Predicting the success of in vitro fertilization in patients with chronic endometritis and reproductive disorders using neural network technology (secondary analysis of the results of the TULIP-2 randomized controlled trial)
Sukhanov A.A., Dikke G.B., Mudrov V.A., Kukarskaya I.I.
When assisted reproductive technologies are used, recurrent implantation failures are observed in 7.7–67.5% of patients with chronic endometritis (CE).
Objective: To develop a predictive model of the probability of clinical pregnancy and live birth in women with uterine infertility due to CE using neural network technology at the stage of selection for in vitro fertilization (IVF) programs with cryotransfer and evaluate the effectiveness of this model.
Materials and methods: The secondary analysis of the results of the TULIP-2 randomized controlled trial was carried out. A total of 188 patients who met the objectives of this analysis were selected from the electronic database. The patients were divided into two comparison groups: group I (n=102) included patients who became pregnant, group II (n=86) included those who did not become pregnant.
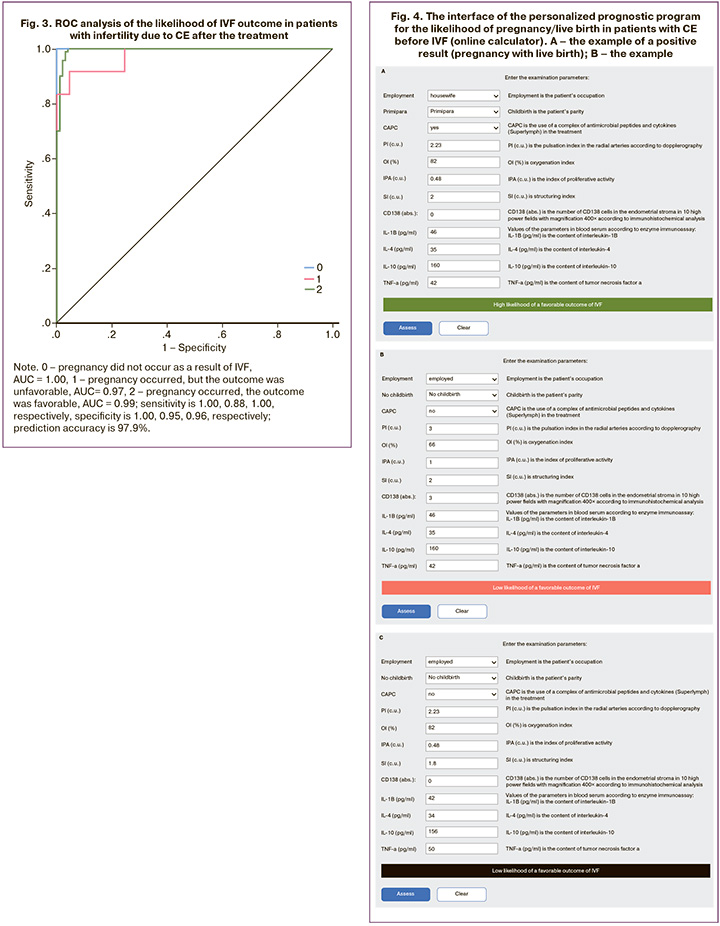
Results: The model of predicting the success of IVF was created on the basis of 11 most significant parameters, which were identified after obtaining the results of the logistic analysis. The model was made using neural network technology. In order to predict the outcome of IVF, the following indicators were included in the structure of the multilayer perceptron: treatment, which included a complex of antimicrobial peptides and cytokines, CD-138, pulsation index in radial arteries according to Dopplerometry, oxygenation indices, proliferative activity, structuring according to laser conversion testing, interleukins such as -4, -10, -1ß, tumor necrosis factor-α according to enzyme immunoassay. The accuracy of the prediction was 97.9% (sensitivity is 100.0%, specificity is 96.4%). The information value of the model was confirmed by ROC analysis, the area under the curve (ROC-AUC) was 0.9, p<0.001. An online calculator was developed for the practical use of the model of individual prediction of IVF success.
Conclusion: The model of predicting clinical pregnancy and live birth as a result of IVF in patients with infertility caused by chronic endometritis, using neural network technology, has a high predictive accuracy and makes it possible to determine the need for administering another course (courses) of treatment for chronic endometritis or making a decision on the IVF procedure.
Authors’ contributions: Sukhanov A.A. – collection of clinical material, formation of an electronic database, writing fragments of the article and editing the article; Dikke G.B. – development of the concept, design and program of the study, supervision during the study, analysis of the results of statistical processing of clinical material and their interpretation, search for literary sources, writing fragments of the article and editing the article after reviewing; Mudrov V.A. – development of the study program, statistical processing of clinical material, analysis of results, development of the prognostic model using neural network technology and its interpretation, writing the program for an online calculator, writing a fragment of the article and editing the article after reviewing; Kukarskaya I.I. – conducting the study in the clinic, supervision during the study.
Conflicts of interest: The authors report no conflicts of interest and guarantee that the article is the original work of the authors.
Funding: The study was carried out using own resources. The publication of the article was supported by Pentcroft Pharma Company.
Ethical Approval: The study was approved by the Ethical Review Board of the Perinatal Medical Center, Tyumen, Russia).
Authors' Data Sharing Statement: The data supporting the findings of this study are available on request from the corresponding author after approval from the principal investigator.
For citation: Sukhanov A.A., Dikke G.B., Mudrov V.A., Kukarskaya I.I. Predicting the success of in vitro fertilization in
patients with chronic endometritis and reproductive disorders using neural network technology
(secondary analysis of the results of the TULIP-2 randomized controlled trial).
Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2024; (4): 103-114 (in Russian)
https://dx.doi.org/10.18565/aig.2024.47
Keywords
Recurrent implantation failures following assisted reproduction treatment are observed in 7.7–67.5% of patients with reproductive disorders associated with chronic endometritis (CE) [1, 2]. The effectiveness of in vitro fertilization (IVF) in patients with CE does not exceed 30% per treatment cycle and it is even lower in women over 36 years of age [3].
