Vacuum extraction delivery: 11 years of delivery experience, maternal and fetal outcomes
Shramko S.V., Alekseeva M.V., Renge L.V., Vlasenko A.E.
The frequency of operative vaginal births using vacuum extraction delivery, also known as fetal vacuum extraction delivery (FVE), varies significantly worldwide and comprises 2.8–16.7% of the total number of births, whereas in Russia it is no more than 1.23%. Improved models of the ventouse systems, along with obvious simplicity and convenience, make the FEV method widely and safely used.
Objective: To assess the outcomes of FVE during vaginal delivery (VD) and cesarean section (CS) for mothers and their newborns.
Materials and methods: A retrospective analysis of the outcome of 387 deliveries by FVE using the KIWI vacuum system was performed on the basis of the births and newborns histories at the 2nd Maternity Department of the Novokuznetsk Perinatal Center for the period of 2013–2023. Parity, duration of labor, course of the postpartum period in women and the condition of newborns were studied.
Results: The duration of the FVE was: 5.0 (5.0; 8.0) minutes for VD and 1.0 (1.0; 2.0) minute for CS. In 85% of VD cases and in 96% of CS cases, the postpartum period passed without complications. In 58% of VD cases and in 62% CS cases, the newborns had no complications and there were no cases of severe obstetric trauma. 83% of children were extracted in satisfactory condition, in 2% of CS cases, the death of the newborn occurred. Clinically significant injuries such as subgaleal hematomas and skull fractures were not registered.
Conclusion: When used in a timely manner, taking into account contraindications, observing the conditions and impeccable technique, FVE can be considered a safe procedure both for the mother and the fetus.
Authors’ contributions: Shramko S.V., Renge L.V., Alekseeva M.V. – study concept and design; Alekseeva M.V., Shramko S.V. – data collecting and analysis; Vlasenko A.E. – statistical analysis; Shramko S.V., Alekseeva M.V. – manuscript drafting; Shramko S.V., Renge L.V. – manuscript editing.
Conflicts of interest: The authors declare no conflicts of interest with respect to this publication.
Funding: The study was performed without external funding.
Ethical Approval: The study was approved on February 20, 2025 by the Research Ethics Committee of the Novokuznetsk State Institute for Advanced Medical Studies – Branch of Russian Medical Academy of Continuous Professional Education,
Ministry of Health of Russia.
Patient Consent for Publication: The mothers of newborns provided informed consent for the publication of their data.
Authors' Data Sharing Statement: The data supporting the findings of this study are available on request from the corresponding author after approval from the principal investigator.
For citation: Shramko S.V., Alekseeva M.V., Renge L.V., Vlasenko A.E. Vacuum extraction delivery:
11 years of delivery experience, maternal and fetal outcomes.
Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2025; (8): 80-87 (in Russian)
https://dx.doi.org/10.18565/aig.2025.75
Keywords
In some cases, a prolonged second stage of labor may cause maternal and perinatal morbidity, as well as mortality [1, 2]. Instrumental vaginal birth (use of vacuum extraction and obstetric forceps) can help reduce the duration of the second stage of labor [3]. Caesarean section (CS) in the second stage of labor in case of fetal hypoxia is believed to be a life-saving measure. Currently, the frequency of CS is grows progressively. Worldwide it is not less than 21%, in Russia the CS rate goes up to 30–40%. Moreover, the main indications for its implementation have moved from the absolute category to relative ones [4, 5]. Unfortunately, the high frequency of abdominal delivery has not led to a decrease in maternal morbidity and mortality and has not promoted an improvement in perinatal outcomes. On the contrary, such a situation has a negative impact on the reproductive potential of the population. It is accompanied by an increase in the number of maternal complications and an increased risk in pregnancies associated with placenta scar ingrowth and incompetent uterine scars [4]. In addition, CS increases the risk of intraoperative complications: massive blood loss, purulent-inflammatory postpartum diseases. It can also become the cause of maternal and perinatal morbidity and mortality [4–6]. Given the decrease in a population health index, along with the increase rate for antibiotic resistance, CS without strict indications causes concern and prompts the search for other methods of delivery. It also requires discussion of the eligibility of its use in case of a prolonged second stage of labor and fetal distress [7–9].
