Ultrasound diagnosis in pregnancy in the evolving coronavirus (COVID-19) pandemic
The paper reviews current international and Russian recommendations for organizing and conducting ultrasound examinations in obstetric practice during the pandemic of the novel coronavirus infection COVID-19. It discusses questions on disease control measures and choices of type of personal protective equipment for healthcare workers. The algorithms for scheduling screening and fetal monitoring examinations, invasive procedures in cases of fetal malformations and pregnancy complications in patients with suspected or confirmed COVID-19 and in cases with limited human resources in diagnostic departments have been provided. Using the given information in daily practice will ensure the epidemiological safety and clinical effectiveness of the diagnostic departments in our country during COIVID-19 pandemic.Gus A.I., Papageorghiou A., Yarygina T.A., Shuvalova M.P.
Keywords
The protection of motherhood and childhood is one of the priority tasks of our country, enshrined in the Constitution of the Russian Federation (Article 38) [1]
The pandemic of a novel coronavirus SARS-CoV-2 can cause the clinical condition COVID-19 (hereinafter — COVID-19), and this can have serious consequences for pregnant and non-pregnant women. The outbreak of COVID-19 is likely to cause an increase in maternal and perinatal mortality directly (due to the symptoms of the condition such as respiratory disease); but also due to indirect effects, such as delay in seeking medical care or limits on the availability of providing, and timeliness of receiving, medical care due to quarantine measures.
Ultrasound examination in pregnancy care is an important diagnostic tool that allows identification of a wide range of pathologies in early pregnancy – such as pregnancy loss and ectopic pregnancy [2]; of the developing fetus [3, 4]; and that can predict - and through appropriate interventions can lead to prevention of - a number of the great obstetrical syndromes, such as fetal growth restriction [5], preeclampsia [6, 7], premature birth [8, 9], and stillbirth [10]. In this connection, in the context of the evolving coronavirus (COVID-19) pandemic [11], pregnant patients should be provided with safe and effective medical care, including prenatal ultrasound diagnostics.
The consensus of experts from The International Federation of Gynecology and Obstetrics (FIGO) [12] recommends standardization of screening, admission, and management of pregnant women in the COVID19 pandemic in accordance with local, federal, and international guidelines in all medical centers.
It is important to note that the International Society of Ultrasound Diagnostics in Obstetrics and Gynecology (ISUOG) in its consensus statement [13] classifies ultrasound examinations as a situation with a higher risk of viral transmission, due to the inability to maintain a safe (2 meter) distance between a patient and a sonographer. Therefore, it becomes important to develop new principles and approaches in organization of the work of diagnostic departments, with an important new aspect: to prevent the spread of infection [14].
Patient factors, risk of COVID-19 and indication or the scan
First of all, everything possible should be done to reduce visits to clinics to strictly indicated examinations in order to reduce the risk of viral transmission and protect both patients and staff [13—15]. It is important for heads of diagnostic departments to be prepared for reorganization of work in the event of staff shortage associated with self-isolation, illness, or transfer to other departments and clinics [13].
The 3 basic groups of factors that currently determine work of the diagnostic department during the COVID19 pandemic [13—15]:
- Health status of patients, which will depend on the likelihood of infection with COVID-19;
- Scan indications and priority;
- The internal situation in the diagnostic departments, depending on the number of staff present at the workplace.
For scheduling ultrasound examinations, the ISUOG consensus [13] recommends compulsory separation of all patients into 3 groups depending on the likelihood of infection with COVID-19:
- asymptomatic patients without potential contact with COVID-19;
- asymptomatic patients with epidemiological risk factors in contact with COVID-19;
- Patients with probable / confirmed COVID-19.
The first step is to separate unambiguously or probably infected patients (with clinical symptoms) from those who are presumably not infected (without clinical symptoms), while taking into account the large number of asymptomatic cases of COVID-19 [16].
The clinical manifestations of an acute respiratory infection suspicious of COVID-19 include: body temperature above 37.5°C and one or more of the following symptoms: cough (dry or with sputum), dyspnea, chest tightness, sore throat, runny nose, and other catarrhal symptoms, weakness, headache, anosmia, diarrhea [11].
To assess the risk of infection in each patient, it is important to consider not only the clinical manifestations, but also the epidemiological risk factors in contact with COVID-19, which include [11]:
- Return from a foreign trip, particularly a high incidence area, in the last 14 days;
- Close contact, over the past 14 days, with a person suspected of having COVID-19;
- Close contact, over the past 14 days, with a person who has a laboratory diagnosis of COVID-19;
- Work with patients with confirmed / suspicion of COVID-19.
Following the recommendations of the ISUOG consensus [13], it is good practice to undertake “sorting” of patients according to the probability of infection with COVID-19 (face-to-face or by correspondence):
Questioning patients for the presence of clinical symptoms and epidemiological risk factors when registering for an ultrasound examination and with telephone confirmation a day before the appointment [13].
