Pregnancy management tactics in reversed arterial perfusion syndrome
Objective. To compare the efficiency of surgical and medical management tactics for RAPS-complicated pregnancy.Kostyukov K.V., Gladkova K.A., Tetruashvili N.K.
Subjects and methods. Perinatal outcomes were retrospectively analyzed in 47 patients with multiple pregnancy complicated by RAPS who had been examined and treated at the Academician V.I. Kulakov National Medical Research Center of Obstetrics, Gynecology, and Perinatology, Ministry of Health of Russia, in 2010 to 2017. According to the proposed pregnancy management tactics, the patients were divided into two groups: 1) 17 patients who had undergone medical pregnancy management; 2) 28 pregnant women who had intrauterine treatment. According to the type of an operation performed, Group 2 was divided into two Subgroups A and B. The findings were processed using descriptive statistical methods.
Results. In Group 1 including patients undergoing medical management tactics, an unfavorable outcome was observed in 9 (52.9%) cases mainly due to the progression of pump fetal cardiomyopathy and polyhydramnios. The mean delivery time in this group was 32.3 ± 5.4 weeks. A favorable outcome was observed in 78.6% of cases in Group 2, with 77.3 and 83.3% in Subgroup A and B, respectively. The mean delivery time in Group 2 was 34.5±3.1 weeks.
Conclusion. The rate of a favorable RAPS-complicated pregnancy outcome was significantly higher in the intrauterine treatment group than that in the medical management tactics group (78.6 and 47.1%, respectively; P = 0.0023).
Keywords
Twin reversed arterial perfusion sequence (TRAP) is a rare complication of monochorionic multiple pregnancy with the incidence of 1 in 35,000 births. It is characterized by the presence of fetal malformations and the absence of the functioning heart in one of the twins (acardiac twin); at the same time, its blood supply is ensured by the other twin (pump twin). An unfavorable outcome of pregnancy complicated by TRAP is observed in 60–85%.
The pathogenesis of this condition is not completely clear. Presumably, the acardiac twin develops under the conditions of the existence of two dominant anastomoses in the monochorionic placenta [1]. By the arterio-arterial anastomosis, the pump-twin pumps blood to the acardiac twin and by the veno-venous anastomosis it returns. Thus, the pump-twin provides the blood circulation to the acardiac twin with the opposite direction of the blood flow. Actually, the development of insufficiency of most organs in the acardiac twin is associated with hemodynamic dysfunction, it is manifested by the fact that blood under low pressure comes to it with low oxygen [2, 3].
The main ultrasound feature of TRAP includes: the absence of the normally functioning heart and reverse blood flow in the umbilical artery in an abnormally formed fetus. Additional features include a wide range of fetal abnormalities: acrania or other head and brain malformations, limbs reduction, thickening of the nuchal translucency, single umbilical artery, and other major anomalies [4]. In the first trimester of pregnancy the acardiac twin can be diagnosed as vanishing twin, especially if there are structures of the skull and vertebral column. However, during ultrasound examinations acardiac twin will grow. Differential diagnosis is also performed with teratoma. Unlike teratomas, acardiac twin always has a relationship to the placenta through the umbilical cord [5].
Pregnancy complications in TRAP sequence are caused by active growth of the acardiac twin, which is a reflection of its excessive blood supply from the pump-twin. Progressively increasing blood volume in the common circulation leads to the development of cardiomyopathy, heart failure and finally to intrauterine death of the pump twin. Also, the increased amniotic fluid volume due to polyuria of the pump twin leads to premature rupture of membranes and premature birth [6].
