The effect of cytokine therapy on uterine-endometrial blood flow and reproductive function in various morphological types of chronic endometritis
Ozerskaya I.A., Porkhovaty S.Ya., Kazaryan G.G., Ozhogina E.V.
Objective: To evaluate the impact of cytokine therapy on utero-endometrial blood flow in different morphological types of chronic endometritis.
Materials and methods: We analyzed data from 298 women of reproductive age with a confirmed diagnosis of chronic endometritis (CE). The study group comprised 140 patients in whom standard anti-inflammatory therapy was supplemented with Superlymph. The control group included 158 patients treated with a similar regimen but without cytokine therapy. Doppler parameters of uterine artery blood flow were assessed, including arterial perfusion index (API) and volumetric blood flow indices (VI, FI, and VFI).
Results: Following therapy, a significant decrease in vascularization was observed in women with mixed and hyperplastic CE morphotypes, which was attributed to the normalization of venous outflow in the uterine mucosa. However, this pronounced effect was not observed in women with a hypoplastic morphotype. During the first six months after completing complex treatment with exogenous cytokines, clinical pregnancy rates were 38.8% in the study group compared to 27.5% in those receiving only anti-inflammatory therapy (RR=1.412; 95% CI 1.008–1.997). In the study group, pregnancy occurred 1.9 times more frequently in women with hyperplastic macrotype than in those with hypoplastic macrotype CE.
Conclusion: The administration of exogenous cytokines, in conjunction with anti-inflammatory therapy, restores venous outflow in the endometrium for mixed and hyperplastic macrotypes of CE, while enhancing the effectiveness of pathogenetic treatment in the hypoplastic macrotype. This approach increases pregnancy rates by 1.5 times in cases of thin endometrium, by 1.8 times in cases of mixed macrotype, and by 1.3 times in cases of hyperplasia.
Authors' contributions: Ozerskaya I.A. – conception and design of the study, editing of the manuscript; Porkhovaty S.Ya., Kazaryan G.G. – collection and processing of materials; Ozhogina E.V. – statistical analysis; Kazaryan G.G., Ozhogina E.V. – drafting of the manuscript.
Conflicts of interest: The authors have no conflicts of interest to declare.
Funding: There was no funding for this study.
Ethical Approval: The study was reviewed and approved by the Research Ethics Committee of the Peoples' Friendship University of Russia.
Patient Consent for Publication: All patients provided informed consent for the publication of their data.
Authors' Data Sharing Statement: The data supporting the findings of this study are available upon request from the corresponding author after approval from the principal investigator.
For citation: Ozerskaya I.A., Porkhovaty S.Ya., Kazaryan G.G., Ozhogina E.V. The effect of cytokine therapy on uterine-endometrial blood flow and reproductive function in various morphological types of chronic endometritis.
Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2025; (6): 114-123 (in Russian)
https://dx.doi.org/10.18565/aig.2025.58
Keywords
Chronic endometritis (CE) is prevalent among women experiencing infertility and miscarriage, with histological and morphological signs detected in 86.7% and 70.2% of cases, respectively [1]. Various classifications of chronic endometritis have been reported previously. These include classifications based on etiological factors (non-specific and specific) as well as atrophic, cystic, and hypertrophic types [2]; hypoplastic (both focal and diffuse forms), those without signs of hyper- and hypoplasia, and hyperplastic types [3]; and classifications by morphohistological type – hypoplastic, mixed, and hyperplastic [4, 5]. The hypoplastic macrotype is characterized by dystrophic-atrophic changes in the endometrium, whereas the mixed macrotype features alternating areas of dystrophy and fibrosis, often accompanied by hyperplastic polypoid growths, all of which exhibit lymphocytic infiltration of the uterine mucosa [6, 7]. The ultrasound features of various morphological types of chronic endometritis, along with changes following standard anti-inflammatory treatment, have been detailed in domestic literature [8–10]. These findings suggest that while complete restoration of the mucosal structure is not achieved, there is a reduction in the frequency of pathological signs. Specifically, the volume of endometrial tissue increases with the hypoplastic morphotype and decreases with the hyperplastic morphotype. In addition to antibacterial, antiviral, and antimycotic medications, local cytokine therapy is employed to alleviate inflammatory manifestations and aid in endometrial restoration [11]. Recent scientific studies have demonstrated that such treatments among women suffering from chronic endometritis, infertility, and miscarriage lead to a decrease in inflammation related to the autoimmune component, normalization of pro- and anti-inflammatory cytokines and immunoglobulins in the endometrium [12–20]. Research indicates an improved sensitivity to anti-inflammatory therapy, reduction in treatment duration, and restoration of reproductive function.
Dobrokhotova Yu.E. et al. assessed the intensity of angiogenesis by studying VEGF-A, VEGFR-1 and -2, and CD34 before and after cytokine therapy for chronic endometritis [16]. The authors reported a significant enhancement in tissue blood supply at the microvascular level, which not only increased the frequency of pregnancies, but also the rate of live births.
By contrast, some data suggest otherwise. For instance, the inclusion of the drug "Superlymph" in the complex therapy for chronic endometritis resulted in decreased vascularization of the uterine mucosa, as detected at the macrovascular level through ultrasound scanning [21]. Using volumetric blood flow indices that reflect arteriovenous blood supply and assessments of arterial blood flow based on hemodynamic parameters of the uterine arteries, the authors indicated that this reduction in vascularization correlates with the restoration of venous outflow in the uterus and endometrium. However, no studies have been identified that examined blood flow in the uterus, including the endometrium, during treatment with cytokine drugs in women with various morphological types of chronic endometritis.
This study aimed to evaluate the impact of cytokine therapy on uteroendometrial blood flow across different morphological types of chronic endometritis.
