Comparison of the effectiveness of ultrasound diagnosis in assessment of uterine scar defets after cesarean section
Aim: To improve the effectiveness of uterine scar assessment after cesarean section (CS) using ultrasound techniques. Materials and methods: A comparative study included 65 patients with thinned uterine scar after CS, who were planning repeated pregnancy. The first stage of research was a routine pelvic ultrasound examination on the outpatient basis, which was performed outside the Research Center for Obstetrics, Gynecology and Perinatology. The second stage was expert pelvic ultrasound examination and scar measurements using a modified Delphi procedure that was performed in the National Medical Research Center for Obstetrics, Gynecology and Perinatology. At the third stage, two specialists of the Center independently performed complex ultrasound, which included expert pelvic ultrasound examination and hysterosalpingography (HSG). The results of measurements of cesarean section scars obtained at the 1st and 2nd stages of research and during expert pelvic ultrasound examination and HSG, as well as the consistency of measurement results obtained by 2 sonographers at the third stage were evaluated. Results: The comparative analysis of routine and expert pelvic ultrasound showed that statistically significant differences were found in measurement of residual myometrial thickness (RMT) (3.21 (1.2) mm and 2.76 (1.0) mm, respectively, р<0.05), width and depth of SC scar. The comparative analysis of expert US and HSG showed that statistically significant differences were found in measurements of RMT (2.83 (1.1) mm and 2.4 (0.95) mm, respectively, р<0,05, width, length and depth of niche. The comparative analysis of the results independently obtained by 2 sonographers during performance of expert ultrasound and HSG did not show statistically significant differences. However, according to the Bland–Altman analysis, the scatter plot of the obtained values was less in HSG than in expert US. This indicates a greater reproducibility of the research method. Conclusion: When uterine scar defect after cesarean section is found during ultrasound at the stage of outpatient examination, it is appropriate to refer the patient to a specialized medical institution to undergo examination there and to define management strategy. Expert pelvic US using Delphi criteria helps to determine how accurately cesarean section scars can be detected. In doubtful cases, as well as when it is required to take a decision on necessity and the volume of surgery, it is preferable to perform HSG that ensures high reproducibility and provides additional "navigation" information for the surgeon.Sidorova T.A., Martynov S.A., Adamyan L.V., Letunovskaya A.B., Boykova Yu.V.
Keywords
Currently, about 20% of pregnant women undergo cesarean section (CS) [1]. In most regions of the world this rate is higher and continues to increase reaching 40.5% in some countries [2]. According to Rosstat, in Russia the rate of CSs was 17.9% in 2005, and 30.3% in 2020 [3]. V.I. Krasnopolsky et al. [4] reported that the rate of CSs in some large perinatal Centers in Russia reaches 40% and higher.
Uterine scar defect may be a cause of menstrual disorder, chronic pelvic pain and secondary infertility. In pregnancy, most serious clinical conditions associated with uterine scar defects are ectopic pregnancy in the scar, placenta ingrowth and placenta previa, uterine rupture. Due to this, the assessment of uterine scar condition in non-pregnant women and assessment-based prediction of the course of subsequent pregnancy and birth is of particular relevance.
The scar defect (thinning of the scar) should be defined as thinned scar area compared to the surrounding intact myometrium. Uterine scar defects can be in the form of niche and without niche [5].
A niche is understood as an anechoic area in the uterine cavity at the scar site after cesarean section with a depth of at least 2 mm, according to some authors 3 –– 5 mm [6]. Most often, the term "niche" is used in the absence of gradual changes in myometrial thickness at the site of the defect, at the same time the niche has scraggy and often “undermining” edges.
Currently, the most common and available utltrasound techniques are transvaginal ultrasonography and sono-hysterosalpingography (sono-HSG) with contrast agents. Saline solutions, sono-contrast agents and gels are used as a contrast medium. Numerous options for assessment of uterine scars have been proposed, that along with determination of the width, length, depth, the localization of the defect, the residual myometrial thickness (RMT) at the scar site include the description of the scar shape, the presence of streaks, measurement of the niche volume and the degree of thinning (thinning index), etc., which are necessary for further patient management strategy. The possibilities of 2D and 3D ultrasound, computer modelling of the niche shape in sono-HSG have been described. The advantages of 2D ultrasound are the prevalence and accessibility of the method, the possibility of rapid training and education of specialists. 3D ultrasound provides three-dimensional images, computer modelling and more accurate assessment of niche shape and volume. Sono-HSG with contrast fluid filled in the uterine cavity and niche makes it possible to evaluate in detail the RMT, the shape and edges of the niche, the presence of leakage and branches, as well as to carry out automated determination of the niche volume using special software programs. Besides evaluation of the scar condition, the assessment of fallopian tubes patency during using sono-HSG is especially important for the patients planning future pregnancy [6–14]. However, currently, there is no common point of view regarding the choice of the diagnostic method, as well as no generally accepted measurement technique for assessment of uterine scar defects after CS.