The key issue of pregnancy management is the risk assessment of unfavorable outcome. In case of the diagnosis of TRAP sequence before 12 weeks of gestation, it is recommended to inform the woman about the high rates of adverse perinatal outcomes and suggest terminating the pregnancy. The pregnancy is preserved when the diagnosis of this syndrome is late. Pregnancy management is divided into conservative follow-up and fetal surgery. In order to improve the perinatal outcomes of pregnancy complicated by TRAP, various intrauterine interventions are undertaken to stop the blood flow to the acardiac twin. Currently, the question remains unknown whether intrauterine intervention should be performed in all patients with TRAP, since the operation has risks such as pump twin death, preterm rupture of membranes and premature birth. On the other hand, in the absence of increased blood supply and growth of the acardiac twin, conservative follow-up management should be performed.
In this regard, it is relevant to conduct a study aimed to determine the appropriate management of monochorionic multiple pregnancy complicated by TRAP, and clear indications for fetal surgical treatment.
The objective of the study is to compare the effectiveness of surgical and conservative management of pregnancy complicated by TRAP.
Materials and Methods
This is a retrospective study of 47 patients with multiple pregnancy complicated by TRAP. The patients were examined and treated at National Medical Research Center of Obstetrics, Gynecology and Perinatology named after Academician V.I. Kulakov, Moscow from 2010 to 2017.
Prenatal diagnosis of TRAP sequence was based on the detection of monochorionic multiple pregnancy and the presence of abnormalities in one of the fetuses, reversed blood flow in the umbilical artery and the absence of the normally functioning heart. The progression of TRAP sequence was diagnosed by confirmation of the increasing size of the acardiac twin and preservation of blood flow in the vessels of the umbilical cord and the body.
In each case, a detailed pump twin anatomy assessment was performed in order to exclude congenital malformations. Special attention was paid to the echographic signs of the pump twin cardiomyopathy that was manifested by cardiomegaly, myocardial hypertrophy, insufficiency of atrioventricular valves, abnormal blood flow in the ductus venosus and polyhydramnios.
All patients were explained various options of pregnancy management in TRAP, including expectant management and fetal surgery. The choice of pregnancy management was based on the gestational age at the time of hospitalization to Research Center, the clinical condition and the patient’s request. Fetal surgery was offered to patients from 15 to 23 weeks of gestation in cases of progressive acardiac twin growth and patients with signs of the pump twin cardiomyopathy, and also in cases with monoamniotic pregnancies. Expectant management was recommended in the absence of signs of TRAP sequence progression, the absence of blood flow in the acardiac twin, as well as in pregnancy more than 23 weeks of gestation, due to the technical difficulties to coagulate large umbilical vessels.
In group 1 there were 17 patients with expectant management. Group 2 included 28 pregnant women who underwent fetal surgery. Depending on the type of surgery performed, group 2 was divided into two subgroups – a and b. Subgroup a included 22 patients who underwent interstitial laser ablation of the umbilical cord vessels under ultrasound guidance. This operation was performed under local anesthesia. An 18G needle was used for the puncture of the anterior abdominal wall, the uterine wall and the body of the acardiac twin. Under ultrasound guidance with color Doppler mapping, the end of the needle was brought to the umbilical cord, 0.7 mm Nd:YAG light guide of the laser (Dornier Medilas Fibertom 8100, Dornier MedTech, Germany) was introduced into the needle. Several sessions of ablation of continuous-wave 50 W power were conducted prior to the absence of blood flow in the umbilical vessels.
Six patinets with monoamniotic monochorionic multiple pregnancies underwent laser ablation and dissection of the umbilical cord of the acardiac twin under fetoscopic guidance.
The data were analyzed using Excel (Microsoft Office 2011) and SPSS Statistics 20.0 (SPSS Inc., Chicago, IL, USA). Mathematical methods of data analyzing include statistical and correlation analysis. To determine the significance of the differences of the compared categorical variables, we used the Fisher exact test and the χ2 test, and the Mann-Whitney test for continuous variables. The Pearson coefficient value less than 0.05 was taken as the level of statistical reliability.
Results
We performed a study of 47 pregnancies affected by TRAP sequence at National Medical Research Center of Obstetrics, Gynecology, and Perinatology, Moscow.