Materials and methods
This prospective pilot study included 298 women of reproductive age with clinically and morphologically verified diagnoses of chronic endometritis. Before prescribing etiological treatment, the following hysteroscopic macrotypes of chronic endometritis were identified: hypoplastic, hyperplastic, and mixed. These were identified according to the classification proposed by Radzinsky V.E. et al. (2017) [4, 6, 7]. According to the hysteroscopic description, the results of the ultrasound examination indicated that the hypoplastic macrotype corresponded to a corrected endometrial volume of less than 5%, the mixed type corresponded to a corrected endometrial volume of 5–10%, and the hyperplastic type corresponded to a corrected endometrial volume of greater than 10% [9].
The study group consisted of 140 patients, of whom 51 had a hypoplastic macrotype, 36 had a mixed macrotype, and 53 had a hyperplastic macrotype. These women received anti-inflammatory therapy, including combinations of antibiotics such as the latest generation macrolides + nitroimidazole, macrolides + third-generation cephalosporins, and protected penicillins and macrolides. The therapy was supplemented with antifungal, antiviral, and immunomodulatory drugs (interferons, hyperimmune and polyspecific immunoglobulins, abnormal nucleotides). As concomitant flora were identified, antiprotozoal, antimicrobial agents, and antiseptics were prescribed. Additionally, this group received cytokine therapy in the form of a single course of the drug "Superlymph" 25 U in 1 suppository vaginally at night, lasting 20 days.
The control group comprised 158 women who received anti-inflammatory treatment according to the same scheme but without the use of exogenous cytokines. In this group, 30, 71, and 57 patients had hypoplastic, mixed, and 57 with a hyperplastic macrotype, respectively. When prescribing therapy, clinicians were guided by the standards of medical care and drugs registered in the Russian Federation, and current instructions for medical use were published in the Register of Medicines (https://www.rlsnet.ru/).
The study did not include women with concomitant pathologies, such as endometriosis, uterine fibroids, uterine malformations, and pathology of the tubes and/or ovaries.
The study was reviewed and approved by the Research Ethics Committee of the Patrice Lumumba Peoples' Friendship University of Russia.
All patients provided informed consent for the publication of their data.
The clinical diagnosis of endometritis was based on medical history, symptoms, and bimanual examinations. Morphological diagnostics were based on the results of cytological and histological studies of the endometrium after hysteroscopy, and morphological and immunohistochemical analyses of endometrial tissue obtained during a pipelle biopsy. Plasma cells (CD138) and/or monoclonal antibodies against immune cell antigens (CD4, CD8, and CD20) were also detected.
Pelvic ultrasound examination was performed using a volumetric intracavitary sensor with subsequent reconstruction in 3D mode via transvaginal access using the Affiniti70 device (Philips, Netherlands). The study was conducted one month after the treatment ended during the early proliferative phase. The following parameters were considered: uterine body volume, endometrial thickness, and corrected endometrial volume.
To quantitatively assess the degree of uterine and endometrial vascularization, the QLab application program was used, operating in the angio mode with 3D reconstruction to obtain the vascularization index (VI), flow index (FI), and vascularization-flow index (VFI). During pulsed wave Doppler sonography of the uterine arteries (UA), the following parameters were studied: maximum blood flow velocity (Vmax), end-diastolic velocity (Vmin), average velocity (Vmean), pulsatility index (PI), and resistance index (RI), and the UA diameter was measured.
The arterial perfusion index (API) was then determined, which reflects the perfusion of 1 cm3 of the uterine body with blood flowing through both UAs, expressed as a percentage. For this purpose, the volumetric blood flow (cm3 per cardiac cycle) in each UAs was calculated using the following formula:
Vvol = Vmean × S, where S is the area of the uterine artery (cm2).
API was calculated using the following formula:
API (%) = (VvolUAright + VvolUAleft)/Vuterus × 100, where VvolUAright – the volumetric blood flow through the right UA (cm3); VvolUAleft – volumetric blood flow in the left MA (cm3); Vuterus – uterine volume (cm3).
The impact of the therapy was assessed by complex changes in uterine hemodynamic parameters, including the endometrium, as well as by the pregnancy rate in each group, taking into account the chronic endometritis macrotype within 6 months after the end of the treatment course. Pregnancy was visualized as a fertilized egg with a live embryo in the uterine cavity during ultrasound examination for at least 6 weeks. During the 6-month observation period, 16/298 (5.4%) women abandoned their reproductive plans for family reasons, or contact with them was lost due to a change in residence. Among them, 11 (7.9%) were in the study group and 5 (3.2%) were in the control group.
Statistical analysis
Statistical analyses were performed using SPSS v. 27.0 (IBM, USA) software. The normality of the distribution of continuous variables was tested using the Shapiro–Wilk test. As most of the data did not follow a normal distribution, all results are presented as the median (Me) with interquartile ranges (Q1; Q3). Categorical variables were presented as counts (n) and percentages (%). The comparison of groups by categorical variables was performed by analyzing contingency tables using the Pearson chi-square test with Yates' correction. Two independent groups were compared using the Mann–Whitney U test with a critical significance level of p<0.05. The nonparametric Kruskal–Wallis test was used for the three independent groups. If the p-value was less than 0.05, paired comparisons of the groups were performed with a correction for multiple comparisons. The critical significance level for this correction was set at p<0.017. The relationship between the treatment factor and outcome was assessed using the relative risk (RR) with a 95% confidence interval (CI).
