The influence of cytokine therapy on ultrasound assessment of uterine hemodynamics in treatment of chronic endometritis
Ozerskaya I.A., Porkhovatyi S.Ya., Kazaryan G.G., Ozhogina E.V.
Objective: To evaluate the effect of chronic endometritis treatment including cytokine therapy on uterine artery and endometrial blood flows.
Materials and methods: The retrospective analysis of 298 women of reproductive age with a verified diagnosis of chronic endometritis was performed. The main group consisted of 140 patients. The patients received standard anti-inflammatory therapy and cytokine therapy (the drug Superlymph). The comparison group included 158 patients who received similar treatment, but without cytokine therapy. Doppler sonography assessment of uterine artery blood flow and calculation of arterial perfusion index (PI), as well as VI, FI and VFI was performed.
Results: After therapy in combination with treatment with cytokines, there was redistribution of arteriovenous blood flow and restoration of balanced microcirculation, so that the blood volume of the arterial bed was in compliance with venous blood volume. This was evidenced by a significantly decreased uterine artery and endometrial VI, FI and VFI, and relatively stable arterial PI. Hypervascularization of the uterus and endometrium during the inflammatory process was caused by venous outflow obstruction, but not by increased arterial inflow.
Conclusion: The effectiveness of anti-inflammatory therapy for chronic endometritis in combination with treatment with exogenous cytokines improves the hemodynamics of the uterus and endometrium by restoring venous outflow.
Authors' contributions: Ozerskaya I.A. – the concept and design of the study, article editing, Porkhovatyi S.Ya , Kazaryan G.G. – material collection and processing; Ozhogina E.V. – article writing.
Conflicts of interest: The authors confirm that they have no conflict of interest to declare.
Funding: The study was conducted without any sponsorship.
Ethical Approval: The study was approved by the Ethics Committee of the Faculty of Continuous Medical Education, RUDN University.
Patient Consent for Publication: The patients have signed informed consent for publication of their data.
Authors' Data Sharing Statement: The data supporting the findings of this study are available on request from the corresponding author after approval from the principal investigator.
For citation: Ozerskaya1 I.A., Porkhovatyi S.Ya., Kazaryan G.G., Ozhogina E.V. The influence of cytokine therapy on ultrasound assessment of uterine hemodynamics in treatment of chronic endometritis.
Akusherstvo i Gynecologia/Obstetrics and Gynecology 2024; 11: 128-136 (in Russian)
https://dx.doi.org/10.18565/aig.2024.176
Keywords
Chronic endometritis (CE) remains understudied pathology till the present day, and is associated with adverse reproductive outcomes, such as failed implantation and recurrent miscarriage [1]. Changing perception of the etiological factor of CE in recent decades, that confirms the important role of dissociations between facultative and obligate anaerobes and viruses, often leads to the development of clinically latent and atypical forms of the disease, which unconditionally complicate the diagnosis of CE and significantly reduce the effectiveness of classical treatment regimens [2–4].
The latent course of CE increases persistent damage duration and leads to the imbalance of proangiogenic and antiangiogenic factors caused by inflammatory process, occurrence of hypoxia, tissue ischemia, that ultimately causes impairment of the blood supply not only to the endometrium, but also to the uterus [5–7]. Anatomical and pathological changes are manifested by high vascular density and endothelial cell proliferation and edema associated with hyaline arteriolosclerosis, lumen occlusion, small vessel thrombosis and segmental fibrinoid necrosis [8].
Given that the inflammatory process negatively affects the uterine mucosa and is a cause of circulatory disorders, detection of vascular bed-specific pathology will improve the non-invasive diagnosis of CE. According to the International Endometrial Tumor Analysis (IETA) consensus statement it was proposed to use the IETA scoring method for ultrasound assessment of vascularization in the middle of the uterus – 4-point grading scale of 1 (vascularity) to 4 (hypervascularity), that can be applied in endometrial diseases, including CE [9]. The disadvantage of this subjective method includes dependency on doctor’s experience, scanner settings and specifications.
Spectral Doppler ultrasonography is used to measure the endometrial and myometrial vascular beds. However, spectral Doppler helps to evaluate the parameters only in one selected vessel, that may incorrectly reflect changes in blood flow through the entire organ [10].
Three-dimensional (3D) Doppler ultrasound helps to evaluate vascularization in the entire organ or its part, for example, in the uterus or endometrium, and is an appropriate tool for assessment of physiological and pathological changes in blood flow.
Treatment of CE starts with administration of antibacterial and/or antiviral drugs, followed by treatment that is aimed at restoring homeostasis, including adequate blood supply to the endometrium. The second stage includes hormonal, metabolic and immunomodulatory therapy, physiotherapy [11].
