Maternal mortality in the Far Eastern Federal District during the pre-epidemic period and three years of the COVID-19 pandemic
Belokrinitskaya T.E., Shmakov R.G., Frolova N.I., Brum O.Yu., Krivoshchekova N.A., Pavlova T.Yu., Rinchindorzhiyeva M.P.
Objective: This study aimed to evaluate the structure and indicators of maternal mortality (MM) in the Far Eastern Federal District (FEFD) during the pre-epidemic period and the first three years of the novel coronavirus infection (NCI) pandemic.
Materials and methods: A retrospective comparative analysis of the dynamics of the MM indicators and structure in FEFD for the years 2019–2022 was conducted. A statistical database was generated from the emergency notification cards of the MM cases. In all cases of maternal loss from COVID-19, SARS-CoV-2 was identified by PCR in the nasopharyngeal material.
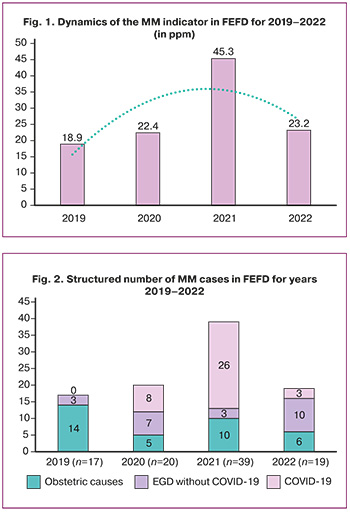
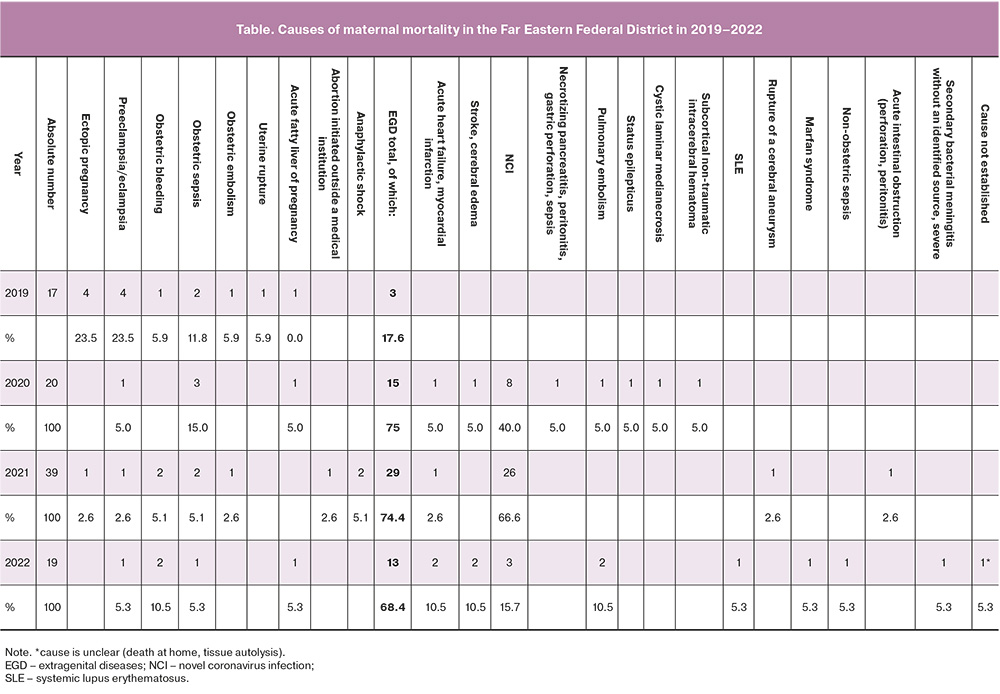
Results: The dynamics of the MM rate in FEFD during the reported period showed trends similar to those of the all-Russian rate. However, the MM rate exceeded the all-Russian rate by 18.9‰ (RF 9.8‰) in 2019, by 22.4‰ (RF 16.3‰) in 2020, by 45.3‰ (RF 42.4‰) in 2021, and by 23.2‰ (RF 12.6‰) in 2022. In the pre-epidemic year 2019, obstetric causes accounted for the largest proportion (82.4%), whereas the proportion of extragenital diseases (EGD) was significantly lower at 17.6% (χ2=11.8; p<0.001). In the first year of the COVID-19 pandemic (2020), MM increased owing to a significant increase in EGD mortality from 17.6% in 2019 to 75.0% (χ2=9.9; p=0.002), of which NCI accounted for a large proportion (40.0%). Maternal mortality from non-communicable diseases increased 2.0-fold: 17.6% (2019) vs. 35.0% (2020), indicating organizational challenges in the care of patients with EGD. The proportion of obstetric causes of MM decreased from 82.4% to 25.0% (χ2=9.9, p=0.002). In the second year of the epidemic, there was a 2.0-fold increase in MM due to a multiple of COVID-19 maternal losses: 66.6% (2021) vs. 40.0% (2020) (χ2=3.9; p=0.050), driven by the greater pathogenicity of the delta strain. The proportion of obstetric causes of MM did not change significantly: 20.5% (2021) vs. 25.0% (2020), p=0.951, but there was a 1.5-fold increase in the number of female villagers (43.6% vs. 30%). In the third year of the pandemic, EGDs remained the leading cause of MM, with no significant change in their proportion: 68.4% (2022) vs. 66.6% (2021), p=0.870. Notably, there was a significant decrease in the proportion of MM cases from the NCI (15.7 % (2022) vs. 66.6 % (2021), p<0.001), while there was a significant increase in the number of losses from severe non-infectious EGD. None of these pregnant and postpartum women had been examined by a specialist prior to pregnancy and had received no pre-pregnancy care. There was late seeking of medical attention and, in some cases, underestimation of severity and clinical symptoms in primary health care settings and by allied specialists.