The Delphi technique is important with regard to the methodological aspect [6]. 20 experts in uterine scar defects after cesarean section, who have publications in peer-reviewed journals were involved in the study. The authors performed meta-analysis of literature as well as the blind cross-sectional survey and came to consensus regarding the method for detection and description of uterine scar defects, as well as US assessment of specific features of measurements. The experts of Delphi group acknowledged the informativity of sono-HSG, and its advantages in evaluation of the shape of the defect and visualization of niche edges. However, sono-HSG was not recommended as a mandatory evaluation of uterine scar defects after cesarean section. At the same time, numerous publications on diagnostic value of sono-HSG suggest that the method is good not only due to informativity, but also high reproducibility, although there are some differences between measurements of uterine scar parameters using US and sono-HSG.
Fundamentally based on Delphi technique [6], the goal of our research was to improve the effectiveness of uterine scar assessment after cesarean section (CS) using different ultrasound techniques.
Materials and methods
The comparative research was carried out in the Academician V.I. Kulakov National Medical Research Center for Obstetrics, Gynecology and Perinatology, Ministry of Health of Russia. The study group included 65 patients with uterine scar after cesarean section (the previous cesarean section was performed more than 1 year ago), who were planning to become pregnant again. The inclusion criteria were the patients aged 18–45 years; pregnancy planning; US-based thinning of uterine scar after cesarean section (RMT<5 mm); patient’s informed consent to participate in the study. The exclusion criteria were the age of women under 18 years and over 45 years; acute pelvic inflammatory disorders, severe comorbid somatic diseases; malignant neoplasms.
At the first stage, the patients in the proliferative phase on days 5–11of the menstrual cycle underwent a routine pelvic ultrasound examination on the outpatient basis. US examination was carried out by different investigators – not from the National Medical Research Center for Obstetrics, Gynecology and Perinatology (the Center), using ultrasound systems of different classes.
At the second and third stages, expert-guided pelvic US and sono-HSG were carried out in the Center for further diagnostic findingsi.
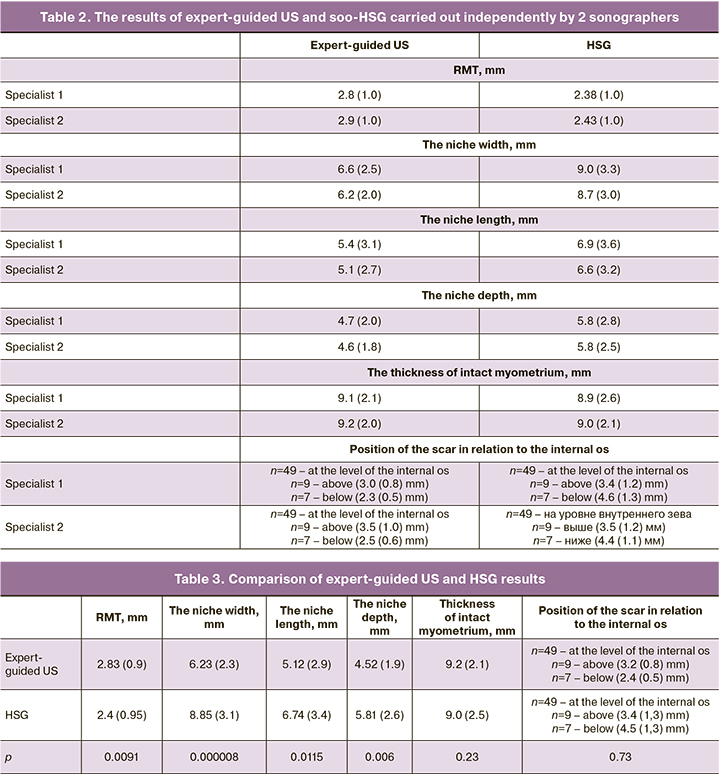
Expert-guided pelvic ultrasound was carried out in the proliferative phase on days 5–11 of the menstrual cycle using Samsung WS80А 7.5 MHz device (Elite (Samsung Medison, South Korea). The assessment was performed by the specialists of the Department of Ultrasound and Functional Diagnostics of the Center with more than 10 years work experience in obstetrics and gynecology, who have performed more than 10 000 investigations) and have a significant experience in ultrasound diagnosis of uterine scars after cesarean section. Topography and anatomic features of internal female reproductive organs were described. Separately, the uterine scar parameters were measured using Delphi technique [6]. The maximum niche length and depth (in the saggital plane); the minimal RMT at the scar site (in the saggital plane perpendicular to the serosa from the upper inner contour of the defect to the serosa, while the endometrium and serosa were not measured); the maximum niche width (in the transverse plane); the thickness of intact myometrium – the thickness of the anterior wall of the uterus near the upper edge of the niche (in the saggital plane) were measured. The distance between the niche and the vesicouterine fold, as well as the distance between the lower edge of the niche and the external os of the cervix were not assessed (according to the Delphi recommendations, these parameters are not mandatory for evaluation). At the same time, we found it necessary to include one more parameter – the location of the scar in relation to the internal cervical os (the minimum distance from the internal os to the nearest edge of the niche in the sagittal plane), since it exhibits more accurately the "cervicalization", i.e. a low location of the scar. The last three parameters are more important for surgeons as an additional “navigation” data during surgery.
