Экономические аспекты последствий своевременно и адекватно не скорректированного дефицита железа у беременных заслуживают рассмотрения прежде всего в силу широкой распространенности этого патологического состояния: достаточных запасов железа к моменту наступления беременности не имеют 50–60% женщин [1], в процессе ее прогрессирования – от 15% до 80% [2], в послеродовом периоде – до 36,0% [3]. И если у женщин с клиническими проявлениями анемии риски течения и исходов беременности так или иначе оцениваются, то сравнимый по рискам, но практически не контролируемый в рутинной дородовой практике железодефицит коррекции не подвергается.
Распространенность дефицита железа определяет масштаб социально-экономических потерь, обусловленных этим состоянием нездоровья женщин при беременности и в родах. Соответственно, учитывая, что большинство железодефицитных состояний являются обратимыми и в 94% случаев могут быть скорректированы патогенетическим лечением [4], весомыми аргументами в пользу более активных действий по диагностике, профилактике и лечению железодефицита в акушерстве могут стать оценка потенциально предотвращаемого социально-экономического ущерба общества и расчет возможной прикладной выгоды здравоохранения в случае своевременного выявления и коррекции дефицита железа: за счет минимизации риска кровотечений/кровопотери, снижения/исключения трансфузий компонентов крови, сокращения числа дней пребывания беременных/родильниц в стационаре, уменьшения неблагоприятных отдаленных последствий для матери и новорожденного [5–9]. Согласно данным зарубежных исследователей [10, 11], потенциальная рентабельность целевых профилактических и лечебных мероприятий, обеспечиваемая совокупностью достигаемых результатов, может быть столь существенной, что в условиях относительно низких расходов на здравоохранение в РФ (2020 г. – 4,4% ВВП)1 и с учетом государственной установки на эффективное использование ресурсов2 не может и не должна игнорироваться.
Цель исследования: оценить потенциальные страновые и прикладные выгоды здравоохранения при переходе от сложившейся к оптимизированной практике3 коррекции дефицита железа/железодефицитной анемии (ДЖ/ЖДА) у беременных.
Материалы и методы
Оценку потенциального ущерба от исходов беременностей, протекавших с ДЖ/ЖДА, проводили в рамках концепции Глобального бремени болезней (Global Burden of Disease, GBD [12]) по методике, подробно описанной авторами в одной из предыдущих статей [13]. При моделировании потенциально предупрежденных потерь посредством своевременной и адекватной терапевтической коррекции дородового железодефицита исходили из понимания, что таковая является составляющей комплекса мероприятий менеджмента крови пациентов (МКП), сфокусированных на устранении дефицита железа, предотвращении потери крови, оптимизации физиологической переносимости анемии [14]. За основу брали расчетные удельные потери на один случай заболевания/состояния по причине дефицита железа/анемии у женщин старше 15 лет в 2019 г.: в расчетах с позиции понесенного ущерба – российские (YLD’=0,26), в расчетах с позиции потенциально предупрежденного ущерба (модельные) – германские (YLD’=0,014)4.
Модельная оценка прикладных выгод здравоохранения в случае дородовой коррекции дефицита железа была проведена в отношении потенциально предупрежденных расходов родовспомогательных учреждений, связанных с трансфузиями компонентов крови и увеличением продолжительности пребывания в стационаре родильниц, у которых анемия явилась причиной осложненных родов. Материалом для анализа послужили данные медицинских карт 292 беременных с диагностированной железодефицитной анемией, поступивших на роды в Перинатальный центр ГБУЗ «ККБ № 2» (Краснодар) и ГБУЗ НО «Дзержинский перинатальный центр» (Дзержинск, Нижегородская область) в течение второго полугодия 2019 г. и первого полугодия 2020 г. По причине очевидной зависимости оцениваемых показателей от способа родоразрешения часть расчетов проводили дифференцированно для родов через естественные родовые пути (183/292 (62,67%)) и посредством кесарева сечения (109/292 (37,3%)). Результаты расчетов в выборке позволяют оценить всю исследуемую совокупность (518 671/1 440 574 (36%) беременных с анемией от родов, принятых в РФ в 2019 г. [3]). Все расчеты проводились с помощью табличного редактора EXCEL и пакета прикладных программ STATISTICA.