Conclusion: The dynamics and structure of MM in FEFD, as revealed in this study, underscore the need for management decisions aimed at improving the current system of medical examination of fertile-age patients and routing of pregnant women who are at risk of developing critical obstetric conditions.
Authors' contributions: Belokrinitskaya T.E., Shmakov R.G. – conception and design of the study; Brum O.Yu.,
Krivoshchekova N.A., Pavlova T.Yu., Rinchindorzhiyeva M.P. – data collection and analysis; Frolova N.I. – statistical analysis; Belokrinitskaya T.E., Frolova N.I. – drafting of the manuscript; Shmakov R.G. – editing of the manuscript.
Conflicts of interest: The authors have no conflicts of interest to declare.
Funding: There was no funding for this study.
Acknowledgements: We gratefully acknowledge the specialists of the Maternal and Child Health Protection Divisions of the Departments and Ministries of Health of the FEFD subjects for providing timely information: N.Y. Vladimirova, J.B. Vasilieva (Khabarovsk), O.V. Vanchikova (Petropavlovsk-Kamchatsky), N.V. Dyachek (Magadan), O.N. Kolesova (Yuzhno-Sakhalinsk), T.Yu. Kurleeva, I.V. Artyukhova (Vladivostok), M.E. Stolbova, T.Yu. Stolbova, T.Yu. Radovich (Chukotka AO), E.V. Pastukhova (Jewish AO).
Authors' Data Sharing Statement: The data supporting the findings of this study are available upon request from the corresponding author after approval from the principal investigator.
For citation: Belokrinitskaya T.E., Shmakov R.G., Frolova N.I., Brum O.Yu., Krivoshchekova N.A., Pavlova T.Yu., Rinchindorzhiyeva M.P. Maternal mortality in the Far Eastern Federal District during the pre-epidemic period and three years of the COVID-19 pandemic. Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2023; (11): 87-95 (in Russian)
https://dx.doi.org/10.18565/aig.2023.160
Keywords
According to estimates presented in a report by United Nations agencies on February 23, 2023, a woman dies during pregnancy or childbirth every two minutes. This report highlights an alarming deterioration in women's health, noting increasing or persistent maternal mortality (MM) rates in nearly all global regions. Experts believe that the COVID-19 pandemic may have contributed to the slowdown in maternal health. However, current global evidence is limited to 2020, necessitating further information to fully understand the pandemic's impact on MM [1].
For three years, the world has been grappling with a pandemic of novel coronavirus infection (NCI) caused by the Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2). Originating in December 2019 in Wuhan City, Hubei Province, China, the virus rapidly spread worldwide, posing a major challenge to the most resourceful health systems. Faced with the threat of NCI spread, restrictive quarantine measures took precedence: routine outpatient visits for pregnant women were canceled or postponed, obstetric hospitals were repurposed into infectious disease hospitals, and intensive care units (ICU) were equipped with ventilators. Medical personnel were urgently redeployed and, in some cases, retrained to assist COVID-19 patients [2].