Complex ultrasound examination, including 2 stages (transvaginal expert-guided ultrasound similar to the above described, and subsequent sono-HSG) was carried out on days 7–11 of the menstrual cycle using WS80A (Samsung Medison, Ю. Корея) transvaginal ultrasound machine with 7.5 MHz frequency. For comparative assessment of two methods, assessment of uterine scar parameters was performed independently by 2 sonographers in a successive order in each case in real time. The first specialist had 15 years experience in sono-HSG performance (he carried out more than 300 sono-HSG investigations). The second specialist had 25 years work experience in the Center, but less experience in sono-HSG performance. Both 2 specialists were not aware of the results obtained by them until the end of measurements.
The procedure of sono-HSG was done in the following way. The patients underwent preliminary laboratory testing: smears for vaginal flora examination and blood test for hepatitis B and C, syphilis and HIV. 0.9% sodium chloride solution was used as anechoic contrast medium. After the first stage of examination (transvaginal ultrasonography), Cusco speculum was used to retract the vaginal wall for exposure of the cervix. Vagina and cervix were cleaned with anticeptic solution (Octenisept). Soft 6600 Angiotech (5Fr) balloon catheter was placed in the cervix and fixed due to inflated balloon. 10–20 ml of sterile 0.9% sodium chloride solution at T 36.6°С was injected in the cervix to carry out accurate contrast-enhanced transvaginal ultrasound for real-time data monitoring. Ultrasound contrast agents were used for tubal assessment. Topography and anatomic features of internal female reproductive organs were described, and the uterine scar parameters were measured using Delphi technique. At the end of the procedure the balloon catheter was removed from the cervix.
Statistical analysis
Statistical data processing and analysis was performed using Microsoft Excel 2010 и STATISTICA Application v.10.0. The Kolmogorov–Smirnov and Shapiro–Wilk tests were used to assess the normality of data distribution. Normal distribution is shown as median (standard deviation). Student’s T-test was used to compare the obtained data. The consistency of different measurements obtained by the two methods, as well as by two independent investigators, was analyzed using Bland–Altman plot. Statistical hypothesis testing was significant at р<0.05.
Results
The average age of patients was 34.0 (3.9) years and varied from 29 to 43 years. 51 patients underwent 1 CS in anamnesis, 11 patients had 2 CSs, and 3 patients had 3 CSs. At the time of the research, more than 1 year passed after CS in all women. Previously, emergency C-section were performed in 67.7% of patients (44 women), and elective C-section was performed in 32.3 % (21 women).
Most common clinical manifestation of uterine scar defect was scanty vaginal discharge in 51 patients after menses (for 2–20 days, on average 7 days); in 5 patients before menses (on average 2 days); in 3 patients in the middle of the menstrual cycle (on average 3.5 days). In addition to these complainеs, pregnancy did not occur in 7 patients, despite regular sexual life and non-use of contraception for more than 1 year; and 4 patients had algomenorrhea that occurred after cesarean section. Asymptomatic cause was observed in 6 patients.
The comparative analysis of the results of routine US and expert-guided US showed that statistically significant differences were found in assessment of RMT, width and depth of the niche, and no statistically significant differences were found in measurement of the niche length, the thickness of intact myometrium, and the position of the scar in relation to the internal os (Table 1).