Patients with clinical symptoms should not undergo elective ultrasound examinations. The clinic staff should clarify that if symptoms persist, the patient should report this to the clinic by phone without making a personal visit [15].
Questioning patients for their clinical symptoms and epidemiological risk factors and temperature measurement before they enter a clinic [13, 15, 17].
If clinical symptoms and / or epidemiological risk factors are detected in the patient or her companion, their passage to clinic is prohibited. Scans that can be safely postponed should be rescheduled in 2 weeks, assuming resolution of symptoms. Clinically urgent / indicated scans must be carried out in an isolated room, with personnel using appropriate personal protective equipment; the patients must also be provided with a surgical mask [14, 17].
For effective planning of ultrasound diagnostic departments work, it is necessary to divide scans based on their urgency [13, 18]:
- Scans that need to be undertaken without delay;
- Scans that can be delayed for a few weeks without affecting clinical care;
- Scans that can be canceled for the duration of the pandemic.
Every effort should be made to monitor pregnant women in accordance with national recommendations [19, 20], strictly observing additional measures related to the COVID-19 pandemic.
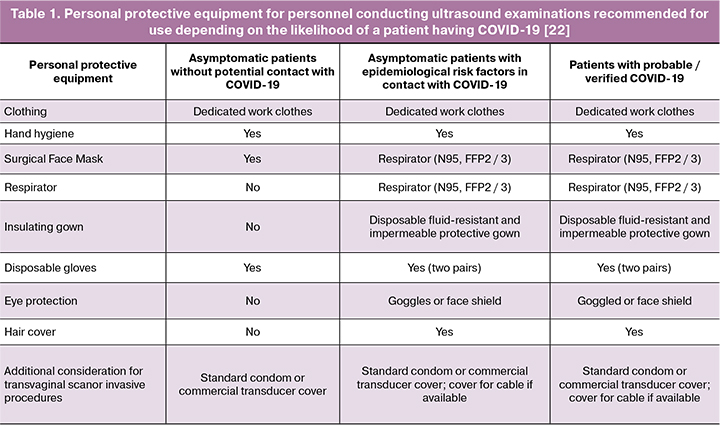
Personal Protective Equipment and ultrasound scans during the COVID-19 pandemic
During the pandemic, it is important to strictly follow the rules described by the ISUOG Safety Committee: “Safe performance of obstetric and gynecological scans and equipment cleaning in the context of COVID-19”, translated into Russian [21], and “Use of personal protective equipment and hazard mitigation in relation to SARS-CoV-2 for practitioners undertaking obstetric and gynecological ultrasound” [22]. The Table 1 presents the basic principles for choosing of personal protective equipment recommended for use by ultrasound providers based on risk assessment of patient for COVID-19.
Considerations for clinical areas during the COVID-19 pandemic
In addition to personal equipment, the Society for Maternal and Fetal Medicine (SMFM, USA) [23] recommends the following practice in the “COVID-19 Pandemic Ultrasound Practice Suggestions”:
- minimize cluster in ultrasound rooms by removing all unnecessary items (for example, additional bins, chairs);
- in the waiting room remove and keep all other sensors separately when not in use, especially those that are fragile and can be damaged by disinfectant solutions, such as three-dimensional (3D) probes.
To reduce the risk of transmission of COVID-19, it is important: (1) to follow the admission schedule while maintaining the necessary time for each patient; (2) to increase intervals between scans to avoid congestion of waiting patients; (3) to ensure that the distance between the seats in the waiting room is at least 2 m from each other [11].
During the pandemic, scans should be carried out by an experienced staff, the presence of trainees or observers is prohibited [13].
It is recommended not to allow accompanying persons to be in clinics, with the exception of cases of their direct participation in patient care [23].
Avoid the presence of children and persons over 60 years old together with the patient [13, 23].
Other considerations
During the examination, the ISUOG [13] and SMFM [23] consensus statements ask clinicians to consider saving visual information not in the form of separate pictures, but as video loops (clips) containing the image of individual anatomical areas of the fetus, which allows to reduce the study time. After that, in offline mode, without direct contact of sonographers with patients, standard images and measurements can be obtained on the basis of video loops (clips).
Additionally, to minimize the time of personal contact between a sonographer and a patient and ensure maximum safety, individual counseling by a specialist based on the results of an ultrasound examination can be excluded [23]. In this case, the results can be explained by telephone or telemedicine consultation [23].
Ultrasound in early pregnancy in the context of the COVID-19 pandemic
Ultrasound examination is a fundamental link for clinical decision-making in early pregnancy. However, in a pandemic, to reduce the risk of transmitting COVID-19 between patients and health care providers, it is necessary to minimize the visits of pregnant women to clinics. Ultrasound examinations should be carried out only at a high risk of complications, mainly an ectopic pregnancy, in which a visit to a medical institution will be safer than remote consultation [2].