During our research two pregnancies were terminated at gestational age less than 12 weeks, in the first case the reason was early ultrasound identification of fetal malformations of pump twin (interventricular septal defect, common arterial trunk), in the second case it was the patient’s request. TRAP was worsening the progress of monochorionic diamniotic twins in 34 patients (72.3%). This complication occurred in seven patients (14.9%) with monochorionic monoamniotic twins pregnancies, in three patients (6.4%) with dichorionic triamniotic triplet pregnancies and in one patient (2.1%) with monochorionic triamniotic triplet pregnancy.
Group 1 included pregnancies which were managed expectantly. There were thirteen patients with monochorionic diamniotic twins, three patients with monochorionic monoamniotic twins and one patient with dichorionic triamniotic triplet. The second group included nineteen patients with monochorionic diamniotic twins, four patients with monochorionic monoamniotic twins, two patients with monochorionic triamniotic triplet pregnancy and one patient with dichorionic diamniotic triplet pregnancy.
We divided our patients into different groups according to pregnancy management and pregnancy outcomes as presented in Figure 1. In the first group we noticed positive progression of pregnancy in eight cases (47.1 %); it should be noted that five of them at the gestational age before 20 weeks showed total spontaneous perfusion of the blood flow in the umbilical cord and torso vessels of fetus with acardia. Adverse perinatal outcomes took place in nine cases (52.9%), among them six cases were due to the increased blood supply of fetus with acardia. Polyhydramnios and cardiomyopathy developed in those pump twins, which were the reason of perinatal loss. Antenatal death of the pump twins was revealed in three cases before 16 weeks gestation without any signs of decompensation. Average term of delivery in the first group was 32.3 ± 5.4 weeks. The second group showed positive outcome in 78.6% cases (22 out of 28 patients).
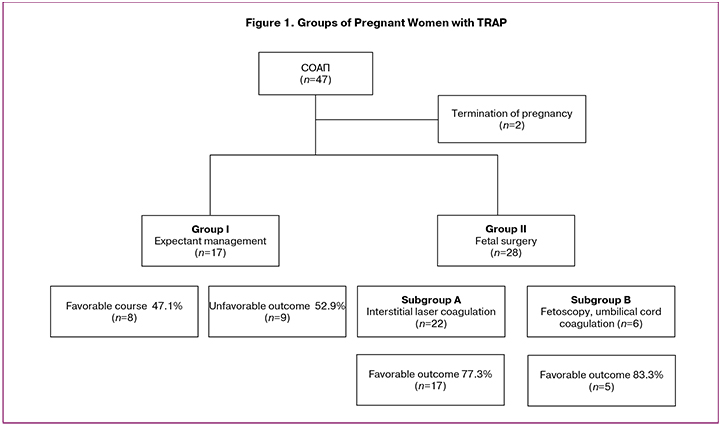
The most common method of intrauterine TRAP treatment was interstitial laser coagulation of vessels of acardiac fetuses. It was performed at gestational age 19.3 ± 3.2 weeks. This operation was done to 22 patients who were included into subgroup a. The frequency of positive outcomes in this subgroup was 77.3% (17 out of 22 patients). Interstitial laser coagulation of vessels of acardiac twin was not totally performed in four cases, therefore in those observations blood flow existed during the whole gestation. Meanwhile, the growth dynamics of acardiac fetuses were less expressed, than before the intervention, and the signs of cardiomyopathy and polyhydramnios were not noticed in the pump twin.
Five patients showed negative outcomes after interstitial laser coagulation of vessels of acardiac fetuses. Four patients suffered from death of the pump twin in early postoperative period. One patient had preterm rupture of amniotic fluid and preterm delivery (12 days after operation) at 23 weeks gestation. The child died in the early neonatal period because of prematurity. Coagulation and intersection of umbilical cord of acardiac fetus under fetoscopy control was performed to six patients from subgroup b at gestational age of 21.2 ± 2.4 weeks. The frequency of positive outcome was in five out of six patients (83.3%). One patient had preterm amniotic fluid rupture and abortion at 19 weeks 4 days gestation. Average term of delivery was 34.5 ± 3.1 weeks. It is worth noting that the frequency of preterm delivery in subgroup a was less than in subgroup b, it was – 4.5% and 16.7%, respectively.
