По данным ВОЗ, пандемия COVID-19, став глобальной проблемой мирового здравоохранения, наиболее остро отражается на женщинах, находящихся на различных этапах беременности – от зачатия до родов, а также в послеродовом периоде [1, 2]. Известно, что при беременности на фоне изменений в иммунной и сердечно-легочной системе создаются благоприятные условия для развития респираторных вирусных инфекций [3]. В настоящее время имеются противоречивые данные относительно большей подверженности беременных женщин инфицированию COVID-19, а также не существует конкретных рекомендаций относительно диагностики, лечения и социально-психологического сопровождения при беременности с COVID-19 [4]. Отмечается, что клиническая картина инфекции COVID-19 у беременных сопоставима с таковой у инфицированных небеременных женщин, а частыми симптомами являются лихорадка, кашель, миалгия, боль в горле [5].
Исследованиями показано, что летальность при COVID-19 среди беременных достигает 25%; частота преждевременных родов составляет от 4,3 до 25,0%, преэклампсии – 5,9%, выкидышей – 14,5%, преждевременного разрыва плодных оболочек – 9,2% и задержки роста плода – 2,8–25,0% [6].
Наиболее острой и малоизученной остается проблема, связанная с влиянием пандемии на психоэмоциональное состояние беременных и женщин в ближайшем послеродовом периоде. Так, результаты целого ряда исследований показали, что беременные женщины имеют самые высокие показатели депрессии, тревоги и стресса, которые могут усугубляться пандемическим контекстом COVID-19 [7–9].
Также было отмечено, что беременные женщины, испытавшие сильный стресс, связанный с инфицированием COVID-19, имеют наиболее высокий риск неблагоприятных перинатальных исходов [10]. Большинство клиницистов стремятся лучше понять ее феноменологию, сделав акцент на содержание коллективного беспокойства с помощью проведения различных контент-анализов и разработки системных подходов к психокоррекции возникших состояний, что позволит значительно смягчить акушерские и соматические осложнения, возникающие во время беременности, как последствия стресса [11, 12].
В связи с вышеизложенным, целью исследования явилось проведение структурного анализа нарушений психоэмоционального статуса беременных женщин с пневмонией COVID-19.
Материалы и методы
Фундаментом исследования послужили результаты обследования и лечения 3080 беременных женщин и молодых матерей, инфицированных SARS-CoV-2 во время пандемии COVID-19 в условиях родильного отделения Республиканской специализированной инфекционной больницы Зангиота № 1 с декабря 2020 г. по 1 января 2022 г.
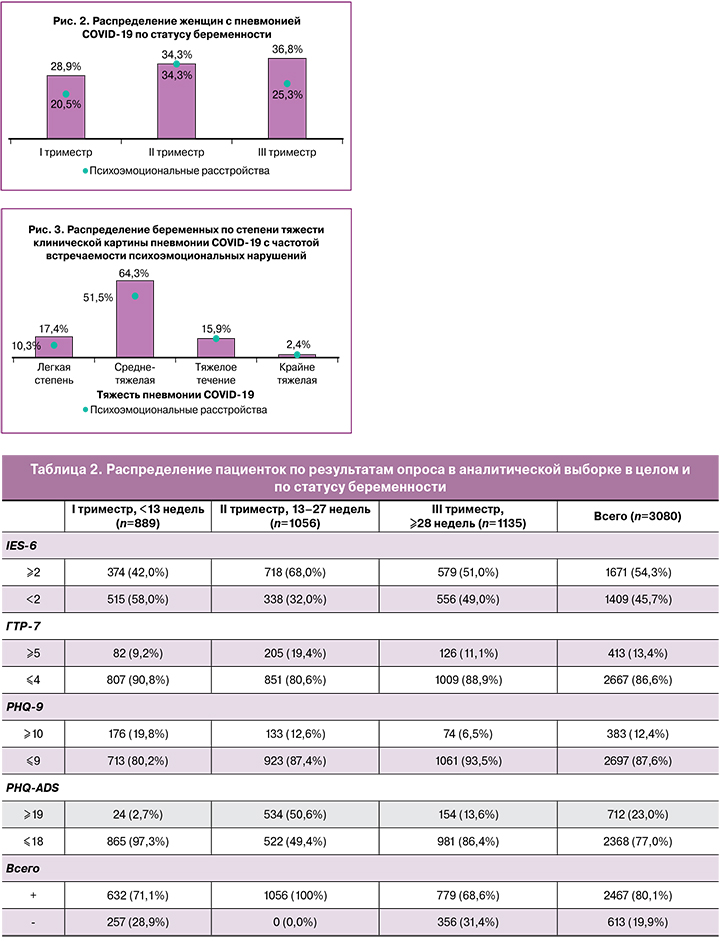
Большинство женщин (48,0%; 1478/3080) находились в возрастном диапазоне 26–30 лет, а также большинство женщин (84,0%; 2586/3080) не имели выкидышей в анамнезе. По количеству беременностей в анамнезе больше всего отмечено случаев с двумя (31,0%; 956/ 3080) и одной беременностью (27,5%; 847/3080) в анамнезе. Всего 5,9% (183/ 3080) беременных были первородящими (табл. 1). На момент поступления больных в стационар в I триместре беременности (<13 недель гестации) находились 889/3080 женщин (28,9%), во II триместре (13–27 недель гестации) – 1056/3080 женщин (34,3%) и больше всего в III триместре беременности (≥28 недель гестации) – 1135/3080 женщин (36,8%). Согласно международным критериям оценки степени тяжести инфекции COVID-19, у беременных женщин в подавляющем большинстве (64,3%; 1980/3080) случаев диагностировано среднетяжелое течение пневмонии. Клиническая картина беременных с инфекцией COVID-19 была представлена двусторонней пневмонией у 48,0% (1478/3080). При этом до 50% поражения легких по данным мультиспиральной компьютерной томографии имели большинство (60,0%; 1848/3080) пациенток.