The initial year of the pandemic lacked systematic reviews and meta-analyses on COVID-19 in pregnant women. Scientific literature mainly comprised case series suggesting that the original (Wuhan) strain of SARS-CoV-2 from China did not exhibit heightened tropism toward pregnant, parturient, and postpartum women [3]. During the first year of the pandemic, 27.4% of SARS-CoV-2-infected mothers remained asymptomatic; of those with symptoms, most experienced mild disease (52.7%), with smaller proportions having moderate (16.6%), severe (2.5%), or extremely severe (0.5%) cases. The incidence of invasive mechanical ventilation (IVP) was lower in this cohort than in the general population (0.48% vs. 1.05%, p<0.001) [4].
Throughout the subsequent years of SARS-CoV-2 circulation, natural mutations in the spike protein have led to the emergence of new genetic variants that significantly alter infectivity, virulence, transmissibility, and tropism across different populations [5–8]. Currently, over 1000 SARS-CoV-2 variants exist, with the WHO recognizing five Variants of Concern (VOC): alpha, beta, gamma, delta, and omicron [8, 9].
Over the three years of the COVID-19 pandemic, information on the morbidity and mortality of pregnant women across countries has accumulated and been organized, revealing an unprecedented increase in MM due to NCI [4, 10, 11].
The Far Eastern Federal District (FEFD), established by the Russian Federation's President on May 13, 2000, initially comprised 9 subjects and expanded to 11 subjects by decree No. 632 on November 3, 2018. It includes 4 oblasts (Amur, Magadan, Sakhalin, and Jewish Autonomous Okrug), 4 krais (Transbaikal, Kamchatka, Primorsky, Khabarovsk), 2 republics (Buryatia, Sakha (Yakutia)), and Chukotka Autonomous Okrug [12]. Covering the largest territory among all Russian Federation federal districts at 40.6%, it boasts the lowest population density at 1.16 people/km² (compared to the Russian Federation's 8.55 people/km² as of January 1, 2023).
The Far East exhibits diverse climates, ranging from arctic and subarctic in the north of Yakutia and Kamchatka, in Magadan Oblast and Chukotka to monsoon climate in Sakhalin, Jewish AO and partially Amur Oblasts, Primorsky and Khabarovsk Krais. This variation stems from the vast expanse from north to south (nearly 4500 km) and from west to east (2500–3000 km), along with the mountainous terrain and permafrost. Cyclones, prolonged heavy rain, typhoons, and fog are common along the coast throughout the year. Kamchatka experiences snow cover of up to a height of 6 m. The summer season results in the highest precipitation levels, often leading to river overflow and floods. Dust storms from Mongolia and northern China have affected the southern and central areas. The abundance of forests and rugged landscapes increased the likelihood of large-scale forest fires.
This study aimed to evaluate the structure and indicators of maternal mortality in the Far Eastern Federal District during both the pre-epidemic period and the initial three years of the novel coronavirus infection pandemic.
Materials and methods
A retrospective comparative analysis of the dynamics of the MM indicator and the structure of the FEFD for the years 2019–2022 was carried out. We did not include indicators before 2019 in the analysis because the Transbaikal Territory and the Republic of Buryatia entered the FEFD only in November 2018 [12].
The statistical database was formed on the basis of "Report Cards on Maternal Deaths" (Form No. 003/u-MM). In all cases of maternal deaths due to COVID-19, SARS-CoV-2 was identified by polymerase chain reaction in nasopharyngeal material [9, 13].
Statistical analysis
Statistical analysis was performed using the IBM SPSS Statistics Version 25.0 software (International Business Machines Corporation, license No. Z125-3301-14, USA). Considering that the numerical variables were not normally distributed, they were reported as the median and interquartile range Me (Q1; Q3). Categorical variables are described as frequencies and percentages. Mathematical analysis included descriptive statistics, assessment of the difference (nature of change) between the studied indicators in the pre-epidemic period and during the three years of the pandemic (delta, ∆), and analysis of contingency tables, where Pearson's χ2 test was used to compare categorical variables. The Yates correction was used when the expected frequencies were between 5 and 10. The values were considered statistically significant with a value of χ2>3.84, at p≤0.05. The strength of association between the studied variables and COVID-19 was estimated using the odds ratio (OR). Confidence intervals (CI) were calculated for a confidence level of p=95%.
Results and discussion
The dynamics of the MM rate in FEFD during the reported period showed trends similar to those of the all-Russia rate. However, the MM rate exceeded the all-Russian rate by 18.9‰ (RF 9.8‰) in 2019, 22.4‰ (RF 16.3‰) in 2020, 45.3‰ (RF 42.4‰) in 2021, and 23.2‰ (RF 12.6‰) in 2022 (Fig. 1). Relative to the pre-epidemic year of 2019, a significant increase in the rate was observed during the COVID-19 pandemic: ∆+18.5% in 2020, ∆+139.6% in 2021, and ∆+22.6% in 2022.
