Impact of the novel coronavirus infection (COVID-19) experienced by pregnant women on the health of newborns
Background: Due to the high spread rate of SARS-CoV-2 and to the rapid increase in its incidence, including those among pregnant women, the novel coronavirus infection (COVID-19) has become a challenge in modern healthcare. Objective: To analyze the impact of the novel coronavirus infection experienced by pregnant women on the health of newborns in the early neonatal period. Materials and methods: A retrospective analysis was carried out of the birth records of 400 women who had experienced the novel coronavirus infection during pregnancy and the neonatal records of their newborns (n=500) who received health care in the clinical units of the V.I. Kulakov National Medical Research Center of Obstetrics, Gynecology, and Perinatology, Ministry of Health of Russia (Center), in July 2020 to July 2021. A comparison group consisted of randomly selected birth records of 495 pregnant women who had not been infected with COVID-19 and the neonatal records of their babies (n=500) born at the same Center at the same time. Results: The vast majority of women who had been infected with COVID-19 during pregnancy were found to have familial obstetric/gynecological and/or somatic histories. Among the factors aggravating pregnancy in the presence of COVID-19, chronic hypertension, hereditary thrombophilia, fat metabolism disorders, urogenital infections, and anemia are more common than those in the control group (p<0.05). This female group also tended to have miscarriage; however, no statistically significant differences could be detected (p=0.06). There were no statistically significant differences in the term and frequency of cesarean delivery in pregnant women in the study and control groups (p>0.05). Neonates born to women who had been infected with COVID-19 in the first trimester had its statistically significantly higher morbidity rates (p<0.05). The frequency of perinatal complications was higher in newborns whose mothers had experienced the novel coronavirus infection in the first trimester. Neonatal infants borns from women who had a new coronavirus infection in the third trimester, rhinitis and otitis media are statistically significantly more common in the early neonatal period. Among the factors leading to disruption of early neonatal adaptation of children whose mothers had a new coronavirus infection during pregnancy, the following were statistically significantly more common: infectious and inflammatory diseases (rhinitis, otitis media), hemorrhagic syndrome, and hypoglycemia (p<0.05). Neonates born to women who had been infected with COVID-19 in the first trimester were observed to have statistically significantly higher morbidity rates (p<0.05). The incidence of perinatal complications was higher in newborns whose mothers had experienced the novel coronavirus infection in the first trimester. Neonatal infants born to women who had the novel coronavirus infection in the third trimester were statistically significantly more commonly recorded to have rhinitis and otitis media in the early neonatal period. Among the factors leading to failure of early neonatal adaptation of babies whose mothers had the novel coronavirus infection during pregnancy, there were statistically significantly more often infectious and inflammatory diseases (rhinitis, otitis media), hemorrhagic syndrome, and hypoglycemia (p<0.05). Conclusion: The incidence of perinatal complications in babies born to women who had been infected with COVID-19 depended on their gestational age and was higher than that in newborns whose mothers had experienced the novel coronavirus infection in the first trimester. At the same time, the incidence of infectious and inflammatory diseases proved to be higher in infants whose mothers had a coronavirus infection in the third trimester. Failure of early neonatal adaptation of babies born to women who had an infection caused by SARS-CoV-2 during pregnancy may be due to both infectious and non-infectious factors that complicate the course of pregnancy and childbirth.Kosolapova Yu.A., Boris D.A., Poludenko N.D., Makieva M.I., Nikitina I.V., Inviyaeva E.V., Vtorushina V.V., Krechetova L.V., Mikhanoshina N.V., Zubkov V.V., Degtyarev D.N.
Keywords
COVID-19 is an acute infectious disease caused by an RNA-containing virus of the Betacoronavirus genus of the Coronaviridae family. The virus was given the official name of SARS-CoV-2 by the International Committee on Taxonomy of Viruses [1].
During the pandemic in the Russian Federation, its Government Communication Center registered more than 21 million COVID-19 cases. More than 78 thousand cases of COVID-19 varying in severity have been registered in pregnant women in Russia since the start of 2022 [2]. Considering the data available in modern literature, the physiological adaptive changes during pregnancy may be a certain background, in which a pregnant woman’s susceptibility to COVID-19 increases, compared with non-pregnant women of reproductive age [3].