The studies in the recent years have reported the effectiveness of using local cytokine therapy, which includes a complex of natural antimicrobial peptides, cytokines and is a universal immune system stimulator, that has antibacterial, antiviral and antioxidant activity reducing inflammation with subsequent regeneration and epithelialization of damaged surface [12–18]. The studies have proven that cytokine therapy reduces inflammation and the level of autoimmune component, normalizes concentrations of pro- and anti-inflammatory cytokines, immunoglobulins in the endometrium. The authors reported rapid and stable eradication of the signs of the disease, that made it possible to increase sensitivity to antibacterial therapy, as well as reduce the recovery time of patients.
Cytokines are communicating mediators between the cells of the immune system and are involved in regulation of the immune response [19]. An additional dose of exogenous cytokines helps to improve the functional activity of cells with poor activity and suppresses excessive activity, that helps to normalize cell function. This assertion was confirmed in the study by Tapilskaya N.I. et al. (2022), where reduced counts of CD8+ T-cells and CD20+ B cells and, conversely, increased count of CD4+ T helper cells were found in the stromal component of the endometrium, that led to reduced signs of CE in a significantly larger number of patients who received antibacterial and cytokine therapy, compared with the standard course of treatment [20].
Thus, local cytokine therapy is one of the effective alternative methods for treatment of chronic inflammation in the endometrium, and administration of cytokine drugs is a promising augmentation to the complex treatment of CE. There were no works found in domestic and foreign literature, that are devoted to ultrasound examination of blood flow in the uterus including the endometrium, when cytokine drugs are included in the treatment regimen.
The objective of the study was to evaluate the effect of chronic endometritis treatment including cytokine therapy on uterine artery and endometrial blood flows.
Materials and methods
The retrospective cohort study included 298 women of reproductive age with 298 women of reproductive age with clinical and morphological diagnosis of CE.
The main group consisted of 140 patients, who received anti-inflammatory therapy including, including combinations of antibiotics, such as new-generation macrolides and nitroimidazole; macrolides and third-generation cephalosporins; beta-lactamase resistant penicillins and macrolides. The therapy was supplemented with antifungal, antiviral and immunomodulatory drugs. After concomitant flora was identified, antiprotozoal drugs, antimicrobial agents and antiseptics were indicated. Additionally, this group of patients received cytokine therapy as a single course of treatment with the drug “Superlymph” (25 U/1vaginal suppository at night,) for 20 days.
The comparison group consisted of 158 women, who received similar anti-inflammatory treatment, but without using exogenous cytokines. The clinicians indicated treatment in accordance with the standards of medical care in the Russian Federation and the current instructions for medical use of the drugs registered in the Russian Federation, that are published in the Register of Medicines (https://www.rlsnet.ru/).
The women with concomitant pathology, including endometriosis, uterine fibroids, the pathology of fallopian tubes and/or ovaries, were not included in the study.
Approval of the Ethics Committee of the Faculty of Continuous Medical Education, RUDN University, was obtained before this study began.
The patients have signed informed consent for publication of their data.
The age of patients in the main group was 34.7 (6.6) years, and in the comparison group – 33,5 (5,4) years.
The clinical diagnosis of CE was made based on the anamnestic data, complaints, and bimanual examination. Morphological diagnosis was based on the results of cytological and histological findings in the endometrium after hysteroscopy, morphological and immunohistochemical analysis of tissue samples obtained from endometrium by pipelle biopsy, and detection of plasma cells (CD138) and/or CD4, the anti-CD4, anti-CD8, anti-CD20 monoclonal antibodies.
Pelvic ultrasound was performed using the Affiniti70 device (Philips, the Netherlands) and volumetric intracavitary sensor for transvaginal access with subsequent image-based 3D reconstruction in the early proliferative phase of the menstrual cycle. The control examination was performed one month after the end of treatment, also in the early proliferative phase.
Quantitative assessment of the degree of vascularization of the uterus and endometrium was performed using QLAB software package for 3D angiographic reconstruction and measurement of vascularization index (VI), flow index (FI) and vascularization flow index (VFI).
Pulsed wave Doppler ultrasound of the uterine arteries (UA) was used to assess maximum blood flow velocity (Vmax), end-diastolic velocity (Vmin), mean blood flow velocity (Vmean), pulsatility index (PI) and resistance index (RI), as well as to measure the diameter of UA.
Subsequently, the value of arterial perfusion index (arterial PI) expressed as percentage was determined, which reflects the perfusion of 1 cm3 of the uterine body with blood incoming by the two UA. For this purpose, the volume of blood (in cm3) in one cardiac cycle in each uterine artery was calculated using the following formula:
Vvol = Vmean×S, where S is the area of uterine artery (cm2).
Arterial PI is calculated using the formula:
Arterial PI (%)= (Vvol (right UA) +Vvol (left UA)/UV×100,
where Vvol (right UA) is the volume of blood in the right uterine artery (см3); Vvol (left UA) is the volume of blood in the left uterine artery (см3); UV is uterine volume (см3).