Discussion Nowadays we continue discussing the proper choice of tactics of managing women with multifetal pregnancies complicated by TRAP. Moore et al. analyzed the outcomes of 49 pregnancies with TRAP. According to their data, perinatal mortality rate was 55% [7]. The pregnancy outcome depended directly on the degree of blood supply in acardiac fetus. It is well known that the risk of heart failure in a pump twin increases during the increased blood supply and growth progression of acardiac fetus. For the prognostic features of perinatal outcomes Moore and authors proposed to use the pump twin and acardiac fetus size ratio. When ratio is more than 70%, the chance of developing such complications as preterm labor, polyhydramnios, heart disorders of the pump twin significantly increases [7]. According to this fact, some authors prefer tactics of expectant management of patients with multiple pregnancy under regular ultrasound control of the pump twin [8]. In concordance with this research, according to other studies the survival rate of pump twins was approximately 88%, in cases when the size of acardiac fetus was less than 50% of pump twin size. The supporters of the conservative method consider the proofs and effectiveness of early operative intervention insufficient. Confirming their opinion it is very important to estimate the parameters of pump twin state carefully and regularly and provide operative intervention only in case of signs of decompensated heart activity or polyhydramnios. There is also another tactics of managing pregnancies complicated by TRAP. Early intrauterine intervention could be performed for preventive purposes before the complications can occur. As reported by Lewi et al., during the expectant management tactics in every third TRAP case the pump twin dies before 18 weeks of gestation. It happens without any predictors of possible negative outcome [10]. According to other authors’ data, fetal death before 16 weeks of gestation occurs in 83–100% of cases [10, 11].Results of early intrauterine intervention are very well promising – the pump twin survival rate reaches up to 80% [12].
Therefore, due to impossibility of accurateprediction of TRAP complications, cases of pump twin death without signs of decompensation and also technical difficulties appearing during the late operative intervention, the majority of researchers choose preventive intrauterine treatment at 16–20 weeks gestation [ 9, 13].
During the last decade next methods for blood system dissociation between the pump twin and acardiac fetus were offered: injection of 96 degree ethanol into the intraperitoneal part of umbilical artery [14], ligature of umbilical cord during fetoscopy [15], fetoscopic laser coagulation [13], mono and bipolar coagulation of umbilical cord vessels, interstitial laser coagulation under ultrasound control [12], high frequent ablation of acardiac fetus vessels [16], injection of the thrombogenic coil into the umbilical artery under ultrasound control, artificial embolization of acardiac fetus circulatory system [17], hysterectomy and selective delivery of acardiac fetus, coagulation of fetal vessels using high frequent ultrasound.
Nowadays the ultrasound-based interstitial laser coagulation of vessels is the most frequently applied approach. It is possible because of their less invasive nature, in comparison with high frequent ablation and fetoscopic access, and possibility to perform intervention at the early term of gestation [11]. Meta-analysis based on 10 researches of 51 TRAP cases managed by interstitial laser coagulation of acardiac fetus vessels demonstrated that positive outcome for the pump twin can be seen in 80% of cases, but preterm delivery (before 3 gestation weeks) occurred in 11%. Recenlty published meta-analysis showed improved outcomes, if the treatment was performed before 16 gestation week. In 18 cases, the patients underwent FLS before 16 weeks of gestation, survival rate of the pump twin was 88.9% (16 out of 18 cases) and preterm delivery frequency was 11.1% (11). In our research the amount of negative outcomes after interstitial laser coagulation was also low 22.7% (5 and 22).
