Applying HFMEA to prevent response time delay of emergency cesarean section surgery service
Handini Diny Rachma Putri, Dewi Arlina
Background: Patient safety is crucial for enhancing hospital care quality. Many medical errors are preventable, and a high incidence of adverse events and near-misses in hospitals indicates room for improvement. The identification and mitigation of potential failure modes within a service process can prevent numerous adverse events. One effective approach involves identifying failure modes within the service process. Healthcare failure mode and effect analysis (HFMEA), based on a systems approach to problem-solving, is an important aspect of patient safety efforts. According to national quality indicators, emergency obstetric services should be capable of initiating caesarean delivery within 30 minutes of the decision to operate.
Objective: To identify failure modes in the patient service process for emergency cesarean sections and the root causes of failures in subprocesses.
Materials and methods: This qualitative study was presented descriptively and involved focus group discussions with personnel directly involved in the service process of emergency cesarean section surgery.
Results: Eleven process flows were identified in the emergency cesarean section surgery service, encompassing 16 service subprocesses, and more than 30 failure modes were discovered across all service subprocesses. Of these, five failure modes necessitated follow-up and action.
Conclusion: This study highlights five critical failure modes that require attention. This suggests the need to enhance the flow of the emergency cesarean section service process and boost the commitment of all service providers.
Auhors’ cotributions: Handini Diny Rachma Putri, Dewi Arlina – developing the concept and design of the study; Handini Diny Rachma Putri – data collection and processing, drafting the manuscript, editing of the manuscript.
Conflicts of interest: Authors declare lack of the possible conflicts of interests.
Funding: The study was conducted without sponsorship.
Ethical Approval: The study was approved by the Health Research Ethics Committee of Medical Faculty and Health Science, Universitas Muhammadiyah Yogyakarta, Indonesia.
Patients’ Consent for Publication: All respondents provided informed consent for the publication of their data.
For citation: Handini Diny Rachma Putri, Dewi Arlina. Applying HFMEA to prevent response time delay of emergency cesarean section surgery service.
Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2024; (1): 82-89 (in Russian)
https://dx.doi.org/10.18565/aig.2023.244
Keywords
The World Health Organization (WHO) estimates that 8,800 mothers died out of 4.5 million live births in 2013 [1]. Maternal mortality is a major global problem. Although maternal mortality declined in the United States, this occurred in the middle of the 20th century; this progress stalled at the end of the 20th century. Subsequently, maternal mortality increased during the early 21st century. Around the year 2000, the maternal mortality rate began to rise and has almost doubled since then. Given that at least half of maternal deaths in the US are preventable, the increase in maternal mortality in the US is both historic and alarming [2].
In the previous study mentioned, 417 datasets were obtained from 115 countries and consisted of 60,799 deaths. Approximately 73% (1,771,000 of 2,443,000) of all maternal deaths between 2003 and 2009 were due to direct obstetric causes, and deaths due to indirect causes accounted for 5–27% (672,000) of all deaths [3]. Indonesia, which has many significant social, political, and economic developments, still struggles with high maternal mortality rates. Descriptive data from the 2012 Indonesian Demographic and Health Survey (IDHS) showed that the maternal mortality rate increased significantly from 228 per 100,000 live births in 2007 to 359 per 100,000 live births in 2012 [4].
The incidence of maternal mortality in hospitals is a part of patient safety incidents that fall into the category of sentinel events. Despite the benefits of vaginal delivery compared to a caesarean section, in many cases, especially in emergency caesarean deliveries, it can substantially reduce maternal and infant mortality and morbidity [5]. Response time is defined as the time in minutes from the time a cesarean section is decided until the doctor performs the surgical incision.
The response time for category 1 cesarean section is 30 minutes, and category 2 is between 30 and 75 minutes. In general, the problems faced in meeting the response time are the preparation for surgery (from informed consent to the operating room), anesthesia consultation, patient transport to the operating room, anesthesia preparation, waiting time for the effectiveness of anesthesia to work, the presence of operating personnel (obstetrician, anesthetist, pediatrician/neonatal nurse, surgical nurse), and operating teamwork [6].