It is customary to diagnose COVID-19 by the detection of SARS-CoV-2 RNA in nasopharyngeal swabs by polymerase chain reaction (PCR), regardless of the clinical manifestations of the disease [4, 5].
According to the literature, pregnant women aged over 35 years with overweight, obesity, chronic hypertension, or diabetes mellitus are a group at highest risk for severe forms of COVID-19 infection [6, 7].
Medical tactics during the course of the novel coronavirus infection depend on the severity of the disease, its clinical presentations, as well as on fetal status, gestational age, and the need to transfer the woman to an appropriate healthcare facility [5].
According to the literature, neonatal infants born to mothers who have experienced the novel coronavirus infection, as well as those born to women with other respiratory viral infections during pregnancy are at higher risk for pathological conditions, such as fetal distress (26.5–30.0%), low birth weight (25.0%), or neonatal asphyxia (1.4%). Neonatal intensive care unit (NICU) admission is required in 43.0% of cases, whereas the perinatal mortality rate is 0.35–2.2%, compared with neonates born to mothers without COVID-19 during pregnancy [8–10].
Objective: to analyze the impact of the novel coronavirus infection (COVID-19) experienced by pregnant women on the health of newborns in the early neonatal period.
Materials and methods
A total of 985 birth records and 1000 neonatal ones of babies born between 26 0/7 and 41 0/7 weeks’ gestation at the Academician V.I. Kulakov National Medical Research Center of Obstetrics, Gynecology, and Perinatology (Center), Ministry of Health of Russia in July 2020 to July 2021 were retrospectively analyzed. The investigation was approved by the local Ethics Committee. Voluntary informed consent to the babies’ participation in the study was signed by the patients’ official representatives.
The patients were divided into 2 groups: a study group of 490 pregnant women who had been infected with COVID-19 and their newborns (n=500) and a comparison group of 495 women without COVID-19 and their babies (n=500). We analyzed the clinical and anamnestic data of the women, the course of their current pregnancy, childbirth, delivery methods, as well as the characteristics of the early neonatal period in their newborns. Their physical developments were assessed using Intergrowth-21st growth curves separately for female and male babies, which took into account the 3rd, 10th, 50th, 90th, and 97th percentiles for their body weight, height, and head circumference [11]. The laboratory and instrumental studies included complete blood count (for all newborns), C-reactive protein test, urinalysis, radiography and ultrasound of the brain and internal organs, echocardiography if indicated for children in need of specialized healthcare care.
Statistical analysis
The results were statistically processed using Microsoft Excel 2013 and Statistica 10 software. The most effective normality test is the Shapiro–Wilk W-test, since it is more powerful than a wide range of alternative normality tests. For normal distribution samples, statistically significant differences between the tests were assessed using Student’s t-tests. Arithmetic mean (M), standard deviation (SD), and a t-test were used for quantitative assessment of normal distribution. If the normal distribution hypothesis was rejected during a check, then the findings were processed using nonparametric statistical methods. Fisher’s exact test was used to compare the groups by qualitative characteristics. Differences were considered statistically significant at p<0.05.
Results and discussion
The women in the study (n = 490) and control (n=495) groups who gave birth to babies between 26 0/7 and 41 6/7 weeks (38.8 (1.8) weeks) of gestation were comparable for age and showed no statistically significant differences (p>0.05).
Considering that the Center is the highest (III B)-level facility in the perinatal care system, where there are more commonly patients with complicated pregnancy or concomitant severe extragenital pathology than those in the general population. An analysis of clinical and anamnestic data has indicated that a greater number of women who were infected with COVID-19 during pregnancy have familial somatic and obstetric/gynecological histories.