Результаты
Из числа поступающих на родоразрешение с диагнозом анемии в 26 случаях (8,9%) она фиксируется на протяжении всех трех триместров. В I триместре диагноз анемии впервые выставляется у 28/292 беременных (9,6%), во II – у 113/292 беременных (38,7%), в III – у 151/292 (51,7%). С диагнозом анемии средней тяжести (умеренной) на роды поступают 12,3% беременных, при этом непосредственно перед родоразрешением концентрация гемоглобина ниже 100 г/л отмечается у 41,1% женщин, а концентрация сывороточного ферритина, в тех случаях, когда проводится его определение (23,3%), всегда ниже 30 мкг/л (табл. 1).
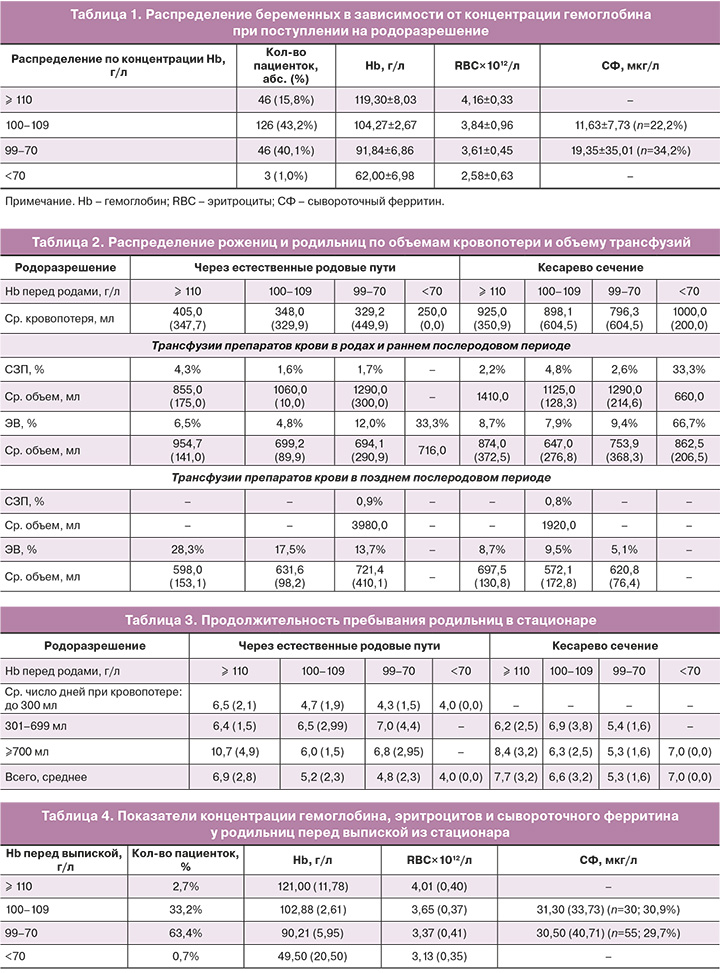
Средний объем кровопотери при родах через естественные родовые пути составляет 348,91±387,65 мл, при кесаревом сечении – 832,57±520,29 мл. Объем переливаемых компонентов крови в тех случаях, когда трансфузии проводится, составляет в среднем 728,83±247,36 мл эритроцитной взвеси (ЭВ) и 1068,33±267,98 мл свежезамороженной плазмы (СЗП) при самостоятельных родах (13,11%) и соответственно 701,56±292,57 мл и 1116,67±209,13 мл при кесаревом сечении (25,7%) – результаты представлены в таблице 2.
Данные таблицы 3 указывают на тот факт, что различия в длительности пребывания родильниц в стационаре при естественных родах (5,30±2,49) и кесаревом сечении (6,28±2,84) составляют в среднем около 1,0 дня (95% ДИ [0,91;1,06], уровень значимости р<0,055).