The diagnosis of CE, its treatment and management of infertility using IVF are associated with the increased time interval before the expected pregnancy, an adverse effect on the psychological and emotional state of the couple, and high costs. These factors can be minimized if there is information about the expected success of IVF before undergoing this treatment [4]. However, the existing tools for determining predictors of success have not been widely used in routine clinical practice due to their complexity, low predictive accuracy and questionable clinical benefit.
Thus, a systematic review and meta-analysis of 22 studies assessed the clinical significance of endometrial thickness for the outcome of IVF, and the authors concluded that it is not possible to predict pregnancy and live birth using this parameter [5]. A later systematic review of 20 studies made a gentler conclusion: the results of IVF in patients with impaired endometrial receptivity depend not only on the thickness of the endometrium, but also on a number of other risk factors, both in the cycles of fresh embryo transfer and frozen embryo transfer. In order to improve endometrial receptivity, it is necessary to use a personalized approach with effective diagnostic and treatment methods; moreover, it is important to continue research on the significance of endometrial thickness, treatment protocols, and other factors [6].
Currently, there are models for predicting the probability of live birth after one to three IVF cycles, where multiple clinical and laboratory parameters are used (one of the studies includes up to 100 variables), as well as the number of extracted oocytes, which give a limited prognostic accuracy of less than 60%, AUC ranging from 0.51 to 0.60 [7–10]. McLernon D.J. et al. (2016) gave an individual assessment of the cumulative chances of a couple to have a child after six consecutive IVF cycles using parameters which were obtained both before treatment and after the first transfer of fresh embryos (the index of prognostic value for the model before IVF was 0.73, and it was 0.72 after the first cycle); all characteristics of patients and treatment had a statistically significant univariate relationship with live birth, except for unexplained infertility [11]. The models developed by Xu T. et al. (2022) are limited to predicting pregnancy immediately after the IVF cycle, but not live birth, with an accuracy of 68% [12]. It is worth noting that there was a study where the authors assessed the possibility of predicting the probability of a live birth in the first IVF cycle before performing it and developed three models based on an independent data set; the model which included the anti-mullerian hormone parameter had a prognostic accuracy of 71% [13]. A systematic review carried out in 2020 assessed the quality of 35 models predicting IVF results and noted that the model developed by McLernon was the most qualitative and informative [14].
However, the limited amount of the findings does not allow the clinicians to use the entire array of obtained biological parameters and determine their value for the prognosis; that is why predictive models based on modern algorithms, such as neural networks, are actively introduced into medical practice [15]. Despite promising data, artificial intelligence (AI) has not received the status of the gold standard yet; therefore, there was a systematic review of 18 studies aimed at evaluating the predictive capabilities of AI-based models [16]. The synthesis of the data obtained from this analysis showed that such models are able to predict accurately the outcome of IVF in terms of clinical pregnancy with fetal heartbeat (72%) and live birth (90%).
VerMilyea M. et al. (2022) applied deep learning (medical image analysis) to predict embryo viability based on microscopy; the cumulative accuracy was 64% for both viable and non-viable embryos, and it demonstrated the reliability of the model and its generalizability, exceeding the result by 42% compared with the assessment by embryologists [17]. Mihara M. et al. (2023) described the use of deep learning for the diagnosis of CE based on histological and immunohistochemical patterns and noted the potential for improving diagnosis, overcoming the disunity of histological and hysteroscopic assessments, the development of standardized diagnostic criteria and uniform clinical recommendations for this disease [18].
Along with this, scientific and practical interest regarding the prognosis of pregnancy/live birth following IVF in patients with endometritis-associated infertility (implantation defect, unexplained infertility) remains strong; studies on the search for predictors of the success of this intervention after the treatment of CE have not been conducted and, therefore, this issue is relevant for modern reproductive medicine.
The aim of the study was to develop a predictive model of the probability of clinical pregnancy and live birth in women with endometritis-associated infertility using neural network technology at the stage of selection for in vitro fertilization (IVF) programs with cryotransfer and evaluate the effectiveness of this model.
Materials and Methods
Design. This the secondary analysis of the results of the study “The course and outcomes of pregnancy resulting from in vitro fertilization in patients with chronic endometritis who received complex treatment using the Superlymph drug at the preconception stage” (the TULIP-2 randomized controlled trial) [19].
Materials. The data of 600 female patients from the electronic database were used in the study. The women were diagnosed with uterine infertility, implantation defect (N97.2), chronic inflammatory uterine disease (N71.1) which were confirmed histologically and immunohistochemically; the patients met the inclusion/exclusion criteria, they underwent treatment for CE and IVF (cryopreservation) in the Perinatal Medical Center (Tyumen, Russia) from September 2019 to June 2023. The treatment of CE administered at the preconception stage included antibacterial therapy, progestogens in the second phase of the cycle, and a complex of natural antimicrobial peptides and cytokines. The current analysis included 188 patients from this database who had a complete data set of clinical, functional, laboratory, histological, immunohistochemical findings, enzyme immunoassay and laser conversion (Foton-Bio spectrometer) before and after the treatment (patients with missing data were excluded from the analysis). The patients were divided into two comparison groups: group I (n=102) included patients who became pregnant, group II (n=86) included those who did not become pregnant.
The main research results are the creation of predictors and a model for the prognosis of pregnancy/live birth following frozen embryo transfer in the IVF cycle, a personalized prediction program (online calculator) to assess the individual chance of pregnancy/live birth in patients with CE before IVF.
