Comparative analysis of stillbirth causes and rates in the Russian Federation in 2019 and 2020
Aim: To make a comparative analysis of causes and rates of early neonatal mortality in the Russian Federation in 2019 and 2020.Shchegolev A.I., Tumanova U.N., Chausov A.A., Shuvalova M.P.
Materials and methods: This study was based on the analysis of statistical forms А-05 of the Federal State Statistics Service (Rosstat) for the years 2019–2020. These forms included medical records of perinatal deaths related to stillbirths. Stillbirth rates were calculated as the ratio of stillbirths to the total number of babies born alive and dead multiplied by 1000.
Results: In 2020, the number of babies born alive decreased by 7.6%, and the number of babies born dead increased by 1.12% versus the data reported in 2019. In 2020, the rate of stillbirth (5.67‰) increased by 4.2% versus the rate in 2019 (5.44‰). Most of all, the increase in stillbirths was noted in the South and Siberian Federal Districts. In general, the most common causes of stillbirths in the Russian Federation were respiratory disorders: the number of antenatal hypoxia was 78.2 (80.5%) and fetal intrapartum hypoxia was 6.7 (5.0%) of total number of stillbirths in 2019 and 2020, respectively. The proportion of congenital anomalies as the main disease was 6.7 (5.4%) of total number of stillbirths in 2019 and 2020, respectively. It was noted, that the number of stillborn babies with unknown causes of death increased by 52.2% in 2020 (4.7% of total number of stillborn babies) versus 2019 (3.1% of total number of stillborn babies)). Significant differences between the rates of major diseases that caused stillbirths were registered in different Federal Districts of the Russian Federation.
Conclusion: According to Rosstat data, in 2020 (due to COVID-19 pandemic), the absolute number of babies born dead increased by 1.1% and the rate of stillbirths increased by 4.2% compared to 2019. Increased proportion of respiratory diseases, in particular, antenatal hypoxia and congenital pneumonia, reflects the direct and indirect effects of SARS-CoV-2 infection.
Keywords
The year 2020 was marked not only by active studies of novel coronavirus strain SARS-CoV-2 (Severe Acute Respiratory Syndrome Coronavirus 2), but also by novel coronavirus disease COVID-19. Predominantly, the elderly people were affected and had a severe course of the disease, and this is considered to be a specific feature of COVID-19 [1, 2].
It should be noted, that during previous outbreaks of coronavirus infections, in particular, Middle East Respiratory Syndrome (MERS) and Severe Acute Respiratory Syndrome (SARS), both maternal and infant morbidity and mortality rates increased, although no clearly confirmed cases of vertical transmission of infections were observed [3].
Currently, a sufficient number of publications on SARS-CoV-2 coronavirus have appeared both in the form of descriptions of individual observations and systematic reviews suggesting a possibility of the so-called vertical (transplacental) transmission of SARS-CoV-2 infection from mother to fetus [4–6].
Due to this, it is an urgent task to clarify the features of fetal injuries and death.
The aim of this study was a comparative analysis of causes and rates of early neonatal mortality in the Russian Federation in 2019 and 2020.
Materials and methods
This study was based on the analysis of statistical forms А-05 of the Federal State Statistics Service (Rosstat) for the years 2019–2020. These forms included medical records of perinatal deaths related to stillbirths. Stillbirth rates were calculated as the ratio of the number of stillbirths to the total number of babies born alive and born dead multiplied by 1000. According to the Order of the Ministry of Social Development of Russia No. 1687 dated 27.12.2011 “On medical criteria for birth, the form of the birth document and issuance procedure”, starting from January 01, 2012, “stillbirth is defined as the birth of a baby at ≥22 weeks’s gestation with birth weight 500 g or more (or less than 500 g for multiple births) or when the baby's body weight at birth is unknown, and the body length is ≥ 25 cm in the absence of the signs of a live birth”. The bodies of all stillborn babies are subject to mandatory post-mortem autopsy with appropriate diagnosis, records and subsequent compiled statistics.
Rosstat’s statistical forms “А-05” contain grouped information on the number of stillborn babies depending on the major diseases (initial cause of death), as well as maternal diseases and conditions that contributed to newborn death. Major diseases (initial causes of death) are classified in 9 groups: group I – birth traumas; II – neonatal respiratory disorders; III – infectious diseases; IV – hemorrhagic and hematologic disorders; V – endocrine, metabolic and other pathologies, specific for neonatal period; VI – congenital anomalies, VII – traumas and intoxication; VIII – other causes of death, IX – observations with unknown cause of death.
Statistical analysis
Stillbirth rates were calculated as the ratio of the number of stillbirths to the total number of babies born alive and born dead multiplied by 1000. Chi-square (χ2) test was used for comparison of qualitative data, and stillbirth rates were estimated as relative risk (RR) with 95% confidence interval (CI). Statistical data analysis was performed using IBM SPSS Statistics v26.
Results
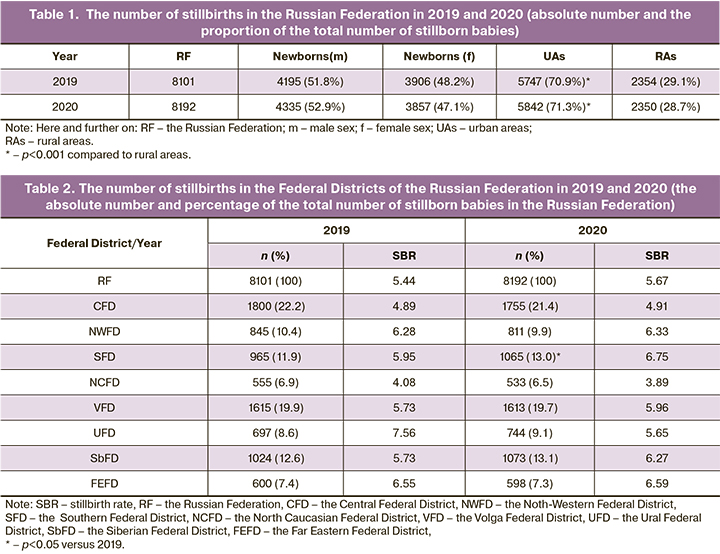
According to reported data in Rosstat’s statistical forms А-05, in 2019, 1 481 074 live born and 8101 stillborn babies were registered in the Russian Federation (Table1). In 2020, 1 436 514 infants were born alive, and their number was 7.6% less compared to 2019, and 8192 babies were born dead, and their number was 1.1% higher compared to 2019 г. As a result of these demographic changes, in 2020, the calculated stillbirth rate was (5.67‰), and that was 4.23% higher compared to 5.44‰ in 2019.