Экстрагенитальные заболевания отмечались у 1232/3080 (40,0%) пациенток и были представлены: вегетососудистой дистонией, гипертонической болезнью различной степени тяжести, хроническим бронхитом, тонзиллитом, хроническим пиелонефритом, хроническим гастритом, колитом, панкреатитом, аутоиммунным тиреоидитом, метаболическим синдромом, ожирением, миопией. У 943 пациенток отмечалось сочетание различных заболеваний. Гинекологические заболевания в анамнезе: эктопия шейки матки, воспалительные заболевания матки и ее придатков, опухоли и опухолевидные образования яичников, миома матки, внематочная беременность, бесплодие различного генеза отмечались у 914 пациенток.
Выявление и оценка степени тяжести психоэмоциональных нарушений проводились по шкале оценки тревожных расстройств ГТР-7, шкале оценки посттравматических стрессовых расстройств (ПТСР) IES-6 и шкале оценки депрессивного синдрома PHQ-9 [13–16]. Выявление сочетанной психоэмоциональной патологии производили по специальной объединенной шкале PHQ-ADS, которая представляет собой сумму баллов из опросников PHQ-9 и ГТР-7 (максимальный балл 48, сочетание ПТСР, тревоги и депрессии проявляется при 20 и более баллах).
Результаты
По результатам заполнения специализированных шкал и опросников, за весь период исследования значительная часть женщин (80,1%; 2467/3080) набрали баллы на уровне или выше пороговых значений, что было характерно для умеренного и выраженного ПТСР, умеренной и выраженной тревоги и клинически значимой депрессии. В структуре психоэмоциональных нарушений 54,3% (1671/3080) приходилось на ПТСР (≥2,0 балла по шкале IES-6); 13,4% (413/3080) больных имели клинические проявления от умеренной до выраженной тревоги (≥5 баллов по шкале ГТР-7), а депрессивные состояния различной степени выраженности отмечали 12,4% (383/3080) женщин (≥10 баллов по шкале PHQ-9).
Таким образом, в более чем половине случаев мы сталкивались с ПТСР, из числа которых в 712/3080 случаях (23,0%) диагностировали сочетанные нарушения психоэмоционального состояния, т.е. к имеющимся расстройствам присоединялись клинические проявления тревоги и/или депрессии (рис. 1, табл. 2).
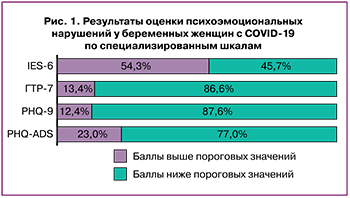
Исходя из периода беременности на момент поступления женщин с пневмонией COVID-19 в стационар, сроки гестации до 13 недель (I триместр) характеризовались преобладанием ПТСР, что было выявлено в 42,0% (374/889) случаев. Также в I триместре в 19,8% (176/889) случаев отмечались депрессивные состояния и в 9,2% (82/889) – тревожные расстройства (табл. 2). Таким образом, частота встречаемости различных психоэмоциональных нарушений у беременных женщин на фоне инфицирования COVID-19 в I триместре беременности составила 71,1% (632/889).