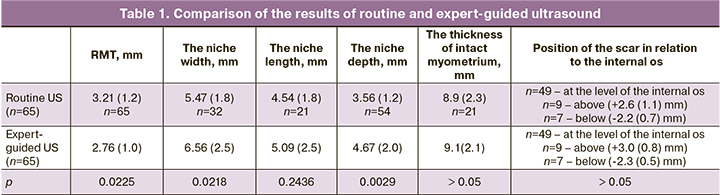
It should be noted, that the analysis of the results of routine US performed at the outpatient stage showed that in the vast majority of cases, the assessment of uterine scar parameters was incomplete. RMT and the niche depth were measured mostst often, while the niche width and length were measured less than in half of patients. Other parameters were not included in reports (Table 1).
According to expert-guided US results, in 7 cases the scar was positioned in the upper one-third of the cervix, in 9 cases – in the lower one-third of the uterine wall, and in other cases – in the projection of the internal os. In 4 patients 2 scars after 2 CSs, in 1 patient 2 scars after 3 CSs, in 4 patients 2 scars after 2 CSs, and in 1 patient 2 scars after 3 CSs were detected. In other patients only 1 scar was visualized independently on the number of C-sections in anamnesis.
The measurement results of uterine scar parameters obtained independently by 2 sonographers who carried out expert-guided US and sono-HSG are shown in Table 2.
To compare the results obtained by two methods (expert-guided US and sono-HSG), the mean values of uterine scar parameters measured by both specialists were analyzed (Table 3).
The comparative analysis of the results obtained by expert-guided US and sono-HSG showed statistically significant differences in measurements of RMT, the niche width, length and depth. No statistically significant differences were found neither in intact myometrium thickness nor in position of the scar in relation to the internal os.
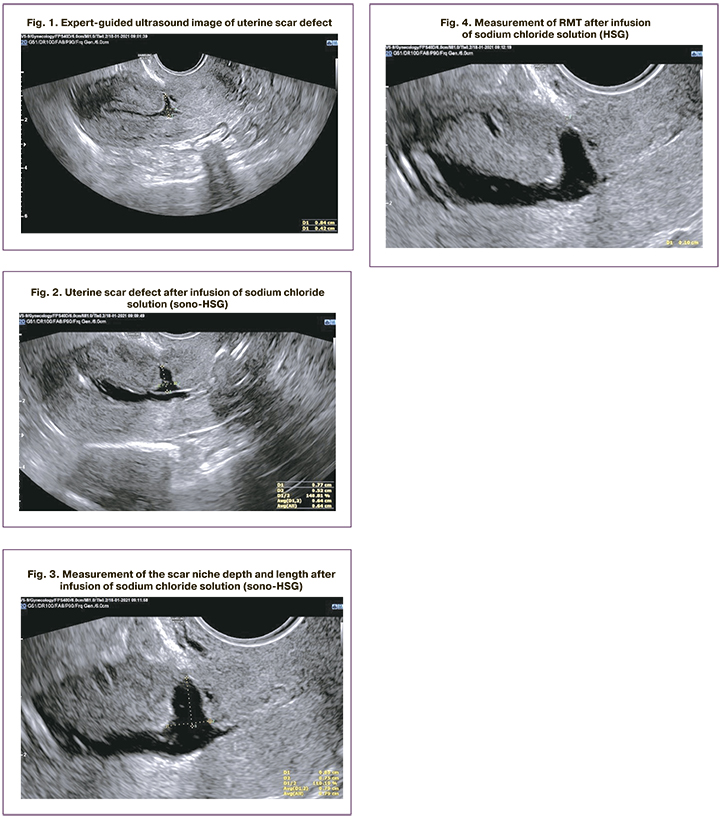
The consistency of assessment of the same parameters by 2 specialists, who varied in their level of training for 2 investigation methods (expert-guided US and sono-HSG) was analyzed. Student’s T-test for independent variables did not find statistically significant differences. Due to this, Bland–Altman plot was used for analysis. The mean values of differences between the measurements performed independently by 2 professionals, as well as the upper and lower ranges of 95% confidence interval (CI) for differences between the measurements performed by 2 specialists were calculated (Table 4). The closer the mean values were to zero and narrower was the range of 95% confidence interval, the more identical were measurement values.
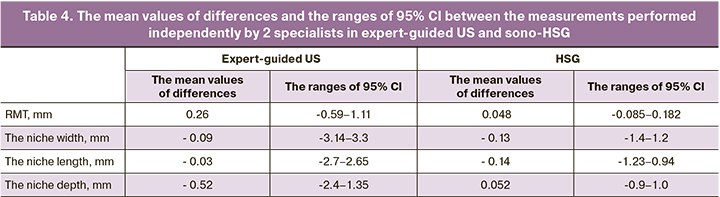
Since the residual myometrial thickness is of fundamental importance in making a decision about surgical correction of uterine scar, based on the obtained data, Bland–Altman plots were constructed to determine the consistency of measurements of this particular parameter (Fig.5).