Indications for urgent scan in early pregnancy include [2]:
- pain in the lower abdomen, especially in the presence of risk factors for ectopic pregnancy in patients who have not yet undergone ultrasound examination,
- massive bleeding,
- systemic symptoms of blood loss.
An urgent scan is indicated for clinical signs of septic miscarriage – signs of infection (e.g. temperature, offensive smelling discharge) in association with symptoms of retained pregnancy tissue (pain and/or bleeding). It should be remembered that temperature can be a sign of COVID-19 [18].
If an urgent scan is necessary for a patient with suspicion of (or confirmed) COVID-19, it should be carried out in an isolated room using appropriate personal protective equipment. If technically feasible, a separate ultrasound machine and cabinet for patients with suspected or confirmed COVID-19 is recommended.
It is imperative that equipment disinfection rules are developed specifically for the pandemic period [21].
Suspected patient information regarding possible COVID-19 should be immediately reported to all relevant health authorities.
In the context of the pandemic it is recommended not to conduct ultrasound examinations to simply monitor the development of pregnancy in patients without clinical complaints (including in the presence of complicated obstetrical history), and in the presence of minor discharge from the genital tract without pain.
In the absence of indications for an urgent scan, the first dating scan should be performed at the first trimester screening scan at 11–13 weeks.
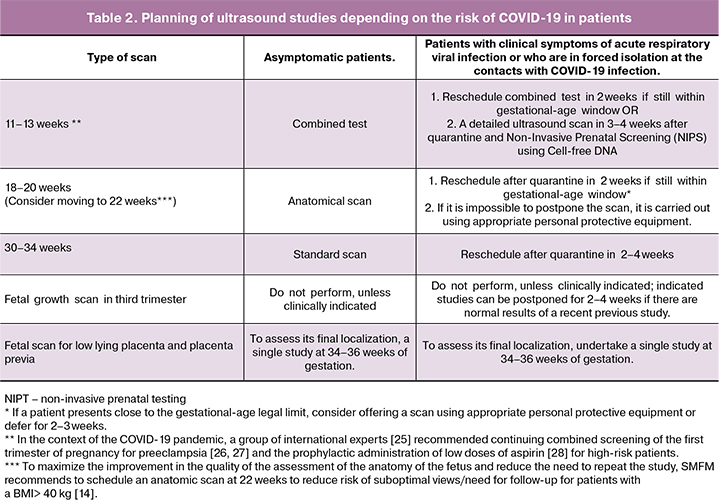
Planning for ultrasound in obstetrics in the context of the COVID-19 pandemic
Taking into account the recommendations of international organizations [13, 23, 24] and the provisions of Russian law [19, 20], for patients without a confirmed diagnosis of COVID-19, the following scheme of planned ultrasound examinations can be proposed (Table 2).
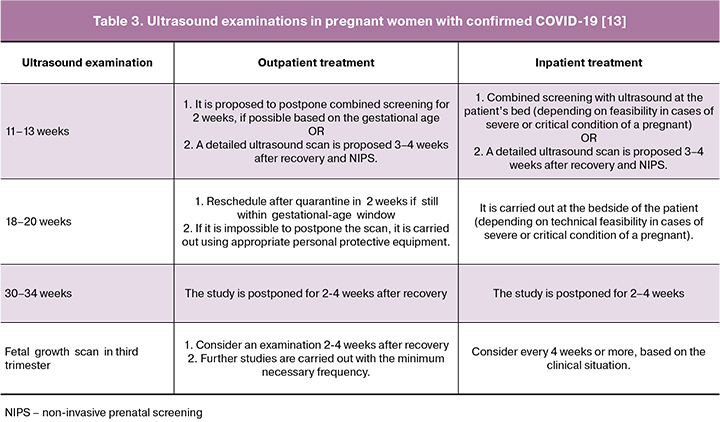
Planning ultrasound examinations in patients with probable or confirmed COVID-19
The following must be taken into account in the necessary order [13, 29, 30]:
Patients suspected of having COVID-19 should be examined in isolation from other women.
Cases of confirmed COVID-19 infection should be examined in an isolated room with negative pressure. If there is a severe condition of the patient this may need to be in the intensive care unit.
Personnel must wear appropriate personal protective equipment.
If necessary, a study to assess fetal growth, amniotic fluid volume, and Doppler of the umbilical artery can be performed at the bedside of the pregnant woman.
Studies should be conducted by an experienced professional to reduce the duration of the examination.
The results of published studies do not report any evidence of a congenital infection in severe acute coronavirus respiratory syndrome (SARS-CoV-2) pregnant women, and there is currently no evidence of a risk of congenital malformations in the first or early second trimester of pregnancy. However, a thorough detailed anatomical ultrasound examination at weeks 18–23 of pregnancy is indicated for pregnant women with confirmed COVID-19.