Intrauterine intervention in the pregnancies complicated by TRAP, is usually performed at 17–18 weeks gestation under the fetoscopy control. The common indication for operative intervention is monoamniotic multifetal pregnancy with TRAP, when it remains not only coagulation of acardiac fetus umbilical cord, but also its transection, because of the chance of umbilical cord entanglement. As result the possibility of pump twin death is very high. The variety of researches demonstrates data about positive outcomes frequency, which is more than 80% during this type of therapy. But the risk of preterm rupture of membranes is 22%–57%, which usually leads to preterm delivery. In addition the umbilical cord coagulation of acardiac fetus under the fetoscopy control at 17 weeks gestation is followed by higher chance of pump twin death. Literally acardiac fetus umbilical cord coagulation and transection under the fetoscopy control is a method of choice just in case of monoamniotic twins. During our research six fetoscopic laser coagulations and acardic fetuses umbilical cord transections were performed. The rate of positive outcome was 83.3% (5 out of 6 cases). We must notice the high rate of preterm deliveries in comparison with subgroup, where interstitial laser coagulation of vessels was performed, 16.7% and 4.5%, respectively.
Conclusion
The prognosis for the pump-twin in a twin reversed arterial perfusion sequence is usually unfavorable. The natural course of this syndrome is accompanied by high rates of perinatal morbidity and mortality. Unfortunately, the expectant management of pregnancy does not prevent the development of complications. According to our results, timely performed fetal surgery for TRAP sequence contributes to a significant reduction in perinatal losses.
References
1. Baergen N.R. Manual of pathology of the human placenta. 2nd ed. Springer; 2011.
2. Lewi L., Deprest J., Hecher K. The vascular anastomoses in monochorionic twin pregnancies and their clinical consequences. Am. J. Obstet. Gynecol. 2013; 208(1): 19-30. doi: 10.1016/j.ajog.2012.09.025.
3. Низяева Н.В., Костюков К.В., Гладкова К.А., Куликова Г.В., Щеголев А.И. Роль синдрома обратной артериальной перфузии близнецов в развитии плода-акардиуса. Архив патологии. 2016; 78(4): 54-7.
4. Костюков К.В., Павлов К.А., Дубова Е.А., Стыгар А.М., Гус А.И., Щеголев А.И. Синдром обратной артериальной перфузии (клинические наблюдения и обзор литературы). Медицинская визуализация. 2012; 6: 120-6.
5. Курмангали Ж.К., Джаманаева К.Б., Жулаушинова М.Е., Усеева М.С. Случай синдрома обратной артериальной перфузии с благоприятным исходом для ребенка. Акушерство и гинекология. 2014; 5: 84-6.
6. Прибушеня О.В., Новикова И.В., Семенчук В.Л., Лазаревич А.А., Белуга М.В. Синдром обратной артериальной перфузии близнецов: медико-генетическое консультирование, акушерская тактика и методы коррекции. Пренатальная диагностика. 2015; 3: 215-23.
7. Moore T.R., Gale S., Benirschke K. Perinatal outcome of forty-nine pregnancies complicated by acardiac twinning. Am J Obstet Gynecol 1990;163:907-12.
8. Jelin E., Hirose S., Rand L., Curran P., Feldstein V., Guevara-Gallardo S. et al. Perinatal outcome of conservative management versus fetal intervention for twin reversed arterial perfusion sequence with a small acardiac twin. Fetal Diagn. Ther. 2010; 27(3): 138-41. doi: 10.1159/000295176.
9. Lewi L., Valencia C., Gonzalez E., Deprest J., Nicolaides K.H. The outcome of twin reversed arterial perfusion sequence diagnosed in the first trimester. Am. J. Obstet. Gynecol. 2010; 203:213. e1-4. doi: 10.1016/j.ajog.2010.04.018.
10. Scheier M., Molina F.S. Outcome of twin reversed arterial perfusion sequence following treatment with interstitial laser: a retrospective study. Fetal Diagn. Ther. 2012; 31(1): 35-41. doi: 10.1159/000334156.