На момент выписки послеродовая анемия у большинства родильниц (97,3%) остается нескорректированной: в 64,1% случаев выписка проводится при показателях гемоглобина ниже 100 г/л, о чем свидетельствуют данные таблицы 4.
При оценке актуальных и потенциально предупрежденных расходов родовспомогательных учреждений на ведение рожениц и родильниц с анемией исходили из ряда статистических данных, предпосылок и допущений.
1. Среднероссийский показатель анемии беременных – 36% (518 671 случаев); анемии как заболевания, приведшего к осложнениям в родах и послеродовом периоде, – 26,3% (136 410 случаев) [3].
2. 362 946 (70%) женщин с анемией рожают через естественные родовые пути, 155 726 (30%) – посредством кесарева сечения (расчеты по данным [3]).
3. Средняя длительность пребывания в стационаре родильниц без анемии: 3,5 дня – при самостоятельных родах, 5,0 дня – при кесаревом сечении (локальные данные); из общего числа осложнений в послеродовом периоде превышение указанных значений в 83,2% случаях расценивалось как обусловленное осложнениями по причине анемии, но не связанное с трансфузиями компонентов крови; при расчете понесенных расходов в этой группе исходили из условной тарифной стоимости лечения осложнений в послеродовом периоде 13 141,43 руб.6, умноженной на число родильниц, превысивших среднюю длительность пребывания в стационаре; полученные значения одновременно расценивались как потенциально предупрежденные расходы в случае исключения осложнений при адекватной дородовой коррекции ДЖ/ЖДА.
4. Трансфузии плазмы и эритроцитной взвеси проводятся в родах и раннем послеродовом периоде в 16,1% случаев с анемией; средняя стоимость 1 л любого компонента крови условно принималась равной средней стоимости 1 л цельной крови – 16 589,92 руб. [15]; при расчете стоимости компонентов крови исходили из средних объемов трансфузий и их расчетной стоимости на одного реципиента; понесенные в связи с трансфузиями расходы одновременно расценивались как потенциальная экономия в случае их исключения при адекватной дородовой коррекции ДЖ/ЖДА.
Оценка понесенного/предупрежденного социально-экономического ущерба
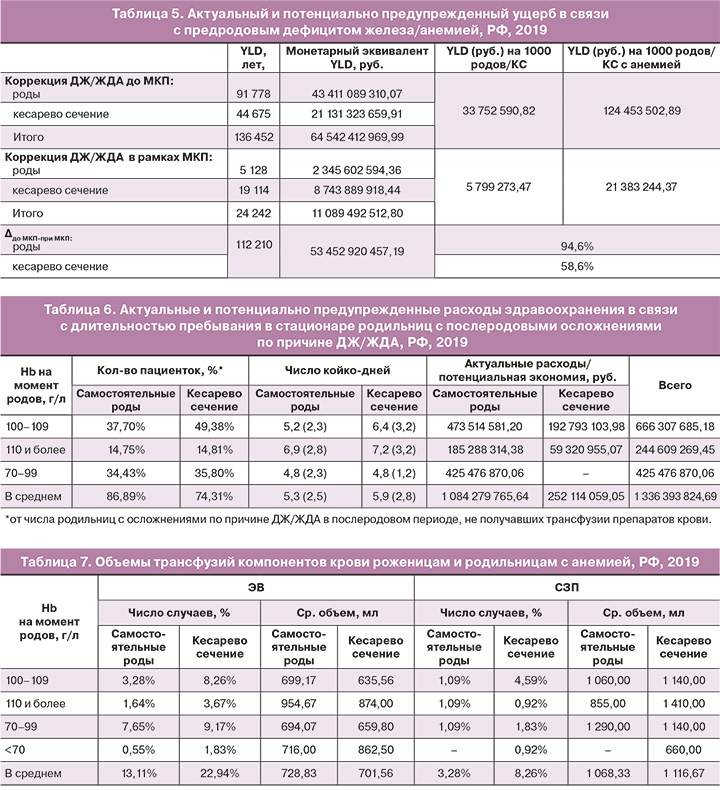
Согласно проведенным расчетам, актуальный ущерб (YLD7), рассчитанный для годового числа родов с дефицитом железа/анемией у 36% беременных, потенциально составляет более 136,5 тыс. потерянных лет жизни и 64,5 млрд руб. в их монетарном выражении – данные представлены в таблице 5. При этом высокие удельные потери на каждую тысячу родов/КС с сопутствующими ДЖ/ЖДА предопределяют высокие удельные потери на все роды, принятые в 2019 г. В случае проведения комплексных мероприятий МКП, позволяющих аналогично модельным расчетам снизить коэффициент YLD’ с 0,26 до 0,014, суммарные потери (лет жизни и их монетарного выражения) могут уменьшиться в 5,6 раза. Соответственно, потенциально предупрежденный годовой социально-экономический ущерб от дефицита железа/анемии, осложняющих беременность и роды, может составить более 112,2 тыс. лет жизни, или 53,5 млрд руб. в монетарном выражении.