In women with confirmed COVID-19, everything possible should be done to postpone ultrasound scan if they are not hospitalized [13].
If women are hospitalized, fetal monitoring is necessary [31]. Electronic monitoring of the fetal heart rate and / or ultrasound should be used to assess the condition of the fetus depending on gestational age. Doppler assessment of the presence of fetal heart tones will be sufficient until a viable gestational age is reached and closer monitoring is recommended when the fetus reaches viability [12].
For this group of patients, the following option for planning ultrasound studies can be proposed (Table 3).
Dynamic monitoring of growth and functional status of the fetus in the high-risk group in the context of the COVID-19 pandemic
Patients with preeclampsia, diabetes mellitus, cholestasis, cardiovascular disease, coagulopathy, other chronic diseases as well as cases of abnormal placenta invasion, high risk of chromosomal pathology, congenital malformations and fetal growth restriction (FGR) require close monitoring.
In the pandemic, the frequency of growth scans should be reviewed and minimized [13, 17]. All non-urgent visits to a medical facility should be reduced.
During the COVID-19 pandemic, taking into account the recommendation on social distance and the ratio of benefits and risks, ISUOG [13] recommends additional ultrasound examinations at 28 and 36 weeks of gestation for the following groups of patients:
- Patients with gestational diabetes with satisfactory control of glycemia.
- Patients with chronic diseases (for example, bronchial asthma and epilepsy) who do not receive ongoing medical treatment.
- Patients with a high body mass index.
Based on these recommendations and the order of the Ministry of Health of Russia [19] on the timing of obstetric ultrasound examinations, in organizations where there is Doppler assessment of the pulsatility index of the uterine arteries at 20–24 weeks, it is possible to separate patients for additional assessment of fetal growth in the 3 trimester of pregnancy:
- With normal values of the average pulsatility index of the uterine arteries at 20-24 weeks, the next ultrasound examination is carried out at 34–36 weeks of pregnancy.
- With an increase of the average pulsatility index of the uterine arteries at 20–24 weeks above the 95th percentile, dynamic monitoring of fetal growth from 28 weeks of pregnancy is recommended.
During the pandemic, SMFM recommends [23] to increase the intervals between dynamic observations to 4–8 weeks in the absence of evidence for emergency.
- in case of FGR with estimated fetal weight of more than 3 percentile and normal blood flow in the umbilical arteries, repeat scan can be conducted after 4 weeks.
- in case of early FGR with fetal estimated weight or abdominal circumference of less than the 3rd percentile, the next growth scan should be scheduled in 3 weeks [23].
What to do if there is a lack of ultrasound resources or staff shortages
The Royal College of Obstetricians and Gynecologists (GB) [15] has approved the prioritization of scans, based on evidence and the need to ensure the safety of clinic staff:
- Anatomical ultrasound examination of the fetus at 18–23 weeks of gestation.
- Ultrasound examination ± combined screening at 11–14 weeks.
- Ultrasound studies to assess fetal growth.
The Royal College of Obstetricians and Gynecologists (RCOG) [15] recommends to the heads of clinical departments to carry out preliminary work planning at the beginning of each week and daily distribution of appointments between specialists.
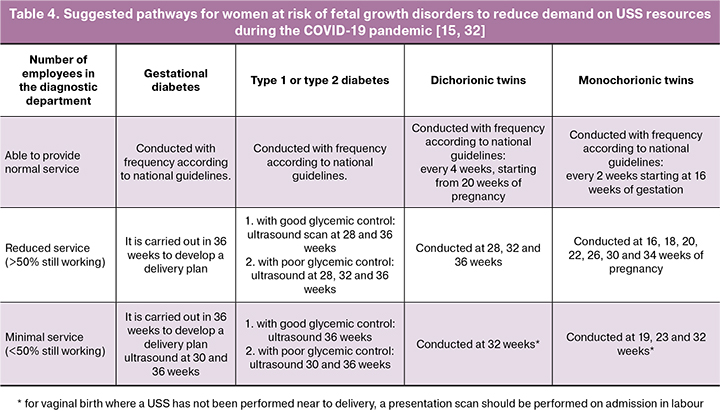
RCOG [15, 32] suggests the following planning scheme, depending on the number of staff in the department. Each organization should modify it, taking into account the current situation (Table 4):
Indications for emergency scan or medical intervention, of primary importance and carried out without delay, regardless of the potential presence of COVID-19 in the patient, are:
- Feto-fetal transfusion syndrome requiring immediate surgical treatment;
- Severe anemia in the fetus with the need for intrauterine correction
- Fetal hydrops;
- Severe FGR in a potentially viable fetus with the estimated mass of more than 500 g).
In these cases the patient should be referred to the regional medical center by prior agreement if it is impossible to provide medical care at the patient’s place of residence [17].