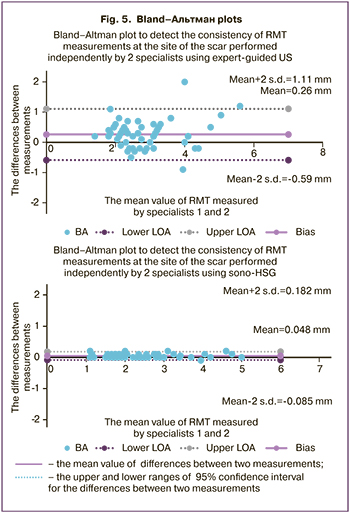
The analysis of Bland–Altman plots showed that the mean difference between the values obtained by specialists 1 and 2, who carried out expert-guided US and sono-HSG, was close to zero. This proved the consistency of measurements. However, more attention was drawn to the fact that the differences between expert-guided US results had a wider 95% CI versus sono-HSG results. This indicated a large scatter of data in expert-guided US, and accordingly, more pronounced consistency and homogeneity of data obtained in sono-HSG.
The obtained data were further confirmed during hysteroscopy and/or laparoscopy.
Discussion
In the modern world, an increasing tendency of high rates of cesarean sections is observed. This is both due to expanded indications for operative delivery, and the increased number of primipara women of late reproductive age. Wide prevalence and high rates of CSs, that have no tendency to reduction, recently cause increased attention to the problem of uterine scar after cesarean section. At the same time, numerous studies are devoted not only to assessment of the uterine scar condition during pregnancy and at birth, but also detection of uterine scar defects after previous cesarean section in the non-pregnant women as well as different techniques for its correction. The conclusions made by ultrasound diagnosticians are often the ground for surgical intervention. Moreover, RMT is a major parameter that influences making a decision about metroplasty, and less often the other parameters: the niche length, width and depth, or the thinning index of RMT/the thickness of intact myometrium. Also, metroplasty performance depends on the position of the uterine scar in relation to the internal os. Since the decision about surgery directly depends on the accuracy and consistency of measurements of these parameters, the goal of our study was to improve the effectiveness of uterine scar assessment after performance of CS using ultrasound techniques.
The results obtained by us showed discrepancy in the assessment of uterine scar condition between routine US and expert-guided US. This is especially important for further strategies of patient management, as well as for defining the indications for surgery and choosing the method of surgical treatment. A thorough assessment detected a number of systemic disorders.
Firstly, it should be noted that in the vast majority of ultrasound findings performed by different specialists at the outpatient stage, the measurements of uterine scar parameters were carried out not in full scope. RMT and the niche depth were measured most often, while the niche width and length were measured less than in half of patients, and the other parameters were not registered in parameter measurement reports. This fact indicates the absence of generally accepted research method for uterine scar assessment after cesarean section.
Secondly, we found statistically significant differences in measurements of RMT, the niche width and depth, including “overestimation” of the scar thickness and “underestimation” of the niche parameters at the outpatient diagnostic stage. The differences found by us could be due to lack of a unified method for measuring the uterine scar parameters. Most probably, “overestimation” of the value of RMT is due to inclusion of the serous layer and the areas of fibrosis, and possibly endometrium in measurement, although these layers are not recommended for registration. Also, it is possible that RMT was measured not perpendicular to the seous layer. Moreover, ultrasonography was carried out using the US machines of different class, and this could influence the quality of measurements; and the sonographers had different levels of training, as well as they had no experience in uterine scar examination after CS. Baranov А. et al. [7] reported that skill formation is of high importance even in experienced ultrasound diagnosticians, because it is important for diagnostic accuracy. In addition, the term “incompetent uterine scar” was often used in expert-guided US reports, and as we previously pointed out, this term can not be acceptable [5].
At the same time, of particular note is time consistency of sonography performance by two specialists. The assessed uterine scar condition in phase 1 on days 5–11 of the menstrual cycle.
Thus, the first part of our study showed significant differences in assessment of uterine scar condition after CS using routine and expert-guided US.
The next goal of the study was to compare the accuracy in diagnosing uterine scar defects by specialists with different work experience who are experienced in using a unified approach to transvaginal expert-guided US and sono-HSG, as well as comparison between the 2 methods based on comparative characteristics of uterine scar.