Statistical analysis
IBM SPSS Statistics 27.0 (IBM, USA) was used for statistical analysis. Normality of distribution was tested using the Shapiro–Wilk test. Given that most of the data did not follow the normal distribution, all results are presented as median (Me) and interquartile range (Q1; Q3).
Comparison between two independent groups (the main group and the comparison group) was made using the nonparametric Mann–Whitney U test. Comparison between two related groups (arterial PI in the right UA and in the left UA before and after treatment in each group) was made using the nonparametric Wilcoxon test. The dynamic variable values was assessed as the difference between the values before and after treatment. The obtained values were tested for normality of distribution. The differences were described using Me, (Q1; Q3) and nonparametric criteria. Discrete data are represented as absolute value of the number (n) and relative value (%). The hypothesis of equality of means of binary matched-pairs data in the groups was tested using the McNemar test with Yates' correction.
The Spearman rank correlation coefficient was used to identify and assess relationship between two compared quantitative variables, and Chaddock scale was used for interpretation of correlation analysis. The threshold of statistical significance was at p<0.05.
Results
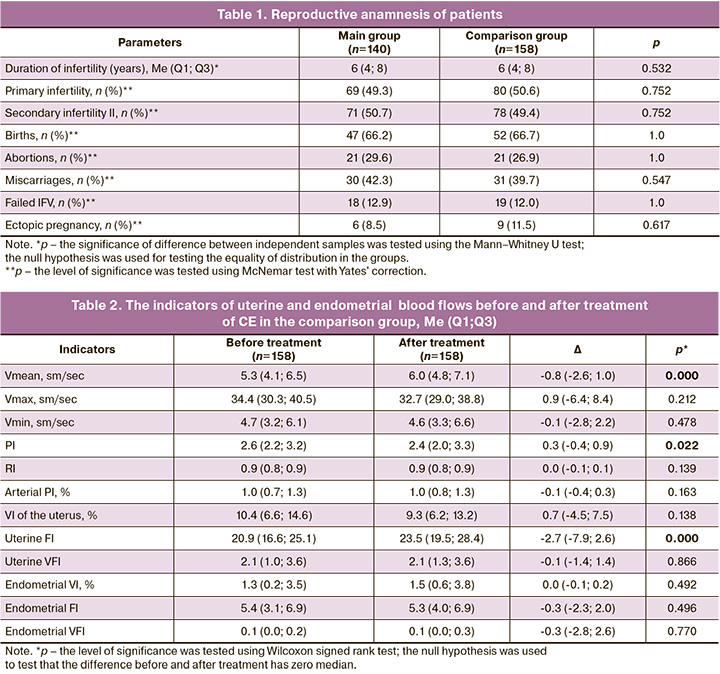
The age of patients was 34 (29; 44) years in the main group, and 33 (26; 42) years in the comparison group (p>0.05). Duration of infertility was 2–12 years in the main group, and 1– 13 years in the comparison group. There were no statistically significant differences between the groups in reproductive anamnesis (Table 1).
Analysis of blood flow in left and right uterine arteries found no asymmetric values (р>0,05).
Anti-inflammatory therapy in patients with CE in both groups led to changes in the hemodynamics of the uterus and endometrial blood flow. Thus, in the comparison group, the standard treatment demonstrated statistically significantly increased mean blood flow velocity (Vmean), reduced uterine artery pulsatility index (PI), increased uterine FI. In the main group, the use of cytokine therapy influenced vascularization of the uterus and endometrium, that was manifested by reduced uterine VI and VFI scores, as well as endometrial VI, FI and VFI scores (p<0.05), while it had no effect on the velocity indicators and angle-independent indices (Tables 2–4).