Most adverse and sentinel events are preventable. The success of prevention and system approaches lies in the ability of the system to identify potential risks, recognize events as early as possible, and establish a barrier mechanism. One method of finding failure modes in outcomes can be done by using the HFMEA, or Healthcare Failure Mode Effect and Analysis method. HFMEA is another form of FMEA commonly used in the health sector. HFMEA itself has high practicality for healthcare quality improvement and error reduction and has been widely used to improve healthcare processes in hospitals [7] .
HFMEA is an important aspect of patient safety efforts, based on a systems approach to problem solving. HFMEA aims to break the chain of events that lead to recurring problems, find underlying system-based issues that are not properly addressed, and focus on prevention rather than punishment. The Joint Commission recommends using either FMEA or HFMEA for proactive risk management, as both are easy-to-learn techniques. In addition, FMEA in particular has been used for many years in other high-risk industries and has been shown to reduce the risk of error [8].
On the basis of data from the national quality indicator achievement report in a class C hospital in 2022, the average hospital achievement value in the emergency cesarean section response time indicator was 0% in Quarter I, 63% in Quarter II, 56% in Quarter III, and 5% in Quarter IV. In February 2023, there were 3 data points on the response time of emergency cesarean section surgery with an average length of time of 116 minutes, not yet in accordance with the achievement target of ≥80%.
This study aims to identify the failure mode of a patient service process with emergency cesarean section and the cause of failure in the subprocess.
Materials and methods
This study uses the observation method conducted in one class C hospital using the HFMEA method. The method of data collection involves conducting document examinations, interviews, and group discussions involving managers and staff of hospitals, operating rooms, delivery rooms, and maternal inpatient rooms. The total number of informants was 14 people. The focus of this research is on the service process of patients with cesarean section surgery and the cause of the failure mode in each subprocess. The service process was limited to emergency cesarean section patients. Data analysis was conducted following qualitative data analysis, through the steps of data collection, data presentation, and conclusion drawing. Triangulation was done by conducting interviews again at different times and confirming through medical record documents.
Results
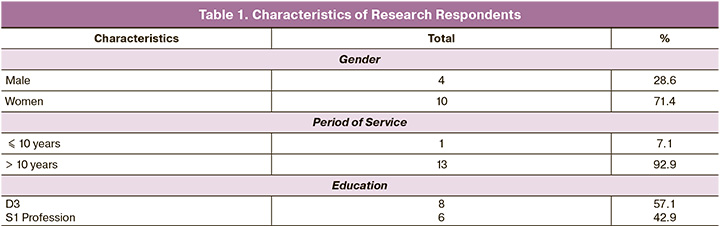
The study included fourteen respondents; there were three heads of the departments and one PONEK (Comprehensive Obstetric Neonatal Emergency Services) coordinator, five team leaders, and five executive nurses. The characteristics of the respondents can be seen in Table 1.
A total of 11 process flows of emergency cesarean section surgery were identified including 16 subprocesses. There were 33 failure modes in all sub-processes of cesarean section surgery services; the list of failure modes is shown in Table 2.