Results
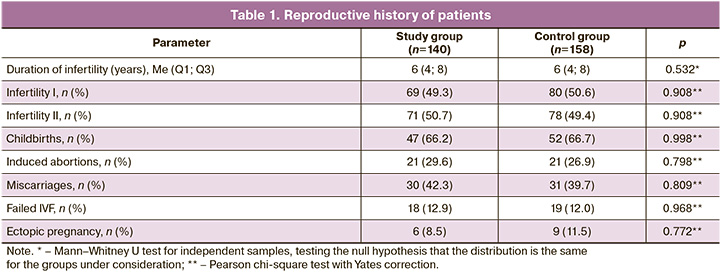
The median age of the patients in the study group was 34 (29–44) years and 33 (26–42) years in the control group (p>0.05). The duration of infertility ranged from 2 to 12 years in the study group and from 1 to 13 years in the control group. No statistically significant differences were found between the groups in terms of the reproductive history (Table 1).
Analysis of the blood flow indicators of the right and left UA levels did not reveal any asymmetry in the digital values (p>0.05); therefore, the average values of each indicator were used. Among women with hypoplastic macrotype CE, cytokine therapy had no significant effect on the hemodynamics of the uterus and endometrium, with the exception of the uterine and PI of the uterine arteries (Table 2).
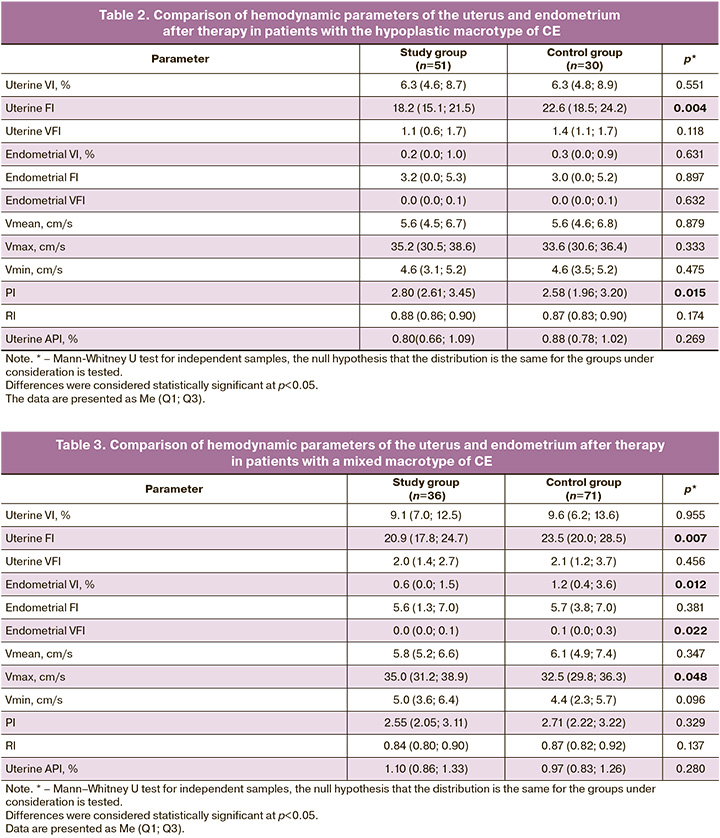
Among patients with mixed macrotype CE, cytokine therapy led to lower endometrial vascularization parameters (VI and VFI) (p<0.05). Additionally, this group exhibited an increased maximum blood flow velocity in the UA compared with patients receiving standard anti-inflammatory treatment; however, the uterine flow index (FI) was lower than that of the control group (Table 3).
The same trend was observed among women with the hyperplastic macrotype of CE: a significant decrease in endometrial vascularization (VI) and lower FI values in the uterus with the addition of cytokines to the treatment complex than in the control group (Table 4).
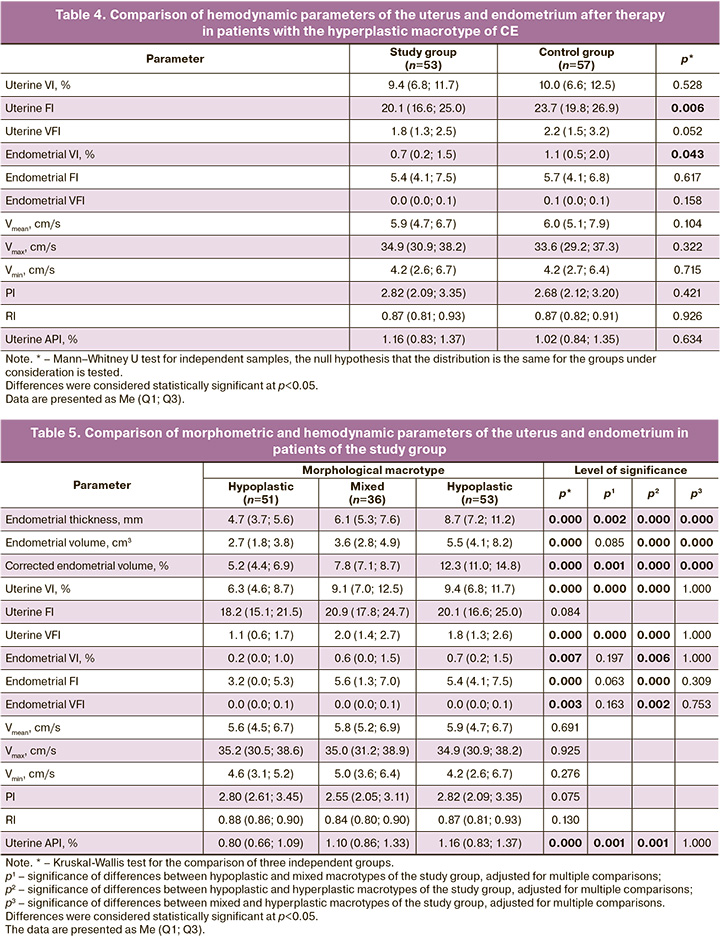
Hemodynamic parameters of the uterus and endometrium depended on the macrotype of CE. In the study group, differences were observed in the degree of vascularization and morphometric parameters of the endometrium. Thus, the values of VI, FI, and VFI of the uterus and endometrium, as well as API, were significantly higher in the presence of a hyperplastic macrotype than in a hypoplastic macrotype.