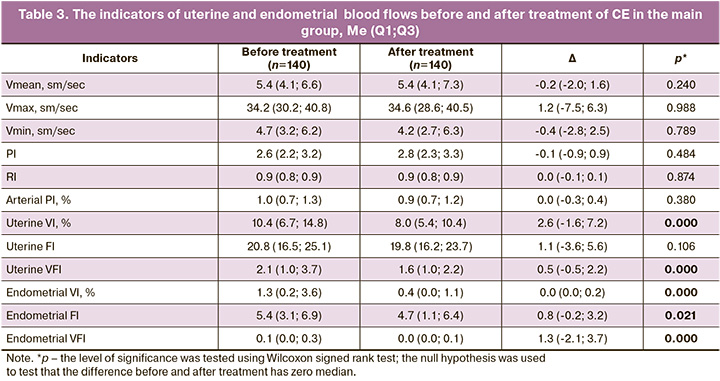
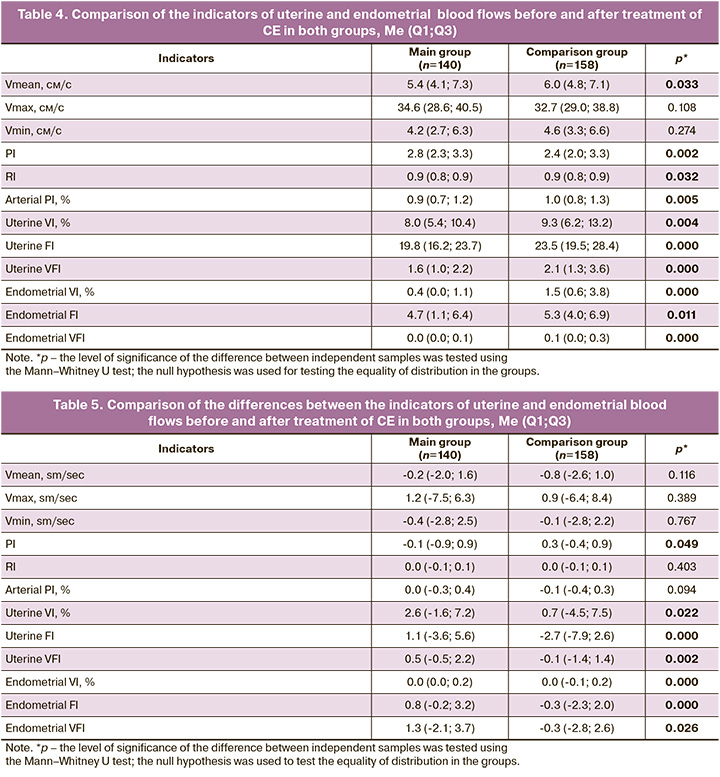
Cytokine therapy significantly potentiated the efficacy of anti-inflammatory therapy, that led to a marked decrease in vascularization both of the uterus and endometrium; while it had no significant influence on the uterine artery blood flow (Table 5).
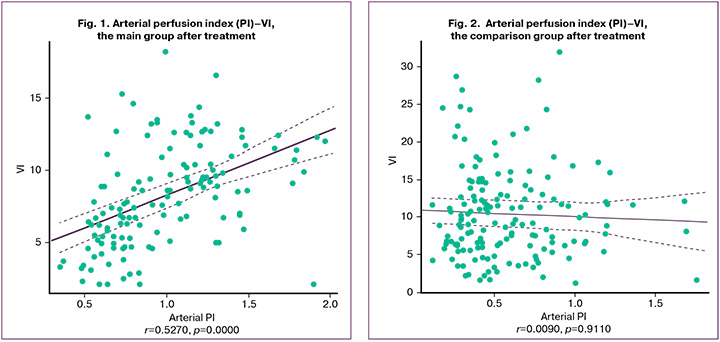
Before treatment, relationship closeness between arterial PI and uterine VI was r=-0.116, and between arterial PI and endometrial VI it was r=0.038. After treatment the values of these indicators were r= 0.527 (Fig.1) and r=0.261 in the main group, and r=-0.009 (Fig.2) and r= -0.014 in the comparison group, respectively.
Discussion
One of the links in the chain of pathophysiological processes in inflammation is a microcirculatory dysfunction in the lesion site, which is manifested by vasodilation, blood and lymphatic stasis, that ultimately leads to plasma exudation and leukocyte migration [5], which influence the degree of vascularization, both of the endometrium and the uterus, that has been previously proven [21, 22].
Despite wide application of color mapping in routine diagnostic practice, its possibilities are limited for determination of the degree of vascularization in tissues, when it is necessary to evaluate microcirculation of the vascular network, in particular, in the middle of the uterus, including the endometrium. The limitation of the method is interpretation of blood flow indicators in a single vessel in strict compliance to the certain insonation angle, that is not always possible, given the pronounced non-linear flow patterns of spiral and basal arterioles and veins, as well as their small lumen. The lack of relationship between the blood flow indicators in the UA and in the endometrium was reported by many authors [23–26]. According to Motovilova T.M. et al. (2013), Doppler ultrasound of the uterine blood vessels is of particular importance in dynamic monitoring to assess the effectiveness of treatment of chronic endometritis [27]. The authors indicate that impaired uterine arterial blood flow with predominant impairments in the basal and spiral arteries, as well as the difficulties in visualization of the terminal arteries indicate impaired tissue perfusion against the background of the chronic inflammatory process in the endometrium. According to endometrial Doppler data, the use of laser therapy led to pronounced positive dynamics in 78.2% of cases.
Using three-dimensional color Doppler sonography, VOCAL and Qlab software programs enabled objective assessment of the degree of vascularization and measurements of VI, FI and VFI.