Во II триместре беременности (13–27-я недели гестации) в 100% (1056/1056) случаев отмечаются ПТСР, тревога или депрессия от умеренной до выраженной степени тяжести, определяемые по специальным шкалам IES-6, ГТР-7 и PHQ-9. При этом наибольшую частоту (68,0%; 718/1056) имеет ПТСР (табл. 2). По встречаемости сочетанной психоэмоциональной патологии при беременности на фоне COVID-19 данный период гестации также имеет статистически значимые высокие цифры по отношению к другим триместрам – 50,6% (534/1056) против 2,7% (24/ 889) в I триместре и 13,6% (154/ 1135) в III триместре беременности (табл. 2). Среди женщин в III периоде беременности (≥28 недель гестации) наиболее высокой также была встречаемость ПТСР, составив 51,0% (579/1135). Тревожные расстройства диагностированы в 11,1% (126/1135) случаев; депрессивные состояния были наименьшими, составив 6,5% (74/1135).
Выявлена сравнительно большая частота встречаемости психоэмоциональных расстройств (51,5%; 1585/3080) в когорте среднетяжелого течения (n=1980) COVID-19 (рис. 3). В самой же структуре среднетяжелого течения пневмонии COVID-19 большая часть женщин (59,5%; 1178/1980) имели клинику ПТСР (более 2 баллов по шкале IES-6); в остальных случаях отмечались чисто тревожные (10,1%; 200/1980; более 5 баллов по ГТР-7) и депрессивные (10,5%; 207/1980; более 10 баллов по шкале PHQ-9) состояния (табл. 3, рис. 4). Практически равную частоту встречаемости имели ПТСР среди беременных с COVID-19 тяжелой и крайне тяжелой степени (54,3 и 52,7% соответственно), так же, как и тревожные (28,6 и 28,4% соответственно) и депрессивные (17,1 и 18,9% соответственно) состояния.
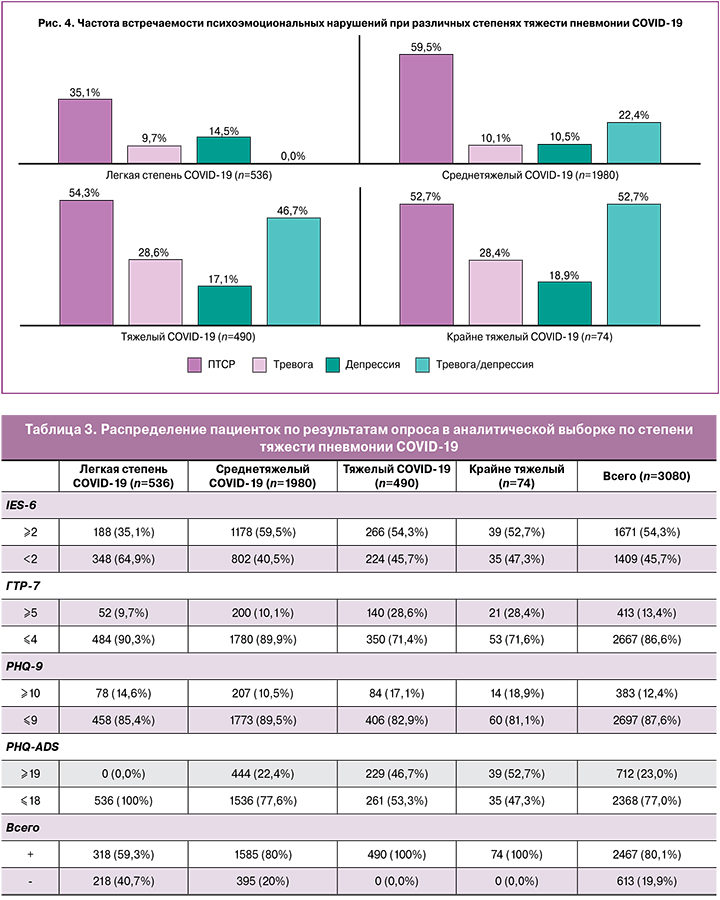
Высокая частота встречаемости смешанных психоэмоциональных расстройств, оцененных по шкале PHQ-ADS выше 19 баллов, была характерна для беременных женщин с пневмонией COVID-19 тяжелой и крайне тяжелой степени – 46,7 и 52,7% соответственно (рис. 4, табл. 3). Таким образом, с усугублением клинической картины пневмонии COVID-19 отмечалась 100% распространенность психоэмоциональных расстройств.
Чисто депрессивный синдром имеет высокую частоту в I триместре, проявляется во II триместре со значимо низкой частотой и имеет наименьшую частоту встречаемости в III триместре. Данное обстоятельство обуславливалось увеличением количества женщин с ПТСР и сочетаниями депрессии с тревогой по мере повышения статуса беременности.
Обсуждение
С пандемией COVID-19 практически всеми клиницистами отмечается значительное возрастание психоэмоциональных расстройств. Так, Green S.M. et al. (2021) провели исследование с участием 84 беременных, из которых у одной трети основные опасения были связаны с влиянием COVID-19 на течение беременности, а 40% беспокойств – с перинатальным контекстом [17].
