Recovery of menstrual function in patients with placenta accreta spectrum disorders
Aim. To investigate the menstrual function recovery time in patients with placenta accreta spectrum disorders.Marchenko R.N., Kukarskaya I.I.
Material and methods. The study prospectively analyzed 147 medical records of pregnant women with abnormal placental implantation, who underwent different methods of intraoperative hemostasis. Uterine artery embolization, hysterectomy, and surgical hemostasis without hysterectomy were performed in groups I1, I2, and I3, respectively. The study evaluated postoperative blood loss, hormonal levels, and menstrual function recovery time. Statistical analysis was performed using the Statistica 6 software.
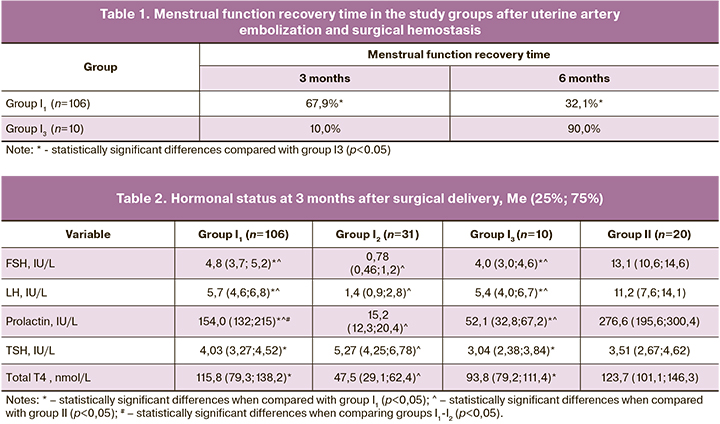
Results. During the three months of the study, menstrual cycle returned in 67.9% and 10% of patients in groups I1 and I3, respectively. The fastest return to normal levels of hormones was observed in patients of group I1.
Conclusion. The embolization of the uterine arteries is an effective organ-sparing technique that contributes to the rapid resumption of menstrual function.
Keywords
Despite medical advances, massive postpartum hemorrhage continues to be a significant clinical problem for the obstetricians and gynecologists [1–4]. In recent years, there has been a growing incidence of obstetric hemorrhage associated with placenta accreta spectrum disorders [5–8]. Currently, it has become possible not only to control intraoperative blood loss but also to carry out organ-sparing operations with intraoperative blood salvage and auto-transfusion of processed red cells. Moreover, there has been a persistent tendency to the more frequent use of uterus preserving surgeries; algorithms and techniques for appropriate surgical interventions have been developed [9–11].
The use of modern organ-sparing procedures in the management of patients with abnormal placental implantation opens up new perspectives that not only save the life of both the mother and the neonate but also prevent the loss of reproductive function. At the same time, the organ-sparing strategy is a relatively new approach. At the moment, there is still not enough information regarding the recovery of menstrual function after different surgical procedures. Given the above, this study aimed to investigate the recovery of menstrual function in patients with placenta accreta spectrum disorders.
Materials and methods
This retrospective, controlled, single-center study analyzed 147 medical records of pregnant women with a singleton pregnancy ending in a live-birth or spontaneous abortion between 2005 and 2020. Patients participating in the study had a final diagnosis classified under ICD-10 codes as placenta accreta/increta/percreta (placenta accreta spectrum). All women received antenatal and maternity care at the Tyumen Regional Perinatal Center. All study participants were divided into three clinical groups based on the type of surgical intervention for postpartum hemorrhage caused by placenta accreta spectrum. Uterine artery embolization, hysterectomy, and surgical hemostasis (compression sutures) without hysterectomy were performed in groups I1 (n=106), I2 (n=31), and I3 (n=10), respectively. The mean age of patients in groups I1, I2, and I3, was 29.2 (2.9), 32.2 (3.4), and 31.6, respectively. The control group (group II) comprised healthy women-donors (n=20), whose data were used mainly for comparing results of laboratory and instrumental examinations.
Baseline clinical evaluation of all participants included both standard examination under state guarantees of free medical care and specific studies. Reproductive hormone profile included serum prolactin, follicle-stimulating hormone (FSH), luteinizing hormone (LH), thyroid-stimulating hormone (TSH), and total thyroxine (T4).
The sample size necessary to identify differences between study groups was calculated using a standardized formula (Lopez-Jimenez F. et al., 1998) [12]. Statistical analysis was performed using the Statistica-6 software. The distribution of continuous variables was tested for normality using the Kolmogorov-Smirnov test, as well as according to the rule of two and three sigmas (σ). A visual assessment of the normality included analysis of scatterplots and histograms.