To interpret this phenomenon, it was interesting to compare vascularization indices in the uterus and endometrium, which reflect arteriovenous oxygen saturation and arterial PI indicating arterial blood supply to the uterus. It was found that before treatment, there was absence of the strength of relationship between arteriovenous and arterial blood flow both in the uterus and endometrium. After treatment in the main group, relationship strength was high in the uterus, and low in the endometrium (r=0.261). In the comparison group, relationship strength in the uterus and endometrium was low. The analysis showed that the degree of vascularization depends not only on the inflowing arterial blood, but also on adequate venous outflow, which is impaired in CE. In the course of treatment, there are changes in hemodynamics of the uterine arteries, but not to the extent of restoration of venous blood outflow, which is more pronounced in the uterus. As a result of the use of cytokine therapy, impairment of venous outflow in the endometrium was successfully eliminated, while the similar effect was not achieved using the standard treatment regimen. This result demonstrates that impairment of uterine hemodynamics due to the venous link and minor changes in arterial blood flow can be restored by cytokine therapy, and also casts doubt on the advisability of assessment of the velocity indicators and angle-independent UA indices to evaluate the treatment effect of CE.
FI is a measure of the intensity of blood flow in the uterus. Despite statistically significant difference between the groups after treatment, FI was reduced with cytokine treatment augmentation (p>0.05), and increased in the group receiving standard therapy (p<0.05). This may arise from specific features of the myometrial microcirculatory bed, mainly due to the middle circular layer, represented by smooth muscle fibers, a large number of blood vessels, including veins. The contractile activity of the sub-endometrial layer of the myometrium through mechanical force on the vascular wall can improve venous and lymphatic drainage [27]. Apparently, for this reason, there was a significant difference in uterine artery FI between the main group and the comparison group.
In the work of Selezneva T.A. et al. (2016) studied the effect of a drug that stimulates the production of endogenous interferons and has anti-inflammatory and immunomodulatory effects on blood flow in the radial and basal branches of UA in women with CE [28]. It has been shown that complex treatment leads to reduction of RI in terminal branches of UA. However, the influence of treatment on blood flow in spiral arteries has not been assessed.
Ozerskaya I.A. et al. (2018) reported end-diastolic velocity increase in the early proliferative phase of the menstrual cycle in patients with endometritis, that led to the increased average blood flow velocity, which was also higher compared to healthy women, but not led to changes in arterial perfusion index [29]. Accordingly, confirmed reduction of Vmean in the main group was reflected in reduced arterial PI compared to the group of women, who received antibacterial therapy, and the difference was 5.1% (p<0.05), but no statistically significant deviations were found compared to the indicators before treatment.
Analysis of the obtained data confirms the fact that in the case of cytokine treatment augmentation to anti-inflammatory therapy of CE, redistribution in the arterial-venous bed and restoration of normal the microcirculatory blood flow occurs in such a way that the volume of blood in the afferent (arterial) vessels was the same as the volume of blood in the efferent (venous) link. This is demonstrated by reduced VI, FI and VFI of the uterus and the endometrium with fairly monotonous values of arterial PI, that leads to reduced exudation and the release of proinflammatory cytokines, and helps reduce the inflammatory process. It can also be suggested that uterine and endometrial hypervascularity during the inflammatory process is caused not by the increased arterial inflow, but by obstruction (or difficulty) of the venous and lymphatic outflow, which accompany inflammation.
It should be taken into account that dilated arcuate vessels сan also lead to myometrial hypervascularity based on high uterine VI values. However, diagnostically significant is a combination with endometrial hypervascularity.
Our study on ultrasound assessment of treatment effectiveness based on changes in uterine and endometrial blood flow can be considered to be one of the first studies related to this topic. Undoubtedly, further research is needed to clarify the specific features of endometrial blood supply in various morphotypes of CE, as well as the regimens and duration of treatment.
Conclusion
The effectiveness of anti-inflammatory therapy for chronic endometritis augmented with exogenous cytokines improves the hemodynamics of the uterus and endometrium by restoring venous outflow, that leads to normalization of endometrial blood flow and confirms the advisability of using Superlymph in complex treatment.
References
- Puente E., Alonso L., Laganà A.S., Ghezzi F., Casarin J., Carugno J. Chronic endometritis: old problem, novel insights and future challenges. Int. J. Fertil. Steril. 2020; 13(4): 250-6. https://dx.doi.org/10.22074/ijfs.2020.5779.
- Кулаков В.И., Шуршалина А.В. Хронический эндометрит. Гинекология. 2005; 7(5-6): 302-4. [Kulakov V.I., Shurshalina A.V. Chronic endometritis. Gynecology. 2005; 7(5-6): 302-4. (in Russian)].
- Зароченцева Н.В., Аршакян А.К., Меньшикова Н.С., Титченко Ю.П. Хронический эндометрит: этиология, клиника, диагностика, лечение. Российский вестник акушера-гинеколога. 2013; 13(5): 21-7. [Zarochentseva N.V., Arshakyan A.K., Men’shikova N.S., Titchenko Yu.P. Chronic endometritis: etiology, clinical features, diagnostics, treatment. Russian Bulletin of Obstetrician-Gynecologist. 2013; 13(5): 21-7. (in Russian)].