Statistical analysis
Statistical data analysis was performed in accordance with the principles of the International Committee of Medical Journal Editors (ICMJE) and the recommendations “Statistical Analysis and Methods in the Published Literature” (SAMPLE). Statistical processing of the research results was carried out using the IBM SPSS Statistics Version 25.0 software package (International Business Machines Corporation, USA). The normality of the data distribution was determined using the Kolmogorov–Smirnov test. Taking into account the distribution of quantitative variables, which is different from normal in most cases, the data obtained are presented in the form of the median, the first and third quartiles, Me (Q1; Q3). Nominal data were described with absolute values (n) and percentage (%). The comparison of independent parameters between the groups was carried out using the Mann–Whitney U test; quantitative parameters were measured in two stages (before and after treatment) and evaluated using the Wilcoxon rank T-test, which was automatically converted to the Z value (z-score) at the conclusion of SPSS. The comparison of independent nominal data was carried out using Pearson’s chi-squared (χ2) test, while a likelihood correction was applied in small samples, the Yates’ correction for continuity was used for the sample with a number of observations less than 10, and the Fisher’s exact test was used for the number of observations less than 5. The McNemar χ2 test was used to compare two dependent groups of the nominal data. In all cases, p<0.05 was considered statistically significant in type I and type II errors α=5% and β=20%, respectively. Correlations between the studied parameters were determined using the Spearman correlation coefficient, and the connection strength was determined on the Chaddock scale.
Neural network analysis. In order to create a prognosis model, the multilayer perceptron was used (the Neural Networks module of the IBM SPSS Statistics V. 25.0 program (IBM Corporation, USA)). Statistically significant parameters were included in the samples used for training (n=188) and testing (n=57). The test sample was generated using the randomization method. The diagnostic informative value of the prognosis model was determined with the help of ROC analysis.
Results
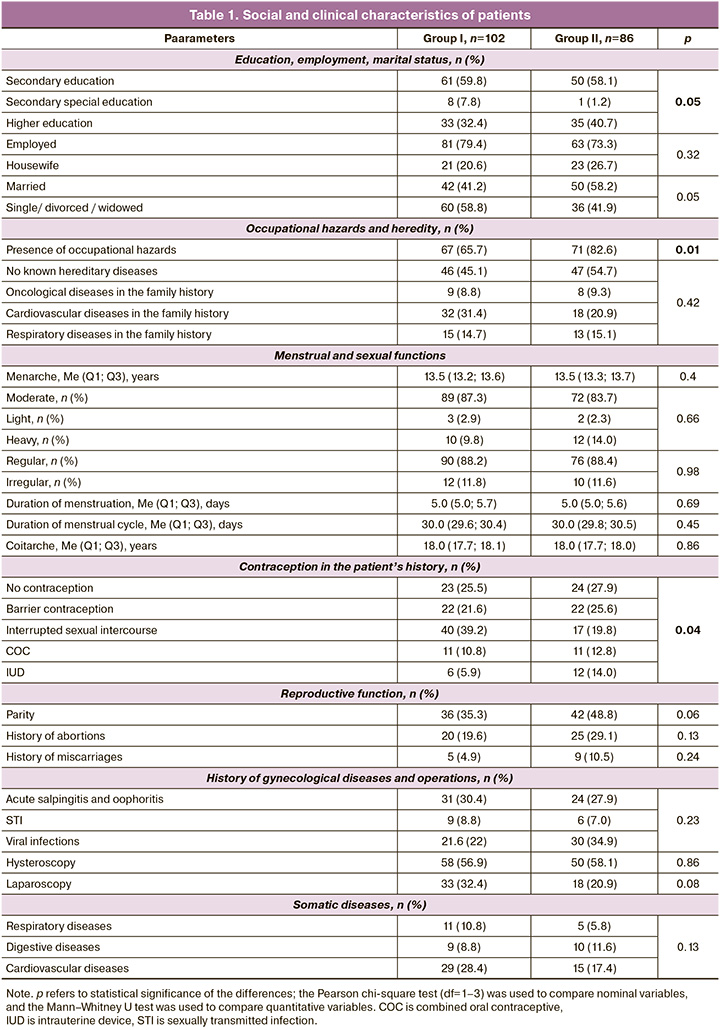
General information about the patients. The age of the patients ranged from 18 to 45 years, Me (Q1; Q3) = 36.0 (35.1; 36.1) and 36.0 (35.1; 36.1) years in groups I and II, respectively (p=0.89). The social and clinical characteristics of the patients are presented in Table 1; the analysis of the data showed the difference between the groups in terms of education, marital status, occupational hazards, and methods of contraception.
The duration of infertility up to 5 years was observed in 78.4% (80/102) and 73.3% (63/86) of patients, infertility for 5 years or more was in 21.6% (22/102) and 26.7% (23/86), respectively, p=0.41 and averaged 2.0 (2.0; 3.2) and 2.0 (2.0; 3.3) years, respectively, p=0.51.
The treatment performed in the preconception period did not have any statistically significant differences in the composition of medications, namely, all patients received antibacterial therapy; progestogen in the second phase of the cycle was taken by 51.0% (52/102) and 55.8% (48/86) of patients, p=0.51; the complex of natural antimicrobial peptides and cytokines was taken by 67.6% (69/102) and 55.8% (48/86) of women, p=0.1, respectively.
Results of the functional and laboratory research methods. The dynamics of the parameters of ultrasound and laser conversion testing are presented in Table 2.
The parameters of ultrasound and dopplerometry, as well as laser conversion testing after treatment, showed significant improvements in both groups. However, these improvements were statistically significantly greater in patients from group I compared to those in group II.
A similar conclusion can be made regarding the results of immunohistochemical study and enzyme immunoassay (Table 3).
IVF outcomes
Among the patients of group I, 88.2% (90/102) of the pregnancies ended in live birth or 47.9% of pregnancies in the total number of treated patients ended in live birth (90/188). The duration of infertility among patients with a favorable outcome was 1.0 (1.0; 2.7) years, while those with an unfavorable outcome were infertile for 2.0 (2.0; 3.3) years (p=0.08). Termination of pregnancy in patients with a favorable outcome occurred after 39.0 (37.4; 39.0) weeks, while termination of pregnancy in patients with an unfavorable outcome occurred after 8.0 (7.6; 11.3) weeks (p<0.001).
The absence of live birth in group I (n=12) was associated with spontaneous miscarriage before 12 weeks in 83.4% (10/12) of cases, before 22 weeks – in 8.3% (1/12), antenatal fetal death – in 8.3% (1/12). Other pregnancy complications (premature birth, preeclampsia, abruptio placentae, hypoxia and fetal growth retardation) ranged from an average of 6.6 and 9.4% of cases in groups I and II, respectively, which was statistically comparable (p=0.36).