The absolute number of maternal deaths in the FEFD was 17 in 2019; 20 in 2020; 39 in 2021; and 19 in 2022. The overall structure of MM causes in the FEFD for the analyzed period (2019–2022) is shown in Figure 2, and the details are given in the table. According to the information, in the pre-epidemic period, obstetric causes had the largest share, 82.4% (14/17), while the share of extragenital disorders (EGD) was significantly lower (17.6% (3/17, χ2=11.8; p<0.001). In 2019, the leading causes of MM were ectopic pregnancy (23.5%), severe preeclampsia (23.5%), obstetric sepsis (11.8%), obstetric hemorrhage, obstetric embolism, uterine rupture were registered with equal frequency (5.9% each). Thus, in the pre-epidemic period, 41.2% of the cases of MM in the FEFD were due to three modifiable causes: pre-eclampsia (23.5%), sepsis (11.8%), and hemorrhage (5.9%). According to the Ministry of Health of Russia, a similar figure for the Russian Federation in 2019 was 40.3% (p>0.05). It should be noted that this structure of MM causes is largely due to the violation of the routing of pregnant women; in 2019, 47.1% of maternal deaths occurred at home (17.7%) and in level 1 health facilities (29.4%), while 52.9% occurred at level 2 (17.6%) and level 3 (35.3%) health facilities.
With the increase in COVID-19 incidence between 2020-2022, a number of obstetric hospitals in FEFD were converted to infectious disease mono-hospitals: four (25%) were level 3 and four (10%) were level 2.
From the first year of the COVID-19 pandemic (2020), MM increased due to a significant increase in EGD-related mortality in pregnant and postpartum women from 17.6% in 2019 to 75.0% (χ2=9.9; p=0.002). NCI accounted for a large proportion of this group (40.0% (8/20), followed by cardiovascular disease (10.0%), nervous system disease (15.0%), pulmonary embolism (TELA) (5.0%), and necrotizing pancreatitis (5.0%) accounted for 35.0%. Thus, during the COVID-19 pandemic, maternal mortality from non-communicable diseases increased 2.0-fold: 17.6% (2019) vs. 35.0% (2020), indicating organizational challenges in the care of patients with EGD (7/12, χ2=3.5; p=0.061). The proportion of obstetric causes of maternal mortality decreased from 82.4% (14/17) to 25.0% (5/20, χ2=9.9; p=0.002), followed by obstetric sepsis (15.0%), preeclampsia (5.0%), and acute fatty liver dystrophy (5.0%).
In the second year of the SARS-CoV-2 pandemic, MM increased even more: 2019 – 18.9, 2020 – 22.4, 2021 – 45.3 per 100 thousand live births. The 2.0-fold increase in MM in 2021 compared to 2020 was mainly due to multiple COVID-19 maternal losses: 66.6% (26/39) vs. 40.0% (8/20, χ2=3.9; p=0.050). Similar dynamics of the increase in mortality in the population as a whole, and maternal mortality in particular, in the second year of the pandemic, have been noted by other authors and explained by the greater pathogenicity of the delta strain, which emerged as a result of a natural mutation of the SARS-CoV-2 virus and prevailed in the epidemic waves of 2021 [14–16]. Domestic and foreign studies have convincingly demonstrated that the circulation of the delta genetic variant in 2021 was accompanied by a more severe course of the disease and worldwide resulted in a significant increase in the number of pneumonias, need for hospitalization in the ICU, need for invasive ventilatory support, and consequently, an increase in the incidence of adverse outcomes [14–17].
In an in-depth case analysis of the characteristics of MM from COVID-19, we found that the mean age of the patients was 32.3 (21–39) years and the mean gestational age was 30±1.46 weeks. In all cases, the women were not vaccinated against COVID-19. Overall, pregnant women in FEFD showed low adherence to NCI vaccination, with the proportion of mothers vaccinated in 2021 being 6.4% [18]. The highest risk of MM was associated with late hospitalization from the onset of disease symptoms (5.3±1.2 days vs. 3.5±1.1 days in the near miss group, p=0.048), which together with an unfavorable comorbid background including obesity (OR = 80.3; 95% CI 9.34–690.19); diabetes (OR=11.3; 95% CI 2.0–63.27); chronic arterial hypertension (OR=17.2; 95% CI 1.80–163.62); respiratory diseases (OR=12.2; 95% CI 1.19–123.96); anemia (OR=4.5; 95% CI 1.28–16.02), resulted in more pronounced pulmonary damage. Thus, the presence of grade 3-4 lung lesions on computed tomography at admission was associated with 9-fold higher risk of mortality (OR=9.1; 95% CI 3.03–27.14). Late hospitalization is also a risk factor for MM because it is accompanied by late initiation of anticoagulant and glucocorticoid therapy, often excluding the possibility of using genetically engineered drugs [19]. The risk factors for adverse maternal outcomes were the re-transportation of patients and treatment in infectious disease hospitals with no possibility of emergency delivery.