- Смирнова Д.В., Герасимов А.М., Кулида Л.В., Малышкина А.И., Вертелецкая Т.В., Васильева Н.В. Значение маркеров менструальной крови для диагностики хронического эндометрита у пациенток с бесплодием. Российский вестник акушера-гинеколога. 2023; 23(2): 19-25. [Smirnova D.V., Gerasimov A.M., Kulida L.V., Malyshkina A.I., Verteletskaya T.V., Vasil’eva N.V. The significance of menstrual blood markers for the diagnosis of chronic endometritis in patients with infertility. Russian Bulletin of Obstetrician-Gynecologist. 2023; 23(2): 19-25. (in Russian)]. https://dx.doi.org/10.17116/rosakush20232302119.
- Шанин В.Ю. Воспаление. Глава 12. В кн.: Шевченко Ю.Л., ред. Клиническая патофизиология. СПб.: Специальная литература; 1998: 170-97. [Shanin V.Yu. Inflammation. Ch. 12. In: Shevchenko Yu.L., ed. Clinical pathophysiology. St. Petersburg: Special literature; 1998: 170-97. (in Russian)].
- Радзинский В.Е., Ордиянц И.М., Добрецова Т.А. Эндометрий в огне. Острое и хроническое воспаление эндометрия: от новых взглядов к новым стратегиям. StatusPraesens. Гинекология, акушерство, бесплодный брак. 2016; 2: 126-32. [Radzinskii V.E., Ordiyants I.M., Dobretsova T.A. Endometrium on fire. Acute and chronic inflammation of the endometrium: from new views to new strategies. StatusPraesens. Gynecology, Obstetrics, Infertile Marriage. 2016; (2): 126-32. (in Russian)].
- Kitaya K., Yasuo T. Immunohistochemistrical and clinicopathological characterization of chronic endometritis. Am. J. Reprod. Immunol. 2011; 66(5): 410-15. https://dx.doi.org/10.1111/j.1600-0897.2011.01051.x.
- Buzzaccarini G., Vitagliano A., Andrisani A., Santarsiero C.M., Cicinelli R., Nardelli C. et al. Chronic endometritis and altered embryo implantation: a unified pathophysiological theory from a literature systematic review. J. Assist. Reprod. Genet. 2020; 37(12): 2897-911. https://dx.doi.org/10.1007/s10815-020-01955-8.
- Озерская И.А., Казарян Г.Г., Минашкина Е.В., Гус А.И. Использование дескрипторов Международной группы по анализу опухолей эндометрия (International Endometrial Tumor Analysis, IETA) для диагностики хронического эндометрита. Ультразвуковая и функциональная диагностика. 2023; 3: 50-66. [Ozerskaya I.A., Kazaryan G.G., Minashkina E.V., Gus A.I. International Endometrial Tumor Analysis (IETA) descriptors in the diagnosis of chronic endometritis. Ultrasound and Functional Diagnostics. 2023; (3): 50-66. (in Russian)]. https://dx.doi.org/10.24835/1607-0771-2023-3-50-66.
- Jokubkiene L., Sladkevicius P., Rovas L., Valentin L. Assessment of changes in endometrial and subendometrial volume and vascularity during the normal menstrual cycle using three-dimensional power Doppler ultrasound. Ultrasound Obstet. Gynecol. 2006; 27(6): 672-9. https://dx.doi.org/10.1002/uog.2742.
- Краснопольская К.В., Оразов М.Э., Ершова И.Ю., Федоров А.А. Тонкий эндометрий и бесплодие. 2-е изд. М.: ГЕОТАР-Медиа; 2022. 208с. [Krasnopol’skaya K.V., Orazov M.E., Ershova I.Yu., Fedorov A.A. Thin endometrium and infertility. 2nd ed. Moscow: GEOTAR-Media; 2022. 208p. (in Russian)].
- Доброхотова Ю.Э., Боровкова Е.И., Нугуманова О.Р. Улучшение процессов ангиогенеза и репродуктивных исходов у пациенток с хроническим эндометритом. Акушерство и гинекология. 2021; 3: 145-52. [Dobrokhotova Yu.E., Borovkova E.I., Nugumanova O.R. Improving angiogenesis processes and reproductive outcomes in patients with chronic endometritis. Obstetrics and Gynecology. 2021; (3): 145-52. (in Russian)]. https://dx.doi.org/10.18565/aig.2021.3.145-152.
- Дикке Г.Б., Остроменский В.В. Нарушение иммунного статуса при хроническом эндометрите и опыт его коррекции посредством локальной цитокинотерапии. Акушерство и гинекология. 2019; 9: 139-46. [Dikke G.B., Ostromenskii V.V. Impaired immune status in chronic endometritis and experience of its correction through local cytokine therapy. Obstetrics and Gynecology. 2019; (9): 139-46. (in Russian)]. https://dx.doi.org/10.18565/aig.2019.9.139-146.