A distinctive feature of both compared periods (2019 and 2020) was an absolute increase in the number of stillborn babies compared to previous years. In 2012, when presently existing birth registration criteria entered into force (body weight at birth ≥500 g at 22 weeks’ gestation and over), 12 142 stillborn infants were registered in the Russian Federation, and stillbirth rate was 6.34‰ [7]. In 2014 and 2016, the total number of stillborn babies was 11 593 and 10 884, and stillbirth rate was 6.02 and 5.73‰, respectively [8, 9]. Moreover, in 2010, when according to the order No 318 of 04.12.1992 and Resolution No. 190 of 04.12.1992 of the State Committee for Statistics (Goskomstat, former name of Rosstat), stillbirth was defined as birth of a baby at ≥ 28 weeks’ gestation with birth weight ≥ 1000 g, the total number of stillborn infants was 8 300, and the stillbirth rate was 4.62‰ in the Russian Federation [10]. This means that overall stillbirth rate in the country decreased in 2020 compared to the rates in 2012, 2014 and 2016 by 10.6%, 5.81% and 1.05%, respectively. But, as has been described before, the rate increased by 4.23% compared to the year 2019. Thus, on the background of stable trend of stillbirth reduction in 2020, the incidence of stillbirth was higher.
In 2019, the percentage of stillborn male and female babies was 51.8% and 48.2%, respectively, but 52.9% and 47.1%, respectively, in 2020. In other words, in 2020, the proportion of stillborn boys slightly increased and the proportion of stillborn girls decreased. At the same time, a significantly greater number of stillbirths in the compared years was in urban areas versus rural areas: 70.9% in 2019 and 71.3% in 2020 (Table 1).
The number of stillbirths was different in the Federal Districts of the Russian Federation (Table 2). In 2019 and 2020, the highest stillbirth rates were traditionally in the Central Federal District (22.2 and 21.4% of total stillbirths in the Russian Federation, respectively), and in the Volga Federal District (19.9 and 19.7%). The lowest stillbirth rates were in the North Caucasian Federal District (6.9% and 6.5%, respectively). In addition, the increase in the number of stillbirths in three Federal Districts (Southern, Ural and Siberian Federal Districts), and the reduction of absolute number of stillbirths in the remaining five Federal Districts was registered. At the same time, the number of stillbirths increased in 6 Federal Districts in 2020 compared to 2019, and decreased only in 2 Federal Districts (the Ural and North Caucasian Federal Districts). The highest increase in the number of stillbirths by 13.4% and 9.4% was in the South and Siberian Federal Districts versus 2019. In the Ural Federal District the number of stillbirths decreased by 25.3%.
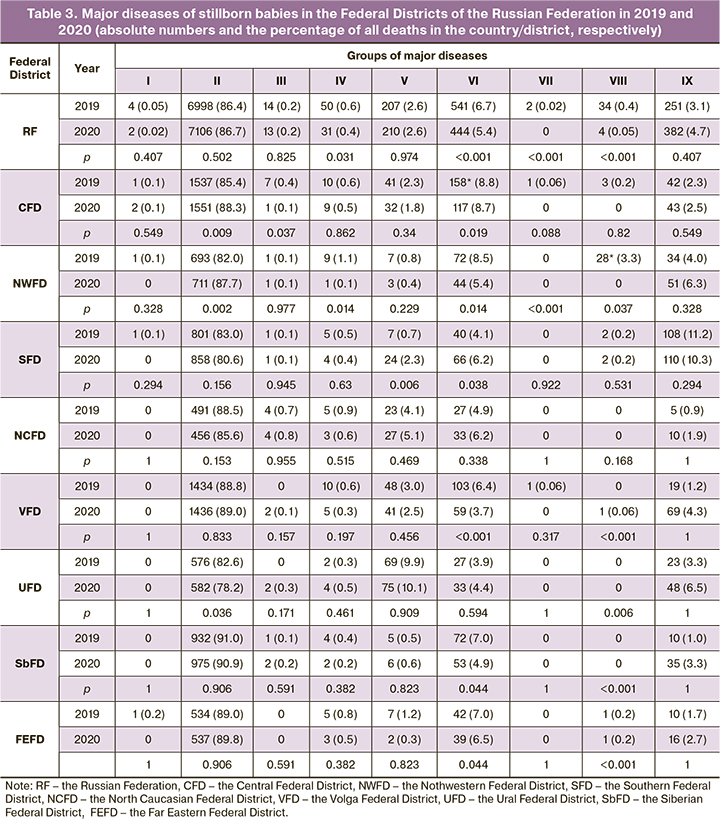
Analyzing stillbirth, it is important to determine the causes of death (Tables 3, 4). Usually, the most common causes of stillborn babies are respiratory disorders (group II). In 2019, in the whole country, the disorders of this group caused 6998 stillbirths, which accounted for 86.4% of the total number of stillborn babies. In 2020, these disorders were the causes of 7106 (86.7%) stillbirths. It means that in 2020, the absolute number of stillbirths due to respiratory disorders increased by 1.5%. In addition, in 2020, the stillbirth rate as a result of respiratory disorders (4,92‰) increased by 4.7% versus 2019 (4.70‰).