Data with non-normal distribution were reported as a median (Me) and an interquartile range (25 and 75 percentiles). Independent samples showing normal distribution were compared with the Student t-test. The Mann-Whitney test was used to compare independent samples with non-normal distribution. The critical level of significance when testing statistical hypothesis was considered at p<0.05. A correlation analysis was carried out using the Spearman correlation coefficient.
Results
In patients who underwent uterine artery embolization, the recovery of menstrual function was achieved earlier than in patients after surgical hemostasis. Three months after surgery, 72 and 1 patients resumed menstrual function in groups I1 and I3, respectively (p <0.05) (table 1). At six months after surgery, 34 and 9 patients in groups I1 and I3, respectively, resumed menstrual function (p <0.05). This fact suggests a more favorable effect of uterine artery embolization on the rate of menstrual function recovery compared with surgical hemostasis, which is probably associated with blood loss volume and the restoration of hypothalamic-pituitary-ovarian regulation.
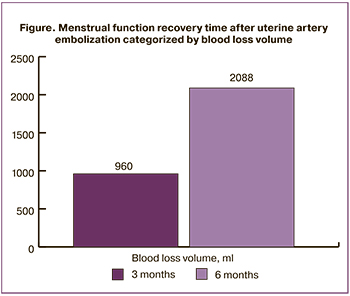 In the group of patients who underwent embolization of the uterine arteries, the time between intervention and menstrual function recovery was analyzed depending on the blood loss volume. In patients with severe blood loss, the menstrual function returned significantly later (Figure). This observation confirms the assumption that menstrual function recovery time depends on the volume of blood loss.
In the group of patients who underwent embolization of the uterine arteries, the time between intervention and menstrual function recovery was analyzed depending on the blood loss volume. In patients with severe blood loss, the menstrual function returned significantly later (Figure). This observation confirms the assumption that menstrual function recovery time depends on the volume of blood loss.
Correlation analysis showed a strong inverse correlation between blood loss volume and menstrual function recovery time (rs = -0.84, p=0.04). No statistically significant differences were found between degrees and extent of morbid placental invasion (p> 0.05).
Analysis of hormonal status revealed a significant decrease in hormone concentrations in patients undergoing hysterectomy with adnexectomy (p <0.05). There were no statistically significant differences in mean values between groups I1 and I3 (p> 0.05) (Tables 2–4), except for the prolactin level, which in group I1 was closer to the control values. No statistically significant differences were found in the dynamics of hormonal status indicators. At the same time, the changes were typical for the first three months of the postpartum period.
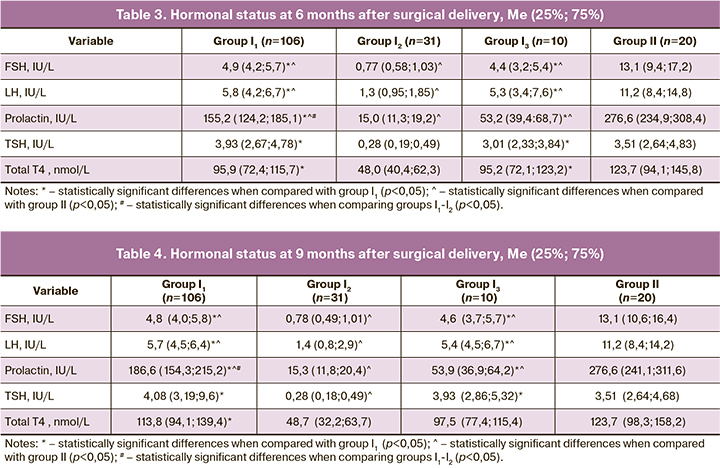
It should also be noted that in group I1, the coordinated functioning of the hypothalamus, pituitary, and thyroid gland recovered faster, which was probably associated with a lower blood loss volume in patients of this group.
In group I2, even at 9 month after the intervention, patients had laboratory signs of hypothyroidism, which indicated pronounced changes in the regulation of the hypothalamic-pituitary-thyroid axis hormones.
No differences between the study groups were observed in laboratory findings at different time points after surgical delivery. There was a significant increase in hemoglobin level, which returned to normal by nine months after delivery.
During the early postoperative period, we noted only a tendency to a decrease in the main red blood parameters, which, of course, were associated with massive blood loss. It should be emphasized that during observation against the background of continued treatment, the hemoglobin level increased by nine months by almost 20% compared with the early postoperative period.
