmail.com
117997, Russia, Moscow, Ac.Oparina str.4.
Vladimir E. Frankevich, PhD, chief of the Department of Systems Biology in Reproduction, National Medical Reseach Center for Obstetrics, Gynecology and Perinatology named after Academician V.I.Kulakov of the Ministry of Healthcare of Russian Federation. Tel. +74954380788. E-mail: v_frankevich@oparina4.ru
117997, Russia, Moscow, Ac.Oparina str.4.
For citation: Tonoyan N.M., Tokareva A.O., Chagovets V.V., Starodubtseva N.L., Kozachenko I.F., Adamyan L.V., Frankevich V.E. Possibilities for predicting recurrent uterine myoma by plasma lipidomic analysis.
Akusherstvo i Ginekologiya / Obstetrics and Gynecology. 2019; (11): 136-51.(in Russian)
http://dx.doi.org/10.18565/aig.2019.11.136-151