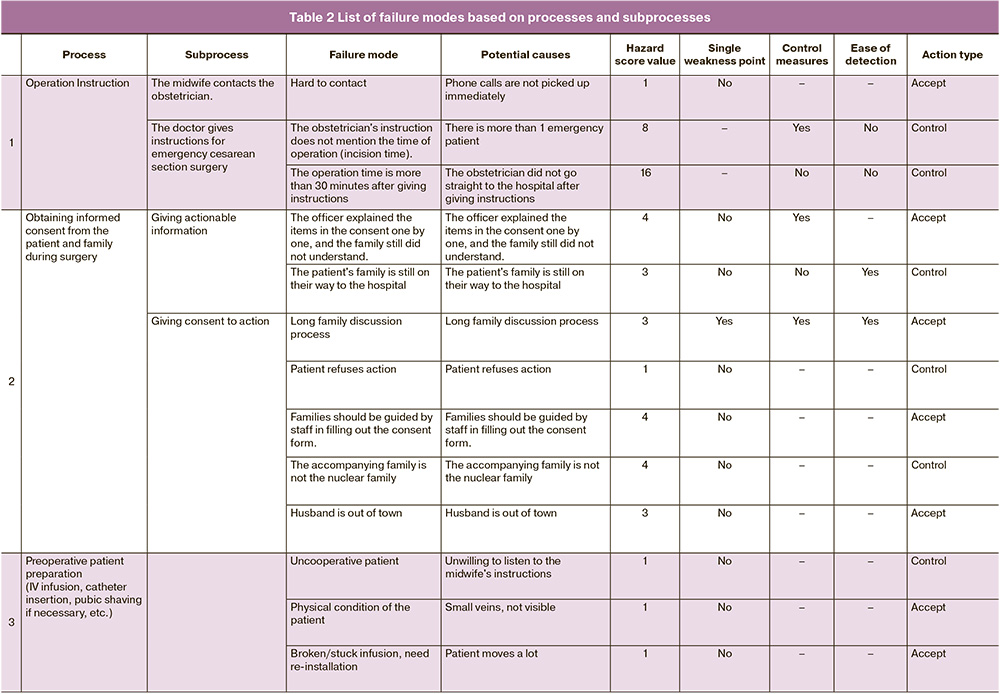
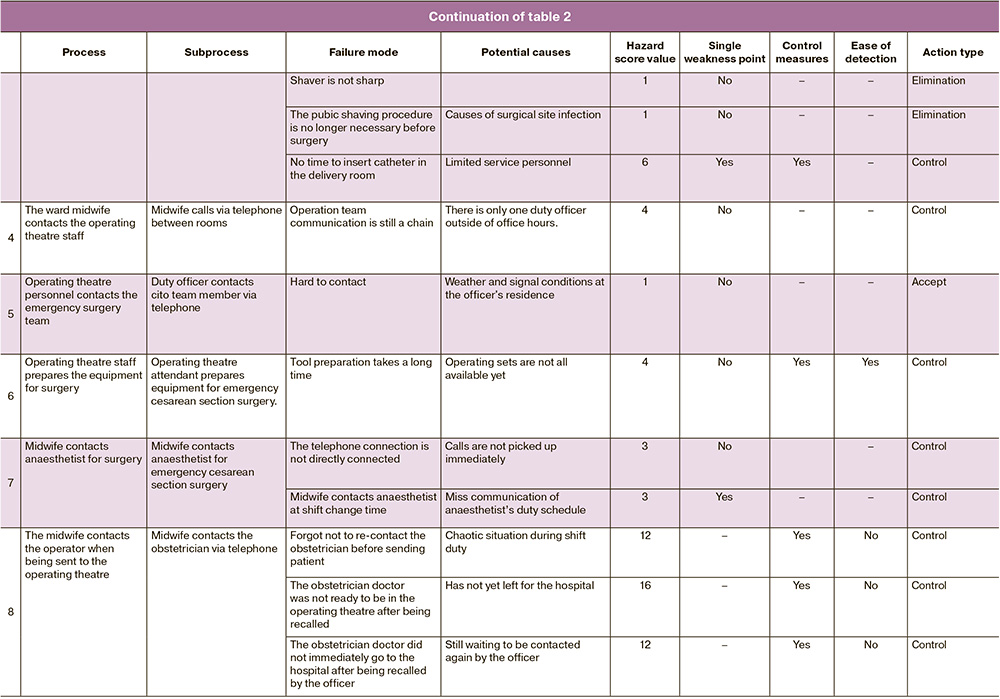
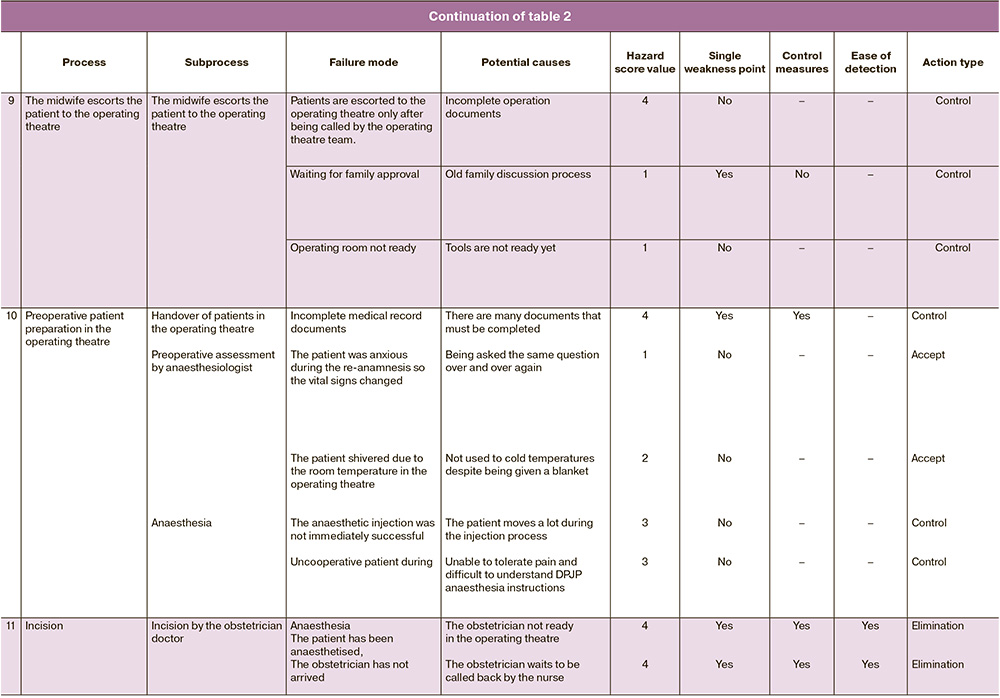
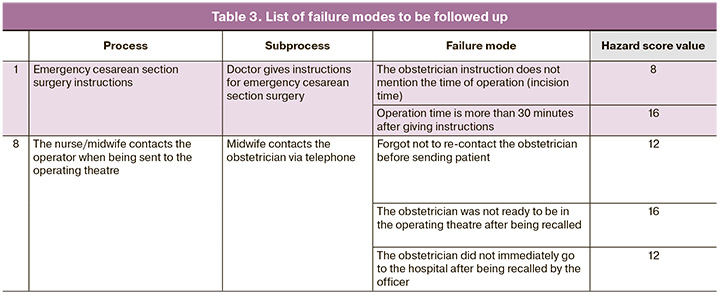
Of the 11 emergency cesarean section service process flows, there are 16 service subprocesses and 33 failure modes. A total of 5 failure modes have Hazard score values equal to or greater than 8, and 28 failure modes do not require further action based on decision tree analysis. The results of the analysis conducted by the HFMEA team found that of the 33 potential causes of failure, 28 do not need to be followed up, and 5 potential causes need to be followed up, as they were revealed in the process of emergency cesarean section surgery instructions and the process of nurses or midwives contacting the operator when being sent to the operating room. The list of failure modes to be followed is described in Table 1.3.
Discussion
Communication and transitions in patient care are the main causes of potential patient safety incidents in the surgical process. This can be prevented by redesigning the surgical patient care process and improving the work of the provider team [9]. This is in accordance with the results of a literature review study [10] that concluded that surgical safety can be realized with effective and standardized communication among health professionals during the perioperative process. According to the study, one of the key strategies to improve the transfer of information and communication (ITC) in surgical care, particularly the need for information and the method of transfer for each need, must be determined in all phases of surgical care, i.e. pre-, intra-, and post-surgery.
In this study, communication barriers were found in communication between care providers, namely nurses, midwives, and obstetricians. There were such obstacles as difficulties in the process of contacting doctors and conveying messages. In the process of handing over patients in the operating room, nurses have carried out procedures as they should, one of which is checking the completeness of the patient’s medical record documents. If the patient handover process is not carried out according to procedures, it can cause negligence, a decrease in accuracy, and cause information not to be conveyed. The Joint Commission on Accreditation of Healthcare Organizations (JCAHO) National Patient Safety Goal has established effective communication as one of the strategies to reduce adverse events in medical care [9].