In 2021 vs. 2020, the proportion of obstetric causes of MM did not change significantly (20.5% (8/39) vs. 25.0% (5/20), χ2=0.004; p=0.951). However, it is worth noting the fact that there was a 1.5-fold increase in the number of rural residents among women: 43.6% (17/39) vs. 30% (6/20), χ2=0.535; p=0.465, and the causes included obstetric hemorrhage and obstetric sepsis (5.1% each), out-of-hospital abortion, ectopic pregnancy, preeclampsia, and amniotic fluid embolism (2.6% each), with half of the deaths occurring in level 1 facilities (37.5%, 3/8) or at home (12.5%, 1/8). The present findings suggest that there were irregularities in the routing and evacuation of pregnant women with high obstetric risk without NCI in FEFD in 2021.
In the third year of the COVID-19 pandemic, MM decreased 1.95-fold relative to the previous year (2021, 45.3; 2022, 23.2 per 100,000 live births), but did not reach the pre-epidemic rate (2019, 18.9‰). In the structure of causes of MM in FEFD in 2022, EGDs continued to lead the way, with the proportion not significantly different from that in 2021 (68.4% (13/19) vs. 66.6% (26/39), χ2=0.027; p=0.870). Notably, the proportion of MM cases from NCI decreased significantly in 2022 compared to 2021 (15.7% (3/19) vs. 66.6% (26/39), χ2=11.3; p<0.001). This can be explained by the fact that in 2022, the dominant strain in the FEFD population was Omicron, which was characterized by high contagiousness and transformation of the disease towards a more favorable course. Its clinical manifestation was dominated by symptoms similar to seasonal acute respiratory infections, and there was a significant decrease in the number of pneumonias and almost no fatalities [7, 20].
The negative trend of 2022 in FEFD is an increase in the number of MM cases from non-infectious EGD. Thus, acute cerebral circulation disorder (including recurrent hemorrhagic stroke) was registered in the structure of MM (10.5%, 2/19); severe cardiovascular disease: 1 – rheumatic heart disease. Acquired heart defect: mitral, aortic, tricuspid valve. Operated heart: mitral valve prosthesis with Edwards #27 xenoaortic biological prosthesis, De Vega tricuspid valve annuloplasty from 2008. Mitral valve replacement with Medeng mechanical prosthesis #25, aortic valve replacement with Medeng mechanical prosthesis #19 dated 13.11.2019, complicated by valve prosthesis thrombosis, acute heart failure, pulmonary edema; 2 – congenital heart defect, mitral valve insufficiency; and grade 3, eccentric hypertrophy. with eccentric myocardial hypertrophy with dilatation of cardiac cavities, complicated by pulmonary edema (10.5%, 2/19), massive pulmonary embolism (10.5%; 2/19), secondary bacterial meningitis with no identified source, severe (5.3%; 1/19); surgical sepsis with recurrent diaphragmatic hernia (5.3%; 1/19); Marfan syndrome with aortic aneurysm dissection (5.3%; 1/19); and decompensated systemic lupus erythematosus with multi-organ lesions (5.3%; 1/19). All pregnant and postpartum women who died from EGD were not examined before pregnancy, they lacked pre-pregnancy care, there was a delay in seeking medical care, and in some cases - underestimation of severity and clinical symptoms at the level of primary care and allied health professionals.
In the structure of maternal mortality in the third year of the pandemic, obstetric causes accounted for 26.4% (5/19), which was not significantly different from that in 2020 (20.5%, 8/39) and 2021 (25.0%, 5/20) (χ2=0.3; p=0.861). Obstetric hemorrhage ranked first (10.5%, 2/19), with severe preeclampsia, obstetric sepsis, and acute fatty liver dystrophy (5.3% each, 1/19) reported with equal frequencies. Note that cases of maternal deaths from obstetric hemorrhage occurred in level 2 and obstetric sepsis in level 1facilities, accounting for 75% of the manageable causes of MM (3/4).