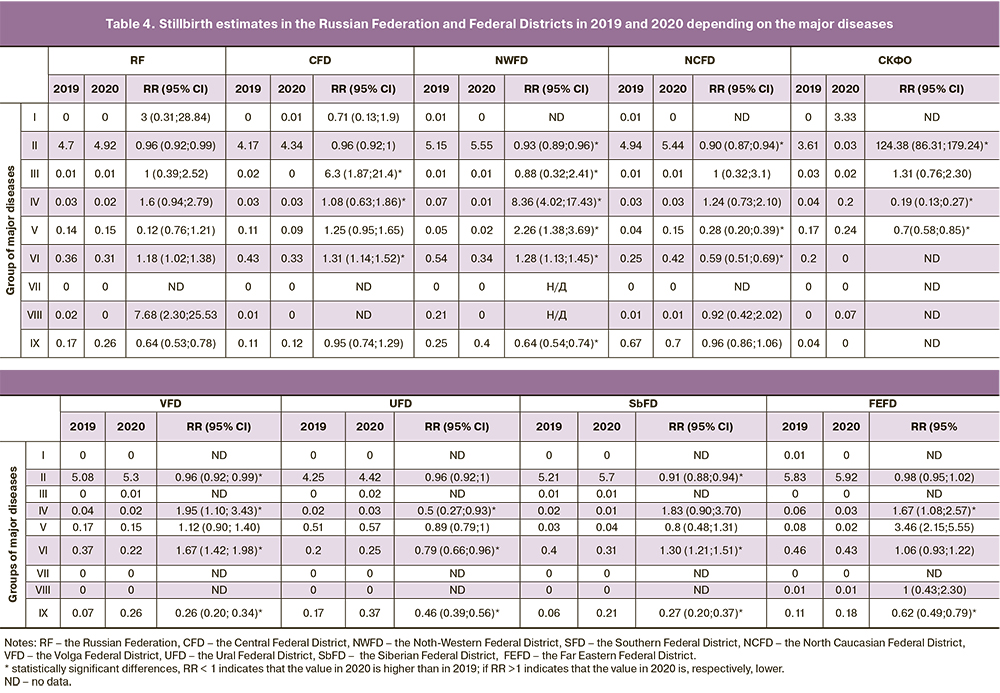
In study periods, among the group of respiratory disorders, the highest rate among all initial causes of death accounted for fetal hypoxia. In 2019, it was registered in 6338 cases of stillbirth and accounted for 78.2% of all cases of stillbirth. In 2020, the number of such cases increased up to 6598 (by 4.1% versus 2019, р<0.001), and reached 80.5% of total number of stillborn babies. Intrapartum fetal hypoxia ranked second among the causes of death. It was diagnosed in 544 stillbirths (6.7% of all stillborn babies) and 409 (5.0%) in 2019 and 2020, respectively (р<0.001). Moreover, congenital pneumonia was registered as the major disease among the respiratory disorders in 22 and 27 stillborn babies in 2019 and 2020, respectively. This means that in 2020, the percentage of congenital pneumonia as the initial cause of death increased by 22.7% (p=0.499).
The diseases included in the group of congenital anomalies (group IV) ranked second among the initial causes of stillbirths in the Russian Federation (Tables 3, 4). In 2019 they were registered in 541 cases (6.7% of all cases of stillbirth), in 2020 they were less often: in 444 cases (5,4% of all cases of stillbirth) (р<0.001). Most often, the conditions that were included in the subgroup of the so-called “other types of congenital anomalies”, including multiple congenital malformations, were represented as the major disease. In 2019 and 2020, these congenital anomalies were registered as the major disease in 204 cases (2.5% of all stillborn babies) and 181 cases (2.2%), respectively. Congenital heart defects ranked second in the incidence rate among the group of congenital anomalies in both study years: in 75 cases (13.9% of all congenital anomalies) as the major disease, and 0.9% of total number of stillborn babies in 2019; and 72 cases (16.2% and 0.9% of all congenital anomalies and all stillborn babies, respectively) in 2020.
Endocrine, metabolic and other pathologies, specific for neonatal period (group V) ranked third and reached 2.6% of total number of stillborn babies.
It should be noted, that infectious diseases as the initial cause of death were detected only in 14 and 13 cases in 2019 and 2020, respectively. In addition, there was no a separate category for records of the number of stillborn babies due to COVD-19 in the Rosstat statistical forms. For this reason, it was not possible to assess the role of COVID-19 in stillbirth. According to the existing rule for filling in these forms, as well as recommendations of the WHO and the Ministry of Health of Russia [11], the cases of COVID-19 (ICD-10 U07.1,2) should be included in the category “Other causes of fetal death” (group VIII). In 2019, 34 cases of stillbirth were included in this category, and only 4 cases in 2020.
At the same time, it is noteworthy that the number of stillborn babies with unknown cause of death increased by 52.2% (382 cases, 4.7% of total number of stillborn babies) in 2020 versus 2019 г. (251 cases, 3.1% of total number of stillborn babies) (р<0.001).
The analysis of the groups of major diseases that caused stillbirth (Tables 3, 4) showed that significant difference between the rates in different Federal Districts. So, in 2019, the rate of respiratory disorders as the most common cause of death of stillborn babies varied from 82.0% in the Nothwestern Federal District to 91.0% in the Siberian Federal District. At the same time, stillbirth rates due to respiratory disorders varied from 3.61‰ in the North Caucasian Federal District to 5.83‰ in the Far Eastern Federal District.
In 2020, the proportion of respiratory disorders fluctuated from 80.6% in the Southern Federal District up to 90.7% in the Siberian Federal District. At the same time, the stillbirth rates due to respiratory disorders increased in 2020 versus 2019 in all Federal Districts, except for the North Caucasian Federal District. The most significant increase in the rates of stillbirth due to respiratory disorders was in the Southern Federal District (by 10.1%) and in the Siberian Federal District (by 9.4%). In the North Caucasian Federal District, stillbirth rates reduced by 7.8% in 2020 versus 2019 (Fig. A).