Discussion
Until recently, hysterectomy was the method of choice in patients with placenta accreta spectrum, but now many patients are managed with current organ-sparing treatment options, among which uterine artery embolization is considered the most attractive. The advantages of this technique include the ability to maintain fertility, the simplicity of the technique, and safety. To date, this fertility-preserving approach is used in the management of fibroids and cervical and uterine body malignant neoplasms [13–15].
However, current literature is lacking sufficient coverage of using uterine artery embolization I the management of patients with placenta accreta spectrum. In the course of our study, uterine artery embolization was fund to be the favored approach for the management of bleeding in patients with the placenta accreta spectrum. This treatment option ensures maximum recovery and preservation of menstrual function. The use of this technique minimizes intraoperative trauma and postoperative hormonal imbalance (due to the minimization of mental and physical stress factors). We also established a relationship between blood loss volume during childbirth and menstrual function recovery time, which once again emphasizes the advantage of a minimally invasive approach.
Patients undergoing uterine artery embolization had shorter menstrual function recovery time than patients who had surgical hemostasis. Such significant differences can be associated with several factors, the most important of which is the blood loss volume, as well as the restoration of the hypothalamic-pituitary-ovarian regulation. This was manifested by more rapid changes in the FSH and LH concentrations leading to the restoration of their physiological levels. This fact is emphasized by the results of the correlation analysis showing a strong inverse correlation between blood loss volume and menstrual function recovery time, as well as by changes in hormonal status.
Conclusion
Women who underwent uterine artery embolization experienced more rapid recovery of their menstrual function, which helps them prepare for a pregnancy in the future. The study findings suggest that uterine artery embolization is the most appropriate technique in patients with placenta accreta spectrum disorders. This treatment modality can be recommended for routine clinical application in obstetric hospitals that have the necessary equipment.
References
- Курцер М.А., Бреслав И.Ю., Григорян А.М., Кутакова Ю.Ю., Черепнина А.Л., Штабницкий А.М. Актуальные вопросы лечения послеродовых кровотечений в акушерстве. Медицинский алфавит. 2018; 1(9): 14-7. [Kurtser M.A., Breslav I.Y., Grigoryan A.M., Kutakova Y.Y., Cherepnina A.L., Shtabnitskiy A.M. Highlights of management postpartum haemorrhage in obstetrics. Medical alphabet. 2018; 1(9):14-7. (in Russian)].
- Зверев Д.А., Приворотский В.В., Зазерская И.Е., Доброскок И.Н. Методика временной эндоваскулярной эмболизации маточных артерий при оперативном родоразрешении. Евразийский союз ученых. 2014; 8-6: 24-5. [Zverev D.A., Privorotsky V.V., Zazerskaya I.E., Dobroskok I.N. The technique of temporary endovascular uterine artery embolization during surgical delivery. Eurasian Union of Scientists. 2014; 8-6: 24-5. (in Russian)].
- Виницкий А.А., Шмаков Р.Г. Современные представления об этиопатогенезе врастания плаценты и перспективы его прогнозирования молекулярными методами диагностики. Акушерство и гинекология. 2017; 2: 5-10. [Vinitsky A.A., Shmakov R.G. Modern ideas about the etiopathogenesis of abnormal placental implantation and the prospects for its prediction by molecular diagnostic methods. Obstetrics and gynecology. 2017; 2: 5-10. (in Russian)]. https://dx.doi.org/10.18565/aig.2017.2.5-10.
- Хасанов А.А. Диагностика, профилактика и органосохраняющие методы родоразрешения беременных с врастанием плаценты. Казанский медицинский журнал. 2016; 97(4): 477-85. [Khasanov A.A. Diagnosis, prevention and organ-preserving method of delivery in pregnant women with placenta accreta. Kazan medical journal 2016; 97(4): 477-85. (in Russian)]. https://dx.doi.org/10.17750/KMJ2015-477.
- Carusi D.A. The placenta accreta spectrum: epidemiology and risk factors. Clin. Obstet. Gynecol. 2018; 61(4): 733-42. https://dx.doi.org/10.1097/GRF.0000000000000391.
- Sun W., Yu L., Liu S., Chen Y., Chen J., Wen S.W., Chen D. Comparison of maternal and neonatal outcomes for patients with placenta accreta spectrum between online-to-offline management model with standard care model. Eur. J. Obstet. Gynecol. Reprod. Biol. 2018; 222: 161-5. https://dx.doi.org/10.1016/j.ejogrb.2018.01.035.