The COVID-19 pandemic has led to increased rates and changes in the pattern of maternal mortality compared to the pre-pandemic period. On one hand, the proportion of NCI has increased among the causes of MM, while on the other hand, the number of maternal deaths from manageable obstetric causes has risen at levels 1 and 2 of healthcare facilities, particularly among rural women. These facts indicate emerging organizational issues, including disruptions in the routing and evacuation of at-risk pregnant women without NCI. These disruptions have been caused by the reprofiling of level 2 and 3 obstetric hospitals into infectious disease-centered facilities in several areas. Additionally, there is a shortage of medical personnel (retraining and illness) responsible for providing care to pregnant and parturient women. Natural disasters, such as large-scale floods and fires in 2021–2022 in many FEFD regions have also contributed to these challenges.
The high morbidity and mortality of pregnant women with COVID-19 are largely due to the lack of pre-pregnancy care and the failure to address pre-existing conditions that increase the risk of severe COVID-19 outcomes. These conditions include obesity, hypertension, diabetes, and iron deficiencies. Furthermore, maternal irresponsibility for their own health, such as non-compliance with preventive measures, refusal to be vaccinated, and delayed medical care seeking, also play a significant role.
During the pandemic period of 2020–2022, the increase in the number of MM cases from non-infectious EGD emergencies has been attributed to inadequate medical examination and pre-pregnancy care for patients with somatic comorbidities. This is compounded by the lack of highly qualified counseling by specialized allied healthcare professionals such as cardiologists, neurologists, and rheumatologists. As a result, timely diagnosis and correction of disorders were not performed, safe fertility terms were not established or agreed upon, and the patients and their families were not informed about the associated pregnancy risks.
Overall, the COVID-19 pandemic has significantly impacted MM rates and patterns in FEFD, driven not only by increased maternal losses directly from NCI, but also by increased mortality rates from non-communicable diseases and manageable obstetric causes. To reduce the incidence of life-threatening conditions and adverse maternal outcomes, full dispensary monitoring and pre-pregnancy care should be provided, and routing schemes for high-risk patients during pregnancy, delivery, and the postpartum period should be optimized. Given the regional geographic and climatic features of the FEFD (long distances, remote areas, and a high frequency of typhoons, snow drifts, floods, and fires), as well as its demographic characteristics (low population density), a system of remote monitoring with risk stratification in the dynamic stages of pregnancy needs to be expanded. Additionally, interregional cooperation should be developed to evacuate patients for delivery and/or treatment in perinatal and multidisciplinary hospitals at an appropriate level and profile.
Conclusion
The dynamics and structure of MM in FEFD, as revealed in this study, underscore the need for management decisions aimed at improving the current system of medical examination for women of childbearing age and the routing of pregnant women at risk of developing critical obstetric conditions.
References
- WHO. A woman dies every two minutes due to pregnancy or childbirth: UN agencies. 23 February 2023. https://www.who.int/ru/news/item/23-02-2023-a-woman-dies-every-two-minutes-due-to-pregnancy-or-childbirth--un-agencies
- RCOG. Restoration and Recovery: Priorities for obstetrics and gynaecology. A prioritization framework for care in response to COVID-19. Version 2.1. Published Friday 26 June 2020. 27 р.
- Chen H., Guo J., Wang C., Luo F., Yu X., Zhang W. еt al. Clinical characteristics and intrauterine vertical transmission potential of COVID-19 infection in nine pregnant women: a retrospective review of medical records. Lancet. 2020; 395(10226):809-15. https://doi.org/10.1016/S0140-6736(20)30360-3.
- Белокриницкая Т.Е., Артымук Н.В., Филиппов О.С., Фролова Н.И. COVID-19 у беременных Сибири и Дальнего Востока: итоги 2 лет пандемии. Акушерство и гинекология. 2022; 4: 47-54. [Belokrinitskaya T.E., Artymuk N.V., Filippov O.S., Frolova N.I. COVID-19 in pregnant women of Siberia and the Russian Far East: 2-year results of the pandemic. Obstetrics and Gynecology. 2022; (4): 47-54 (in Russian)]. https://dx.doi.org/10.18565/aig.2022.4.47-54.
- Faria N.R., Mellan T.A., Whittaker C., Claro I.M., Candido D.S., Mishra S. еt al. Genomics and epidemiology of the P.1 SARS-CoV-2 lineage in Manaus, Brazil. Science. 2021; 372(6544):815-21. https://dx.doi.org/10.1016/10.1126/science.abh2644.
- Andeweg S.P., Vennema H., Veldhuijzen I., Smorenburg N., Schmitz D., Zwagemaker F. еt al.; SeqNeth Molecular surveillance group and RIVM COVID-19 Molecular epidemiology group. Elevated risk of infection with SARS-CoV-2 Beta, Gamma, and Delta variants compared with Alpha variant in vaccinated individuals. Sci. Transl. Med. 2023;15(684):eabn4338. https://dx.doi.org/10.1016/10.1126/scitranslmed.abn4338.