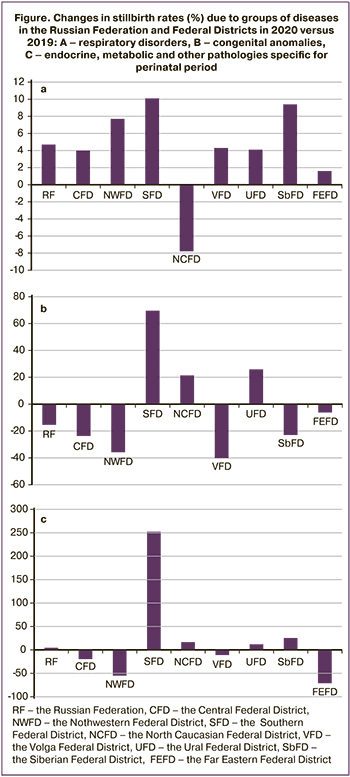
In 2019, the ratio of congenital anomalies, that ranked second in the country among the causes of stillbirths, varied from 3.9% in the Ural Federal District to 8.9% in the Central Federal District. At the same time, the the rates of stillbirth due to congenital anomalies varied from 0.20‰ in the Ural Federal District to 0.54‰ in the Northwestern Federal District. In 2020, the rates of stillbirth due to congenital anomalies increased in the Southern Federal District (by 69.6%), in the Ural Federal District (by 25.9%) and in the North-Caucasian Federal District (by 21.4%) versus the year 2019. In other Districts these values decreased from 40.3% in the Volga Federal District to 6.2% in the Far Eastern Federal District (Fig. B). It is noteworthy that in Ural Federal District, congenital anomalies in the studied years ranked third among the causes of stillbirth. The group of endocrine, metabolic and other pathologies specific for perinatal period ranked second, and their ratio was 9.9% and 10.1% in 2019 and 2020, respectively.
In other Federal Districts the ratio of endocrine, metabolic and other pathologies specific for perinatal period varied from 0.5% in the Siberian Federal District to 4.1% in the North-Caucasian Federal District in 2019, and from 0.4% in the Northwestern Federal District to 5.1% in the North-Caucasian Federal District in 2020.
At the same time, stillbirths associated with this group of diseases increased in the Southern, North-Caucasian, Ural and Siberian Federal Districts in 2020 versus 2019 and decreased in the Central, Northwestern, Volga and Far Eastern Federal Districts. Most significant increase in stillbirths (by 252.4%) was registered in the Southern Federal District, and reduction by 71.1% was in the Far Eastern Federal District (Fig. C).
Also, it should be noted, that in 2020 the absolute number of stillborn babies with unknown cause of death increased versus 2019. The highest rates of the total number of stillbirths were in the Southern Federal District: 11.2% and 10.3% in 2019 and 2020, respectively.
Therefore, both the absolute number of stillborn babies and stillbirth rates increased in the Russian Federation in 2020 versus 2019. Most significant increase was in the Southern and Siberian Federal Districts.
The available published data on stillbirths in the period of COVID-19 pandemic are based both on the data provided by some healthcare facilities and the analysis of national (state) registers.
Thus, the analysis of stillbirths in St George’s University Hospital (London, UK) by A. Khalil et al. [12] found that the rate of stillbirths increased by 3.9 times in the period from February 1, 2020 to June 14, 2020 compared to the previous 4 months (from October 1, 2010 to January 31, 2020), when no cases of COVID-19 were registered (9.31 versus 2.38 per 1000 births, p=0.01). As it is known, stillbirth is defined as fetal death at 24 or more completed weeks of gestation in the United Kingdom. At the same time, all pregnant women who had stillbirths, had no the symptoms of COVID-19, and post-mortem examination of the bodies of stillborn babies and placentas showed no signs of SARS-CoV-2 infection [12].
Similar increase of stillbirth rate by 4 times (from 0.1% to 0.4‰, p=0.037) was observed in Shamir Medical Center (Zerifin, Israel) from February 21, 2020 (the date of first diagnosed case of COVID-19 infection in Israel) to April 30, 2020, versus the same period in the previous 3 years (2017–2019) [13].
A threefold increase in stillbirths during the lockdown period (March-May, 2020) (3.23‰) compared to the same period in 2019 (1.07‰), was noted in Lazio, the administrative region of Italy. The capital of this region is Rome, where about 10% of all births take place in Italy [14]. The authors reported [14] that the study was limited by its retrospective nature and lack of information on the causes of stillbirth. In this regard, the authors concluded that increased stillbirth was a result of lifestyle changes due to lockdown, in particular, reduction in follow-up visits to clinics because of fear to be infected with SARS-CoV-2 and suspension of medical examination of pregnant women.
V. Kumari et al. stick to similar opinion [15]. They reported a significant increase in the proportion of stillbirths (3.15% versus 2.25%; p=0.02) in 4 hospitals in West India after anti-COVID-19 restrictions were introduced (March 25–June 2, 2020) compared to the control period 10 weeks prior to lockdown (January 15–March 24, 2020). Moreover. The authors point out that a significant reduction in hospital admission of pregnant women for delivery to a third level hospitals in the lockdown period was due to the public transport shutdown, and most pregnant women in India used public transportation to hospital for emergency visits to hospital.
Other Indian researchers reported similar causes of increased stillbirths in the period of COVID-10 [16]. They analyzed pregnancy outcomes in the period from March to September, 2020, versus the period from March to September 2019, when a significant increase was in the rate of stillbirths – 37.4‰ versus 29.9‰ (p=0.045).