The obtained results indicate a high consistency of measurements performed independently by 2 sonographers, both in transvaginal sonography and sono-HSG. No statistically significant differences were found in the parameters, although variations in the values were less in sono-HSG than in US examination. One of the sonographers had less experience in carrying out sono-HSG. At the same time, he noted that sonographic images were very clear, and this facilitated the performance of measurements of all uterine scar parameters and influenced the accuracy of the results. This is confirmed by Monteagudo А., Regnard С., Osser О., Baranov А. [7–10], who reported a more clear visualization of the niche edges in sono-HSG. Thus, according to Baranov A. et al. [7] a high correlation between measurements of RMT and the thickness of intact myometrium was detected independently by two experts borth in US examination (the correlation coefficient was 0.87 and 0.82, respectively) and in sono-HSG (the correlation coefficient was 0.96 and 0.85, respectively). Moreover, the authors noted that measurement of RMT using sono-HSG was most consistent.
The results obtained by us indicate a high reproducibility of both methods (expert-guided US and sono-HSG) and a decrease in the rate of discrepancies in measurements of uterine scar parameters performed in the specialized healthcare institutions. Ultimately, this is provided by availability of the modern equipment, extensive experience of specialists, as well as knowledge and skills in using techniques for measurement of uterine scar defects after CS.
Sono-HSG measurements were most consistent. Moreover, the difference in the experience of the sonographers did not influence the accuracy of uterine scar measurements. It proves that sono-HSG has a greater reproducibility and due to this, it can be considered as a “gold standard” among existing sonographic methods for diagnosis of uterine scar defects after cesarean section.
Comparison of both methods (expert-guided US and sono-HSG) in assessment of uterine scar condition after CS showed significant differences in measurements of RMT, the niche width, length and depth, and did not find differences in assessment of the thickness of intact myometrium and the position of the scar in relation to the internal os. At the same time, the values of RMT were lower and the values of the niche parameters were higher in sono-HSG. Apparently, this was due to dilatation of the niche filled with a contrast medium, and the change in measurement angle of RMT.
Menada Valenzano М. et al. [11] also reported that the niche sizes were significantly larger in sono-HSG versus US examination.
Rasheedy R. et al. [12] noted that RMT at the scar site was greater in sono-HSG versus US examination – 10.09 (2.74) mm and 11.18 (2.50) mm, respectively (r=0.914). Also, larger width and depth of the niche in sono-HSG and no differences between the methods used in assessment of the thickness of intact myometrium were noted.
In the prospective cohort study by Antila-Langsjö R. et al. [13], 2 methods (US and sono-HSG with sodium chloride solution as a contrast medium) in diagnosing scar defects after CS were compared. Sono-HSG assessment showed larger niche depth and width and the mean values of RMT – 3.7 mm and 3.3. respectively, versus ultrasound results.
The similar tendency was noted in the study by Baranov А. et al. [7]. Sono-HSG measurement of both RMT and the thickness of intact myometrium was greater bersus US – 5.6 mm and 4.8 mm, respectively; 8.9 mm and 8.5 mm, respectively.
At the same time, Osser O.V. et al. [10] found greater length and width of the niche according to sono-HSG results and the absence of differences between the methods for RMT measurement.
Variability in results obtained in comparison of two diagnostic methods for assessment of the same parameters can only mean one thing – the absence of a unified method for measurements, especially at the initial stages of assessment of this condition. With experience accumulation, an increasing number of investigators note lower values of RMT in sono-HSG compared to US. This may be due to better visualization of the thinnest areas of the scar when the niche is filled with contrast medium. This fact should be considered in interpretation of the results of different sonographic methods with purpose to determine the indications for surgical correction of uterine scar defects.
Conclusion
Thus, our study showed extensive diagnostic possibilities of ultrasonic techniques for detection of uterine scar condition after cesarean section. In most cases, discordant assessments of ultrasound diagnosticians is because of the absence of a unified method for measurements. Due to this, standardization of uterine scar evaluation after cesarean section is of great importance.
The Delphi technique summarized the experience of twenty recognized experts in ultrasound diagnostics. In our opinion, it offers the best algorithm and method for measurement of uterine scar after cesarean section. Following the principles outlined in Delphi guidelines will make it possible to standardize ultrasound techniques (both echography and sono-HSG) and reduce the frequency of discrepancies in measurements of the same parameters by different specialists.