The results of previous research mentioned that the FMEA method showed that the overall efficiency of surgery services in the hospital can be improved by improving list management, or rescheduling, reducing patient time, improving service flow, strengthening the Day Care Surgery Program, and establishing a pre-anesthesia clinic [11]. Health Care Failure Mode and Effect Analysis (HFMEA) is used to proactively evaluate the health care process [12]. FMEA focuses on the product manufacturing process and involves calculating a priority number of risks through a three-variable equation where each variable is given a score from one to ten. This opinion is corroborated by a literature review and according to this review FMEA demonstrated a successful team effort to evaluate high-risk procedures prospectively [13]. FMEA is an effective and useful method for assessing the likelihood of failure of a high-risk process such as drug use, although it also has drawbacks such as subjectivity, the inability to extrapolate results to other settings, and the inability to reproduce results.
In general, the problems encountered in meeting the response time were surgical preparation (from informed consent to the operating room), anesthesia consultation, patient transport to the operating room, anesthesia preparation, waiting time for anesthesia to take effect, attendance of operating personnel (obstetrician, anesthetist, pediatrician/neonatal attendant, surgical nurse), and surgical teamwork. In addition, the implementation of an on-site duty doctor was significantly associated with improved response time in obstetric emergency care [14]. The recommended response time for a caesarean section is 30 minutes in a category 1 emergency caesarean section. However, it is still very difficult to fulfill, and the reason is usually due to delays in anesthesia, an incomplete operating team, a full operating room, and the transfer of patients from the room to the operating room [15].
In cases of delivery with an emergency cesarean section, which takes more than 30 minutes from decision-making, this significantly increases the actions for newborns, one of which is the installation of intubation in newborns. In a study conducted at Dr. Sardjito Hospital, the response time of an emergency cesarean section itself, especially for category 1, is longer due to various reasons, including a full operating room, an incomplete operating team, the length of time to get anesthetic doctor approval, waiting for the perinatology team, long laboratory tests, and transferring patients from the room or emergency room to the operating room. Even in one case where the response time for category 1 emergency cesarean section was 360 minutes, this happened because the operating room was busy due to concurrent operations with surgical colleagues [16].
After identifying potential incidents and their causes, the expected actions and outcomes were identified based on the Hazard score and decision tree analysis. The expected outcomes include the commitment of all service providers in the process of emergency caesarean section surgery services. The commitment of the cesarean section service provider in this case is from the doctor in charge of patient care to fulfill the 30-minute operation response time, which aims to achieve patient safety in the hospital.
Conclusion
The process flow and subprocesses of cesarean section surgery services in this hospital have largely run according to established policies. Among the 11 process flows of emergency cesarean section services in the hospital, there are 16 subprocesses; 33 failure modes were found in all subprocesses. There are five failure modes that need follow-up.
This study suggests redesigning procedures in the process flow of cesarean section services, improving the commitment of all service providers, and establishing an onsite duty obstetrician-gynecologist to increase the speed of service response time and reduce repetitive procedures.
References
- World Health Organization, United Nations Population Fund, World Bank, United Nations Population Division & United Nations Children's Fund (UNICEF). Trends in maternal mortality: 1990 to 2013: estimates by WHO, UNICEF, UNFPA, The World Bank and the United Nations Population Division: executive summary. World Health Organization. https://iris.who.int/handle/10665/112697
- Neggers Y.H. Trends in maternal mortality in the United States. Reprod. Toxicol. 2016;64:72-6. https://dx.doi.org/10.1016/j.reprotox.2016.04.001.
- Khan K.S., Wojdyla D., Say L. Gülmezoglu A.M., Van Look P.F. WHO analysis of causes of maternal death: a systematic review. Lancet. 2006;367(9516):1066-74. https://dx.doi.org/10.1016/S0140-6736(06)68397-9.
- Indonesia 2012 DHS. Stud. Fam. Plann. 2014;45(3):399-409.https://dx.doi.org/10.1111/j.1728-4465.2014.00399.x.