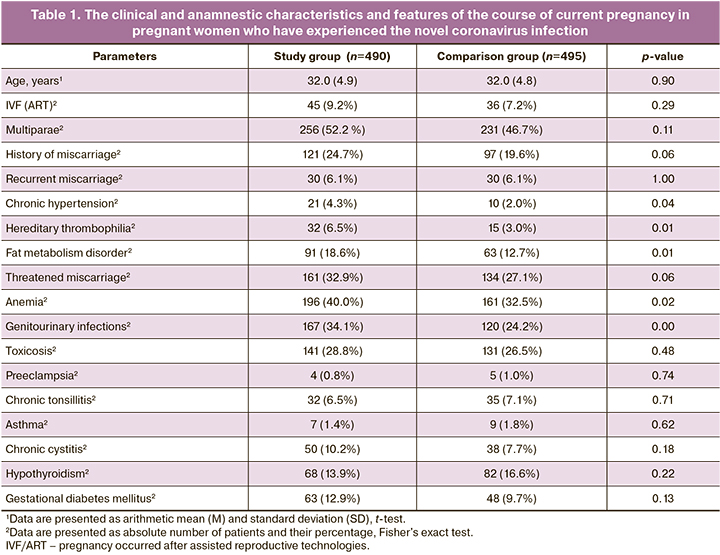
In the pattern of extragenital pathologies, chronic hypertension, hereditary thrombophilia, or fat metabolism disorders were statistically significantly more common in the study group (p<0.05). Respiratory, digestive, and urinary tract diseases were also analyzed; however, no statistically significant differences could be identified. The study group more often included multigravid or multiparous women who had a history of spontaneous miscarriages (121/490 (24.7%) and 97/495 (19.6%)) in the groups, respectively; however, no statistically significant difference could be found (p=0.06).
Analyzing the course of current pregnancy revealed that in the study group women, their pregnancy more frequently occurred in the presence of threatened miscarriage with the formation of retrochorial hematoma in the first trimester; however, no statistically significant differences could be detected (p=0.09). In the second and third trimesters, anemia and exacerbation of genitourinary infections were statistically significantly more often seen in the study group (p<0.05).
The clinical characteristics of pregnant women and the features of their current pregnancy are described in Table 1.
The women delivered between 26 0/7 and 41 6/7 weeks’ gestation; their singleton and multiple pregnancies accounted for 480/490 (98.0%) and 10/490 (2.0%) cases, respectively. Most (445/490 (90.8%)) of the pregnancies occurred spontaneously; 45/490 (9.2%) pregnancies did after assisted reproductive technologies. The pregnant women in the study control groups showed no statistically significant differences in the term and frequency of cesarean delivery (p>0.05). There were 151/490 (30.8%) and 151/495 (30.5%) cesarean deliveries in the study and control groups, respectively; 339/490 (69.2%) and 344/495 (69.5%) natural births were observed in these groups.
The gestational age (GA) distribution of newborns was comparable in the study and control groups: 9/500 (1.8%) and 6/500 (1.2%) births at 22–33 weeks’ gestation (p>0.05); 28/500 (5.6%) and 25/500 (5.0%) births at 34-36 weeks (p>0.05); and 463/500 (92.6%) and 469/500 (93.8%) births at 37–41 weeks (p>0.05). There were 37/500 (7.4%) and 31/500 (6.2%) preterm births in the study and control groups, respectively (p>0.05). It is important to note that the relative number of premature babies born to women who had experienced the novel coronavirus infection in the first trimester was statistically significantly higher than those born to women who had this disease in the second and third trimesters: 92/500 (18.4%) versus 27/500 (5.4%) and 24/500 (4.8%) babies, respectively (p<0.05).
GA, sex, anthropometric characteristics, and Apgar scores for newborns at one minute and five minutes after their birth are given in Table 2.