When uterine scar defect after cesarean section is suspected at the outpatient stage, it is appropriate to refer the patient to a specialized medical institution to undergo examination. Expert-guided US (performed by a specialist experience in assessment of uterine scar defects using Delphi criteria and expert-class device) makes it possible to detect with high accuracy the uterine scar defect.
It is important to note that in doubtful cases, as well as when it is necessary to take a decision about surgery and its volume, it is preferable to carry out sono- HSG that ensures high reproducibility and provides additional "navigation" information for the surgeon.При выявлении подозрения на дефект РМ после КС на амбулаторном этапе целесообразно направить пациентку на обследование в специализированное медицинское учреждение. Expert-guided ultrasound performed by the specialist who has experience in measurements of uterine scar defects using expert class machine using Delphi criteria, makes it possible with high accuracy to determine the degree of the uterine scar defect after CS.
It is important to note, that in doubtful cases, as well as in making a decision about necessity of the surgical treatment and the volume of surgery, it is preferable to carry out HSG, which has a high producibility and provides the surgeon with the additional “navigation” information about the condition of the defect area.
Further research in this filed, as well as prospective studies of uterine scar condition during pregnancy and at birth are necessary for development of modern classification of uterine scar defects after cesarean section.
References
- Donnez O. Cesarean scar defects: management of an iatrogenic pathology whose prevalence has dramatically increased. Fertil. Steril. 2020; 113(4): 704-16. https://dx.doi.org/10.1016/j.fertnstert.2020.01.037.
- Betrán A.P., Ye J., Moller A.B., Zhang J., Gülmezoglu A.M., Torloni M.R. The increasing trend in caesarean section rates: global, regional and national estimates: 1990-2014. PLoS One. 2016; 11(2): e0148343. https://dx.doi.org/10.1371/journal.pone.0148343.
- Здравоохранение в России. 2021. Статистический сборник. М.: Росстат; 2021. 171 с. [Health care in Russia. 2021. Statistical collection. M.: Rosstat; 2021. 171 p. (in Russian)].
- Краснопольский В.И., Буянова С.Н., Щукина Н.А., Логутова Л.С. Несостоятельность шва (рубца) на матке после кесарева сечения: проблемы и решения (редакционная статья). Российский вестник акушера-гинеколога. 2015; 15(3): 4-8. [Krasnopol'skiĭ V.I., Buianova S.N., Shchukina N.A., Logutova L.S. Uterine suture (scar) incompetence after cesarean section: Problems and solutions (an editorial). Russian Bulletin of Obstetrician-Gynecologist. 2015; 15(3): 4-8. (in Russian)]. https://dx.doi.org/10.17116/rosakush20151534-8.
- Мартынов С.А., Адамян Л.В. Рубец на матке после кесарева сечения: терминологические аспекты. Гинекология. 2020; 22(5): 70-5. [Martynov S.A., Adamyan L.V. Cesarean scar defect: terminological aspects. Gynecology. 2020; 22(5): 70-5. (in Russian)]. https://dx.doi.org/10.26442/20795696.2020.5.200415.
- Jordans I.P.M., de Leeuw R.A., Stegwee S.I., Amso N.N., Barri-Soldevila P.N., van den Bosch T. et al. Sonographic examination of uterine niche in non-pregnant women: a modified Delphi procedure. Ultrasound Obstet. Gynecol. 2019; 53(1): 107-15. https://dx.doi.org/10.1002/uog.19049.
- Baranov A., Gunnarsson G., Salvesen K.Å., Isberg P.E., Vikhareva O. Assessment of Cesarean hysterotomy scar in non-pregnant women: reliability of transvaginal sonography with and without contrast enhancement. Ultrasound Obstet. Gynecol. 2016; 47(4): 499-505. https://dx.doi.org/10.1002/uog.14833.
- Monteagudo A., Carreno C., Timor-Tritsch I.E. Saline infusion sonohysterography in nonpregnant women with previous cesarean delivery: the "niche" in the scar. J. Ultrasound Med. 2001; 20(10): 1105-15. https://dx.doi.org/10.7863/jum.2001.20.10.1105.
- Regnard C., Nosbusch M., Fellemans C., Benali N., van Rysselberghe M., Barlow P., Rozenberg S. Cesarean section scar evaluation by saline contrast sonohysterography. Ultrasound Obstet. Gynecol. 2004; 23(3): 289-92. https://dx.doi.org/10.1002/uog.999.
- Osser O.V., Jokubkiene L., Valentin L. High prevalence of defects in Cesarean section scars at transvaginal ultrasound examination. Ultrasound Obstet. Gynecol. 2009; 34(1): 90-7. https://dx.doi.org/10.1002/uog.6395.