Comparison of mixed and hypoplastic macrotypes indicated the significance of differences in VI, VFI of the uterus, and API. At the same time, none of the parameters of volumetric blood flow of the uterus and endometrium (VI, FI, and VFI), including API of the uterus, in patients with mixed and hyperplastic macrotypes showed significant differences. There were also no significant differences among all parameters of blood flow UA among women with different macrotypes (Table 5).
Within six months after the end of treatment, clinical pregnancy occurred in 38.8% of patients in the study group and 27.5% in the control group (RR=1.412; 95%CI1.008–1.997). Cytokine therapy increased the pregnancy rate in patients with all types of CE: hypoplastic (26.1% vs. 17.9%), mixed (41.2% vs. 23.2%), and hyperplastic (38.8% vs. 27.5%) (Table 6).

In the study group, clinical pregnancy was recorded 1.9 times more often in women with the hyperplastic macrotype of CE than in those with the hypoplastic macrotype (RR=1.878; 95% CI 1.068–3.301).
It was also recorded 1.2 times more often in women with the hyperplastic macrotype than in those with the mixed macrotype (RR=1.190; 95% CI 0.727–1.948). Finally, it was recorded 1.6 times more often in women with the hyperplastic macrotype than in women with the hypoplastic macrotype (RR = 1.578; 95% CI 0.840–2.966).
Discussion
This study aimed to evaluate the effect of cytokine therapy on the hemodynamics of the uterus, including endometrium and reproductive function, across various macrotypes of chronic endometritis. The results indicate that cytokines reduce the blood supply to the endometrium in cases of hyperplastic and mixed morphological types (p<0.05), while vascularization of the hypoplastic endometrium remained virtually unchanged. This effect is likely associated with the relief of microcirculation disorders in lesions, as evidenced by vascular dilation and congestion in the blood and lymph circulation [22]. Hysteroscopy findings reveal that the most common signs of chronic endometritis are venous congestion and edema [23, 24]. These changes are characteristic of hyperplastic and mixed macrotypes, whereas the hypoplastic type is characterized by fibrosis and vascular sclerosis leading to endometrial ischemia [4, 25].
Borisevich O.O. and Shatilina A.Yu. investigated the arterial blood flow of the uterus at the MA level to evaluate the effect of rehabilitation on women with infertility and miscarriage due to chronic endometritis. The authors reported a significant increase in the API of the uterus and a subjective increase in vascularization with complex treatment, including electropulse and manual therapy, as well as sodium chloride baths [26]. However, our study does not support this conclusion; the increase in API was not associated with treatment, but rather with the macrotype of chronic endometritis. The absence of an effect of treatment on blood flow in the UA and API in both the study and control groups confirmed normalization of the venous link. Notably, the API of the uterus in the study group showed significant differences not only between the hypo- and hyperplastic macrotypes but also between the hypoplastic and mixed types; in contrast, the control group exhibited a difference in the endometrium only between the hypo- and hyperplastic types. Cytokines have antiviral, antimicrobial, and antifungal effects, which reduce the development of inflammatory reactions and stimulate regeneration [11]. In hyperplastic macrotypes, venous stasis processes appear to be more pronounced and are alleviated by cytokine therapy, leading to a significant decrease in the VI of the endometrium compared to that in the control group. In hypoplastic macrotypes, however, venous outflow disturbances are absent, as dysplastic processes characterized by non-functioning glands and unevenly dense stroma with areas of fibrosis predominate [27]. Consequently, the effect of exogenous cytokines on the hemodynamics of the "thin" endometrium is not pronounced. Researchers suggest that endometrial hypoplasia results from chronic endometritis [28], which can persist for more than two years and is often accompanied by a history of inflammatory diseases of the pelvic organs [27]. As the duration of infertility in women with chronic endometritis increases, the blood supply to the uterus and endometrium diminishes [29], making restoration with medications particularly challenging in the hypoplastic macrotype, as indicated by the study results. Currently, there is no standardization in the diagnosis and treatment of chronic endometritis in our country or abroad. The clinical guidelines on " inflammatory diseases of the female pelvic organs," approved by the Ministry of Health of the Russian Federation in 2024, state that the effectiveness of therapy is evaluated based on histological analysis of an endometrial biopsy [30]. The European Society of Human Reproduction and Embryology (ESHRE) has noted the role of chronic endometritis in the failure of infertility treatments using assisted reproductive technology (ART) [31]. These recommendations indicate that there are currently no studies assessing the value of 3D ultrasound in treating patients with implantation disorders. However, given its low cost and non-invasiveness, it is advisable to use this diagnostic method both before planning IVF and when evaluating treatment.
In Japan, an analysis of the diagnostic methods and treatment monitoring for chronic endometritis was conducted across 339 ART clinics [32]. The researchers found significant variability in diagnostic and treatment approaches, both between institutions and among clinicians within the same clinic, underscoring the necessity of establishing uniform diagnostic criteria and treatment protocols for chronic endometritis.