The first vacuum device to facilitate vaginal delivery was presented to the medical community in the 19th century by doctor James Simpson from Edinburgh (UK). But only in the 1950s vacuum delivery began to be actively introduced into practice as an alternative method to obstetric forceps. Initially, a stainless steel metal cup was used, later it was replaced by a pyocrylic one, and currently polyethylene or silicone cups are used [10]. Instrumental vaginal delivery is recommended in cases of a prolonged second stage of labor. According to many authors, the most objective approach to assessing the condition of the fetus during labor, taking into account the indications and the condition, makes fetal vacuum extraction a low-trauma intervention that has certain advantages in comparison with CS [9–12]. Conducting vacuum delivery allows to reduce the number of emergency CS during the expulsion period without worsening the birth outcomes for the mother and the newborn, and also makes it possible to avoid the risks of anesthetic complications, bleeding and infection [13]. In addition, the procedure is less expensive, does not lead to the formation of an uterine scar and abnormal placentation in further pregnancies, and also has a significantly shorter recovery period compared to CS [14, 15]. In economically developed countries, the incidence of vacuum deliveries is 2.8–16.7% of the total number of births [16]. In comparison, in the UK, the rate of vaginal operative births is 10–13% of all births, in Sweden it is 6%, and more often in primiparous women (14%) than in multiparous (2.8%). In Singapore, vaginal delivery rate is 4.5%, in Israel it is 5.9%, in the USA – 2.6% [17].
All of the above, as well as the desire of the authors to share their 11 years’ experience of using vacuum extraction as a safe method of delivery in the second stage of labor, served as the basis for this article.
Aim of study: to assess the outcomes of vacuum delivery in vaginal birth and in CS both for the newborn and the mother.
Materials and methods
The study included 387 women in labor who underwent fetal vacuum extraction using the KIWI single-use vacuum system: in 284 cases the birth was vaginal (VB), in 103 cases a CS was performed.
Study design: we retrospectively analyzed 387 birth histories (medical record form No. 096/u) and newborn cards for the period 2013–2023 as well as reporting documents of the 2nd maternity department of the Novokuznetsk Perinatal Center. Inclusion criteria: vacuum delivery with the KIWI single-use vacuum system for weak pushing, fetal distress during the pushing stage, planned shortening and relief of the pushing stage in women with extragenital pathology or preeclampsia. Exclusion criteria: presence of an uterine scar after myomectomy or CS; fetal head above the narrow part of the small pelvis; extended fetal head. The following aspects were studied: parity, duration of labor, course of the postpartum period in women and condition of newborns. The obtained information was converted into a database format.
The main evaluation criterion was the neonatal morbidity rate (neonatal complications). Additionally, we analyzed the nosological structure of complications, anthropometric parameters of newborns, Apgar scores, frequency of artificial lung ventilation, neonatal mortality, and maternal complications.
Statistical analysis
The normality of distribution of quantitative variables was assessed using the Shapiro–Wilk test. For data with normal distribution, descriptive statistics are presented as mean values (M) and standard deviations (SD), otherwise the median (Me) and interquartile range (Q1; Q3) are given. Comparison of two groups by quantitative characteristics was carried out using Student's t-test (Welch's test for the absence of variances equality) in the case of normal distribution of indicators and the Mann–Whitney test otherwise.
The c2 criterion was used to compare categorical variables. In case of units with expected values less than 5%, the Fisher’s exact test was applied. To identify categories that made a non-random contribution to the criterion statistics (post-hoc comparisons), an analysis of Haberman standardized residuals with Benjamini – Hochberg method for multiple comparisons was performed.
For the primary endpoint of the study, the risk difference (RD) with 95% confidence interval (CI) was calculated, reflecting the magnitude of the effect of the studied interventions. Differences were considered statistically significant at p≤0.05. Calculations and charts were performed using the R-statistical environment (v.3.6, GNU GPL2 license).
Results
Our analysis was conducted in a level II maternity unit where the rate of abdominal delivery over an 11-year period (2013–2023) comprised 24–29% (Figure).