K.A. Ashish et al. [17] reported the increased number of stillbirths by в 1.5 times (from 14 to 21 per 1000 of all newborns, p=0.0002) in 9 healthcare facilities in Nepal during 9.5 weeks of the lockdown period (from March 21 to May 30, 2020) compared to 12.5 weeks before isolation (from January 1 to March 2020). It should be noted that Nepal is one of the countries, that is characterized by annual success in reduction of both maternal and perinatal mortality [18]. The main reasons for the increased stillbirth during COVID-19 lockdown are delays in qualified healthcare due to movement restrictions and lack of health workers in the study medical institutions.
The studies, that showed no differences or even reductions in stillbirth rates, came under our notice. Thus, J. Stowe et al. [19] analyzed the annual statistics data on hospitalizations in the UK related to stillbirths during isolation period due to COVID-19 from March 23 to June 23, 2020, and the same period in 2019. In 2019, before COVID-19 occurrence in patients, 565 stillbirths were registered throughout England, and the ratio of stillbirth was 0.40%. During the lockdown period in England from March 23 to June 23, 2020, the number of stillbirths reduced (n=543), but the ratio of stillbirth (0.41%) slightly increased versus 2019 (p=0.69). This means, that according to the authors [19], the number of stillbirths has not changed during COVID-10 pandemic.
According to L. Gallo et al. [20], no statistical difference was between the annual stillbirth rates for singleton pregnancies in the period from March 16 to May 01, 2013 up to the pandemic year 2020 in Brisbane (the third largest city in Queensland state, Australia).
The analysis of stillbirths in Chaim Sheba Medical Center providing healthcare services for the citizens of Ramat Gan and the Central District of Israel, and in Mpilo Central Hospital in Bulawayo (the second largest city in Zimbabwe) showed no significant differences [22].
Stillbirths in Chaim Sheba Medical Center were analyzed during 3 periods: 1st period was from March 20, 2020 (the date of starting isolation regime) to June 27, 2020; the 2nd period included the same dates in 2019, and the 3rd period with the same dates in years 2011–2019. During these periods 22 (0.80%), 22 (0.80%) and 290 (1.0%) stillbirths were registered [21]. In Mpilo Central Hospital, where 8000–10000 deliveries take place per year, the analysis of all births 3 months before and after isolation regime was performed. The average number of births per month (681.0±17.6) and stillbirths (30.9±4.6‰) reduced during isolation period compared to the period before isolation (747.3±61.3, p=0.20) and (33.1±4.8‰, p=0.81), respectively [22]. According to the authors of the article [22], reduction in stillbirths in the last case was associated with the structure and system of activities in the maternity ward aimed at early detection and treatment of pathologies even in pandemic.
Of particular note are the studies that showed significant reduction in stillbirth. So, B. Pasternak et al. [23] made a comparative analysis of stillbirths from April 1 to May 31, 2020, when restriction measures were used in Sweden due to COVID-19 pandemic, and in the period from April to May 2015–2019. According to the data in the Swedish Pregnancy Register of pregnancies, 17661 live births and 47 stillbirths were registered in the study pandemic period. In the same periods in 2015–2019 the total number of 91262 live births and 303 stillbirths occurred. Accordingly, the stillbirth ratio decreased by 18.2% (from 3.3. to 2.7 per 1,000 newborns), respectively.
The above noted differences in stillbirth rates were also reflected in meta-analyses. The systematic review and meta-analysis by B. Chmielewska et al. [24] was based on 12 publications from January 2020 to January 08, 2021 available in international data bases Medline and Embase. Based on the meta-analysis of pooled outcomes of 198 993 pregnancies before and 165 295 pregnancies during COVID-19 pandemic, the authors found a significant increase in stillbirths. (OR 1.28, 95% CI 1.07–1.54).
Meta-analysis of pregnancy outcomes and conditions in newborns presented in 21 articles in the English language before May 2021 and available in data bases PubMed and Embase, was conducted by J. Yang et al. [25]. These articles contained information on 237 381 pregnant women in the pandemic period from 4 weeks to 7 months and 633 050 pregnant women in the period before pandemic, that varied form 2 months to 19 years. The authors reported no significant difference between the stillbirth rates (unadjusted odds ratio [uaOR] 1.08, 95% CI 0.95–1.23, I2=62%) [25].
Meta-analysis of articles in the English language before July 2021 by C.Vaccaro et al. [26] available in Embase, CORD-19, LitCovid (PubMed), WHO Global research on corona virus disease (COVID-19) and MedRxiv showed, that the total number of stillbirths was 901 among 150 219 newborns during COVID-19 isolation period and 1279 stillbirths among 234 187 newborns before isolation. The authors calculated that COVID-19 isolation was characterized by a higher risk of stillbirth compared to pre-isolation period (RR 1.33, 95% CI 1.04–1.69) [26].
This means that available published data contain information both on increase and reduction in stillbirth during COVID-10 pandemic. It seems that there are several underlying reasons behind these differences. The first reason is the difference between the objects of study: one or several medical institutions in one country, regional or national (state) registry. The second reason is the difference in isolation regimes and organization of healthcare for pregnant and puerperant women in different countries during lockdown. The third reason is the difference in determining the gestational age of stillborn babies: 20 weeks or more [16, 25], 22 weeks or more [14, 17, 23] and not less than 24 weeks [12, 19]. The period of time, which is compared with the data in the period of isolation or restriction (a certain period is 2019, the whole year 2019, or several previous years) is of importance. In our opinion, it is more correct to compare the data for the whole years 2020 and 2019, since a longer period especially for several years will reflect the dynamics of the annual decline in stillbirth rates in most countries including the Russian Federation [27].
Nevertheless, most available published data refer to a rise in stillbirth. Unfortunately, almost all these publications do not contain information on the major diseases (initial causes of death) and conditions of stillborn babies that contributed to their death. Apparently, this is why the main reasons for a rise in stillbirths are not diseases, but social and organizational measures, in particular, restrictions on movement of the population during lockdown, and reduced availability for pregnant women to visit healthcare institutions, due to fear of SARS-CoV-2 infection [13, 16, 25].