Among clinicians, the primary criterion for treatment effectiveness is the occurrence and progression of pregnancy. The use of immunomodulatory drugs increases the likelihood of implantation by 1.5–2.5 times [18, 19, 33–37]. In our study, pregnancy was registered 1.4 times more frequently among patients in the study group than among in those the control group (p<0.05). A more pronounced effect was observed in patients with a mixed macrotype of chronic endometritis (1.8 times), while the hypoplastic type showed a 1.5 times increase, and the hyperplastic type a 1.3 times increase. It is likely that the impact of cytokine therapy on endometrial hemodynamics, and consequently, the potential for implantation, is linked to the duration of drug administration. Scientific studies have included a 20-day course of Superlymph with a repeat after 1–1.5 months [38], the administration of two courses with a three-week interval [17], three consecutive cycles starting from the 5th day [15, 39], and a 40-day course [40]. A single 20-day course of cytokine therapy may be insufficient to fully relieve venous outflow disturbances in the endometrium of the hyperplastic macrotype, which is one of the pathogenetic factors of the inflammatory process, as indicated by the study results. Changes in the blood supply to the uterus and endometrium during the treatment of chronic endometritis with various medications, including differing treatment durations and frequencies, require further investigation.
Conclusion
The use of exogenous cytokines in combination with anti-inflammatory therapy restores venous outflow in the endometrium in mixed and hyperplastic macrotypes of chronic endometritis. This approach enhances the effectiveness of pathogenetic treatment in the hypoplastic macrotype, increasing the frequency of pregnancy by 1.5 times in cases of a “thin” endometrium, by 1.8 times in cases of a mixed macrotype, and by 1.3 times in cases of a hyperplastic macrotype.
References
- Зароченцева Н.В., Аршакян А.К., Меньшикова Н.С., Титченко Ю.П. Хронический эндометрит: этиология, клиника, диагностика, лечение. Российский вестник акушера-гинеколога. 2013; 13(5): 21-7. [Zarochentseva N.V., Arshakian A.K., Men’shikova N.S., Titchenko Iu.P. Chronic endometritis: etiology, clinical features, diagnosis, treatment. Russian Bulletin of Obstetrician-Gynecologist. 2013; 13(5): 21-7 (in Russian)].
- Кулаков В.И., Манухин И.Б., Савельева Г.М., ред. Гинекология: национальное руководство. М.: ГЭОТАР-Медиа; 2007. 1072 с. [Kulakov V.I., Manukhin I.B., Savelyeva G.M., eds. Gynecology: National Guide. Moscow: GEOTAR-Media; 2007. 1072 p. (in Russian)].
- Сухих Г.Т., Шуршалина А.В. Хронический эндометрит: руководство. М: ГЭОТАР-Медиа; 2013. 64 с. [Sukhikh G.T., Shurshalina A.V., eds. Chronic endometritis: a guide. Moscow: GEOTAR-Media; 2013. 64 p. (in Russian)].
- Радзинский В.Е., Петров Ю.А., Калинина Е.А., Широкова Д.В., Полина М.Л. Патогенетические особенности макротипов хронического эндометрита. Казанский медицинский журнал. 2017; 98(1): 27-34. [Radzinsky V.E., Petrov Yu.A., Kalinina E.A., Shirokova D.V., Polina M.L. Pathogenetic features of macrotypes of chronic endometritis. Kazan Medical Journal. 2017; 98(1): 27-34. (in Russian)]. https://dx.doi.org/10.17750/KMJ2017-27
- Шелемех К.Е., Петров Ю.А., Купина А.Д. «Золотой стандарт» диагностики хронического воспаления эндометрия. Главный врач Юга России. 2020; 1(71): 27-30. [Shelemeh K.E., Petrov Yu.A., Kupina A.D. “Gold standard” for diagnosing chronic inflammation of the endometrium. Chief physician of the South of Russia. 2020; 1(71): 27-30. (in Russian)].
- Радзинский В.Е., Петров Ю.А., Полина М.Л. Хронический эндометрит: современные аспекты. Кубанский научный медицинский вестник. 2017; 5: 69-74. [Radzinsky V.E., Petrov Yu.A., Polina M.L. Chronic endometritis: modern aspects. Kuban Scientific Medical Bulletin. 2017; 5: 69-74. (in Russian)]. https://dx.doi.org/10.25207/1608-6228-2017-24-5-69-74
- Radzinsky V.E., Kostin I.N., Petrov Yu.A., Polina M.L., Gasanova B.M. Diagnostic significance of chronic endometritis macrotypes differentiation among women with reproductive losses. Gynecol. Endocrinol. 2017; 33(sup. 1): 36-40. https://dx.doi.org/10.1080/09513590.2017.1399697
- Озерская И.А., Казарян Г.Г., Гус А.И. Влияние лечения на ультразвуковые параметры эндометрия у женщин репродуктивного возраста с хроническим эндометритом. Ультразвуковая и функциональная диагностика. 2023; (4): 96-115. [Ozerskaya I.A., Kazaryan G.G., Gus A.I. The impact of treatment on endometrium ultrasound findings in reproductive age women with chronic endometritis. Ultrasound & Functional Diagnostics. 2023; (4): 96-115. (in Russian)]. https://dx.doi.org/10.24835/1607-0771-2023-4-96-115
- Озерская И.А., Казарян Г.Г., Гус А.И. Изменение ультразвуковых параметров на фоне лечения хронического эндометрита в зависимости от морфологического типа у женщин репродуктивного возраста. Ультразвуковая и функциональная диагностика. 2024; (2): 72-90. [Ozerskaya I.A., Kazaryan G.G., Gus A.I. The changes in ultrasound parameters during treatment of chronic endometritis depending on the morphological type in women of reproductive age. Ultrasound & Functional Diagnostics. 2024; (2): 72-90. (in Russian)]. https://dx.doi.org/10.24835/1607-0771-084
- Озерская И.А., Порховатый С.Я., Казарян Г.Г., Ожогина Е.В. Изменения гемодинамики матки после лечения хронического эндометрита. Медицинская визуализация. 2024; 28(4): 100-11. [Ozerskaya I.A., Porkhovaty S.Ya., Kazaryan G.G., Ozhogina E.V. Changes in uterine hemodynamics after treatment of chronic endometritis. Medical Visualization. 2024; 28(4): 100-11. (in Russian)]. https://dx.doi.org/10.24835/1607-0763-1485
- Справочник лекарственных средств «Видаль». Описание препарата «Суперлимф». Доступно по: https://www.vidal.ru/drugs/superlymph__30595 [VIDAL. Description of the drug Superlymph. Available at: https://www.vidal.ru/drugs/superlymph__30595 (in Russian)].