The condition of newborns was assessed according to the Apgar scale in the first and fifth minute of life and it was 8.0 (7.4; 8.0) and 8.0 (7.8; 8.0) scores, respectively; the weight of newborns was 3300.0 (3116.2; 3291.0) g.
Predictors and prognosis model of pregnancy/live birth following IVF
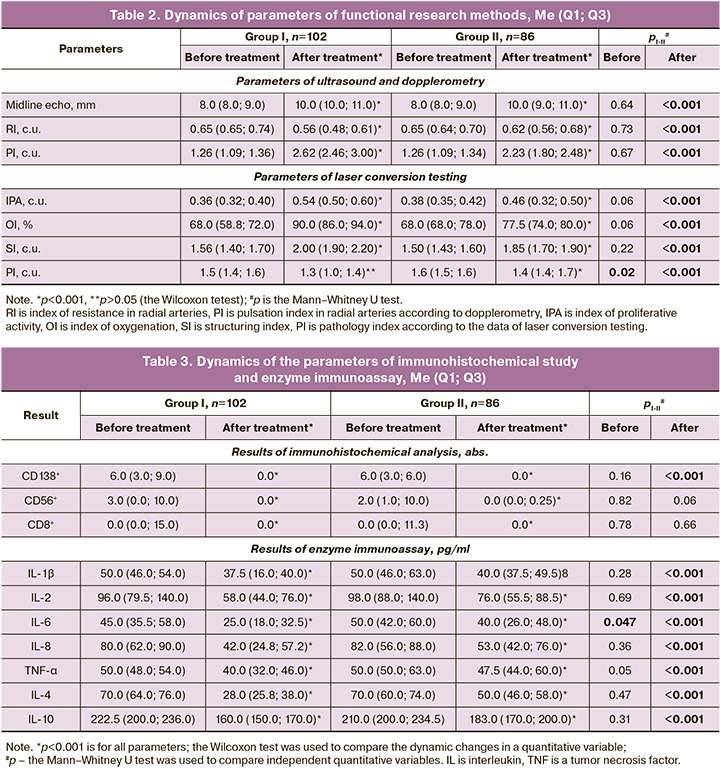
As it is necessary to exclude multicollinearity between the correlating parameters of the research methods, it was decided to use only the most important parameters (predictors) when creating a model for the prognosis of the IVF outcome in patients with infertility after treatment of CE. The multilayer perceptron procedure was chosen for this purpose. There were 11 input-layer neurons, which were the parameters of the study (presence or absence of a complex of antimicrobial peptides and cytokines in the treatment, quantitative variables after treatment, pulsation index in radial arteries, indices of oxygenation, structuring and proliferative activity according to laser conversion testing, CD138 and cytokine interleukin (IL)-4, IL-10, IL-1β and tumor necrosis factor (TNF)-α) that had not only significant differences when comparing the studied groups, but also pathogenetic significance.
Considering the number of input-layer neurons, two hidden layers were included in the architecture of the multilayer perceptron. The automatic choice of architecture made it possible to calculate the optimal number of neurons in these hidden layers, equal to 8 and 6, respectively, that would allow the scientists to predict the outcome as efficiently as possible. The architecture of the developed neural network is shown in Figure 1.
A hyperbolic tangent was used to create a relationship between weighted sums of objects with a subsequent layer of variables of these objects in both hidden layers and in the output layer. The sum of squares was used as the error function. The output layer contained 3 target (dependent) variables (0 – pregnancy did not occur as a result of IVF, 1 – pregnancy occurred, but the outcome was unfavorable, 2 – pregnancy occurred, the outcome was favorable).
The IBM SPSS Neural Network module uses an error back propagation algorithm to train a neural network. When training a neural network, the weights of each neuron are determined by optimizing the loss or cost function. The error back propagation algorithm is based on an iterative process in which the weights of each neuron on each layer are updated in order to minimize the error of the model. Errors are calculated as the difference between the predicted values of the neural network and the real values. The process of updating the weights is performed using the gradient descent method, which adjusts the values of the weights in the direction opposite to the gradient of the loss function. The dependent variable can be predicted more accurately using this model. Thus, the weight of each neuron is determined according to its importance in predicting the dependent variable and is iteratively updated during the learning process of the neural network.
The importance of the above parameters in the structure of the developed neural network, which makes it possible to predict the probability of clinical pregnancy and live birth in patients with infertility and CE, is shown in Figure 2.
The informative value of the prediction. It is worth noting that it is not difficult for the neural network to predict both the pregnancy with a favorable outcome and the negative result of IVF.
The prediction accuracy of the developed model was 97.9%. The developed neural network has high sensitivity (100%) and specificity (96%) for predicting a positive outcome, namely, the clinical pregnancy as a result of IVF and live birth in patients with CE. These parameters are also quite high for pregnancy with an unfavorable outcome: sensitivity (88%) and specificity (95%), but the diagnostic accuracy is low (66.7%).
The informative value of neural network data analysis in predicting the IVF outcome in patients with infertility due to CE is confirmed by the ROC analysis (Fig. 3).
It should be noted that when laser conversion testing data are excluded from the structure of the neural network, the accuracy of the prediction decreases to 94.7%, which determines its significant diagnostic role. Cross-validation was used to confirm the optimal choice of the initial architecture of the multilayer perceptron; therefore, it was possible to evaluate the performance of the model with different architecture parameters. During the comparison of models, it was determined that the original version has the highest accuracy on all folds.
The testing of the neural network on a sample of 57 patients showed that the percentage of incorrect predictions was 5.3% (3/57).
Thus, the developed prognostic model of pregnancy and live birth after treatment of CE in patients with impaired reproductive function using neural network technology is effective with a prediction accuracy of 97.9%.