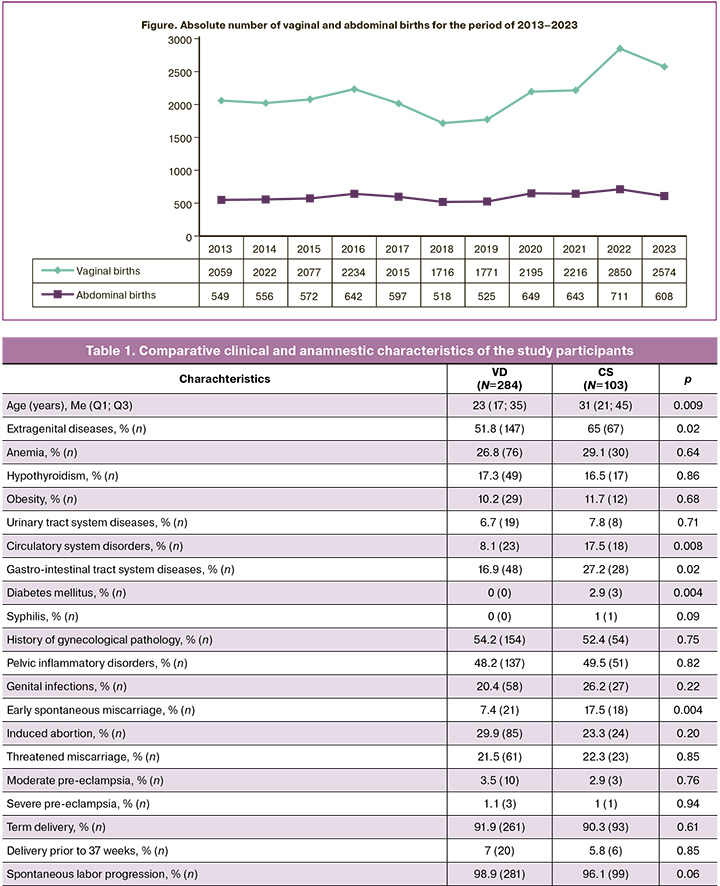
Over the analyzed period, 24 377 births were registered: 387 vacuum-assisted deliveries (1.6%); 6724 births (27.58%) ended with CS, including vacuum extraction in 103 cases (1.5%); with VD (17 653 which is 72.42%) of which vacuum extraction was conducted in 284 cases (1.6%).
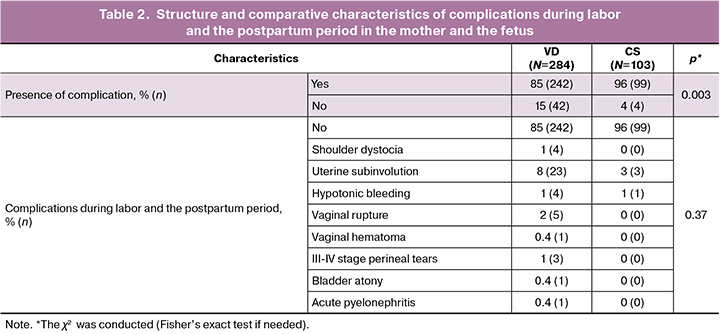
The age of women in the study groups differed significantly (p=0.009): the average age of women with VD was 23 (3.02) years (17; 35), in the group with CS it was 31 (4.97) years (21; 45) (Table 1). Moreover, women with CS significantly more tended to have extragenital diseases (p=0.02) than women with VD. Anemia was the most common indication, without significant differences among the groups; hypothyroidism, obesity and diseases of the urinary system were also observed with the same frequency. In turn, women in the CS group significantly more often had circulatory system disorders (p=0.008), gastrointestinal tract diseases (p=0.02) and diabetes mellitus (p=0.02). It should be emphasized that in most cases a combination of several diseases was observed, which significantly complicated the course of pregnancy and childbirth.
The frequency rate of gynecological pathology in comparison groups did not differ significantly; however, every second examined woman had inflammatory diseases of the pelvic organs, every fifth woman in the group with VD and every fourth woman with CS had previously had genital infections (chlamydia, trichomoniasis). One patient in the CS group had a history of syphilis. Spontaneous miscarriages in early pregnancy were observed more often in the CS group (p=0.004); however, the frequency of induced abortions in the groups pf patients did not differ significantly (p=0.20). Threatened miscarriage and pre-eclampsia complicated the course of pregnancy in the patient groups with the same frequency.
In most women, labor developed spontaneously at 38–40 weeks. The gestation period up to 37 weeks, as well as the tendency for post-term pregnancy, found no significant differences. Labor induction by amniotomy was performed in 3/284 (1%) women in the VD group and in 4/103 (3.8%) women with CS.
In the VD group, fetal vacuum extraction was performed significantly more often (p<0.001) for primigravidi (178/284, 63%) and primiparous women (243/284, 86%); while in the CS group, women with third and more pregnancies (47/103, 46%), second (43/103, 42%), third and more births (19/103, 18%) predominated.
In vaginal delivery group, the main indications for performing vacuum extraction were: weak pushing (74%), fetal distress during the pushing stage of labor (24%), in 6 cases (2%) – planned shortening and relief of the pushing stage related to extragenital pathology or preeclampsia. The total duration of labor was 10.1 (2.9) hours. The 1st stage lasted 9 (7; 11) hours, the 2nd – 1 (0.75; 1.25) hour, pushing – 0.5 (0.42; 0.67) hours, the 3rd – 0.08 (0.08; 0.17) hours, time without amniotic fluid – 7.5 (4.8; 11.0) hours. At the beginning of vacuum extraction procedure, the fetal head was engaged in the pelvic floor in 85% (241/284) and in the narrow part of the small pelvis in 15% (43/284). In 1% (3/284) of cases, vacuum extraction was unsuccessful, and labor ended with CS.