- Лысенко О.В., Рождественская Т.А. Проблема «тонкого» эндометрия в репродуктивной медицине: опыт применения рекомбинантного интерлейкина-2 человека для подготовки пациенток к программам вспомогательных репродуктивных технологий. Журнал акушерства и женских болезней. 2017; 66(4): 46-50. [Lysenko O.V., Rozhdestvenskaya Т.А. The problem of "thin" endometrium in reproductive medicine: experience of application of recombinant interleukin-2 to prepare patients to assisted reproductive technologies programs. Journal of Obstetrics and Women’s Diseases. 2017; 66(4): 46-50. (in Russian)]. https://dx.doi.org/10.17816/JOWD66446-50
- Дикке Г.Б., Остроменский В.В. Нарушение иммунного статуса при хроническом эндометрите и опыт его коррекции посредством локальной цитокинотерапии. Акушерство и гинекология. 2019; 9: 139-46. [Dikke G.B., Ostromensky V.V. Immune dysfunction in chronic endometritis and the experience of its correction using local cytokine therapy. Obstetrics and Gynecology. 2019; (9): 139-46 (in Russian)]. https://dx.doi.org/10.18565/aig.2019.9.139-146
- Оразов М.Р., Михалева Л.М., Семенов П.А., Орехов Р.Е., Лагутина Е.В. Эффективность лечения хронического эндометрита у женщин с неудачами имплантации в анамнезе. Трудный пациент. 2020; 18(8-9): 7-12. [Orazov M.R., Mikhaleva L.M., Semenov P.A., Orekhov R.E., Lagutina E.V. The effectiveness of treatment of chronic endometritis in women with a history of implantation failure. Difficult patient. 2020; 18(8-9): 7-12 (in Russian)]. https://dx.doi.org/10.24411/2074-1995-2020-10053
- Радзинский В.Е., Оразов М.Р., Токтар Л.Р. Михалева Л.М., Семенов П.А., Орехов Р.Е. Лагутина Е.В., Силантьева Е.С. Эффект «разбросанных пазлов»: имплантационные нарушения при хроническом эндометрите. Гинекология. 2020; 22(6): 24-31. [Radzinsky V.E., Orazov M.R., Toktar L.R. Mikhaleva L.M., Semenov P.A., Orekhov R.E. Lagutina E.V., Silanteva E.S. The effect of “scattered puzzles”: implantation disorders in chronic endometritis. Gynecology. 2020; 22(6): 24-31 (in Russian)]. https://dx.doi.org/10.26442/20795696.2020.6.200493
- Доброхотова Ю.Э., Боровкова Е.И., Нугуманова О.Р. Улучшение процессов ангиогенеза и репродуктивных исходов у пациенток с хроническим эндометритом. Акушерство и гинекология. 2021; 3: 145-52. [Dobrokhotova Yu.E., Borovkova E.I., Nugumanova O.R. Improvement of angiogenesis and reproductive outcomes in patients with chronic endometritis. Obstetrics and Gynecology. 2021; (3): 145-52 (in Russian)]. https://dx.doi.org/10.18565/aig.2021.3.145-152
- Тапильская Н.И., Толибова Г.Х., Савичева А.М., Копылова А.А., Глушаков Р.И., Будиловская О.В., Крысанова А.A., Горский А.Г., Гзгзян А.М., Коган И.Ю. Эффективность локальной цитокинотерапии хронического эндометрита пациенток с бесплодием. Акушерство и гинекология. 2022; 2: 91-100. [Tapilskaya N.I., Tolibova G.Kh., Savicheva A.M., Kopylova A.A., Glushakov R.I., Budilovskaya O.V.,
- Krysanova A.A., Gorskii A.G., Gzgzyan A.M., Kogan I.Yu. The effectiveness of local cytokine therapy for chronic endometritis in patients with infertility. Obstetrics and Gynecology. 2022; (2): 91-100 (in Russian)]. https://dx.doi.org/10.18565/aig.2022.2.91-100
- Дикке Г.Б., Суханов А.А., Остроменский В.В., Кукарская И.И. Течение и исходы беременности у пациенток с хроническим эндометритом и нарушением репродуктивной функции, получавших комплексное лечение с использованием препарата «Суперлимф» (рандомизированное контролируемое испытание в параллельных группах «ТЮЛЬПАН»). Акушерство и гинекология. 2023; 4: 132-44. [Dikke G.B., Sukhanov A.A., Ostromensky V.V., Kukarskaya I.I. Course and outcomes of pregnancy in patients with chronic endometritis and impaired reproductive function after receiving complex treatment with drug Superlymph: randomized control trial in parallel groups “TULIP”. Obstetrics and Gynecology. 2023; (4): 132-44 (in Russian)]. https://dx.doi.org/10.18565/aig.2023.74
- Боровиков И.О., Булгакова В.П., Боровикова О.И., Никогда Ю.В., Бирюкова М.И. Подготовка к проведению экстракорпорального оплодотворения пациенток с «тонким» эндометрием – возможности цитокинотерапии. Проблемы репродукции. 2023; 29(3): 31-9. [Borovikov I.O., Bulgakova V.P., Borovikova O.I., Nikogda Y.V., Biryukova M.I. Preparation for in vitro fertilization of patients with a «thin» endometrium – the possibilities of cytokine therapy. Russian Journal of Human Reproduction. 2023; 29(3): 31-9 (in Russian)]. https://dx.doi.org/10.17116/repro20232903131