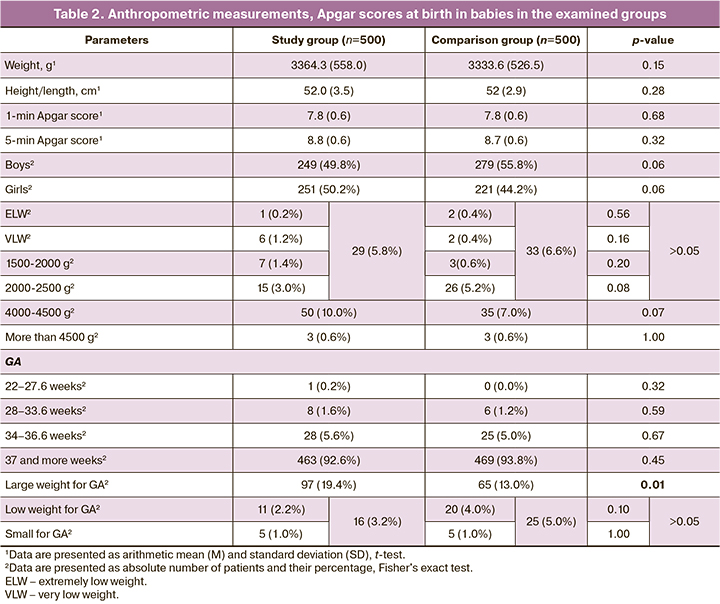
Analyzing anthropometric measurements, GA, and Apgar scores could reveal no statistically significant differences in the assessed groups (p>0.05). Birth weight at term delivery was 3453 (442) and 3396 (437) g in the study and control groups, respectively (p>0.05); that at preterm birth was 2255 (670) and 2391 (777) g in the groups (p>0.05). However, despite the comparability of the groups for birth weight, it is noteworthy that in the study group, the newborns large for GA were born statistically significantly more often (physical development indicators of more than the 90th percentile according to the Intergrowth-21 growth curves): 97/500 (19.4%) versus 65/500 (13.0%) in the groups, respectively (p<0.05).
The signs of intrauterine growth restriction (a baby’s physical development at birth below the 10th percentile according to Intergrowth-21 growth curves) among the neonates born to mothers who had been infected with COVID-19 during pregnancy occurred in 16/500 (3.2%) cases. In the comparison group, among the newborns, physical development indicators of less than the 10th percentile according to the Intergrowth-21 curves were found in 25/500 (5.0%) cases (p>0.05).
Specialized medical care in the NICU was required in 48/500 (9.6%) and 40/500 (8.0%) newborns in the study and control groups, respectively (p>0.05). Non-invasive respiratory therapy was performed in 21/500 (4.2%) cases of the total number of babies in the study group and in 23/500 (4.6%) in the comparison group (p>0.05); mechanical ventilation was needed in 15/500 (3.0%) and 19/500 (3.8%) infants, respectively (p>0.05). Despite NICU therapy, two children died in the study group. The cause of death was congenital bacterial pneumonia in one case with extreme morphological and functional immaturity (at 27 weeks’ gestation) and massive intraventricular hemorrhage in the other case – a late preterm baby. No direct causal relationship could be identified between the babies’ death and maternal COVID-19 disease during pregnancy in any case.
Monitoring and treatment were done in 84/500 (16.8%) newborns in the Unit of Pathology of Newborns and Premature Children and in more than half (49/500 (9.8%)) of them after completion of therapy in the intensive care unit. In the comparison group, 68/500 (13.6%) newborns needed specialized medical care in the neonatal pathology unit (p>0.05).
The incidence of congenital malformations (CMF) due to the high concentration of high-risk pregnant women at the V.I. Kulakov Center was comparable: 16/500 (3.2%) and 22/500 (4.4%) cases in the study and comparison groups, respectively; while that of congenital heart defects (CHD) was 23/500 (4.6%) and 27/500 (5.4%) (p>0.05). Attention is drawn to the incidence of interatrial communications measuring 5 mm or more and to that of congenital cerebral cysts, mainly in babies born to women who were infected with COVID-19 in the second and third trimesters. Thus, there was an interatrial communication in 58/500 (11.6%) infants in the study group and in 37/500 (7.4%) in the control group (p<0.05) and congenital cerebral cysts in 120/500 (24.0%) and 65/500 (13.0%) babies in the study and control groups, respectively (p<0.05).
In the study group, 4/500 (0.8%) children were born with CMF requiring early surgical correction. One child was treated in the Neonatal Surgery Department of the Center for congenital intralobar sequestration of the right lower lobe of the lung. The other 3 children with critical heart defects were transferred to the A.N. Bakulev National Medical Research Center for Cardiovascular Surgery. At the same time, no direct causal relationship was found between fetal CMF and maternal COVID-19 disease during pregnancy, since the women were recorded to have a SARS-CoV-2 contact at 12 weeks or more of gestation.