Only some authors reported on the detected pathologies. So, D.A. Schwartz et al. [28] reported on 5 miscarriages and stillbirths with PCR test results positive for SARS-CoV-2, and all placentas had the signs of chronic intervillositis and necrosis in syncytiotrophoblast. Moreover, in about half of cases of stillbirths during the isolation period (from February 21 to April 30, 2020) and the same period in the previous three years, M. Mor et al. [13] found morphological signs of placental insufficiency, that undoubtedly plays a significant, and potentially a leading role in thanatogenesis.
Indeed, according to literature [29, 30] in pregnant women with SARS-CoV-2 infection, placental lesions were observed in the form of inflammatory reactions and disorders of maternal and fetal circulatory compartments. Previously, our morphometric and immunohistochemical analysis of placentas in peurperant women with COVID-19 found an increase in the number of syncytial nodules, decrease in the degree of vascularization, and increase in VEGF (vascular endothelial growth factor) expression in the villi, that indicated development of pre-existing and placental hypoxia [31, 32].
Additionally, it should be noted that M. Mor et al. [13] found that stillbirths increased by 4 times in Shamir Medical Center (Zerifin, Israel) in the presence of placental lesions and PCR-negative test results for SARS-CoV-2 in stillborn babies. Similar data on placental lesions, as well as Rosstat data on changes in the structure of stillbirth causes in 2020 (the year of the COVID-19 pandemic), indicate the need for a comprehensive clinical and anatomical analysis of all cases of stillbirth. Moreover, placental lesions may also underlie our previously reported increase in the proportion of respiratory disorders, including congenital pneumonia, and infections, including congenital sepsis, among the causes of newborn deaths, who died within the first 168 hours of life in the Russian Federation in 2020 [27].
Conclusion
Thus, according to Rosstat data, increase in the absolute number of stillbirths by 1.1% and stillbirth rate by 4.2% in 2020 (COVID-19 pandemic year) versus 2019 was noted. Analysis of causes of death showed that the proportion of diseases included in the group of respiratory disorders, in particular, fetal hypoxia increased by 4.1% and congenital pneumonia by 22.7%, as well as the number of stillbirths with unknown cause of death increased by 52.2%. At the same time the number of congenital anomalies, which were registered as the major disease, reduced by 17.9%. No data on stillbirths due to COVID-19 were found in Rosstat statistical forms “A-05” in 2020. Accordingly, to indentify a direct or indirect impact of SARS-CoV-2 infection on fetal death and stillbirth, it is necessary to perform detailed clinical and morphological assessment.
References
- Li J., Huang D.Q., Zou B., Yang H., Hui W.Z., Rui F. et al. Epidemiology of COVID-19: A systematic review and meta-analysis of clinical characteristics, risk factors, and outcomes. J. Med. Virol. 2021; 93(3): 1449-58. https://dx.doi.org/10.1002/jmv.26424.
- Wolff D., Nee S., Hickey N.S., Marschollek M. Risk factors for Covid-19 severity and fatality: a structured literature review. Infection. 2021; 49(1): 15-28. https://dx.doi.org/10.1007/s15010-020-01509-1.
- Schwartz D.A., Graham A.L. Potential maternal and infant outcomes from coronavirus 2019-nCoV (SARS-CoV-2) infecting pregnant women: lessons from SARS, MERS, and other human coronavirus infections. Viruses. 2020; 12(2): 194. https://dx.doi.org/10.3390/v12020194.
- Vivanti A.J., Vauloup‑Fellous C., Prevot S., Zupan V., Suffee C., Do Cao J. et al. Transplacental transmission of SARS‑CoV‑2 infection. Nat. Commun. 2020; 11(1): 3572. https://dx.doi.org/10.1038/s41467-020-17436-6.
- Sukhikh G., Petrova U., Prikhodko A., Starodubtseva N., Chingin K., Chen H., Bugrova A., Kononikhin A., Bourmenskaya O., Brzhozovskiy A., Polushkina E., Kulikova G., Shchegolev A., Trofimov D., Frankevich V., Nikolaev E., Shmakov R. Vertical transmission OF SARS-COV-2 in second trimester associated with severe neonatal pathology. Viruses. 2021; 13(3): 447. https://dx.doi.org/10.3390/v13030447.
- Raschetti R., Vivanti A.J., Vauloup-Fellous C., Loi B., Benachi A., De Luca D. Synthesis and systematic review of reported neonatal SARS-CoV-2 infections. Nat. Commun. 2020; 11(1): 5164. https://dx.doi.org/10.1038/s41467-020-18982-9.
- Щеголев А.И., Туманова У.Н., Шувалова М.П., Фролова О.Г. Гипоксия как причина мертворождаемости в Российской Федерации. Здоровье, демография, экология финно-угорских народов. 2014; 3: 96-8. [Shchegolev A.I., Tumanova U.N., Shuvalova M.P., Frolova O.G. Hypoxia as a cause of stillbirth in the Russian Federation. Zdorov'e, demografija, jekologija finno-ugorskih narodov/ Health, demography, ecology of Finno-Ugric peoples. 2014; 3: 96-8. (in Russian)].
- Щеголев А.И., Туманова У.Н., Шувалова М.П. Преждевременная отслойка плаценты в генезе мертворождения. Международный журнал прикладных и фундаментальных исследований. 2016; 7-4: 575-9. URL: https://applied-research.ru/ru/article/view?id=9878 (дата обращения: 04.02.2022). [Shchegolev A.I., Tumanova U.N., Shuvalova M.P. Premature abruptio placentae as the cause of stillbirth. Mezhdunarodnyj zhurnal prikladnyh i fundamental'nyh issledovanij/ International Journal of Applied and Basic Research. 2016; 7-4: 575-9. (in Russian)].