Planning of prenatal echocardiography (ultrasound of the fetal heart) in the context of the COVID-19 pandemic
Considering the fact that prenatal echocardiography is a long-term study, its planning should be commensurate with the priority of patients with urgent need in order to reduce the risk of transmission of viral infection [13].
As in the case of obstetric ultrasound, a three-level approach can be used to prioritize the study [13, 17].
Indications for a planned echocardiographic examination of the fetus are a family history, assisted reproductive technologies, multiple pregnancy, and the use of teratogenic drugs. Routine studies may be postponed for up to four weeks in patients with clinical symptoms of acute respiratory viral infections, patients who are in forced isolation at contacts with COVID-19 or have confirmed COVID-19 [13].
Consider postponing the appointment for 2–4 weeks of urgent echocardiographic examinations with an increased NT of more than 3.5 mm, diabetes mellitus, or maternal epilepsy.
Emergency echocardiographic examinations are carried out immediately in the presence of extracardiac malformations of the fetus or suspected malformations of the heart, when confirmation could significantly affect pregnancy management tactics [13, 17]. It is necessary to use appropriate personal protective equipment if the patient has clinical symptoms of acute respiratory viral infections, risk factors for contacts with COVID-19 or confirmed COVID-19.
If it is necessary to conduct both fetal echocardiography and obstetric ultrasound, they should be organized in one visit of the patient to the clinic [17].
In the pandemic, the number of repeated dynamic observations should be reduced as much as possible [17].
Ultrasound cervical assessment (evaluation of the length of the cervix) in the context of the COVID-19 pandemic
To monitor women at high risk for preterm birth during the COVID-19 pandemic, the following may be recommended:
- If the patient does not have symptoms of infection and no potential contact with COVID-19, measurement of the length of the cervix begins from 16 weeks of pregnancy, if necessary. If the length of the cervix is stable at 18 and 20 weeks, further routine monitoring of cervical condition is not performed [13].
- If the patient has clinical symptoms of infection or potential contacts with COVID-19, it is recommended to prescribe progesterone, if not prescribed earlier, and postpone the visit until the end of the self-isolation / quarantine period [13].
In patients at low risk for preterm birth, it is recommended [23] to perform a transabdominal assessment of the length of the cervix during the second trimester scan, with a refinement of the length measurement by transvaginal ultrasound only in those women whose primary measurement is less than 35 mm.
Planning for diagnostic invasive procedures in the context of the COVID-19 pandemic
According to the temporary guidelines of the Ministry of Health of the Russian Federation “Prevention, diagnosis and treatment of new coronavirus infection (COVID-19)” [11] in pregnant women before 12 weeks of gestation with moderate and severe course of the disease, termination of pregnancy after curing the infection process should be discussed, due to possible embryotoxic effect of drugs.
Given the unstated [12, 13], but probable risk [33] of transmission of the pathogen COVID-19 from mother to fetus during an invasive procedure (based on the available data on the possible vertical transmission of human immunodeficiency virus, hepatitis B, hepatitis C, cytomegalovirus and herpes simplex virus in during invasive testing), in patients with a suspected or probable COVID-19 infection, it is recommended to postpone an invasive procedures for 14 days [12, 13] with amniocentesis preferred over chorionic villus aspiration [13].
If necessary, conducting amniocentesis to detect intrauterine infection and inflammation, it is important to discuss with the patient the expected benefits and possible risks, having received her informed consent [12].
Perinatal consilium for congenital malformations of the fetus in the context of the COVID-19 pandemic
Cases of congenital fetal pathology with possible indications for pregnancy termination should be discussed weekly with participation of neonatologists, cardiologists, and geneticists. In the pandemic, it is possible to conduct consiliums by teleconference [23].
In cases when a consultant is on self-isolation, it is possible to obtain the consultation by phone or video call [17].
If her/his state of health does not allow for a medical consultation, you can replace the consultant with the most competent specialist in this field from those who are present at the workplace [17].
Summary
The above international recommendations serve as the basis for organizing the work of ultrasound diagnostic specialists in obstetrics in the context of the worldwide spread of new coronavirus infection (COVID-19). Strict adherence to the rules of planning and the safe implementation of obstetric ultrasound examinations, thorough disinfection and processing of equipment, the correct use of personal protective equipment will reduce the risk of infection for staff and patients, create the conditions for the full-fledged work of diagnostic departments, saving the lives of unborn children and their mothers.
References
- Конституция Российской Федерации. Доступно по: https://constitutionrf.ru/rzd-1/gl-2/st-38-krf [Constitution of the Russian Federation (in Russian). Available at: http://constitutionrf.ru/rzd-1/gl-2/st-38-krf].
- Bourne T., Kyriacou C., Coomarasamy A., Al-Memar M., Leonardi M., Kirk E. et al. ISUOG Consensus Statement on rationalization of early-pregnancy care and provision of ultrasonography in context of SARS-CoV-2. Ultrasound Obstet. Gynecol. 2020; Apr 8. https://dx.doi.org/10.1002/uog.22046.