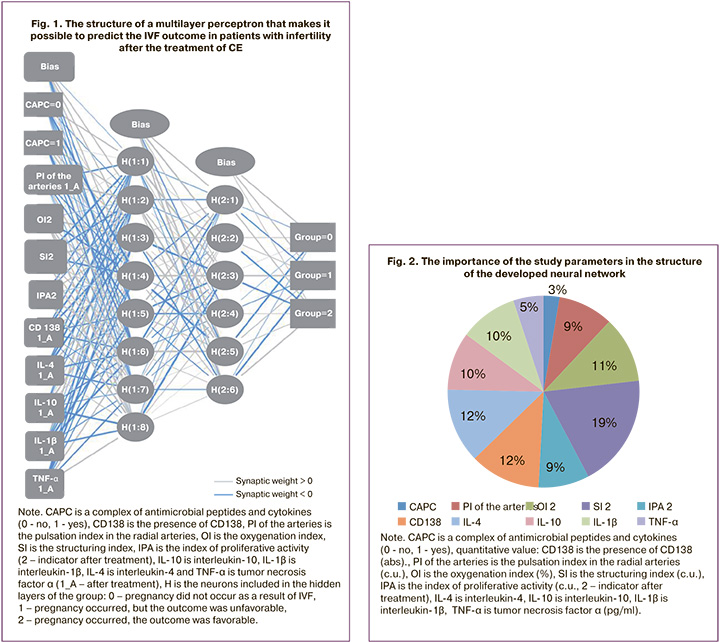
Personalized Prognostic Program
For practical purposes, a personalized prognostic program (online calculator) was developed to assess the individual likelihood of pregnancy/live birth in patients with CE before IVF. Besides the parameters, the importance of which was confirmed by neural network technology, two more parameters were added to this program, namely, employment and a previous history of childbirth, which help differentiate patients who had a pregnancy that ended in a live birth from patients with an unfavorable pregnancy outcome.
The interface of the program with variants of results based on the example of an individual prognosis for three patients is shown in Figure 4.
Thus, it is possible for a doctor in routine clinical practice to use this program for making a decision on the readiness of the endometrium for egg implantation and IVF procedure (if the test result is positive), or on the need for additional courses of treatment for CE (if the test result is dubious or negative).
Discussion
According to recent studies, infertility is caused by the inability of the embryo to implant, and CE is one of the main reasons affecting this process [20–23]. The methods of treatment of CE before IVF have a significant impact on the pregnancy rate. Thus, this parameter was significantly higher when patients received antibacterial therapy than those who did not receive treatment – 43.2% vs. 27.3%, respectively [20], in case of taking the complex of myo-inositol/folic acid – 53% vs. 33% [24], natural antimicrobial peptides and cytokines as part of complex therapy – 57% vs. 38.7% [19], with intrauterine administration of peripheral blood mononuclear cells, OR=2.35 [25]. However, about 50% of IVF cycles remain unsuccessful, and this leads to the need for repeated courses of treatment for CE, new IVF attempts, and additional financial costs; all these factors determine the search for predictors of IVF success.
A modern method of neural network technology which demonstrated its promise in earlier studies in obstetrics and gynecology [26–28], including reproduction and embryology [29–31], could be used for predicting IVF success. The use of neural network technology allowed us to select 11 of the most significant predictors of IVF success from 75 parameters included in the electronic database of patients.
Unlike the study of Hansen K.R. et al. [32] and other studies that indicated age as an important factor determining the success of conception in both natural and IVF cycles, we were unable to identify it as a prognostic parameter in this study, since the age range of the patients included in the analysis was very narrow [(Q1; Q3)=(35.1; 36.1) years old]. The parameter ‘duration of infertility’ turned out to be insignificant, and it is not consistent with the opinion of other authors, including our previous study [19, 33-35]; this could be explained by the treatment of CE with the certain therapy and restoration of endometrial receptivity.
There was a clear relationship between the resolution of CE (absence of CD138 plasma cells in the endometrial stroma), the intake of a complex of natural antimicrobial peptides and cytokines, a progestogen and an antibiotic and an increase in the rate of pregnancy and live birth. This observation is consistent with the conclusions of other researchers that treatment of CE with its resolution provides more chances for successful pregnancy and live birth, in contrast to persistent CE [36].
Such parameters as the pulsation index in the radial arteries of the uterus according to dopplerometry, serum cytokine levels, and parameters obtained by laser conversion testing have not been previously studied as predictors of pregnancy/live birth in IVF programs. In this analysis, these parameters are identified as important ones using neural network technology and they are significant in terms of CE pathogenesis.
The pulsation index reflects a decrease in the reserve of endometrial blood flow, which was identified among the causes of reproductive dysfunction in CE in a systematic review in 2020 [37]. The immunological response to infection with excessive local cytokine production in patients with CE is reflected in a large number of the Russian and foreign studies of recent years [21–23, 37]. The significance of endometrial diagnosis using laser conversion testing with the Foton-Bio spectrometer is actively studied now and gives promising results [38–40]. The description of the method and the clinical significance of the obtained parameters using the Foton-Bio spectrometer are presented in the article [40].
Thus, the prognostic model of pregnancy and live birth as a result of IVF after treatment of CE in patients with impaired reproductive function using neural network technology is a unique tool that allows us to predict the success of treatment with a positive result and a prediction accuracy of 97.9%, which exceeds all known models developed for assisted reproductive technologies.
Conclusion
The model of predicting pregnancy as a result of IVF in patients with infertility caused by CE using neural network technology, has a prediction accuracy of 97.9% and makes it possible to determine the need for administering another course (courses) of treatment for CE (in case of a doubtful/negative success rate of pregnancy/live birth), or making a decision on the IVF procedure (in case of a successful result).
Use the calculator at:
https://pentcroft.ru/informaciya/kalkulyatory/ishodyeko.-prognoz/
References
- Kimura F., Takebayashi A., Ishida M., Nakamura A., Kitazawa J., Morimune A. et al. Review: Chronic endometritis and its effect on reproduction. J. Obstet. Gynaecol. Res. 2019; 45(5): 951-60. https://dx.doi.org/10.1111/jog.13937.