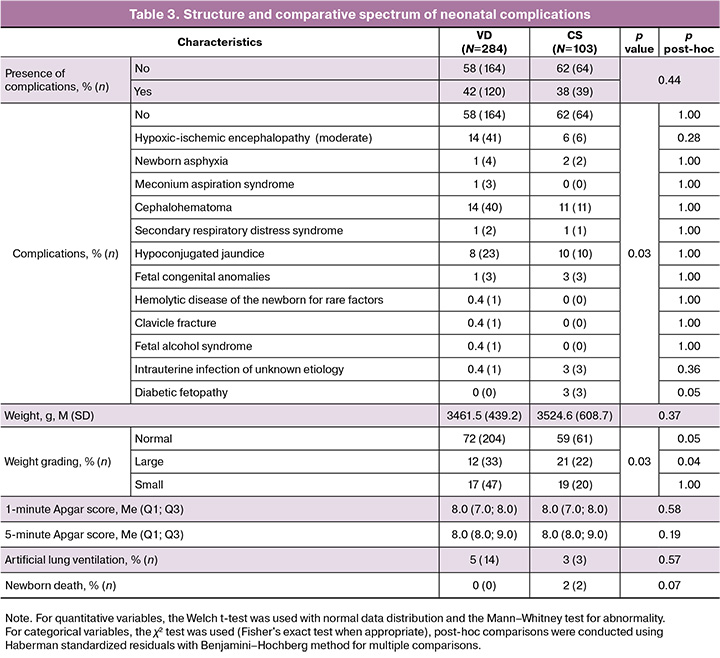
In CS, vacuum extraction procedure was most often elective (80/103, 77.7%). In 23/103 (22.3%) cases it was performed urgently for careful extraction of the fetus with a high position of the head. Moreover, in every fourth case (25/103, 24%) there was a large fetus and in every 10th case the woman was obese. In 242/284 (85%) women with VD and in 99/103 (96%) wpmen with CS, delivery proceeded without complications. The structure and comparative characteristics of complications during labor and the postpartum period in the mother and the fetus are presented in Table 2.
In VD, 15% (42/284) of women had complications during labor: subinvolution of the uterus was recorded in 8% (23/284); hypotonic bleeding — in 1% (4/284) of cases. The volume of blood loss was no more than 600–850 ml (in 3 primiparous women with a large fetus and in a multiparous woman). We observed a single case of bladder atony, not associated with the implementation of vacuum procedure, but caused by the uterine contractility abnormality, prolonged labor and a long position of the fetal head in one plane of the small pelvis. In 9/284 (3.4%) cases, we obsrved complications associated with maternal trauma: perineal and vaginal ruptures, as well as vaginal hematoma. In 3/284 (1%) cases, the median-lateral episiotomy was extended into a third-degree perineal rupture; all women were primiparous and aged under 30, with the fetus weighed no more than 3440 g. All patients were discharged home with perineal healing by primary intention. Fetal shoulder dystocia was observed in 4/284 (1%) cases, and only in primiparous women. In this case, the indication for vacuum extraction procedure was weak labor activity, and in 1 case there was a large fetus. All newborns were discharged home in satisfactory condition.
During CS, complications were observed significantly less frequently (in 4%) (4/103) (p=0.003): in 3 cases it was subinvolution of the uterus and in 1 – hypotonic bleeding.
Complications in newborns were observed with the same frequency both in VD (42%) and in CS (38%) (RD=4.4% [95% CI -6.8; 15.0], p=0.44). Moreover, in CS, diabetic fetopathy (3%) (RD=-3.0% [95% CI -8.2; -0.99, p=0.05) and large fetal weight (RD=-9.7% [95% CI -19.2; -1.7], p=0.04) were significantly more common. We observed hypoxic-ischemic encephalopathy in 14% of VD patients and in 6% of CS patients, and only in the early stages of vacuum extraction procedure (2013–2014) (Table 3). 7 (3%) infants were born with a low Apgar score of 2–4 points, with severe asphyxia recorded in 4 cases and meconium aspiration syndrome in 3 cases; 14 (5%) of them required artificial ventilation. By the second day of life, the condition of 96% of newborns improved.