- Karim J.N., Roberts N.W., Salomon L.J., Papageorghiou A.T. Systematic review of first-trimester ultrasound screening for detection of fetal structural anomalies and factors that affect screening performance. Ultrasound Obstet. Gynecol. 2017; 50(4): 429-41. https://dx.doi.org/10.1002/uog.17246.
- Бартагова М.Н., Гасанова Р.М., Марзоева О.В. Пренатальное консультирование при врожденном пороке сердца у плода в аспекте возможного сочетанного поражения центральной нервной системы. Бюллетень НЦССХ им. АН Бакулева РАМН. Сердечно-сосудистые заболевания. 2019; (Приложение 11): 182. [Bartagova M.N., Hasanova R.M., Marzoeva O.V.Prenatal counseling for congenital heart disease in the fetus in terms of a possible combined lesion of the central nervous system. Bulletin NTSSSH them. AN Bakuleva RAMS. Cardiovascular Disease. 2019; 20(Suppl.11): 182. (in Russian)].
- Williams M., Turner S., Butler E., Gardosi J. Fetal growth surveillance - Current guidelines, practices and challenges. Ultrasound. 2018; 26(2): 69-79. https://dx.doi.org/10.1177/1742271X18760657.
- Rolnik D.L., Wright D., Poon L.C.Y., Syngelaki A., O’Gorman N., de Paco Matallana C. et al. ASPRE trial: performance of screening for preterm pre‐eclampsia. Ultrasound Obstet. Gynecol. 2017; 50(4): 492-5. https://dx.doi.org/10.1002/uog.18816.
- Холин А.М., Ходжаева З.С., Гус А.И. Патологическая плацентация и прогнозирование преэклампсии и задержки роста плода в первом триместре. Акушерство и гинекология. 2018; 5: 12-9. https://dx.doi.org/10.18565/aig.2018.5.12-19. [Kholin A.M., Khodzhaeva Z.S., Gus A.I. Pathological placentation and prediction of preeclampsia and intrauterine growth restriction in the first trimester. Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2018; (5): 12-9. (in Russian)]. https://dx.doi.org/10.18565/aig.2018.5.12-19.
- Berghella V., Palacio M., Ness A., Alfirevic Z., Nicolaides K. H., Saccone G. Cervical length screening for prevention of preterm birth in singleton pregnancy with threatened preterm labor: systematic review and meta-analysis of randomized controlled trials using individual patient-level data. Ultrasound Obstet. Gynecol. 2017; 49(3): 322-9. https://dx.doi.org/10.1002/uog.17388.
- Бабич Д.А., Баев О.Р., Федоткина Е.П., Гус А.И. Диагностические возможности эхоэластографии в акушерстве и гинекологии. Акушерство и гинекология. 2019; 7: 5-12. https://dx.doi.org/10.18565/aig.2019.7.5-12. [Babich D.A., Baev O.R., Fedotkina E.P., Gus A.I. Diagnostic opportunities of echo elastography in obstetrics and gynecology. Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2019; (7): 5-12. (in Russian)]. https://dx.doi.org/10.18565/aig.2019.7.5-12.
- Akolekar R., Tokunaka M., Ortega N., Syngelaki A., Nicolaides K.H. Prediction of stillbirth from maternal factors, fetal biometry and uterine artery Doppler at 19-24 weeks. Ultrasound Obstet. Gynecol. 2016; 48(5): 624-30. https://dx.doi.org/10.1002/uog.17295.
- Временные методические рекомендации «Профилактика, диагностика и лечение новой коронавирусной инфекции (COVID-19)» Министерство здравоохранения Российской Федерации. М.; 2020. Доступно по: https://www.rosminzdrav.ru/ministry/med_covid19 [Temporary guidelines «Prevention, diagnosis and treatment of new coronavirus infection (COVID-19)», Ministry of Health of the Russian Federation. Moscow; 2020. (in Russian)]. Available at: https://www.rosminzdrav.ru/ministry/med_covid19
- Chen D., Yang H., Cao Y., Cheng W., Duan T., Fan C. et al. Expert consensus for managing pregnant women and neonates born to mothers with suspected or confirmed novel coronavirus (COVID‐19) infection. Int. J. Gynecol. Obstet. 2020; 149(2): 130-6. https://dx.doi.org/10.1002/ijgo.13146.
- Abu-Rustum R.S., Akolekar R., Sotiriadis A., Salomon L.J., Da Silva C.F., Wu Q., Poon L.C. ISUOG Consensus Statement on organization of routine and specialist obstetric ultrasound services in the context of COVID-19. Ultrasound Obstet. Gynecol. 2020; Mar 31. https://dx.doi.org/10.1002/uog.22029.