- Оразов М.Р., Михалева Л.М., Семенов П.А., Орехов Р.Е., Лагутина Е.В. Эффективность лечения хронического эндометрита у женщин с неудачами имплантации в анамнезе. Трудный пациент. 2020; 18(8-9): 7-12. [Orazov M.R., Mikhaleva L.M., Semenov P.A., Orekhov R.E., Lagutina E.V. The effectiveness of treatment of chronic endometritis in women with a history of implantation failure. Difficult Patient. 2020; 18(8-9): 7-12. (in Russian)]. https://dx.doi.org/10.24411/2074-1995-2020-10053.
- Радзинский В.Е., Оразов М.Р., Токтар Л.Р., Михалева Л.М., Семенов П.А., Орехов Р.Е., Лагутина Е.В., Силантьева Е.С. Эффект «разбросанных пазлов»: имплантационные нарушения при хроническом эндометрите. Гинекология. 2020; 22(6): 93-100. [Radzinsky V.E., Orazov M.R., Toktar L.R., Mikhaleva L.M., Semenov P.A., Orekhov R.E., Lagutina E.V., Silantyeva E.S. The scattered puzzle effect: implantation disorders in chronic endometritis. Gynecology. 2020; 22(6): 93-100. (in Russian)]. https://dx.doi.org/10.26442/20795696.2020.6.200493.
- Дикке Г.Б., Суханов А.А., Остроменский В.В., Кукарская И.И. Течение и исходы беременности у пациенток с хроническим эндометритом и нарушением репродуктивной функции, получавших комплексное лечение с использованием препарата «Суперлимф» (рандомизированное контролируемое испытание в параллельных группах «ТЮЛЬПАН»). Акушерство и гинекология. 2023; 4: 132-44. [Dikke G.B., Sukhanov A.A., Ostromensky V.V., Kukarskaya I.I. Course and outcomes of pregnancy in patients with chronic endometritis and impaired reproductive function after receiving complex treatment with drug Superlymph: randomized control trial in parallel groups “TULIP”. Obstetrics and Gynecology. 2023; (4): 132-44. (in Russian)]. https://dx.doi.org/10.18565/aig.2023.74.
- Боровиков И.О., Булгакова В.П., Боровикова О.И., Никогда Ю.В., Бирюкова М.И. Подготовка к проведению экстракорпорального оплодотворения пациенток с «тонким» эндометрием - возможности цитокинотерапии. Проблемы репродукции. 2023; 29(3): 31-9. [Borovikov I.O., Bulgakova V.P., Borovikova O.I., Nikogda Yu.V., Biryukova M.I. Preparation for in vitro fertilization of patients with a «thin» endometrium - the possibilities of cytokine therapy. Russian Journal of Human Reproduction. 2023; 29(3): 31-9. (in Russian)]. https://dx.doi.org/10.17116/repro20232903131.
- Суханов А.А., Дикке Г.Б., Кукарская И.И. Эпидемиология женского бесплодия и опыт восстановления репродуктивной функции у пациенток с хроническим эндометритом в Тюменском регионе. Проблемы репродукции. 2023; 29(3): 98-107. [Sukhanov A.A., Dikke G.B., Kukarskaya I.I. Epidemiology of female infertility and the experience of recovery of reproductive function in patients with chronic endometritis in the Tyumen region. Russian Journal of Human Reproduction. 2023; 29(3): 98-107. (in Russian)]. https://dx.doi.org/10.17116/repro20232903198.
- Melo P., Thornton T., Coomarasamy A., Granne I. Evidence for the effectiveness of immunologic therapies in women with subfertility and/or undergoing assisted reproduction. Fertil. Steril. 2022; 117(6): 1144-59. https://dx.doi.org/10.1016/j.fertnstert.2022.04.015.
- Тапильская Н.И., Толибова Г.Х., Савичева А.М., Копылова А.А., Глушаков Р.И., Будиловская О.В., Крысанова А.A., Горский А.Г., Гзгзян А.М., Коган И.Ю. Эффективность локальной цитокинотерапии хронического эндометрита пациенток с бесплодием. Акушерство и гинекология. 2022; 2: 91-100. [Tapilskaya N.I., Tolibova G.Kh., Savicheva A.M., Kopylova A.A., Glushakov R.I., Budilovskaya O.V., Krysanova A.A., Gorskii A.G., Gzgzyan A.M., Kogan I.Yu. The effectiveness of local cytokine therapy for chronic endometritis in patients with infertility. Obstetrics and Gynecology. 2022; (2): 91-100. (in Russian)]. https://dx.doi.org/10.18565/aig.2022.2.91-100.
- Озерская И.А., Казарян Г.Г. Ультразвуковая диагностика эндометрита: особенности кровоснабжения разных морфологических типов. Вестник Российского университета дружбы народов. Серия: Медицина. 2019; 23(2): 147-55. [Ozerskaya I.A., Kazaryan G.G. Ultrasound diagnostics of endometritis: features of blood supply of different morphological types. Bulletin of Peoples' Friendship University of Russia. Series: Medicine. 2019; 23(2): 147-55. (in Russian)]. https://dx.doi.org/10.22363/2313-0245-2019-23-2-147-155.