- Туманова У.Н., Шувалова М.П., Щеголев А.И. Предлежание плаценты в генезе мертворождения (по данным Росстата в 2012–2016 годах). Международный журнал прикладных и фундаментальных исследований. 2018; 3: 81-5. [Tumanova U.N., Shuvalova M.P., Shchegolev A.I. Placenta previa in the genesis of stillbirth (according to Rosstat in 2012–2016). Mezhdunarodnyj zhurnal prikladnyh i fundamental'nyh issledovanij/ International Journal of Applied and Basic Research. 2018; 3: 81-5. (in Russian)]. https://dx.doi.org/10.17513/mjpfi.12153.
- Щеголев А.И., Туманова У.Н., Фролова О.Г. Региональные особенности мертворождаемости в Российской Федерации. В кн.: Крупнов Н.М., ред. Актуальные вопросы судебно-медицинской экспертизы и экспертной практики в региональных бюро судебно-медицинской экспертизы на современном этапе. Рязань; 2013: 163-9. [Shchegolev A.I., Tumanova U.N., Frolova O.G. Regional features of stillbirth in the Russian Federation. In: Krupnov N.M., ed. Topical issues of forensic medical examination and expert practice in the regional bureaus of forensic medical examination at the present stage. Ryazan; 2013: 163-9. (in Russian)].
- Методические рекомендации по кодированию и выбору основного состояния в статистике заболеваемости и первоначальной причины в статистике смертности, связанных с COVID-19. М.; 2020. 24с. [Methodological recommendations for coding and selecting the underlying condition in morbidity statistics and the initial cause in mortality statistics related to COVID-19. M.; 2020. 24 p. (in Russian)]. Available at: https://static-1.rosminzdrav.ru/system/attachments/attaches/000/050/527/original/27052020_MR_STAT_1.pdf
- Khalil A., von Dadelszen P., Draycott T., Ugwumadu A., O'Brien P., Magee L. Change in the incidence of stillbirth and preterm delivery during the COVID-19 pandemic. JAMA. 2020; 324(7): 705. https://dx.doi.org/10.1001/jama.2020.12746.
- Mor M., Kugler N., Jauniaux E., Betser M., Wiener Y., Cuckle H. et al. Impact of the COVID-19 pandemic on excess perinatal mortality and morbidity in Israel. Am. J. Perinatol. 2021; 38(4): 398-403. https://dx.doi.org/10.1055/s-0040-1721515.
- De Curtis M., Villani L., Polo A. Increase of stillbirth and decrease of late preterm infants during the COVID-19 pandemic lockdown. Arch. Dis. Child. Fetal Neonatal Ed. 2021; 106(4): 456. https://dx.doi.org/10.1136/archdischild-2020-320682.
- Kumari V., Mehta K., Choudhary R. COVID-19 outbreak and decreased hospitalisation of pregnant women in labour. Lancet Glob. Health. 2020; 8(9): e1116-7. 10. https://dx.doi.org/1016/S2214-109X(20)30319-3.
- Kumar M., Puri M., Yadav R., Biswas R., Singh M., Chaudhary V. et al. Stillbirths and the COVID-19 pandemic: Looking beyond SARS-CoV-2 infection. Int. J. Gynecol. Obstet. 2021; 153: 76-82. https://dx.doi.org/10.1002/ijgo.13564.
- Ashish K.A., Gurung R., Kinney M.V., Sunny A.K., Moinuddin M., Basnet O. et al. Effect of the COVID-19 pandemic response on intrapartum care, stillbirth, and neonatal mortality outcomes in Nepal: a prospective observational study. Lancet Glob. Health. 2020; 8(10): e1273-81. https://dx.doi.org/10.1016/S2214-109X(20)30345-4.
- McMahon S.A., Ho L.S., Brown H., Miller L., Ansumana R., Kennedy C.E. Healthcare providers on the frontlines: a qualitative investigation of the social and emotional impact of delivering health services during Sierra Leone’s Ebola epidemic. Health Policy Plan. 2016; 31(9): 1232-9. https://dx.doi.org/10.1093/heapol/czw055.
- Stowe J., Smith H., Thurland K., Ramsay M.E., Andrews N., Ladhani S.N. Stillbirths during the COVID-19 pandemic in England, April-June 2020. JAMA. 2020; 325(1): 86-7. https://dx.doi.org/10.1001/jama.2020.21369.
- Gallo L.A., Gallo T.F., Borg D.J., Moritz K.M., Clifton V.L., Kumar S. A decline in planned, but not spontaneous, preterm birth rates in a large Australian tertiary maternity centre during COVID-19 mitigation measures. Aust. N. Z. J. Obstet. Gynaecol. 2021 Jul 12; https://dx.doi.org/10.1111/ajo.13406. 10.1111/ajo.13406.
- Meyer R., Bart Y., Tsur A., Yinon Y., Friedrich L., Maixner N. et al. A marked decrease in preterm deliveries during the coronavirus disease 2019 pandemic. Am. J. Obstet. Gynecol. 2021; 224(2): 234-7. https://dx.doi.org/10.1016/j.ajog.2020.10.017.
- Shakespeare C., Dube H., Moyo S., Ngwenya S. Resilience and vulnerability of maternity services in Zimbabwe: a comparative analysis of the effect of Covid-19 and lockdown control measures on maternal and perinatal outcomes, a single-centre cross-sectional study at Mpilo Central Hospital. BMC Pregnancy Childbirth. 2021; 21(1): 416. https://dx.doi.org/10.1186/s12884-021-03884-5.
- Pasternak B., Neovius M., Söderling J., Ahlberg M., Norman M., Ludvigsson J.F. Preterm birth and stillbirth during the COVID-19 pandemic in Sweden: A Nationwide Cohort Study. Ann. Intern. Med. 2021; 174(6): 873-5. https://dx.doi.org/10.7326/M20-6367.
- Chmielewska B., Barratt I., Townsend R., Kalafat E., van der Meulen J., Gurol-Urganci I. Effects of the COVID-19 pandemic on maternal and perinatal outcomes: a systematic review and meta-analysis. Lancet Glob. Health. 2021; 9(6): e759-72. https://dx.doi.org/10.1016/S2214-109X(21)00079-6.