- Boelig R.C., Saccone G., Bellussi F., Berghella V. MFM guidance for COVID-19. Am. J. Obstet. Gynecol. MFM. 2020; March 19: 100106. https://dx.doi.org/10.1016/j.ajogmf.2020.100106.
- RCOG Guidance for antenatal screening and ultrasound in pregnancy in the evolving coronavirus (COVID-19) pandemic. 2020. Available at: https://www.rcog.org.uk/globalassets/documents/guidelines/2020-03-25-covid19-antenatal-screening.pdf.
- Rasmussen S.A., Smulian J.C., Lednicky J.A., Wen T.S., Jamieson D.J. Coronavirus disease 2019 (COVID-19) and pregnancy: What obstetricians need to know. Am. J. Obstet. Gynecol. 2020; 222(5): 415-26. https://dx.doi.org/10.1016/j.ajog.2020.02.017.
- RCOG Guidance for fetal medicine units (FMUs) in the evolving coronavirus (COVID19) pandemic. 2020. Available at: https://www.rcog.org.uk/globalassets/documents/guidelines/2020-03-25-covid19-fetal-medicine.pdf
- RCOG Guidance for rationalising early pregnancy services in the evolving coronavirus (COVID-19) pandemic. 2020. Available at: https://www.rcog.org.uk/globalassets/documents/guidelines/2020-04-21-guidance-for-rationalising-early-pregnancy-services-in-the-evolving-coronavirus-covid-19-pandemic.pdf
- Приказ Министерства здравоохранения Российской Федерации. Об утверждении Порядка оказания медицинской помощи по профилю «акушерство и гинекология (за исключением использования вспомогательных репродуктивных технологий)» от 01.11. 2012 г. № 572н (ред. от 11.06. 2015 г.). Электронный ресурс. Режим доступа: http://base. garant.ru -2013. [Order of the Ministry of Health of the Russian Federation. On approval of the Procedure for the provision of medical care in the profile «Obstetrics and Gynecology (except for the use of assisted reproductive technologies)» dated 01.11. 2012 No. 572n (as amended on June 11, 2015). Electronic resource. Access Mode: http: // base. garant.ru - 2013.(in Russian)].
- Министерство здравоохранения Российской Федерации. Клинические рекомендации «Нормальная беременность». Российское общество акушеров-гинекологов; 2019. [Ministry of Health of the Russian Federation. Clinical Recommendations «Normal Pregnancy». 2019. (in Russian)].
- Poon L.C., Abramowicz J.S., Dall’Asta A., Sande R., ter Haar G., Marsal K. et al. ISUOG Safety Committee Position Statement: safe performance of obstetric and gynecological scans and equipment cleaning in the context of COVID-19. Ultrasound Obstet. Gynecol. 2020; 55(5): 709-12. https://dx.doi.org/10.1002/uog.22027. Available al: https://www.isuog.org/resource/isuog-safety-committee-statement-covid19-russian-pdf.html.
- Abramowicz J.S., Basseal J.M., Brezinka C., Dall’Asta A., Deng J., Harrison G. et al. ISUOG Safety Committee Position Statement on use of personal protective equipment and hazard mitigation in relation to SARS-CoV-2 for practitioners undertaking obstetric and gynecological ultrasound. Ultrasound Obstet. Gynecol. 2020; Apr 7. https://dx.doi.org/10.1002/uog.22035. Available al: https://www.isuog.org/uploads/assets/9ad9b418-dff8-4da0-9027dd4a751462af/ISUOG-Safety-Committee-statement-COVID19-and-PPE.pdf.
- The Society for Maternal-Fetal Medicine COVID-19 ultrasound practice suggestions. 2020. Available al: https://s3.amazonaws.com/cdn.smfm.org/media/2272/Ultrasound_Covid19_Suggestions_(final)_03-24-20_(2)_PDF.pdf.
- RCOG Guidance for antenatal and postnatal services in the evolving coronavirus (COVID-19) pandemic. 30 March 2020. Available al: https://www.rcog.org.uk/globalassets/documents/guidelines/2020-03-30-guidance-for-antenatal-and-postnatal-services-in-the-evolving-coronavirus-covid-19-pandemic-20200331.pdf.
- Kwiatkowski S., Borowski D., Kajdy A., Poon L.C., Rokita W., WielgoŚ M. Why we should not stop giving aspirin to pregnant women during the COVID-19 pandemic. Ultrasound Obstet. Gynecol. 2020; Apr 18. https://dx.doi.org/10.1002/uog.22049.
- Poon L.C., Shennan A., Hyett J.A., Kapur A., Hadar E., Divakar H. et al. The International Federation of Gynecology and Obstetrics (FIGO) initiative on pre‐eclampsia: A pragmatic guide for first‐trimester screening and prevention. Int. J. Gynaecol. Obstet. 2019; 145(Suppl. 1): 1-33. https://dxdoi.org/10.1002/ijgo.12802.