- Menada Valenzano M., Lijoi D., Mistrangelo E., Costantini S., Ragni N. Vaginal ultrasonographic and hysterosonographic evaluation of the low transverse incision after caesarean section: correlation with gynaecological symptoms. Gynecol. Obstet. Invest. 2006; 61(4): 216-22. https://dx.doi.org/10.1159/000091497.
- Rasheedy R., Sammour H., Elkholy A., Fadel E. Agreement between transvaginal ultrasound and saline contrast sonohysterography in evaluation of cesarean scar defect. J. Gynecol. Obstet. Hum. Reprod. 2019; 48(10): 827-31. https://dx.doi.org/10.1016/j.jogoh.2019.05.013.
- Antila-Långsjö R., Mäenpää J.U., Huhtala H., Tomás E., Staff S. Comparison of transvaginal ultrasound and saline contrast sonohysterography in evaluation of cesarean scar defect: a prospective cohort study. Acta Obstet. Gynecol. Scand. 2018; 97(9): 1130-6. https://dx.doi.org/10.1111/aogs.13367.
- Ludwin A., Martins W.P., Ludwin I. Evaluation of uterine niche by three-dimensional sonohysterography and volumetric quantification: techniques and scoring classification system. Ultrasound Obstet. Gynecol. 2019; 53(1): 139-43. https://dx.doi.org/10.1002/uog.19181.
Received 25.01.2022
Accepted 26.03.2022
About the Authors
Tatyana A. Sidorova, PhD student at Gynecological Department, Academician V.I. Kulakov NMRC for OG&P, Ministry of Health of Russia, +7(495)438-77-83,t_sidorova@oparina4.ru, https://orcid.org/0000-0002-5508-3611, 117997, Russia, Moscow, Ac. Oparina str., 4.
Sergey A. Martynov, Dr. Med. Sci., Leading Researcher at Gynecological Department, Academician V.I. Kulakov NMRC for OG&P, Ministry of Health of Russia,
+7(495)438-77-83, s_martynov@oparina4.ru, https://orcid.org/0000-0002-6795-1033, 117997, Russia, Moscow, Ac. Oparina str., 4.
Leyla V. Adamyan, Dr. Med. Sci., Professor, Academician of RAS, Deputy Director for Science, Head of the Department of Operative Gynecology, Academician V.I. Kulakov NMRC for OG&P, Ministry of Health of Russia, l_adamyan@oparina4.ru, 117997, Russia, Moscow, Ac. Oparina str., 4.
Anna B. Letunovskaya, obstetrician-gynecologist, doctor of ultrasound diagnostics, Academician V.I. Kulakov NMRC for OG&P, Ministry of Health of Russia,
annletynovskaya@yandex.ru, 117997, Russia, Moscow, Ac. Oparina str., 4.
Yulia V. Boykova, PhD, doctor of ultrasound diagnostics, Academician V.I. Kulakov NMRC for OG&P, Ministry of Health of Russia, j_boikova@oparina4.ru,
117997, Russia, Moscow, Ac. Oparina str., 4.
Authors’ contributions: The authors of the research have made a significant intellectual contribution to this study and approved it for publication: Martynov S.A., Sidorova T.A., Letunovskaya A.B., Boykova Yu.V. – the concept and design of the study; Letunovskaya A.B., Boykova Yu.V. – organization and selection of research instrument; Sidorova T.A., Martynov S.A. – material collection and processing, statistical data collection; Sidorova T.A., Martynov S.A. – writing the text of the article; Adamyan L.A., Letunovskaya A.B., Boykova Yu.V. – editing the article.
Conflicts of interest: The authors declare that they have no conflicts of interest.
Funding: The study was conducted without attraction of financial support from the third party.
Ethical Approval: The study was approved by the local Ethics Committee of the Academician V.I. Kulakov National Medical Research Center for Obstetrics, Gynecology and Perinatology, Ministry of Health of Russia.
Patient Consent for Publication: All patients provided informed consent for the publication of their data.
Authors' Data Sharing Statement: The data supporting the findings of this study are available on request from the corresponding author after approval from the principal investigator.
For citation: Sidorova T.A., Martynov S.A., Adamyan L.V.,
Letunovskaya A.B., Boykova Yu.V. Comparison of the effectiveness of ultrasound diagnosis
in assessment of uterine scar defets after cesarean section.
Akusherstvo i Gynecologia/Obstetrics and Gynecology. 2022; 4: 132-140 (in Russian)
https://dx.doi.org/10.18565/aig.2022.4.132-140