NICU admissions from the delivery room occurred in 38/500 (7.6%) and 27/500 (5.5%) babies in the study and control groups, respectively (p>0.05). It is noteworthy that 16/38 (42.1%) infants were full-term in the study group, while only 6/27 (22.0%) full-term children in the control group were admitted to the NICU (p=0.03). The main reasons for NICU admission in the study group were CHD and CMF in 5/38 (13.2%) infants requiring neonatal intensive monitoring, as well as transient tachypnea of the newborn (TTN), respiratory distress syndrome (RDS) in 14/38 (36.8%), and congenital pneumonia in 18/38 (47.4%). In the control group, the reasons for NICU admission were TTN and RDS in 16/27 (59.3%) cases and congenital pneumonia in 11/27 (40.7%). This distribution of newborns seems to be associated with a large number of high-risk perinatal women admitting to the Center (a level IIIB hospital). After their condition stabilization, the children were transferred from the intensive care unit to the neonatal pathology unit.
Despite complicated pregnancies, the majority (444/500 (88.8%) and 447/500 (89.4%)) of babies were born in a satisfactory condition in the study and control groups, respectively, and were monitored in the postpartum department of the obstetric hospital. When monitored in the department, 35/500 (7.0%) babies in each group had failure of early neonatal adaptation, which required their transfer to specialized neonatal departments of the Center. On days 2 and 3 of life, of them, 9/500 (1.8%) and 13/500 (2.6%) postpartum department infants required specialized medical care in the NICU (p>0.05). 26/500 (5.2%) newborns in the study group and 22/500 (4.4%) ones in the control group (> 0.05) were transferred from the postpartum department to the neonatal pathology department for further monitoring, examination, and treatment within the first three days of the early neonatal period The remaining (409/500 (81.8%) and 412/500 (82.4%)) newborns in the examined groups (p>0.05) were discharged home from the postpartum department in a satisfactory condition to be followed up by a local pediatrician.
It is important to note that the morbidity rates in 132/500 (26.4%) children whose mothers had experienced the coronavirus infection in the first trimester were statistically significantly higher than those in 74/500 (14.8 %) and 93/500 (18.6%) children whose mothers had been ill in the second and third trimesters, respectively (p<0.05).
Despite the fact that in the study group, perinatal contact with a novel coronavirus-infected person after birth cannot be ruled out in 19 children, polymerase chain reaction could detect SARS-CoV-2 in the nasopharyngeal swabs of none of the children in the first 2 hours of life, on day 3, and at the time of discharge.
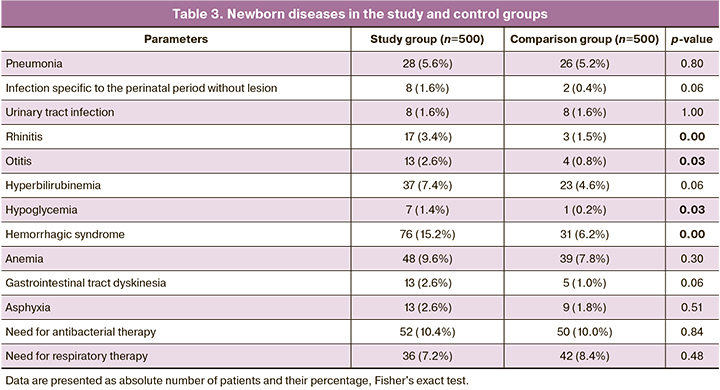
The condition severity in the study group children in need of inpatient treatment was due to perinatal infections (pneumonia, rhinitis, otitis media), hemorrhagic conditions, transient metabolic disorders (neonatal hypoglycemia, neonatal hyperbilirubinemia), and gastrointestinal tract dyskinesia. At the same time, the detection rates for rhinitis, otitis, hypoglycemia, and hemorrhagic syndrome in the newborns of the study group were statistically significantly higher than in those of the comparison group (Table 3).
Conclusions
1. COVID-19 disease during pregnancy is statistically significant more common in women with chronic hypertension, hereditary thrombophilia, lipid metabolism disorders, genitourinary infections, and anemia.