- Ярыгина Т.А., Батаева Р.С. Методика проведения скринингового исследования в первом триместре беременности с расчетом риска развития преэклампсии и задержки роста плода по алгоритму Фонда медицины плода (Fetal Medicine Foundation). Ультразвуковая и функциональная диагностика. 2018; 4: 77-88. [Yarygina T.A., Batayeva R.S. Methods of screening in the first trimester of pregnancy with the calculation of the risk of preeclampsia and fetal growth retardation according to the algorithm of the Fetal Medicine Foundation. Ul’trazvukovaya i funktsional’naya diagnostika/Ultrasound and Functional Diagnostics. 2018; (4): 77-88.(in Russian)].
- Wright D., Poon L.C., Rolnik D.L., Syngelaki A., Delgado J.L., Vojtassakova D. et al. Aspirin for Evidence-Based Preeclampsia Prevention trial: influence of compliance on beneficial effect of aspirin in prevention of preterm preeclampsia. Am. J. Obstet. Gynecol. 217; 217(6): 685. e1-685. e5. https://dx.doi.org/10.1016/j.ajog.2017.08.110.
- RCOG Coronavirus (COVID-19) Infection in Pregnancy 2020. Version 8: Published Friday 17 April 2020. Available al: https://www.rcog.org.uk/globalassets/documents/guidelines/2020-04-17-coronavirus-covid-19-infection-in-pregnancy.pdf .
- Mullins E., Evans D., Viner R.M., O’Brien P., Morris E. Coronavirus in pregnancy and delivery: rapid review. Ultrasound Obstet. Gynecol. 2020; 55(5): 586-92. https://dx.doi.org/10.1002/uog.22014.
- Poon L.C., Yang H., Lee J.C.S., Copel J.A., Leung T.Y., Zhang Y. et al. ISUOG Interim Guidance on 2019 novel coronavirus infection during pregnancy and puerperium: information for healthcare professionals. Ultrasound Obstet. Gynecol. 2020; 55(5): 700-8. https://dx.doi.org/10.1002/uog.22013.
- England NHS. Saving Babies’ Lives Version 2: A care bundle for reducing perinatal mortality. NHS England; 2019.
- Parazzini F., Bortolus R., Mauri P.A., Favilli A., Gerli S., Ferrazzi E. Delivery in pregnant women infected with SARS-CoV-2: A fast review. Int. J. Gynaecol. Obstet. 2020; Apr 9. https://dx.doi.org/10.1002/ijgo.13166.
Received 06.05.2020
Accepted 12.05.2020
About the Authors
Alexandr I. Gus, M.D., Doctor of Medicine, Professor, the Head of Department of Ultrasound and Functional Diagnostics, Radiology Division, FSBI «National Medical Research Center For Obstetrics, Gynecology And Perinatology Named After Academician V.I. Kulakov» Tel.: +7(495)531-44-44.E-mail: a_gus@oparina4.ru. https://orcid.org/0000-0003-1377-3128. 4, Oparina str., Moscow, 117997, Russian Federation.
Aris Papageorghiou, Professor in Fetal Medicine and obstetrics, Fetal Medicine Unit, St George’s University Hospitals NHS Foundation Trust, London, UK; Clinical research director, Oxford Maternal and Perinatal Health Insitute, Nuffield Department of Women's & Reproductive Health, University of Oxford, UK.
Tel.: +44 (0)1865 221019. E-mail aris.Papageorghiou@wrh.ox.ac.uk.
University of Oxford, Level 3, Women's Centre John Radcliffe Hospital Oxford, UK, OX39DU.
Tamara A. Yarygina, M.D., Department of Ultrasound and Functional Diagnostics, Radiology Division, FSBI «National Medical Research Center For Obstetrics, Gynecology And Perinatology Named After Academician V.I. Kulakov». Tel.: +7 (495) 531–44–44. E-mail: tamarayarygina@gmail.com. https://orcid.org/0000-0001-6140-1930.
4, Oparina str., Moscow, 117997, Russian Federation.
Marina P. Shuvalova, M.D., Ph.D., Associate Professor, Deputy Director - Head of Department for Regional Cooperation and Integration, FSBI «National Medical Research Center For Obstetrics, Gynecology And Perinatology Named After Academician V.I. Kulakov».
Tel.: +7(495)438-76-68 E-mail: m_shuvalova@oparina4.ru. https://orcid.org/0000-0002-6361-9383.
For reference: Gus A.I., Papageorghiou А., Yarygina T.A., Shuvalova M.P. Ultrasound diagnosis in pregnancy in the evolving coronavirus (COVID-19) pandemic.
Akusherstvo i Ginekologiya/ Obstetrics and Gynecology. 2020; 5: 42-51 (In Russian).
https://dx.doi.org/10.18565/aig.2020.5.42-51