In VD, the duration of the vacuum extraction procedure took 5.0 (5.0; 8.0) minutes, in CS it lasted for 1.0 (1.0; 2.0) minute.
In our study, there were 2 cases (2%) of early neonatal death during CS not associated with the vacuum extraction procedure: in one case, the cause was a congenital malformation of the fetus incompatible with life, in the other – severe fetal asphyxia during labor.
There were no cases of perinatal mortality after VD. The rooming-in rate on the 1st day after VD was 81% (229/284), while after CS – 54% (56/103) (p<0.001). Every third woman (88/284, 31%) was discharged on the 4th day after VD, against 10% (10/103, p<0.001) after CS, among which the majority (46/103, 45%) were discharged on the 5th day and every fourth patient (24/103, 23%) – on the 6th day (p=0.03). In most cases, newborns were discharged home after VD (96%) and CS (97%). After VD, 8 (3%) newborns were transferred to the intensive care unit (ICU), and 3 (1%) children with concomitant pathology were transferred to the neonatal pathology unit (NPD). After CS, 1 (1%) newborn was transferred to the ICU, and 2 (2%) newborns were transferred to the NPD. 14 newborns required transfer to a children's specialized hospital.
Discussion
The connection between vacuum-assisted delivery and birth trauma is a subject of discussion [17, 18]. It is known that fetal trauma in vacuum delivery can be a consequence of hypoxia and ischemia in the antenatal period, or it can be mechanical (extracranial, cranial, intracranial). Cup marks, bruises or the so-called "chignon" associated with the use of a Kiwi-system occur in 100% of cases. These are considered a normal variant and regarded as cosmetic damage. Clinically insignificant damage includes: retinal hemorrhages (1–29%), superficial abrasions (2–10%), subcutaneous hematomas and cephalohematomas (6–11%) [19]. Clinically significant damage to the tissues of the fetal head are: skin wounds of the head, subgaleal hematomas (0.5–1%), subarachnoid hemorrhages (0.8%), and skull fractures [20]. In our study, we did not encounter these damages; in turn, cephalohematomas were observed in 14% and 11% of cases in VD and CS, respectively. Cephalohematomas did not require intervention and resolved spontaneously within 2–3 months, which is consistent with scientific data [19, 21]. The causes of birth injuries are strong traction against incorrect direction, as well as incorrect positioning of the cup on the fetal head during surgery [22]. In addition, some authors consider slippage of the Kiwi cup (9.6%) to be one of the reasons for unsuccessful vacuum extraction and for fetal trauma [23]. Correct application of the Kiwi cup, namely in the “0-station” of the largest fetal head circumference with the location of the wire point at the “+2” level, allowed us to reduce cup slippage to single cases [20, 22]. It should be emphasized that the duration of the vacuum extraction procedure was: 5.0 (5.0; 8.0) minutes for VD and 1.0 (1.0; 2.0) minute for CS.
It turned out that vacuum extraction in VD was more often used in primigravidi (63%) and primiparous (86%) women, compared to multigravidi (37%) and multiparous (15%) women, respectively. In turn, an inverse correlation was observed for CS: vacuum delivery was more often performed in multigravidi (75%) and multiparous (60%) women, than in primigravidi (25%) and primiparous (40%) women, which is consistent with the literature data [24].
In this study the frequency of shoulder dystocia was 3 times lower than the average reported in the literature (2.7–4.1%) [25, 26] – only in 4 cases (1%) and only in VD. In three of them, the complication was not associated with the birth of children over 4000 g.
The incidence of postpartum hemorrhage after vacuum-assisted delivery did not exceed 1% and was comparable with scientific data (1.6%). The same was observed in VD cases without vacuum procedure (1.2%) [27].
The worldwide frequency of vaginal operative deliveries varies from 2.1 to 19.2%; with vacuum extraction procedure accounting for an average of 4.5%, and in Russia – no more than 1.23%. Portugal (16.7%) and Australia (8.1%) are the leaders in the rate of operative vaginal delivery using vacuum extraction. [28]. According to the annual reports of the obstetric department No. 2 (Perinatal Center of the State Autonomous Healthcare Institution “Novokuznetsk City Clinical Hospital No. 1 named after G.P. Kurbatov”) over an eleven-year period (2013–2023), there has been a tendency towards an increase in the frequency of vacuum-assisted delivery. In 2013, the frequency of fetal vacuum extraction was 0.9% (n=29) of the total number of births, in 2018 – 1.6% (n=28), in 2023 – 1.9% (n=49). At the same time, the frequency of abdominal delivery in 2018 comprised 30.2% (n=518) of the total number of births, in 2023 – 24.3% (n=608) and it does not differ from the global indicators (21%), but is lower than the average in Russia (30–40%) [4, 5].