2. Statistically significantly higher morbidity is seen in neonatal infants born to women who have been infected with COVID-19 in the first trimester (p<0.05). It should also be noted that this group of women tended to have miscarriage, but there were no statistically significant differences (p=0.06).
3. Neonates born to women who have experienced the novel coronavirus infection in the third trimester are statistically significantly more recorded to have rhinitis and otitis media in the early neonatal period.
4. Failure of early neonatal adaptation of babies born to women who have been infected with SARS-CoV-2 during pregnancy may be due both to infectious and non-infectious factors that complicate the course of pregnancy and childbirth.
References
- ICTV. Current ICTV Taxonomy Release. Virus Taxonomy: 2021 Release.
- Отчет о текущей ситуации по борьбе с коронавирусом COVID-19. Коммуникационный центр Правительства Российской Федерации. 2022. [Report on the current situation in the fight against the COVID-19. Communication Center of the Government of the Russian Federation. 2022.(in Russian)].
- de Medeiros K.S., Sarmento A.C.A., Costa A.P.F., Macêdo L.T.A., da Silva L.A.S., de Freitas C.L. et al. Consequences and implications of the coronavirus disease (COVID-19) on pregnancy and newborns: A comprehensive systematic review and meta-analysis. Int. J. Gynecol. Obstet. 2022; 156(3): 394-405.https://dx.doi.org/10.1002/ijgo.14015.
- Абатуров А.Е., Агафонова Е.А., Кривуша Е.Л., Никулина А.А. Патогенез covid-19. Здоровье ребенка. 2020; 15(2): 133-44. [Abaturov A.E., Agafonova E.A., Krivusha E.L., Nikulina A.A. Pathogenesis of covid-19.Child Health. 2020; 15(2): 133-44. (in Russian)].
- Методические рекомендации "Организация оказания медицинской помощи беременным, роженицам, родильницам и новорожденным при новой коронавирусной инфекции COVID-19". [Guidelines "Organization of medical care for pregnant, parturient, and puerperal women and newborns with a new coronavirus infection COVID-19". (in Russian)].Available at: https://static-minzdrav.gov.ru/system/attachments/attaches/000/057/333/original/05072021_MR_Preg_v4.pdf
- Coronavirus (COVID-19) Infection in pregnancy. Information for healthcare professionals. Version 15. 2022.
- Петрова У.Л., Шмаков Р.Г. Новая коронавирусная инфекция 2019 и беременность: что мы знаем? Акушерство и гинекология. 2022; 2: 4-11.https://dx.doi.org/10.18565/aig.2022.2.4-11. [Petrova U.L., Shmakov R.G. The 2019 novel coronavirus infection and pregnancy: What do we know? Obstetrics and Gynecology. 2022; 2: 4-11. (in Russian)]. https://dx.doi.org/10.18565/aig.2022.2.4-11.
- Jafari M., Pormohammad A., Neshin S.A.S., Ghorbani S., Bose D.,Alimohammad S. et al. Clinical characteristics and outcomes of pregnant women with COVID-19 and comparison with control patients: A systematic review and meta-analysis. Rev. Med. Virol. 2021; 31(5): 1-16. https://dx.doi.org/10.1002/rmv.2208.
- Никитина И.В., Донников А.Е., Крог-Йенсен О.А., Ленюшкина А.А., Дегтярева Н.Д. Роль ренин-ангиотензиновой системы, иммунологических и генетических факторов в реализации COVID-19 у детей. Российский Вестник перинатологии и педиатрии. 2020; 65(4): 16-26. [Nikitina I.V., Donnikov A.E., Krog-Jensen O.A., Lenyushkina A.A., Degtyareva N.D. The role of the renin-angiotensin system, immunological and genetic factors in children with COVID-19. Ros Vestn Perinatol i Pediatr/Russian Bulletin of Perinatology and Pediatrics. 2020; 65(4): 16-26. (in Russian)].