- Liu Y., Chen X., Huang J., Wang C.C., Yu M.Y., Laird S., Li T.C. Comparison of the prevalence of chronic endometritis as determined by means of different diagnostic methods in women with and without reproductive failure. Fertil. Steril. 2018; 109(5): 832-9. https://dx.doi.org/10.1016/j.fertnstert.2018.01.022.
- Vaduva C.C., Sandulescu M.S., Tenovici M., Siminel M.A., Novac M.B. Results of in vitro fertilization after diagnosis and treatment of chronic endometritis. Eur. Rev. Med. Pharmacol. Sci. 2023; 27(3): 1069-76. https://dx.doi.org/10.26355/eurrev_202302_31203.
- van Loendersloot L., Repping S., Bossuyt P.M., van der Veen F., van Wely M. Prediction models in in vitro fertilization; where are we? A mini review. J. Adv. Res. 2014; 5(3): 295-301. https://dx.doi.org/10.1016/j.jare.2013.05.002.
- Kasius A., Smit J.G., Torrance H.L., Eijkemans M.J., Mol B.W., Opmeer B.C., Broekmans F.J. Endometrial thickness and pregnancy rates after IVF: a systematic review and meta-analysis. Hum. Reprod. Update. 2014; 20(4): 530-41. https://dx.doi.org/10.1093/humupd/dmu011.
- Moshkalova G., Karibayeva I., Kurmanova A., Mamedalieva N., Aimbetova A., Terlikbayeva A. et al. Endometrial thickness and live birth rates after IVF: a systematic review. Acta Biomed. 2023; 94(3): e2023152. https://dx.doi.org/10.23750/abm.v94i3.14437.
- Broer S.L., van Disseldorp J., Broeze K.A., Dolleman M., Opmeer B.C., Bossuyt P. et al. Added value of ovarian reserve testing on patient characteristics in the prediction of ovarian response and ongoing pregnancy: an individual patient data approach. Hum. Reprod. Update. 2013; 19(1): 26-36. https://dx.doi.org/10.1093/humupd/dms041.
- Lukaszuk K., Kunicki M., Liss J., Lukaszuk M., Jakiel G. Use of ovarian reserve parameters for predicting live births in women undergoing in vitro fertilization. Eur. J. Obstet. Gynecol. Reprod. Biol. 2013; 168(2): 173-7. https://dx.doi.org/10.1016/j.ejogrb.2013.01.013.
- Bjercke S., Fedorcsak P., Åbyholm T., Storeng R., Ertzeid G., Oldereid N. et al. IVF/ICSI outcome and serum LH concentration on day 1 of ovarian stimulation with recombinant FSH under pituitary suppression. Hum. Reprod. 2005; 20(9): 2441-7. https://dx.doi.org/10.1093/humrep/dei101.
- Vaegter K.K., Lakic T.G., Olovsson M., Berglund L., Brodin T., Holte J. Which factors are most predictive for live birth after in vitro fertilization and intracytoplasmic sperm injection (IVF/ICSI) treatments? Analysis of 100 prospectively recorded variables in 8,400 IVF/ICSI single-embryo transfers. Fertil. Steril. 2017; 107(3): 641-8.e2. https://dx.doi.org/10.1016/j.fertnstert.2016.12.005.
- McLernon D.J., Steyerberg E.W., Te Velde E.R., Lee A.J., Bhattacharya S. Predicting the chances of a live birth after one or more complete cycles of in vitro fertilisation: population based study of linked cycle data from 113 873 women. BMJ. 2016; 355: i5735. https://dx.doi.org/10.1136/bmj.i5735.
- Xu T., de Figueiredo Veiga A., Hammer K.C., Paschalidis I.C., Mahalingaiah S. Informative predictors of pregnancy after first IVF cycle using eIVF practice highway electronic health records. Sci. Rep. 2022; 12(1): 839. https://dx.doi.org/10.1038/s41598-022-04814-x.
- Choi B., Bosch E., Lannon B.M., Leveille M.C., Wong W.H., Leader A. et al. Personalized prediction of first-cycle in vitro fertilization success. Fertil. Steril. 2013; 99(7): 1905-11. https://dx.doi.org/10.1016/j.fertnstert.2013.02.016.
- Ratna M.B., Bhattacharya S., Abdulrahim B., McLernon D.J. A systematic review of the quality of clinical prediction models in in vitro fertilisation. Hum. Reprod. 2020; 35(1): 100-16. https://dx.doi.org/10.1093/humrep/dez258.
- Tomita S. Unlocking the potential of bioanalytical data through machine learning. Anal. Sci. 2023; 39(12): 1937-8. https://dx.doi.org/10.1007/s44211-023-00447-w.
- Sfakianoudis K., Maziotis E., Grigoriadis S., Pantou A., Kokkini G., Trypidi A. et al. Reporting on the value of artificial intelligence in predicting the optimal embryo for transfer: a systematic review including data synthesis. Biomedicines. 2022; 10(3): 697. https://dx.doi.org/10.3390/biomedicines10030697.
- VerMilyea M., Hall J.Z.M.M., Diakiw S.M., Johnston A., Nguyen T., Perugini D. et al. Development of an artificial intelligence-based assessment model for prediction of embryo viability using static images captured by optical light microscopy during IVF. Hum. Reprod. 2020; 35(4): 770-84. https://dx.doi.org/10.1093/humrep/deaa013.
- Mihara M., Yasuo T., Kitaya K. Precision medicine for chronic endometritis: computer-aided diagnosis using deep learning model. Diagnostics (Basel). 2023; 13(5): 936. https://dx.doi.org/10.3390/diagnostics13050936.
- Суханов А.А., Дикке Г.Б., Остроменский В.В., Кукарская И.И., Шилова Н.В. Течение и исходы беременности, наступившей в результате экстракорпорального оплодотворения, у пациенток с хроническим эндометритом, получавших комплексное лечение с использованием препарата «Суперлимф» на прегравидарном этапе (рандомизированное контролируемое испытание «ТЮЛЬПАН 2»). Акушерство и гинекология. 2023; 8: 123-34. [Sukhanov A.A., Dikke G.B., Ostromensky V.V., Kukarskaya I.I., Shilova N.V. The course and outcomes of pregnancy resulting from in vitro fertilization in patients with chronic endometritis who received complex treatment using the drug “Superlymph” at the preconception stage (randomized controlled trial “TYULPAN 2”). Obstetrics and Gynecology. 2023; (8): 123-34. (in Russian)]. https://dx.doi.org/10.18565/aig.2023.190.