Прикладная экономика: оценка влияния коррекции ДЖ/ЖДА на отдельные показатели здравоохранения
В случае каких-либо осложнений в послеродовом периоде в связи с ДЖ/ЖДА 94,6% женщин из рожающих самостоятельно и 58,6% из родоразрешаемых кесаревым сечением находятся в стационаре дольше, чем в среднем родильницы с анемией, но без опосредованных ею осложнений. В зависимости от выраженности анемии на момент родов среднее число дней до выписки составляет 5,30 при не потребовавших трансфузий родах через естественные родовые пути и 5,89 при не потребовавших трансфузий операциях кесарева сечения. Согласно примененному в расчетах тарифу законченного случая лечения осложнений в послеродовом периоде, суммарные дополнительные расходы здравоохранения составляют 1,34 млрд руб. Эту же сумму следует считать потенциально сэкономленной при ненаступлении осложнений по причине ДЖ/ЖДА, удлиняющих пребывание родильниц в стационаре сверх средних показателей. Актуальные и потенциально предупрежденные расходы здравоохранения представлены в таблице 6.
В родах и раннем послеродовом периоде трансфузии компонентов крови пациентам с анемией проводятся в 16,4% случаев при самостоятельных родах и в 22,9% случаев при кесаревом сечении с общим соотношением числа трансфузий эритроцитной взвеси и свежезамороженной плазмы 6,9/1. С вариациями по исходной концентрации гемоглобина крови и способу родоразрешения средний объем вводимой ЭВ составляет 714,92±271,71 мл, СЗП – 1 097,33±235,64 мл. Объемы переливаемых компонентов крови представлены в таблице 7. Несоразмерность средних объемов трансфузий ЭВ у рожениц/родильниц и показателей Hb (110 и <70 г/л – 954,67 и 716,00 мл соответственно) объясняется различными клиническими ситуациями, определяющими потребность в компонентах крови.
Исходя из расчетной стоимости компонентов крови на одного реципиента, суммарные расходы на проведение трансфузий составляют более 1,2 млрд руб. Эту же сумму следует считать потенциально сэкономленной при отсутствии необходимости проведения 248 690 трансфузий и неизрасходованных в этой связи 72 473 л крови в случае своевременной коррекции дородового дефицита железа. Полученные результаты представлены в таблице 8.

Таким образом, потенциально понесенные расходы здравоохранения только по двум оцененным параметрам могут составить более 2,5 млрд руб. (1 762 млн руб. на 1000 родов). При адекватной дородовой коррекции ДЖ/ЖДА предупрежденные удельные расходы здравоохранения за счет сокращения продолжительности пребывания родильниц в стационаре могут достичь 927 681,48 руб., за счет исключения трансфузий в родах и раннем послеродовом периоде – 834 608,87 руб.
Обсуждение
Каждый неэффективный элемент системы здравоохранения может быть приравнен к нерациональному расходованию ресурсов, поскольку, увеличивая расходы здравоохранения и ухудшая здоровье напрямую затронутых пациентов, имеет следствием повышение социально-экономического ущерба [18]. Результаты проведенного исследования позволяют утверждать, что к подобным элементам следует отнести несвоевременную и/или неадекватную коррекцию ДЖ/ЖДА у беременных. Широкая распространенность и тяжесть последствий этого патологического состояния обеспечивают весьма значительный вклад в потенциальные ежегодные потери общества: 136,5 тыс. лет жизни и 64,5 млрд руб. в их денежном выражении.