- Dyer O. Covid-19: Omicron is causing more infections but fewer hospital admissions than delta, South African data show. BMJ. 2021;375:n3104. https://dx.doi.org/10.1016/doi: 10.1136/bmj.n3104.
- Sharif N., Alzahrani K.J., Ahmed S.N., Khan A., Banjer H.J., Alzahrani F.M. et al. Genomic surveillance, evolution and global transmission of SARS-CoV-2 during 2019–2022. PLoS One. 2022; 17(8): e0271074. https://doi.org/10.1371/journal.pone.0271074.
- Министерство здравоохранения Российской Федерации. Временные методические рекомендации «Профилактика, диагностика и лечение новой коронавирусной инфекции (COVID-19)». Версия 17 (14.12.2022). [Ministry of Health of the Russian Federation. Temporary methodological guidelines “Prevention, diagnosis and treatment of new coronavirus infection (COVID-19)”. Version 17 (14.12.2022). (in Russian)].
- Chmielewska B., Barratt I., Townsend R., Kalafat E., van der Meulen J., Gurol-Urganci I. et al. Effects of the COVID-19 pandemic on maternal and perinatal outcomes: a systematic review and meta-analysis. Lancet Glob. Health. 2021; 9(6):e759-e772. https://dx.doi.org/10.1016/10.1016/S2214-109X(21)00079-6.
- Litman E.A., Yin Y., Nelson S.J., Capbarat E., Kerchner D., Ahmadzia H.K. et al. Adverse perinatal outcomes in a large United States birth cohort during the COVID-19 pandemic. Am. J. Obstet. Gynecol. MFM. 2022;4(3):100577. https://dx.doi.org/10.1016/10.1016/j.ajogmf.2022.100577.
- Указ Президента Российской Федерации от 03.11.2018 № 632 «О внесении изменений в перечень федеральных округов», утвержденный Указом Президента Российской Федерации от 13 мая 2000 г. № 849. Режим доступа: http://publication.pravo.gov.ru/Document/View/0001201811040002/ [Decree of the President of the Russian Federation of 03.11.2018 No. 632 "On amendments to the list of Federal districts" approved by Decree of the President of the Russian Federation of May 13, 2000 No 849. Available at: http://publication.pravo.gov.ru/Document/View/0001201811040002/(in Russian)].
- Министерство здравоохранения Российской Федерации. Организация оказания медицинской помощи беременным, роженицам, родильницам и новорожденным при новой коронавирусной инфекции COVID-19. Методические рекомендации. Версия 5 (28.12.2021). [Ministry of Health of the Russian Federation. Organization of medical care for pregnant women, women in labor, women in labor and newborns with a new coronavirus infection COVID-19. Methodological guidelines. Version 5 ( 28.12.2021). (in Russian)].
- Mihajlovic S., Nikolic D., Santric-Milicevic M., Milicic B., Rovcanin M., Acimovic A., Lackovic M. Four Waves of the COVID-19 Pandemic: сomparison of Clinical and Pregnancy Outcomes. Viruses 2022; 14(12): 2648. https://dx.doi.org/10.1016/10.3390/v14122648.
- Del Rio C., Malani P.N., Omer S.B. Confronting the Delta variant of SARS-CoV-2, summer 2021. JAMA. 2021; 326(11):1001-2. https://dx.doi.org/10.1016/10.1001/jama.2021.14811.
- Vousden N., Ramakrishnan R., Bunch K., Morris E., Simpson N., Gale C. et al. Management and implications of severe COVID-19 in pregnancy in the UK: data from the UK Obstetric Surveillance System national cohort. Acta Obstet. Gynecol. Scand. 2022;101(4):461-70. https://dx.doi.org/10.1016/ 10.1111/aogs.14329.
- Белокриницкая Т.Е., Фролова Н.И., Колмакова К.А., Шаметова Е.А. Факторы риска и особенности течения COVID-19 у беременных: сравнительный анализ эпидемических вспышек 2020 и 2021 г. Гинекология. 2021; 23 (5): 421-7. [Belokrinitskaya T.E., Frolova N.I., Kolmakova K.A., Shametova E.A. Risk factors and features of COVID-19 course in pregnant women: a comparative analysis of epidemic outbreaks in 2020 and 2021. Gynecology. 2021; 23 (5): 421-7 (in Russian)]. https://dx.doi.org/10.1016/10.26442/20795696.2021.5.201107.