- Суханов А.А., Дикке Г.Б., Кукарская И.И. Эпидемиология женского бесплодия и опыт восстановления репродуктивной функции у пациенток с хроническим эндометритом в Тюменском регионе. Проблемы репродукции. 2023; 29(3): 98-107. [Sukhanov A.A., Dikke G.B., Kukarskaya I.I. Epidemiology of female infertility and the experience of recovery of reproductive function in patients with chronic endometritis in the Tyumen region. Russian Journal of Human Reproduction. 2023; 29(3): 98-107 (in Russian)]. https://dx.doi.org/10.17116/repro2023290319812-18
- Озерская И.А., Порховатый С.Я., Казарян Г.Г., Ожогина Е.В. Влияние цитокинотерапии на гемодинамику матки при лечении хронического эндометрита. Акушерство и гинекология. 2024; 11: 128-36. [Ozerskaya I.A., Porkhovatyi S.Ya., Kazaryan G.G., Ozhogina E.V. The influence of cytokine therapy on ultrasound assessment of uterine hemodynamics in treatment of chronic endometritis. Obstetrics and Gynecology. 2024; (11): 128-36 (in Russian)]. https://dx.doi.org/10.18565/aig.2024.176
- Шанин В.Ю. Воспаление. В кн.: Шевченко Ю.Л., ред. Клиническая патофизиологияю С.-Пб: Специальная литература; 1998: 170-97. [Shanin V.Yu. Inflammation. In: Shevchenko Yu.L., ed. Clinical pathophysiology. St. Petersburg: Special literature; 1998: 170-97 (in Russian)].
- Furui M., Ito A., Fukuda Y., Sekiguchi M., Nakaoka K., Hayashi Y. et al. Endometrial congestion is the only hysteroscopic finding indicative of chronic endometritis. PLoS One. 2024; 19(6): e0303041. https://dx.doi.org/10.1371/journal.pone.0303041
- Mitter V.R., Meier S., Rau T.T., Gillon T., Mueller M.D., Zwahlen M. et al. Treatment following hysteroscopy and endometrial diagnostic biopsy increases the chance for live birth in women with chronic endometritis. Am. J. Reprod. Immunol. 2021; 86(5): e13482. https://dx.doi.org/10.1111/aji.13482
- Шуршалина А.В. Подготовка эндометрия к беременности и программам вспомогательных репродуктивных технологий. Consilium medicum (женское здоровье). 2012; 14(6): 63-6. [Shurshalina A.V. Preparation of the endometrium for pregnancy and assisted reproductive technology programs. Consilium medicum (women's health). 2012; 14(6): 63-6. (in Russian)].
- Борисевич О.О., Шатилина А.Ю. Клиническая роль мануальной и электроимпульсной терапии в улучшении прегравидарной подготовки у пациенток с тонким эндометрием. Реабилитология. 2024; 2(3): 269-76. [Borisevich О.О., Shatilina A.Yu. Clinical role of manual and electropulse therapy in improving preconception care in patients with thin endometrium. Journal of Medical Rehabilitation. 2024; 2(3): 269-76. (in Russian)]. https://dx.doi.org/10.17749/2949-5873/rehabil.2024.24.
- Толибова Г.Х., Траль Т.Г., Коган И.Ю. Морфологические варианты «тонкого» (гипопластичного) эндометрия. В кн.: Коган И.Ю., ред. Эндометрий в репродукции: оценка функции и возможности коррекции: руководство для врачей. М.: ГЭОТАР-Медиа; 2023: 249-54. [Tolibova G.Kh., Tral T.G., Kogan I.Yu. Morphological variants of "thin" (hypoplastic) endometrium. In: Kogan I.Yu., ed. Endometrium in reproduction: assessment of function and possibilities of correction: a guide for doctors. Moscow: GEOTAR-Media; 2023: 249-54. (in Russian)]. https://dx.doi.org/10.33029/9704-6608-7-END-2022-1-480
- Кулавский В.А., Мехдиева Ю.Д., Кулавский Е.В., Фролов А.Л. Современный взгляд на лечение хронического эндометрита. Медицинский вестник Башкортостана. 2015; 10(4): 96-101. [Kulavsky V.А., Mekhdieva Y.D., Kulavsky E.V., Frolov A.L. Current view on chronic endometritis treatment. Medical Bulletin of Bashkortostan. 2015; 10(4): 96-101. (in Russian)].
- Озерская И.А., Иванов В.А., Порховатый С.Я., Казарян Г.Г. Особенности кровоснабжения матки у женщин с хроническим эндометритом в зависимости от длительности бесплодия. Акушерство и гинекология. 2020; 10: 105-12. [Ozerskaya I.A., Ivanov V.A., Porkhovaty S.Ya., Kazaryan G.G. Characteristics of uterine blood supply in women with chronic endometritis depending on the duration of infertility. Obstetrics and Gynecology. 2020; (10): 105-12 (in Russian)]. https://dx.doi.org/10.18565/aig.2020.10.105-112
- Министерство здравоохранения Российской Федерации. Клинические рекомендации. Воспалительные болезни женских тазовых органов. M.; 2024. 49с. [Ministry of Health of the Russian Federation. Clinical guidelines. Inflammatory diseases of female pelvic organs. Moscow; 2024. 49p. (in Russian)].