11. Pagani G., D’Antonio F., Khalil A., Papageorghiou A., Bhide A., Thilaganathan B. Intrafetal laser treatment for twin reversed arterial perfusion sequence: cohort study and meta-analysis. Ultrasound Obstet. Gynecol. 2013; 42(1): 6-14. doi: 10.1002/uog.12495.
12. Berg C., Holst D., Mallmann M.R., Gottschalk I., Gembruch U., Geipel A. Early vs late intervention in twin reversed arterial perfusion sequence. Ultrasound Obstet. Gynecol. 2014; 43(1): 60-4. doi: 10.1002/uog.12578.
13. Hecher K., Lewi L., Gratacos E., Huber A., Ville Y., Deprest J. Twin reversed arterial perfusion: fetoscopic laser coagulation of placental anastomoses or the umbilical cord. Ultrasound Obstet. Gynecol. 2006; 28(5): 688-91. doi: 10.1002/uog.3816.
14. Corbacioglu A., Gul A., Bakirci I.T., Gedikbasi A., Yildirim G. Treatment of twin reversed arterial perfusion sequence with alcohol ablation or bipolar cord coagulation. Int. J. Gynaecol. Obstet. 2012; 117(3): 257-9. doi: 10.1016/j.ijgo.2011.12.022.
15. Takano M., Murata S., Fujiwara M., Hirata H., Nakata M. Experience of fetoscopic laser photocoagulation and cord transection for twin-reversed arterialperfusion sequence. J. Obstet. Gynaecol. Res. 2015; 41(9): 1326-9. doi: 10.1111/jog.12720.
16. Weichert A., Kalache K., Hein P., Brauer M., Hinkson L., Henrich W. Radiofrequency ablation as a minimally invasive procedure in the treatment of twin reversed arterial perfusion sequence in twin pregnancy. J. Clin. Ultrasound. 2013; 41(4): 245-7. doi: 10.1002/jcu.21932.
17. Chaveeva P., Poon L.C., Sotiriadis A., Kosinski P., Nicolaides K.H. Optimal method and timing of intrauterine intervention in twin reversed arterial perfusion sequence: case study and meta-analysis. Fetal Diagn. Ther. 2014; 35(4): 267-79. doi: 10.1159/000358593.
18. Абрамян М.А., Гладкова К.А., Костюков К.В., Тетруашвили Н.К. Открытая и пункционная хирургия плода в современном акушерстве. Акушерство и гинекология. 2014; 1: 3-8.
Received 17.02.2018
Accepted 02.03.2018
About the Authors
Kostyukov, Kirill V., MD, doctor of the Department of the Functional Diagnosis National Medical Research Center for Obstetrics, Gynecology and Perinatology namedafter Academician V.I.Kulakov of Ministry of Healthcare of Russian Federation, Moscow, Russia.
117997, Russia Moscow, Ac. Oparina str. 4. Tel +79262149784, email: kostyukov_k@yahoo.com
Gladkova, Kristina A., MD, senior researcher of the Department of Pregnancy Loss Prevention and Therapy, National Medical Research Center for Obstetrics,
Gynecology and Perinatology named after Academician V.I.Kulakov of Ministry of Healthcare of Russian Federation, Moscow, Russia,
117997, Russia Moscow, Ac. Oparina str. 4. Tel +79163211007, email: k_gladkova@oparina4.ru
Tetruashvili, Nana K., MD, PhD, Head of the Department of Pregnancy Loss Prevention and Therapy, National Medical Research Center for Obstetrics,
Gynecology and Perinatology named after Academician V.I.Kulakov of Ministry of Healthcare of Russian Federation, Moscow, Russia.
117997, Russia Moscow, Ac. Oparina str. 4. Tel +74954381477, email: tetrauly@mail.ru
For citations: Kostyukov K.V., Gladkova K.A., Tetruashvili N.K. Pregnancy management tactics in reversed arterial perfusion syndrome. Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2018; (11): 44-9. (in Russian)
https://dx.doi.org/10.18565/aig.2018.11.44-49