- Reda A. Comments on: conservative surgical treatment of a case of placenta accreta. Rev. Bras. Ginecol. Obstet. 2018; 40(10): 654-5. https://dx.doi.org/10.1055/s-0038-1675221.
- Long Y., Chen Y., Fu X.Q., Yang F., Chen Z.W., Mo G.L. et al. Research on the expression of MRNA-518b in the pathogenesis of placenta accreta. Eur. Rev. Med. Pharmacol. Sci. 2019; 23(1): 23-8. https://dx.doi.org/10.26355/eurrev_201901_16743.
- Creanga A.A., Bateman B.T., Butwick A.J., Raleigh L., Maeda A., Kuklina E., Callaghan W.M. Morbidity associated with cesarean delivery in the United States: is placenta accreta an increasingly important contributor? Am. J. Obstet. Gynecol. 2015; 213(3): 384. e1-11. https://dx.doi.org/10.1016/j.ajog.2015.05.002.
- Maymon S., Maymon R., Bornstein J., Tovbin J., Melcer Y., Frank Wolf M. Comparison of two approaches for placenta accreta: uterine preservation versus cesarean hysterectomy. Harefuah. 2018; 157(11): 696-700.
- Farasatinasab M., Moghaddas A., Dashti-Khadivaki S., Raoofi Z., Nasiripour S. Management of abnormal placenta implantation with methotrexate: A review of published data. Gynecol. Obstet. Invest. 2016; 81(6): 481-96. https://dx.doi.org/10.1159/000447556.
- Lopez-Jimenez F., Pniagua D., Lamas G.A. La interpretacion de los ensayos clinicos negatovos. Rev. Invest. Clin. 1998; 50(5): 435-40.
- Олейникова О.Н. Оценка эффективности эмболизации маточных артерий при маточных кровотечениях различной этиологии. АГ-Инфо. 2009; 2: 38-42. [Oleinikova O.N. Evaluation of the effectiveness of uterine artery embolization in uterine bleeding of various etiologies. AG-Info. 2009; 2: 38-42. (in Russian)].
- Шадрин Р.В., Шумова М.А., Кулик В.В., Назарян Г.С. Органосохраняющие операции у беременных с врастанием плаценты: наш опыт. Научный вестник здравоохранения Кубани. 2017; 2: 108-16. [Shadrin R.V., Shumova M.A., Kulik V.V., Nazaryan G.S. Organ-sparing operations in pregnant women with abnormal placental implantation: our experience. Scientific Bulletin of Health of the Kuban. 2017; 2: 108-16. (in Russian)].
- Дикун Т.В., Брагинец А.С., Терпелова А.С., Кузьмич Н.В., Петрашевский А.И., Крицкий Д.В., Буцанец А.В., Устинович О.Ю. Эмболизация маточных артерий как метод лечения миомы матки. Молодой ученый. 2018; 16: 24-5. [Dikun T.V., Braginets A.S., Terpelova A.S., Kuzmich N.V., Petrashevsky A.I., Kritsky D.V., Butanets A.V., Ustinovich O.Yu. Uterine artery embolization as a treatment for uterine fibroids. Young scientist. 2018; 16: 24-5. (in Russian)].
Received 06.05.2020
Accepted 25.06.2020
About the Authors
Roman N. Marchenko, graduate student of the Department of Obstetrics, Gynecology and Intensive Care with a course of clinical and laboratory diagnostics, Tyumen State Medical University, Ministry of Health of the Russian Federation, Head of the obstetric physiological department No. 2 of the GBUZ TO Perinatal Center city of Tyumen. Tel.: +7(3452)50-82-77. E-mail: vrach08@rambler.ru. 625002, Russia, Tyumen, Daudelnaya str., 1 build. 7.Irina I. Kukarskaya, MD, professor of the Department of Obstetrics, CTNC and Reanimatology with a course of clinical laboratory diagnostics at the Tyumen State Medical University of the Ministry of Health of the Russian Federation, chief obstetrician-gynecologist of the Department of Health of the Tyumen Region, chief doctor of the GBUZ TO Perinatal Center city of Tyumen. Tel.: +7(3452)50-82-77. E-mail: kukarskay@mail.ru. 625002, Russia, Tyumen, Daudelnaya str., 1 build. 7.
For citation: Marchenko R.N., Kukarskaya I.I. Recovery of menstrual function in patients with placenta accreta spectrum disorders.
Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2020; 7: 100-104 (in Russian)
https://dx.doi.org/10.18565/aig.2020.7.100-104