- Vaduva C.C., Sandulescu M.S., Tenovici M., Siminel MA., Novac M.B. Results of in vitro fertilization after diagnosis and treatment of chronic endometritis. Eur. Rev. Med. Pharmacol. Sci. 2023; 27(3): 1069-76. https://dx.doi.org/10.26355/eurrev_202302_31203.
- Тапильская Н.И., Толибова Г.Х., Савичева А.М., Копылова А.А., Глушаков Р.И., Будиловская О.В. и др. Эффективность локальной цитокинотерапии хронического эндометрита пациенток с бесплодием. Акушерство и гинекология. 2022; 2: 91-100. [Tapilskaya NI., Tolibova G.Kh., Savicheva A.M., Kopylova A.A., Glushakov R.I., Budilovskaya O.V., et al. Efficacy of local cytokine therapy for chronic endometritis in infertile patients. Obstetrics and Gynecology. 2022; (2): 91-100. (in Russian)]. https://dx.doi.org/10.18565/aig.2022.2.91-100.
- Доброхотова Ю.Э., Ганковская Л.В, Боровкова Е.И., Зайдиева З.С., Скальная В.С. Модулирование локальной экспрессии факторов врожденного иммунитета у пациенток с хроническим эндометритом и бесплодием. Акушерство и гинекология. 2019; 5: 125-32. [Dobrokhotova Yu.E., Gankovskaya L.V., Borovkova E.I., Zaidieva Z.S., Skalnaya V.S. Modulation of local expression of innate immunity factors in patients with chronic endometritis and infertility. Obstetrics and Gynecology. 2019; (5): 125-32. (in Russian)]. https://dx.doi.org/10.18565/aig.2019.5.125-132.
- Дикке Г.Б., Суханов А.А., Кукарская И.И., Остроменский В.В. Цитокиновый профиль пациенток с хроническим эндометритом и нарушением репродуктивной функции. Вопросы гинекологии, акушерства и перинатологии. 2021; 20(6): 82-91. [Dikke G.B., Sukhanov A.A., Kukarskaya I.I., Ostromensky V.V. Cytokine profile of patients with chronic endometritis and reproductive dysfunction. Gynecology, Obstetrics and Perinatology. 2021; 20(6): 82-91. (in Russian)]. https://dx.doi.org/10.20953/1726-1678-2021-6-82-91.
- Квашнина Е.В., Гвоздикова Т.В., Дружинина А.Ю., Мастерова И.А., Мурунова С.В., Плотавская Т.Б., Тутаков М.А., Павлюченкова С.М., Шилова Н.В., Дикке Г.Б. Роль мио-инозитола в подготовке женщин к программам вспомогательных репродуктивных технологий. Акушерство и гинекология. 2020; 11: 139-46. [Kvashnina E.V., Gvozdikova T.V., Druzhinina A.Yu., Masterova I.A., Murunova S.V., Plotavskaya T.B., Tutakov M.A., Pavlyuchenkova S.M., Shilova N.V., Dikke G.B. The role of myo-inositol in preparing women for programs assisted reproductive technologies. Obstetrics and Gynecology. 2020; (11): 139-46. (in Russian)]. https://dx.doi.org/10.18565/aig.2020.11.139-146.
- Liu M., Yuan Y., Qiao Y., Tang Y., Sui X., Yin P., Yang D. The effectiveness of immunomodulatory therapies for patients with repeated implantation failure: a systematic review and network meta-analysis. Sci. Rep. 2022; 12(1): 18434. https://dx.doi.org/10.1038/s41598-022-21014-9.
- Зиганшин А.М., Дикке Г.Б., Мудров В.А. Прогнозирование клинически узкого таза с помощью нейросетевого анализа данных. Акушерство, гинекология и pепродукция. 2023; 17(2): 210-9. [Ziganshin A.M., Dikke G.B., Mudrov V.A. Prediction of clinically narrow pelvis using neural network data analysis. Obstetrics, Gynecology and Reproduction. 2023; 17(2): 210-9. (in Russian)]. https://dx.doi.org/10.17749/2313-7347/ob.gyn.rep.2023.382.
- Андрейченко А.Е., Лучинин А.С., Ившин А.А., Ермак А.Д., Новицкий Р.Э., Гусев А.В. Разработка и валидация моделей прогнозирования общего риска преэклампсии и риска ранней преэклампсии с использованием алгоритмов машинного обучения в первом триместре беременности. Акушерство и гинекология. 2023; 10: 94-107. [Andreichenko A.E., Luchinin A.S., Ivshin A.A., Ermak A.D., Novitsky R.E., Gusev A.V. Development and validation of models for predicting the overall risk of preeclampsia and the risk of early preeclampsia using machine learning algorithms in the first trimester of pregnancy. Obstetrics and Gynecology. 2023; 10: 94-107. (in Russian)]. https://dx.doi.org/10.18565/aig.2023.101.
- MacEachern S.J., Forkert N.D. Machine learning for precision medicine. Genome. 2020; 64(4): 416-25. https://dx.doi.org/10.1139/gen-2020-0131.
- Siristatidis C., Pouliakis A., Chrelias C., Kassanos D. Artificial intelligence in IVF: a need. Syst. Biol. Reprod. Med. 2011; 57(4): 179-85. https://dx.doi.org/10.3109/19396368.2011.558607.
- Curchoe C.L., Bormann C.L. Artificial intelligence and machine learning for human reproduction and embryology presented at ASRM and ESHRE 2018. J. Assist. Reprod. Genet. 2019; 36(4): 591-600. https://dx.doi.org/10.1007/s10815-019-01408-x.