Traditionally, doctors are more proficient in the C-section technique than in vacuum-assisted method. However, the increase in the number of vaginal deliveries and decrease in abdominal operative deliveries is most likely due to obstetricians changing their opinion in favor of vacuum extraction, as well as the acquisition of positive experience and improvement of manual skills. Moreover, the frequency of vacuum deliveries (1.5–1.6%) in a level 2 obstetric institution does not differ from the average in Russia (1.23%), but is 2.8 times lower than global indicators. (4,5%) [28].
In 85–96% of cases, the postpartum period was uneventful. In most cases (83%), children were delivered in satisfactory condition, without complications (58–62%) and clinically significant injuries, and there were no cases of severe obstetric trauma.
Conclusion
When used in a timely manner, taking into account contraindications, observing the conditions and impeccable technique, vacuum extraction procedure is a safe operation for the mother and fetus, both during vaginal and abdominal births. In order to reduce the risk of neonatal birth trauma, it is necessary to be aware of the biomechanics of childbirth, to timely assess the obstetric situation and technical performance of the operation as well as to continuously improve professional skills and competencies.
References
- Pattinson R.C., Vannevel V., Barnard D., Baloyi S., Gebhardt G. S., Roux K.L. et al. Failure to perform assisted deliveries is resulting in an in-creased neonatal and maternal morbidity and mortality: an expert opinion. S. Afr. Med. J. 2018; 108: 75-8. https://dx.doi.org/10.7196/SAMJ.2017.v108i2.12786
- Kayiga H., Ajeani J., Kiondo P., Kaye D. Improving the quality of ob-stetric care for women with obstructed labour in the national referral hospital in Uganda: lessons learnt from criteria based audit. BMC Pregnancy Child-birth. 2016; 16(1): 152. https://dx.doi.org/10.1186/s12884-016-0949-1
- Bailit J.L., Grobman W.A., Rice M.M. Wapner R.J., Reddy U.M., Varner M.W. et аl. Evaluation of delivery options for second‐stage events. Am. J. Obstet. Gynecol. 2016; 214(638): e1-10. https://dx.doi.org/10.1016/j.ajog.2015.11.007
- Краснопольский В.И., Мельников А.П., Петрухин В.А., Карамян Р.А. Экстраперитонеальное кесарево сечение: место операции в мире и отечественном акушерстве. Акушерство и гинекология. 2020; (9): 11-7. [Krasnopolsky V.I., Melnikov A.P., Petrukhin V.A., Karamyan R.A., Extraperitoneal cesarean section: the place of the operation in the world and in Russian obstetrics. Obstetrics and Gynecology. 2020; (9): 11-7 (in Russian)]. https://dx.doi.org/10.18565/aig.2020.9.11-17
- Сайдалиева Д.А., Додхоева М.Ф., Абдуллаева Р.А. Эпидемиология и факторы риска развития материнского сепсиса. Вестник Авиценны. 2023; 25(2): 248-59. [Sajdalieva D.A., Dodhoeva M.F., Abdullaeva R.A. Epidemiology and risk factors for the development of maternal sepsis. Avicenna Bulletin. 2023; 25(2): 248-59 (in Russian)]. https://dx.doi.org/10.25005/2074-0581-2023-25-2-248-259
- Ивачев А.С., Митрошин А.Н., Боярченко Е.М., Ивачева Н.А. Гнойно-воспалительные осложнения и послеоперационные грыжи после кесарева сечения. Ульяновский медико-биологический журнал. 2024; (2): 90-107. [Ivachev A.S., Mitroshin A.N., Boyarchenko E.M., Ivacheva N.A. Pu-rulent-inflammatory complications and postoperative hernias after cesarean section. Ulyanovsk Medical and Biological Journal. 2024; (2): 90-107 (in Russian)]. https://dx.doi.org/10.34014/2227-1848-2024-2-90-107
- Кузьменков А.Ю., Виноградова А.Г., Трушин И.В., Эйдельштейн М.В., Авраменко А.А., Козлов Р.С. AMRmap – система мониторинга антибиотикорезистентности в России. Клиническая микробиология и антимикробная химиотерапия. 2021; 23(2): 198-204. [Kuz'menkov A.Yu., Vinogradova A.G., Trushin I.V., Ejdel'shtejn M.V., Avramenko A.A., Kozlov R.S. AMRmap – antibiotic resistance monitoring system in Russia. Clinical Microbiology and Antimicrobial Chemotherapy. 2021; 23(2): 198-204 (in Russian)]. https://dx.doi.org/10.36488/cmac.2021.2.198-204