- ESHRE Working Group on Recurrent Implantation Failure; Cimadomo D., de Los Santos M.J., Griesinger G., Lainas G., Le Clef N., McLernon D.J. et al. ESHRE good practice recommendations on recurrent implantation failure. Hum. Reprod. Open. 2023; 2023(3): hoad023. https://dx.doi.org/10.1093/hropen/hoad023
- Jwa S.C., Kuroda K., Shirasawa H., Harada M., Osuga Y., Yamada M. Variation in diagnostic methods, criteria, and treatment for chronic endometritis: A nationwide survey in Japan. J. Obstet. Gynaecol. Res. 2024; 50(9): 1479-84. https://dx.doi.org/10.1111/jog.16051
- Кореева Н.В., Доброхотова Ю.Э. Локальная цитокинотерапия в гинекологической практике (обзор литературы). Проблемы репродукции. 2013; 4: 21-6. [Koreeva N.V., Dobrokhotova Iu.É. Topical cytokinotherapy in gynecological practice (a review). Russian Journal of Human Reproduction. 2013; (4): 21-6. (in Russian)].
- Wu Y., Li L., Liu L., Yang X., Yan P., Yang K., Zhang X. Autologous peripheral blood mononuclear cells intrauterine instillation to improve pregnancy outcomes after recurrent implantation failure: a systematic review and meta-analysis. Arch. Gynecol. Obstet. 2019; 300(5): 1445-9. https://dx.doi.org/10.1007/s00404-019-05275-w
- Maleki-Hajiagha A., Razavi M., Rezaeinejad M., Rouholamin S., Almasi-Hashiani A., Pirjani R. et al. Intrauterine administration of autologous peripheral blood mononuclear cells in patients with recurrent implantation failure: A systematic review and meta-analysis. J. Reprod. Immunol. 2019; 131: 50-6. https://dx.doi.org/10.1016/j.jri.2019.01.001
- Melo P., Thornton T., Coomarasamy A., Granne I. Evidence for the effectiveness of immunologic therapies in women with subfertility and/or undergoing assisted reproduction. Fertil. Steril. 2022; 117(6): 1144-59. https://dx.doi.org/10.1016/j.fertnstert.2022.04.015
- Liu M., Yuan Y., Qiao Y., Tang Y., Sui X., Yin P. et al. The effectiveness of immunomodulatory therapies for patients with repeated implantation failure: a systematic review and network meta-analysis. Sci. Rep. 2022; 12(1):18434. https://dx.doi.org/10.1038/s41598-022-21014-9
- Суханов А.А., Дикке Г.Б., Кукарская И.И. Влияние иммуномодулирующей терапии на репродуктивную функцию у пациенток с бесплодием, обусловленным хроническим эндометритом. Акушерство и гинекология. 2024; 8: 141-52. [Sukhanov A.A., Dikke G.B., Kukarskaya I.I. Influence of immunomodulatory therapy on reproductive function in female patients with infertility caused by chronic endometritis. Obstetrics and Gynecology. 2024; (8): 141-52 (in Russian)]. https://dx.doi.org/10.18565/aig.2024.204
- Толибова Г.Х., Траль Т.Г., Кахиани М.И. Возможности коррекции рецепторного профиля эндометрия при хроническом эндометрите. Акушерство и гинекология. 2024; 10: 121-8. [Tolibova G.Kh., Tral T.G., Kakhiani M.I. Possibilities of correction of the endometrial receptor profile in chronic endometritis. Obstetrics and Gynecology. 2024; (10): 121-8 (in Russian)]. https://dx.doi.org/10.18565/aig.2024.244
- Доброхотова Ю.Э., Ганковская Л.В., Боровкова Е.И., Нугуманова О.Р. Экзогенная цитокинотерапия в лечении пациенток с хроническим эндометритом. Акушерство и гинекология. 2021; 2: 119-26. [Dobrokhotova Yu.E., Gankovskaya L.V., Borovkova E.I., Nugumanova O.R. Exogenous cytokine therapy in the treatment of patients with chronic endometritis. Obstetrics and Gynecology. 2021; (2): 119-26 (in Russian)]. https://dx.doi.org/10.18565/aig.2021.2.119-126
Received 04.03.2025
Accepted 21.05.2025
About the Authors
Irina A. Ozerskaya, Dr. Med. Sci., Professor at the Department of Ultrasound Diagnostics of Continuous Medical Education of the Medical Institute, Patrice Lumumba Peoples’ Friendship University of Russia, 117198, Russia, Moscow, Miklukho-Maklaya str., 6, +7(499)936-87-87, ozerskaya_usd@mail.ru, https://orcid.org/0000-0001-8929-6001Sergey Ya. Porkhovaty, PhD, ultrasound diagnostics doctor, Asklepion Medical Center, 125222, Russia, Moscow, Dubravnaya str., 41, bldg. 2, +7(495)759-99-50,
oracul2003@gmail.com, https://orcid.org/0009-0002-7263-1568
Gayane G. Kazaryan, PhD, Head of the Ultrasound Diagnostics Department, Medscan Medical Center, 119421, Russia, Moscow, Obrucheva str., 21A, +7(495)859-29-45, 79165521271@yandex.ru, https://orcid.org/0000-0002-1198-8187
Ekaterina V. Ozhogina, PhD, Leading Reproductive Specialist, Nova Clinic Center for Reproduction and Genetics, 119415, Russia, Moscow, Lobachevsky str., 20,
+7(495)476-61-19, ozhogina.caterina@yandex.ru, https://orcid.org/0009-0007-5205-2901
Corresponding author: Irina A. Ozerskaya, ozerskaya_usd@mail.ru