- Zaninovic N., Rosenwaks Z. Artificial intelligence in human in vitro fertilization and embryology. Fertil. Steril. 2020; 114(5): 914-20. https://dx.doi.org/10.1016/j.fertnstert.2020.09.157.
- Hansen K.R., He A.L., Styer A.K., Wild R.A., Butts S., Engmann L. et al. Eunice Kennedy Shriver National Institute of Child Health and Human Development Reproductive Medicine Network. Predictors of pregnancy and live-birth in couples with unexplained infertility after ovarian stimulation-intrauterine insemination. Fertil. Steril. 2016; 105(6): 1575-83.e2. https://dx.doi.org/10.1016/j.fertnstert.2016.02.020.
- Kuru Pekcan M., Tokmak A., Ulubasoglu H., Kement M., Özakşit G. The importance of infertility duration and follicle size according to pregnancy success in women undergoing ovulation induction with gonadotropins and intrauterine insemination. J. Obstet. Gynaecol. 2023; 43(1): 2173058. https://dx.doi.org/10.1080/01443615.2023.2173058.
- Zhang L., Cai H., Li W., Tian L., Shi J. Duration of infertility and assisted reproductive outcomes in non-male factor infertility: can use of ICSI turn the tide? BMC Womens Health. 2022; 22(1): 480. https://dx.doi.org/10.1186/s12905-022-02062-9.
- Abdelazim I., Purohit P., Farag R., Zhurabekova G. Unexplained infertility: prevalence, possible causes and treatment options. A review of the literature. J. Obstet. Gynecol. Investigations. 2018; 1(1): 17-22. https://dx.doi.org/10.5114/jogi.2018.74250.
- Liu J., Liu ZA., Liu Y., Cheng L., Yan L. Impact of antibiotic treatment for chronic endometritis on pregnancy outcomes in women with reproductive failures (RIF and RPL): A systematic review and meta-analysis. Front. Med. (Lausanne). 2022; 9: 980511. https://dx.doi.org/10.3389/fmed.2022.980511.
- Buzzaccarini G., Vitagliano A., Andrisani A., Santarsiero C.M., Cicinelli R., Nardelli C. et al. Chronic endometritis and altered embryo implantation: a unified pathophysiological theory from a literature systematic review. J. Assist. Reprod. Genet. 2020; 37(12): 2897-911. https://dx.doi.org/10.1007/s10815-020-01955-8.
- Зуев В.М., Александров М.Т., Хомерики Т.А., Чернышов Г., Метревели Б.Г., Попов С.Н. и др. Клиническое значение лазерного конверсионного тестирования (ЛКТ) в диагностике и лечении хронического эндометрита. Вестник РУДН. Cерия: Медицина. 2012; 6: 95-101. [Zuev V.M., Aleksandrov M.T., Khomeriki T.A., Chernyshov G., Metreveli B.G., Popov S.N. et al. Clinical significance of laser conversion testing (LCT) in diagnosis and treatment of chronic endometritis. Bulletin of RUDN University, Medicine series. 2012; 6: 95-101. (in Russian)]. Available at: https://cyberleninka.ru/article/
- Осипова А.Д., Зуев В.М., Александров М.Т. Значение экспресс-метода лазерной конверсионной диагностики (раман-флуоресцентной составляющей) патологических процессов эндометрия у женщин в перименопаузе. Архив акушерства и гинекологии им. В. Ф. Снегирева. 2019; 2: 85-9. [Osipova A.D., Zuev V.M., Aleksandrov M.T. The significance of the express method of laser conversion diagnostics (Raman fluorescent component) of pathological processes of the endometrium in perimenopausal women. Archive of Obstetrics and Gynecology named after. V.F. Snegirev. 2019; (2): 85-9. (in Russian)]. https://dx.doi.org/10.18821/2313-8726-2019-6-2-85-89.
- Суханов А.А., Дикке Г.Б. Дефект имплантации эмбриона. Положительный прогноз – залог успешного ЭКО. Акушерство и гинекология сегодня. 2023; 4: 10-11. [Sukhanov A.A., Dikke G.B. Embryo implantation defect. A positive prognosis is the key to successful IVF. Obstetrics and Gynecology Today. 2023; (4): 10-11. (in Russian)]. Available at: https://abvpress.ru/
Received 05.03.2024
Accepted 19.03.2024
About the Authors
Anton A. Sukhanov, PhD, Head of the Department of Family Planning and Reproduction, Tyumen Perinatal Center, 1 Daudelnaya str., Tyumen, 625002, Russia;Associate Professor, Department of Obstetrics and Gynecology, Tyumen State Medical University, Ministry of Health of Russia, 10 Permyakov str., Tyumen, 625013, Russia, saa2505anton@yandex.ru, https://orcid.org/0000-0001-9092-9136
Galina B. Dikke, Dr. Med. Sci., Professor, Department of Obstetrics and Gynecology with a Course of Reproductive Medicine, F.I. Inozemtsev Academy of Medical Education, 22 Liter M Moskovskiy Ave., Saint Petersburg, 190013, Russia, galadikke@yandex.ru, https://orcid.org/0000-0001-9524-8962
Viktor A. Mudrov, Dr. Med. Sci., Associate professor, Associate professor, Department of Obstetrics and Gynecology, Faculty of Pediatrics and Faculty of Additional Professional Education, Chita State Medical Academy, Ministry of Health of Russia, 39a Gorkogo str., Chita, 672000, Russia, mudrov_viktor@mail.ru,
https://orcid.org/0000-0002-5961-5400
Irina I. Kukarskaya, Dr. Med. Sci., Professor of the Department of Obstetrics, Gynecology and Reanimatology with a Course of Clinical Laboratory Diagnostics,
Tyumen State Medical University, 10 Permyakov str., Tyumen, 625013, Russia; Chief Physician, Tyumen Region Perinatal Center, 1 Daudelnaya str., Tyumen, 625002, Russia;
Chief Specialist in Obstetrics and Gynecology, Department of Health of the Tyumen Region, https://orcid.org/0000-0002-8275-3553
Corresponding author: Anton A. Sukhanov, such-anton@yandex.ru