- Сугак А.Б., Гребнева О.В., Никитина И.В., Филиппова Е.А., Караваева А.Л.,Тимофеева Л.А., Зубков В.В., Косолапова Ю.А., Макиева М.И.,Дегтярев Д.Н. Первичное скрининговое ультразвуковое исследование новорожденных от матерей, перенесших COVID-19 во время беременности. Неонатология: новости, мнения, обучение. 2021; 9(2): 7-14. https://dx.doi.org/10.33029/2308-2402-2021-9-2-7-14. [Sugak A.B., Grebneva O.V., Nikitina I.V., Filippova E.A., Karavaeva A.L., Timofeeva L.A., Zubkov V.V., Kosolapova Yu.A., Makieva M.I., Degtyarev D.N. Ultrasound screening of newborns from mothers with COVID-19 during pregnancy. Neonatologia: novosti, mneniya, obuchenie/Neonatology: News, Opinions, Training. 2021; 9(2): 7-14. (in Russian)]. https://dx.doi.org/10.33029/2308-2402-2021-9-2-7-14.
- Рюмина И.И., Маркелова М.М., Нароган М.В., Орловская И.В., Перепелкина А.Е., Рындин А.Ю., Гатина Е.А. Малькова Е.А., Косолапова Ю.А., Артамкина Е.И., Соколова Е.В., Титова Е.В., Кириллова Е.А., Деревягина О.С., Зубков В.В. Байбарина Е.Н. Опыт внедрения международных стандартов оценки роста новорожденного INTERGROWTH-21st. Российский вестник перинатологии и педиатрии. 2021; 66(1): 117-24. https://dx.doi.org/10.21508/1027-4065-2021-66-1-117-124. [Ryumina I.I., Markelova M.M., Narogan M.V., Orlovskaya I.V., Perepelkina A.E. et al. Experience in implementing the International Standarts for Assessing Newborn Growth INTERGROWTH-21st. Ros Vestn Perinatol i Pediatr/Russian Bulletin of Perinatology and Pediatrics. 2021; 66(1): 117-24.(in Russian)]. https://dx.doi.org/10.21508/1027-4065-2021-66-1-117-124.
Received 12.08.2022
Accepted 05.09.2022
About the Authors
Yulia A. Kosolapova, Neonatologist, Junior Researcher, Neonatal Department Two, Academician V.I. Kulakov National Medical Research Center for Obstetrics, Gynecology and Perinatology, Ministry of Health of Russia, yu_kosolapova@oparina4.ru, https://orcid.org/0000-0001-8180-3275, 4, Academician Oparin str., Moscow, 117997, Russia.Dayana A. Boris, PhD, Researcher, Academician V.I. Kulakov National Medical Research Center for Obstetrics, Gynecology and Perinatology, Ministry of Health of Russia, dayana_boris@mail.ru, https://orcid.org/0000-0002-0387-4040, 4, Academician Oparin str., Moscow, 117997, Russia.
Natalya D. Poludenko, Clinical Resident, Department of Neonatology, Institute of Neonatology and Pediatrics, Academician V.I. Kulakov National Medical Research Center
for Obstetrics, Gynecology and Perinatology, Ministry of Health of Russia, Natasha-polud@mail.ru, https://orcid.org/0000-0002-1438-7344,
4, Academician Oparin str., Moscow, 117997, Russia.
Mziya I. Makieva, PhD, Neonatologist, Head, Neonatal Department Two, Academician V.I. Kulakov National Medical Research Center for Obstetrics, Gynecology and Perinatology, Ministry of Health of Russia, m_makieva@oparina4.ru, https://orcid.org/0000-0002-2632-4666, 4, Academician Oparin str., Moscow, 117997, Russia.
Irina V. Nikitina, Dr. Med. Sci., Leading Researcher, Resuscitation and Intensive Care Department Two, Institute of Neonatology and Pediatrics, Associate Professor, Department of Neonatology, Academician V.I. Kulakov National Medical Research Center for Obstetrics, Gynecology and Perinatology, Ministry of Health of Russia,
i_nikitina@oparina4.ru, https://orcid.org/0000-0002-1103-1908, 4, Academician Oparin str., Moscow, 117997, Russia.