- Федорова М.Н. Тенденции развития человеческого потенциала России: индикаторы состояния здоровья, образования и культуры населения в 2000–2020 гг. Развитие и безопасность. 2022; 3(15): 72-84. [Fedorova M.N. Tendencies of the development of the human potential in Russia: indicators of health status, education and culture of the population in 2000–2020 уеаrs. Development and security. 2022; 3(15): 72-84 (in Russian)]. https://dx.doi.org/10.46960/2713-2633_2022_3_72
- Sandall J., Tribe R.M., Avery L. Mola G., Visser G.H., Homer C.S. et. аl. Short term and long term effects of caesarean section on the health of women and children. Lancet. 2018; 392: 1349-57. https://dx.doi.org/10.1016/S0140-6736(18)31930-5
- Muraca G.M., Skoll A., Lisonkova S., Sabr Y., Brant R., Cundiff G.W. et al. Perinatal and maternal morbidity and mortality among term singletons following midcavity operative vaginal delivery versus caesarean delivery. BJOG. 2018; 125(6): 693-702. https://dx.doi.org/10.1111/1471-0528.14820
- Mola G.D.L., Unger H.W. Strategies to reduce and maintain low perina-tal mortality in resource poor settings – Findings from a four decade observa-tional study of birth records from a large public maternity hospital in Papua New Guinea. Aust. N. Z. J. Obstet. Gynaecol. 2019; 59(3): 394-402. https://dx.doi.org/10.1111/ajo.12876
- Muraca G.M., Boutin A., Razaz N., Lisonkova S., John S., Ting J.Y. et аl. Maternal and neonatal trauma following operative vaginal delivery. CMAJ. 2022; 194(1): E1-E12. https://dx.doi.org/10.1503/cmaj.210841
- Nolens B., Namiiro F., Lule J., Akker T. van den, Roosmalen J. van, Byamugisha J. Prospective cohort study comparing outcomes between vacu-um extraction and second stage cesarean delivery at a Ugandan tertiary referral hospital. Int. J. Gynaecol. Obstet. 2018; 142(1): 28-36. https://dx.doi.org/10.1002/ijgo.12500
- Nolens B., van den Akker T., Lule J., Twinomuhangi S., van Roosmalen J., Byamugisha J. Birthing experience and quality of life after vacuum delivery and second stage caesarean section: a prospective cohort study in Uganda. Trop. Med. Int. Health. 2018; 23(8): 914-22. https://dx.doi.org/10.1111/tmi.13089
- Ulfsdottir H., Ekéus C., Tedroff K., Åberg K., Pettersson H.J. Long term neurological morbidity among children delivered by vacuum xtraction a national cohort study. Acta Obstet. Gynecol. Scand. 2023; 102(7): 843-53. https://dx.doi.org/10.1111/aogs.14568
- Ekéus C., Wrangsell K., Penttinen S., Åberg K. Neonatal complications among 596 infants delivered by vacuum extraction (in relation to characteristics of the extraction). J. Matern. Fetal Neonatal Med. 2018; 31(18): 2402-8. https://dx.doi.org/10.1080/14767058.2017.1344631
- Åberg K., Norman M., Pettersson K. Järnbert-Pettersson H., Ekéus C. Protracted vacuum extraction and neonatal intracranial hemorrhage among in-fants born at term: a nationwide case-control study. Acta Obstet. Gynecol. Scand. 2019; 98(4): 523-32. https://dx.doi.org/10.1111/aogs.13519
- Thierens S., Binsbergen V. A., Nolens B. Akker T., Bloemenkamp K., Rijken M.J. Vacuum extraction or caesarean section in the second stage of labour: a systematic review. BJOG. 2023; 130(6): 586-98. https://dx.doi.org/110.1111/1471-0528.17394
- O’Mahony F., Hofmeyr G.J., Menon V. Choice of instruments for as-sisted vaginal delivery. Cochrane Database Syst. Rev. 2010; 10(11): CD005455. https://dx.doi.org/10.1002/14651858
- Kong C.W., To W.W.K. Precision of vacuum cup placement and its association with subgaleal hemorrhage and associated morbidity in term neonates. Arch. Gynecol. Obstet. 2024; 309(4): 1411-9. ery. Cochrane Database Syst. Rev. 2010; 10(11): CD005455. 10.1007/s00404-023-07018-4
- Баев О.Р., Гайдарова А.Р., Караваева А.Л. Родовой травматизм новорожденных. Неонатология: новости, мнения, обучение. 2023; 11(2): 67-73. [Baev O.R., Gaydarova A.R., Karavaeva A.L. Birth trauma in newborns. Neonatology: News, Opinions, Training. 2023; 11(2): 67-73 (in Russian)]. https://dx.doi.org/10.33029/2308- 2402-2023-11-2-67-73
- Министерство здравоохранения Российской Федерации. Клинические рекомендации. Оперативные влагалищные роды (роды одноплодные, родоразрешение с наложением щипцов или с применением вакуум-экстрактора). М.; 2023. 28 с. [Ministry of Health of the Russian Federation. Clinical guidelines. Operative vaginal child-birth (unilateral childbirth, delivery with forceps or vacuum extraction). Moscow; 2023. 28 p. (in Russian)].