В период май–июнь 2020 г. в 64 странах был проведен анонимный перекрестный онлайн-опрос беременных и родильниц. Данные этих исследований были размещены на платформе Pregistry для исследований COVID-19 (https://corona.pregistry.com) на 12 языках. Участники выполнили измерения по демографическим характеристикам, воздействию COVID-19 и беспокойству, а также симптомам психического здоровья, включая посттравматический стресс по шкале IES-6, тревогу/депрессию по шкале PHQ-4 и одиночество по шкале UCLA-3 [18, 19]. Из 6894 участников значительная часть женщин набрала баллы на уровне или выше пороговых значений для повышенного ПТСР (2979 [43%]), тревоги/депрессии (2138 [31%]) и одиночества (3691 [53%]). Наиболее часто сообщаемые опасения были связаны с беременностью и родами, в том числе с невозможностью посещения родственниками после родов (59%), с заражением ребенка COVID-19 (59%), с отсутствием поддержки во время родов (55%), изменениями в плане родов (41%). Большее беспокойство, связанное с детьми (т. е. ненадлежащий уход за детьми, риск их заражения), и пропуски визитов к врачу были связаны со значительно более высокими шансами посттравматического стресса, тревоги/депрессии и одиночества [18, 19].
Farrell T. et al. (2020) по результатам своих исследований также выявили высокую распространенность тревожной и депрессивной симптоматики (34,4 и 39,2% соответственно) по шкале PHQ-ADS в одной из самых экономически развитых стран мира – Катаре [20].
Alfayumi-Zeadna S. et al. (2020) оценили распространенность симптомов перинатальной депрессии во время пандемии COVID-19 среди арабских и еврейских женщин в Израиле. Выборка включала 730 перинатальных женщин (604 еврейки и 126 арабок). Распространенность перинатальной депрессии во всей исследуемой популяции составила 40%, среди арабских женщин была значительно выше, чем среди еврейских (58% против 36%, р<0,001). Более высокие значения перинатальной депрессии были в значительной степени связаны с симптомами тревоги (р<0,001) и стресса на фоне COVID-19 (р< 0,001) [21].
Ceulemans M. et al. (2021) провели исследование у 9041 женщины с COVID-19 (в том числе 3907 беременных и 5134 кормящих). Распространенность больших депрессивных симптомов составила 15% в когорте беременных и 13% в когорте грудного вскармливания. Симптомы генерализованной тревоги от умеренной до тяжелой были обнаружены у 11 и 10% беременных и кормящих женщин. Факторами риска, связанными с плохим психическим здоровьем, являлись: наличие хронических психических заболеваний, хронических соматических заболеваний в послеродовом периоде, курение, незапланированная беременность, профессиональный статус [22].
В нашем исследовании с участием 3080 беременных женщин показано влияние статуса беременности на распространенность нарушений психоэмоционального статуса в каждом периоде гестации. Так, женщин с ПТСР и сочетаниями депрессии с тревогой было значимо больше во II триместре беременности; меньшая частота имела место среди женщин в I триместре беременности, что было показано путем частного и общего структурного анализа. Также показано влияние тяжести пневмонии COVID-19 на частоту развития тревожных расстройств и сочетанных нарушений психоэмоционального статуса при беременности. Большая часть беременных женщин с психоэмоциональными расстройствами (51,5%; 1585/3080) были отнесены к когорте среднетяжелого течения COVID-19.
Резюмировать обсуждение можно результатами исследования, полученными Chen Q. et al. (2022), которые показали, что пандемия COVID-19 может оказать пагубное влияние на психическое здоровье женщин после родов. Изучение распространенности и факторов риска депрессии среди женщин в послеродовом периоде могло бы пролить некоторый свет на их психоэмоциональное состояние. Это позволило бы предложить ряд мер поддержки и специализированные вмешательства во время пандемии COVID-19 для улучшения исходов матерей и младенцев. Авторами было настоятельно рекомендовано провести гораздо больше исследований психологического благополучия матерей во время пандемии COVID-19 в странах со средним и низким уровнем дохода [23].
Заключение
Психоэмоциональные нарушения на фоне инфицирования COVID-19 характерны для значительной части (80,1%; 2467/3080) беременных женщин, со 100% (n=1056) показателем во II триместре беременности. Депрессивный синдром наиболее часто выявляется в I триместре, а тревожные состояния и ПТСР более характерны для женщин во II триместре беременности. Обращает на себя внимание также увеличение количества женщин с ПТСР и сочетаниями депрессии с тревогой по мере повышения статуса беременности. Высокая частота встречаемости смешанных психоэмоциональных расстройств выявляется среди беременных женщин с пневмонией COVID-19 тяжелой и крайне тяжелой степени – 46,7 и 52,7% соответственно, что свидетельствует об усугублении клинической картины психоэмоциональных нарушений на фоне прогрессирования пневмонии COVID-19.