- Артымук Н.В., Белокриницкая Т.Е., Парфенова Я.А., Фролова Н.И. Мониторинг вакцинации беременных против COVID-19 в Сибирском и Дальневосточном федеральных округах. Акушерство и гинекология. 2022; 5: 53-8. [Artymuk N.V., Belokrinitskaya T.E., Parfenova Ya.A., Frolova N.I. Monitoring of COVID-19 vaccination in pregnant women of Siberia and the Russian Far East. Obstetrics and Gynecology. 2022; (5): 53-8 (in Russian)]. https://dx.doi.org/10.18565/aig.2022.5.53-58.
- Белокриницкая Т.Е., Артымук Н.В., Филиппов О.С., Фролова Н.И., Парфенова Я.А. Материнская смертность и near miss при новой коронавирусной инфекции (COVID-19) у беременных Сибири и Дальнего Востока. Проблемы репродукции. 2021; 27(5): 114-20. [Belokrinitskaya T.E., Artymuk N.V., Filippov O.S., Frolova N.I., Parfenova Ya.A. Maternal mortality and critical conditions (near miss) in COVID-19 in pregnant women of Siberia and the Far East. Russian Journal of Human Reproduction. 2021;27(5):114-20. (in Russian)]. https://dx.doi.org/10.1016/10.17116/repro202127051114.
- Антонова М.И., Колмакова К.А., Румянцева К.А., Шаметова Е.А., Белокриницкая Т.Е., Фролова Н.И. Факторы риска и особенности течения СOVID-19 у беременных в динамике эпидемического процесса. Медицина завтрашнего дня. Материалы XXI межрегиональной научно-практической конференции студентов и молодых ученых с международным участием. Чита; 2022: 94-5. [Antonova M.I., Kolmakova K.A., Rumyantseva K.A., Shametova E.A., Belokrinitskaya T.E., Frolova N.I. Risk factors and features of the course of COVID-19 in pregnant women in the dynamics of the epidemic process. In: Medicine of Tomorrow. Materials of the XXI interregional scientific and practical conference of students and young scientists with international participation. Chita; 2022: 94-5 (in Russian)].
Received 22.06.2023
Accepted 07.11.2023
About the Authors
Tatiana E. Belokrinitskaya, Dr. Med. Sci., Professor, Head of the Obstetrics and Gynecology Department of the Pediatric Faculty and Faculty of Professional Retraining, Chita State Medical Academy, Ministry of Health of Russia, +7(3022)32-30-58, tanbell24@mail.ru, https://orcid.org/0000-0002-5447-4223, 672000, Russia, Chita, Gorky str., 39a.Roman G. Shmakov, Dr. Med. Sci., Professor of the RAS, Head of the Institute of Obstetrics, Academician V.I. Kulakov National Medical Research Center for Obstetrics, Gynecology and Perinatology, Ministry of Health of Russia, r_shmakov@oparina4.ru, https://orcid.org/0000-0002-2206-1002, 117997, Russia, Moscow, Oparin str., 4.
Nataly I. Frolova, Dr. Med. Sci., Associate Professor at the Department of Obstetrics and Gynecology of the Pediatric Faculty and Faculty of Professional Retraining,
Chita State Medical Academy, Ministry of Health of Russia, taasyaa@mail.ru, https://orcid.org/0000-0002-7433-6012, 672000, Russia, Chita, Gorky str., 39a.
Olga Yu. Brum, Deputy Chief Physician for Obstetrics and Gynecological Care, Transbaikal Regional Perinatal Centre, ymnenkaya@yandex.ru,
https://orcid.org/0000-0002-6065-3666, 672090, Russia, Chita, Kokhansky str., 16.
Natalia A. Krivoshchekova, Deputy Chief Physician for Obstetrics and Gynecology, Blagoveshchensk City Clinical Hospital, zamrod_gkb1@mail.ru, https://orcid.org/0000-0001-9345-1553, 675000, Russia, Amur region, Blagoveshchensk, Gorky str., 247.
Tatiana Yu. Pavlova, PhD, Director, Perinatal Center of the Republic of Sakha (Yakutia) Republican Hospital No. 1 of the National Center of Medicine, tatyanaupavl@mail.ru, https://orcid.org/0000-0002-3319-912X, 677010, Russia, Republic of Sakha (Yakutia), Yakutsk, Sergelyakhskoe highway, 4.
Marina P. Rinchindorzhiyeva, PhD, Head of the Organizational and Methodological Unit, Buryat Republic Perinatal Center, marirmp@mail.ru,
https://orcid.org/0000-0003-1153-6057, 670047, Russia, Republic of Buryatia, Ulan-Ude, Pirogova str., 15B.
Corresponding author: Tatiana E. Belokrinitskaya, tanbell24@mail.ru