Evgeniya V. Inviyaeva, PhD (Bio), Senior Researcher, Laboratory of Clinical Immunology, Academician V.I. Kulakov National Medical Research Center for Obstetrics, Gynecology and Perinatology, Ministry of Health of Russia, e_inviyaeva@oparina4.ru, https://orcid.org/0000-0001-9878-3637,
4, Academician Oparin str., Moscow, 117997, Russia.
Valentina V. Vtorushina, PhD, Allergist/Immunologist, Laboratory of Clinical Immunology, Academician V.I. Kulakov National Medical Research Center for Obstetrics, Gynecology and Perinatology, Ministry of Health of Russia, v_vtorushina@oparina4.ru, https://orcid.org/0000-0002-8406-3206,
4, Academician Oparin str., Moscow, 117997, Russia.
Lyubov V. Krechetova, Dr. Med. Sci., Head, Laboratory of Clinical Immunology, Academician V.I. Kulakov National Medical Research Center for Obstetrics, Gynecology and Perinatology, Ministry of Health of Russia, l_krechetova@oparina4.ru, https://orcid.org/0000-0001-5023-3476, 4, Academician Oparin str., Moscow, 117997, Russia.
Natalya V. Mikhanoshina, Head, Laboratory for Biomaterial Collection and Storage (Biobank), Academician V.I. Kulakov National Medical Research Center for Obstetrics, Gynecology and Perinatology, Ministry of Health of Russia, Mikhanoshina.Natalya@Yandex.Ru, Https://Orcid.Org/0000-0002-2868-0867,
4, Academician Oparin str., Moscow, 117997, Russia.
Viktor V. Zubkov, Dr. Med. Sci., Director, Institute of Neonatology and Pediatrics, Academician V.I. Kulakov National Medical Research Center for Obstetrics,
Gynecology and Perinatology, Ministry of Health of Russia; Professor, Department of Neonatology of the N.F. Filatov Clinical Institute of Children's Health, I.M. Sechenov
First Moscow State Medical University (Sechenov University), Ministry of Health of Russia, v_zubkov@oparina4.ru, https://orcid.org/0000-0001-8366-5208,
4, Academician Oparin str., Moscow, 117997, Russia.
Dmitriy N. Degtyarev, Dr. Med. Sci., Professor, Deputy Director for Research, Academician V.I. Kulakov National Medical Research Center for Obstetrics,
Gynecology and Perinatology, Ministry of Health of Russia; Head, Department of Neonatology, I.M. Sechenov First Moscow State Medical University (Sechenov University), Ministry of Health of Russia, d_degtiarev@oparina4.ru, https://orcid.org/0000-0001-8975-2425, 4, Academician Oparin str., Moscow, 117997, Russia.
Corresponding author: Yulia A. Kosolapova, yu_kosolapova@oparina4.ru
Authors’ contributions: Kosolapova Yu.A., Boris D.A., Poludenko N.D., Makieva M.I., Nikitina I.V., Inviyaeva E.V.,
Vtorushina V.V., Krechetova L.V., Mikhanoshina N.V., Zubkov V.V., Degtyarev D.N. – development of the design of the investigation, obtaining data for analysis, review of publications on the topic of the article, statistical analysis of the findings, writing the text of the manuscript.
Conflicts of interest: The authors declare that there are no possible conflicts of interest.
Funding: The investigation has not been sponsored.
Ethical Approval: The investigation has been approved by the local Ethics Committee, Academician V.I. Kulakov National Medical Research Center of Obstetrics, Gynecology, and Perinatology, Ministry of Health of Russia.
Patient Consent for Publication: The mothers of newborn infants have signed an informed consent form to the publication of their data.
Authors' Data Sharing Statement: The data supporting the findings of this study are available on request from the corresponding author after approval from the principal investigator.
For citation: Kosolapova Yu.A., Boris D.A., Poludenko N.D., Makieva M.I.,
Nikitina I.V., Inviyaeva E.V., Vtorushina V.V., Krechetova L.V., Mikhanoshina N.V.,
Zubkov V.V., Degtyarev D.N. Impact of the novel coronavirus infection (COVID-19) experienced by pregnant women on the health of newborns.
Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2022; 11: 90-98 (in Russian)
https://dx.doi.org/10.18565/aig.2022.11.90-98