- Yang J., D'Souza R., Kharrat A., Fell D.B., Snelgrove J.W., Murphy K.E. et al. COVID-19 pandemic and population-level pregnancy and neonatal outcomes: a living systematic review and meta-analysis. Acta Obstet. Gynecol. Scand. 2021; 100(10): 1756-70. https://dx.doi.org/10.1111/aogs.14206.
- Vaccaro C., Mahmoud F., Aboulatta L., Aloud B., Eltonsy S. The impact of COVID-19 first wave national lockdowns on perinatal outcomes: a rapid review and meta-analysis. BMC Pregnancy Childbirth. 2021; 21(1): 676. https://dx.doi.org/10.1186/s12884-021-04156-y.
- Туманова У.Н., Щеголев А.И., Чаусов А.А., Шувалова М.П. Анализ причин ранней неонатальной смертности в Российской Федерации в 2020 году (год пандемии COVID-19). Вестник Российского государственного медицинского университета. 2021; 5: 76-83. [Tumanova U.N., Shchegolev A.I., Chausov A.A., Shuvalova M.P. Analysis of causes of early neonatal mortality during covid-19 pandemic in 2020 in Russia. Bulletin of Russian State Medical University. 2021; 5: 76-83. (in Russian)]. https://dx.doi.org/10.24075/brsmu.2021.045.
- Schwartz D.A., Baldewijns M., Benachi A., Bugatti M., Collins R.R.J., De Luca D. et al. Chronic histiocytic intervillositis with trophoblast necrosis is a risk factor associated with placental infection from coronavirus disease 2019 (COVID-19) and intrauterine maternal-fetal severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) transmission in live-born and stillborn infants. Arch. Pathol. Lab. Med. 2021; 145(5): 517-8. https://dx.doi.org/10.5858/arpa.2020-0771-SA.
- Oltean I., Tran J., Lawrence S., Ruschkowski B.A., Zeng N., Bardwell C. et al. Impact of SARS-CoV-2 on the clinical outcomes and placental pathology of pregnant women and their infants: A systematic review. Heliyon. 2021; 7(3): e06393. https://dx.doi.org/10.1016/j.heliyon.2021.e06393.
- Щеголев А.И., Туманова У.Н., Серов В.Н. Поражения плаценты у беременных с SARS-CoV-2-инфекцией. Акушерство и гинекология. 2020: 12: 44-52. [Shchegolev A.I., Tumanova U.N., Serov V.N. Placental lesions in pregnant women with SARS-COV-2 infection. Akusherstvo i ginekologiya/ Obstetrics and Gynecology. 2020; 12: 44-52. (in Russian)]. https://dx.doi.org/10.18565/aig.2020.12.44-52.
- Shchegolev A.I., Kulikova G.V., Tumanova U.N., Shmakov R.G., Sukhikh G.T. Morphometric parameters of placental villi in parturient women with COVID-19. Bull. Exp. Biol. Med. 2021; 172(1): 85-9. https://dx.doi.org/10.1007/s10517-021-05337-7.
- Shchegolev A.I., Kulikova G.V., Lyapin V.M., Shmakov R.G., Sukhikh G.T. The number of syncytial knots and vegf expression in placental villi in parturient woman with COVID-19 depends on the disease severity. Bull. Exp. Biol. Med. 2021; 171(3): 399-403. https://dx.doi.org/10.1007/s10517-021-05236-x.
Received 13.12.2021
Accepted 13.01.2022
About the Authors
Alexander I. Shchegolev, Dr. Med. Sci., Professor, Head of the 2nd Pathology Department, Academician V.I. Kulakov National Medical Research Center for Obstetrics, Gynecology and Perinatology, Ministry of Health of Russia, ashegolev@oparina4.ru, https://orcid.org/0000-0002-2111-1530, 117997, Russia, Moscow, Oparina str., 4.Uliana N. Tumanova, Ph.D. in medical sciences, Leading Researcher at the 2nd Pathology Department, Academician V.I. Kulakov National Medical Research Center for Obstetrics, Gynecology and Perinatology, Ministry of Health of Russia, u.n.tumanova@gmail.com, https://orcid.org/0000-0002-0924-6555,
117997, Russia, Moscow, Oparina str., 4.
Andrey A. Chausov, Head of the Information and Analytical Center of the Department of Regional Cooperation and Integration, Academician V.I. Kulakov National Medical Research Center for Obstetrics, Gynecology and Perinatology, Ministry of Health of Russia, a_chausov@oparina4.ru, https://orcid.org/0000-0002-3094-7209,
117997, Russia, Moscow, Oparina str., 4.
Marina P. Shuvalova, Ph.D. in medical sciences, Associate Professor, Deputy Director – Head of the Department of Regional Cooperation and Integration,
Academician V.I. Kulakov National Medical Research Center for Obstetrics, Gynecology and Perinatology, Ministry of Health of Russia, m_shuvalova@oparina4.ru,
https://orcid.org/0000-0002-6361-9383, 117997, Russia, Moscow, Oparina str., 4.
Authors' contributions: Shchegolev A.I. – design of the study, Rosstat data analysis and synthesis, analysis of published scientific papers, article editing; Tumanova U.N. – Rosstat data analysis, review and analysis of published scientific papers, article writing; Chausov A.A. – Rosstat data analysis and processing; Shuvalova M.P. – Rosstat data analysis, article editing.
Conflicts of interest: The authors declare that they have no conflict of interests regarding this publication.
Funding: The study was carried out without any sponsorship.
Authors' Data Sharing Statement: The data supporting the findings of this study are available on request from the corresponding author after approval from the principal investigator.
For citation: Shchegolev A.I., Tumanova U.N., Chausov A.A., Shuvalova M.P. Comparative analysis of stillbirth causes and rates in the Russian Federation in 2019 and 2020
Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2022; 2: 80-90 (in Russian)
https://dx.doi.org/10.18565/aig.2022.2.80-90