- Озерская И.А., Иванов В.А., Порховатый С.Я., Казарян Г.Г. Особенности кровоснабжения матки у женщин с хроническим эндометритом в зависимости от длительности бесплодия. Акушерство и гинекология. 2020; 10: 105-12. [Ozerskaya I.A., Ivanov V.A., Porkhovatyi S.Ya., Kazaryan G.G. Features of the blood supply to the uterus in women with chronic endometritis depending on the duration of infertility. Obstetrics and Gynecology. 2020; (10): 105-12. (in Russian)]. https://dx.doi.org/10.18565/aig.2020.10.105-112.
- Friedler S., Schenker J.G., Herman A., Lewin A. The role of ultrasonography in the evaluation of endometrial receptivity following assisted reproductive treatments: a critical review. Hum. Reprod. Update. 1996; 2(4): 323-35. https://dx.doi.org/10.1093/humupd/2.4.323.
- Ng E.H., Chan C.C., Tang O.S., Yeung W.S., Ho P.C. Relationship between uterine blood flow and endometrial and subendometrial blood flows during stimulated and natural cycles. Fertil. Steril. 2006; 85(3): 721-7. https://dx.doi.org/10.1016/j.fertnstert.2005.09.051.
- Chwalisz K., Garfield R.E. Role of nitric oxide in implantation and menstruation. Hum. Reprod. 2000; 15(Suppl. 3): 96-111. https://dx.doi.org/10.1093/humrep/15.suppl_3.96.
- Ouyang Y., Peng Y., Mao Y., Zheng M., Gong F., Li Y. et al. An endometrial receptivity scoring system evaluated by ultrasonography in patients undergoing frozen-thawed embryo transfer: a prospective cohort study. Front. Med. (Lausanne). 2024; 11: 1354363. https://dx.doi.org/10.3389/fmed.2024.1354363.
- Мотовилова Т.М., Качалина Т.С., Аникина Т.А. Альтернативный подход к лечению больных с хроническим неспецифическим эндометритом. Российский медицинский журнал. 2013; 21(14): 751-4. [Motovilova T.M., Kachalina T.S., Anikina T.A. Alternative approach to the treatment of patients with chronic nonspecific endometritis. Russian Medical Journal. 2013; 21(14): 751-4. (in Russian)].
- Селезнева Т.А., Аболонина О.В., Стовбун С.В., Коробкова Е.В., Кучеров В.А. Комбинированное лечение больных с хроническим эндометритом. Российский вестник акушера-гинеколога, 2016; 16(5): 50-4. [Selezneva T.A., Abolonina O.V., Stovbun S.V., Korobkova E.V., Kucherov V.A. Combined treatment of patients with chronic endometritis. Russian Bulletin of Obstetrician-Gynecologist. 2016; 16(5): 50-4. (in Russian)]. https://dx.doi.org/10.17116/rosakush201616550-54.
- Озерская И.А., Семилетова А.А., Казарян Г.Г. Ультразвуковая диагностика эндометрита: особенности гемодинамики матки. Медицинская визуализация. 2018; 22(6): 82-96. [Ozerskaya I.A., Semiletova A.A., Kazaryan G.G. Ultrasound diagnostics of endometritis: features of uterine hemodynamics. Medical Visualization. 2018; 22(6): 82-96. (in Russian)]. https://dx.doi.org/10.24835/1607-0763-2018-6-82-96.
Received 22.07.2024
Accepted 28.10.2024
About the Authors
Irina A. Ozerskaya, Dr. Med. Sci., Professor at the Department of Ultrasound Diagnostics, Faculty of Continuous Medical Education of the Medical Institute, Peoples’ Friendship University of Russia named after Patrice Lumumba, 117198, Russia, Moscow, Miklukho-Maklaya str., 6, +7(499)936-87-87, ozerskaya_usd@mail.ru,https://orcid.org/0000-0001-8929-6001
Sergei Ya. Porkhovatyi, PhD, Ultrasound Diagnostics Doctor, Asklepion Medical Center, 125222, Russia, Moscow, Dubravnaya str., 41, bldg. 2, +7(495)759-99-50, oracul2003@gmail.com, https://orcid.org/0009-0002-7263-1568
Gayane G. Kazaryan, PhD, Head of the Ultrasound Department, Medscan Medical Center, 119421, Russia, Moscow, Obrucheva str., 21A, +7(495)859-29-45,
79165521271@yandex.ru, https://orcid.org/0000-0002-1198-8187
Ekaterina V. Ozhogina, PhD, Leading Reproductive Specialist, Center for Reproduction and Genetics “Nova Clinic”, 119415, Russia, Moscow, Lobachevsky str., 20, +7(495)476-61-19, ozhogina.caterina@yandex.ru, https://orcid.org/0009-0007-5205-2901
Corresponding author: Irina A. Ozerskaya, ozerskaya_usd@mail.ru