Поскольку принципиальное изменение сложившейся ситуации может быть достигнуто посредством адекватно подобранной и своевременно выполненной патогенетической терапии, правомерно говорить о недостаточной клинической эффективности текущей практики ведения беременных с дефицитом железа/анемией и экономической нецелесообразности применяемых в настоящее время медицинских технологий по его коррекции. Это актуализирует необходимость скорейшего внедрения в медицинскую практику комплекса мероприятий по индивидуальному управлению кровью пациентов, результирующим итогом которых может стать предупреждение расчетного ущерба и обеспечение страновых выгод: монетарный эквивалент удельных (на 1 000 случаев) потерь потенциально снизится на 94,6% при самостоятельных родах и на 58,6% при кесаревом сечении, а общий социально-экономический ущерб – в 5,6 раза.
Более эффективные в контексте лечения железодефицитных состояний медицинские технологии могут оказать позитивное влияние на финансово-экономическую составляющую здравоохранения, снизив/исключив потенциальное потребление ресурсов и эксплуатационных расходов. Согласно расчетам, адекватная дородовая коррекция ЖД/ЖДА позволит сократить длительность пребывания части родильниц в стационаре, исключив тем самым дополнительные расходы здравоохранения на 1,34 млрд руб. Снижение расходов обеспечат также предупрежденные 248 690 трансфузий с не израсходованными в этой связи 72 473 л компонентов крови стоимостью 1,20 млрд руб.
Следует оговориться, что модельные расчеты прикладных выгод здравоохранения могут не принести реальных дополнительных доходов, поскольку использованная для расчетов тарифная стоимость лечения осложнений по причине анемии в послеродовом периоде на практике не суммируется с тарифной стоимостью родоразрешения. Соответственно, лечение родильниц в период их пребывания в стационаре в подавляющем большинстве случаев обеспечивается за счет собственных средств родовспомогательных учреждений, которые стремятся ограничить расходы до суммы, сопоставимой с оплатой одного законченного случая (т.е. родов), или достичь экономии в рамках других лечебных мероприятий.
Подобная практика, при которой оказанные услуги не возмещаются страховыми организациями, имеет очевидным следствием скорейшую выписку родильниц из стационаров даже при неадекватно восстановленных показателях гемоглобина (33,2% родильниц выписываются при концентрации Hb в крови менее 110 г/л, 64,1% – менее 100 г/л), т.е., по сути, с послеродовой анемией и очевидным железодефицитом, что в перспективе еще больше повышает потенциал социально-экономического ущерба. Кроме того, некомпенсируемые больничные расходы затрудняют закупки экономически более выгодных медицинских технологий, прежде всего препаратов железа для внутривенного введения взамен чреватых риском осложнений трансфузий препаратов крови, поставляемых центрами переливания крови. Однако даже с учетом этой пока не решенной проблемы очевидно, что в случае дородовой коррекции ДЖ/ЖДА бóльшая часть затрачиваемых в настоящее время на преодоление последствий анемии средств родовспомогательных учреждений не будет востребована.
Заключение
Проведенное исследование выявило сохраняющуюся актуальность проблемы дефицита железа/анемии у беременных/рожениц/родильниц, преобладание нерациональных практик ее устранения, невнимание к экономическим аспектам применяемых медицинских технологий. Представляется, что скорейшее решение проблемы дородового дефицита железа посредством своевременной диагностики, индивидуального подбора и способа введения железосодержащих препаратов обеспечит снижение общественных потерь. Этот комплекс мероприятий, являющийся одним из трех столпов концепции менеджмента крови пациента, в случае его реализации в предродовом/предоперационном периодах позволит повысить качество оказания медицинской помощи в акушерстве и сэкономить ресурсы здравоохранения.