- Медведева И.Н., Святченко К.С., Барбашова Ю.Ю. Вакуум-экстракция плода: версии и контраверсии. Журнал акушерства и женских болезней. 2017; 66(1): 21-6. [Medvedeva I.N., Svyatchenko K.S., Barbashova Y.Y. Vacuum extraction of the fetus: versions and controversies. Journal of Obstetrics and Women’s Diseases. 2017; 66(1): 21-6 (in Russian)]. https://dx.doi.org/10.17816/JOWD66121-26
- Киселева Л.Г., Сачкова Ю.И. Перинатальный анамнез детей при родоразрешении путем вакуум-экстракции. Вятский медицинский вестник. 2024; 2(82): 20-5. [Kiseleva L.G., Sachkova Yu.I. Perinatal history of children delivered by vacuum extraction. Vyatka Medical Bulletin. 2024; 2(82): 20-5 (in Russian)]. https://dx.doi.org/10.24412/2220-7880-2024-2-20-25
- Levin G., Tsur A., Rottenstreich A., Cahan T., Shai D., Meyer R. The association of vacuum-assisted delivery and shoulder dystocia among macrosomic newborns: a retrospective study. Arch. Gynecol. Obstet. 2021; 304(1): 117-23. https://dx.doi.org/10.1007/s00404-020-05941-4
- Practice Bulletin No 178: Shoulder dystocia. Obstet. Gynecol. 2017; 129(5): e123-33. https://dx.doi.org/10.1097/AOG.0000000000002043
- Gardella C., Taylor M., Benedetti T., Hitti J., Critchlow C. The effect of sequential use of vacuum and forceps for assisted vaginal delivery on neonatal and maternal outcomes. Am. J. Obstet. Gynecol. 2001; 185(4): 896-902. https://dx.doi.org/10.1067/mob.2001.117309
- Tsakiridis I., Giouleka S., Mamopoulos A., Athanasiadis A., Daniilidis A., Dagklis T. Operative vaginal delivery: a review of four national guidelines. J. Perinat. Med. 2020; 48(3): 189-98. https://dx.doi.org/10.1515/jpm-2019-0433
Received 13.03.2025
Accepted 30.06.2025
About the Authors
Svetlana V. Shramko, Dr. Med. Sci., Associate Professor, Department of Obstetrics and Gynecology, Novokuznetsk State Institute for Advanced Medical Studies – branch of Russian Medical Academy of Continuous Professional Education, Ministry of Health of Russia, 654005, Russia, Novokuznetsk, Stroiteley Ave., 5, +7(3843)324-750, shramko_08@mail.ru, https://orcid.org/0000-0003-1299-165XMarina V. Alekseeva, Head of Obstetric Hospital No. 2, Novokuznetsk City Clinical Hospital No. 1 named after. G.P. Kurbatov, Perinatal Center,
Obstetric Department No. 2, 654031, Russia, Novokuznetsk, Izhevskiy proezd, 16, +7(913)316-99-16, arina13_68@mail.ru, https://orcid.org/0000-0001-7553-0856
Ludmila V. Renge, Dr. Med. Sci., Head of the Department of Obstetrics and Gynecology, Novokuznetsk State Institute for Advanced Medical Studies – branch of Russian Medical Academy of Continuous Professional Education, Ministry of Health of Russia, 654005, Russia, Novokuznetsk, Stroiteley Ave., 5, +7(3843)324-750, l.renge@mail.ru, https://orcid.org/0000-0002-7237-9721
Anna E. Vlasenko, Leading Expert, Digital Technologies and Platforms LLC, 115054, Russia, Moscow, Dubininskaya str., 57, build. 1а, vlasenkoanna@inbox.ru,
https://orcid.org/0000-0001-6454-4216