- Miller J.M. Maternal and neonatal morbidity and mortality in cesarean section. Obstet. Gynecol. Clin. North Am. 2015;15(4):629-38.
- Dunn C.N., Zhang Q., Sia J.T., Assam P.N., Tagore S., Sng B.L. Evaluation of timings and outcomes in category‑one caesarean sections: A retrospective cohort study. Indian J. Anaesth. 2016;60(8):546-51. https://dx.doi.org/10.4103/0019-5049.187782.
- Liu H.C., Zhang L.J., Ping Y.J., Wang L. Failure mode and effects analysis for proactive healthcare risk evaluation: A systematic literature review. J. Eval. Clin. Pract. 2020;26(4):1320-37. https://dx.doi.org/10.1111/jep.13317.
- Thornton E., Brook O.R., Mendiratta-Lala M., Hallett D.T., Kruskal J.B. Quality initiatives: application of failure mode and effect analysis in a radiology department. Radiographics. 2011;31(1):281-93. https://dx.doi.org/10.1148/rg.311105018.
- Indiati, Wardhani V., Andarini S. Healthcare failure mode and effect analysis: proses pelayanan operasi di rumah sakit. Jurnal Manajemen Pelayanan Kesehatan. 2012;15(4):166-74.
- Nagpal K., Vats A., Lamb B., Ashrafian H., Sevdalis N., Vincent C., Moorthy K. Information transfer and communication in surgery: a systematic review. Ann. Surg. 2010;252(2):225-39. https://dx.doi.org/10.1097/SLA.0b013e3181e495c2
- Gaur K. Systematic and quantitative assessment and application of FMEA and Lean six sigma for reducing non productive time in operation theatre of a tertiary care hospital in a metropolis. Perioperative Care and Operating Room Management. 2019; 16: 100075. https://dx.doi.org/10.1016/j.pcorm.2019.100075.
- DeRosier J., Stalhandske E., Bagian J.P., Nudell T. Using health care failure mode and effect analysis: the VA National Center for patient safety’s prospective risk analysis system. Jt. Comm. J. Qual. Improv. 2002;28(5):248-67.https://dx.doi.org/10.1016/S1070-3241(02)28025-6.
- Anjalee J.A.L., Rutter V., Samaranayake N.R. Application of failure mode and effect analysis (FMEA) to improve medication safety: a systematic review. Postgrad. Med. J. 2021;97(1145):168-74. https://dx.doi.org/10.1136/postgradmedj-2019-137484.
- Ganap E.P., Hakimi M., Hadijono S., Emilia O. Impact of obstetrician/gynecologist hospitalists on response time of obstetric emergency operation in Sardjito General Hospital Yogyakarta Indonesia: a retrospective cohort study. Jurnal Kesehatan Reproduksi. 2016;3(3): 143-8.
- Le Mitouard M., Gaucher L., Huissoud C., Gaucherand P., Rudigoz R.-C., Dupont C., Cortet M. Decision-delivery intervals: Impact of a colour code protocol for emergency caesareans. Eur. J. Obstet. Gynecol. Reprod. Biol. 2020;246:29-34. https://dx.doi.org/10.1016/j.ejogrb.2019.12.027.
- Gunawan T., Attamimi A., Pradjatmo H. Hubungan response time seksio sesarea emergensi kategori 1 dengan luaran perinatal di RSUP Dr. Sardjito. Jurnal Kesehatan Reproduksi. 2018;5(1):60-71. https://dx.doi.org/10.22146/jkr.37997.
Received 17.10.2023
Accepted 09.11.2023
About the Authors
Diny Rachma Putri Handini, Master of Hospital Administration, Universitas Muhammadiyah Yogyakarta, Yogyakarta, Indonesia, dinyrachma@gmail.com,https://orcid.org/0009-0003-5093-2287
Arlina Dewi, Master of Hospital Administration, Universitas Muhammadiyah Yogyakarta, Yogyakarta, Indonesia, dewikoen@gmail.com, https://orcid.org/0000-0002-5265-591