Анализ научной литературы не позволяет дать однозначную оценку роли пудендальной нейропатии в патогенезе пролапса тазовых органов. Опубликованные данные расходятся как по частоте встречаемости нейропатии при тазовом пролапсе, так и по возможности ее влияния на патогенетические звенья анальной инконтиненции.
Ряд авторов придерживаются точки зрения наличия корреляции между нейропатией полового нерва и тазовым пролапсом (генитальным и/или ректальным).
Так, Pfeifer J. и соавт. [1] при ретроспективном анализе результатов исследования латентного периода проведения возбуждения по двигательным волокнам полового нерва (Pudendal Nerve Terminal Motor Latencies, PNTML) более чем у 1000 пациентов обнаружили двукратное увеличение частоты пролонгированного PNTLM при ректальным пролапсе по сравнению с инконтиненцией, хроническими запорами и тазовой болью. Osterberg A. и соавт. [2] (2000) диагностировали увеличение латентности полового нерва у пациентов с ректальным пролапсом (как полным выпадением, так и внутренней ректальной инвагинацией) в 66% случаев. В то же время Birnbaum E.H. и соавт. [3] приводят данные о наличии пудендальной нейропатии только у 25% пациентов с полным выпадением прямой кишки.
Согласно Roig J.V. и соавт. [4], латентность полового нерва была значимо большей в группе пациенток с полным ректальным пролапсом и инконтиненцией, чем у здоровых женщин.
В исследовании Lubowski D.Z. и соавт. [5] значимо увеличенная PNTML была выявлена у пациентов с опущением промежности. Также и Laurberg S. и соавт. [6] отмечают, что показатели PNTML были значимо выше у женщин старше 50 лет с опущением промежности по данным перинеометрии.
Bakas P. и соавт. [7] выявили, что существует статистически значимая разница в показателях латентности в группе пациенток с генитальным пролапсом и стрессовым недержанием мочи по сравнению со здоровыми добровольцами.
По данным Kiff E.S. и соавт. [8], у 11 пациенток с синдромом опущения промежности и длительным анамнезом затрудненного опорожнения латентный период 2,8 (0,5) мс был статистически значимо больше, чем у здоровых добровольцев.
Согласно Beevors M.A. и соавт. [9], PNTML была значимо увеличена у пациенток с ректоцеле по сравнению с контрольной группой без ректоцеле.
Интересно в аспекте изучения изменения латентности полового нерва с возрастом и наличием родов исследование Boyle D.J. и соавт. [10]. Не делая акцент на наличии пролапса тазовых органов, авторы отмечают увеличение латентности полового нерва с возрастом и особенно вследствие вагинальных родов, при этом наиболее значимым оказалось воздействие на левый нерв.
Snooks S.J. и соавт. [11] также отмечают, что 9/15 (60%) пациенток при солитарной язве прямой кишки имели увеличенный латентный период проведения по двигательным волокнам n. pudendus в среднем до 2,8 мс как результат повреждения терминальных ветвей полового нерва. Авторами даже высказано предположение, что нарушение иннервации наружного сфинктера и пуборектальной мышцы приводит первично к ослаблению мышц тазового дна.
По данным других авторов, корреляции пролапса тазовых органов и пудендальной нейропатии не отмечается.
Так, в исследовании Tetzschner T. и соавт. [12], симптомы опущения промежности и длительность латентного периода не были связаны. Авторы не согласны с теорией прогрессирования пудендальной нейропатии с возрастом на основании результатов проведенного исследования у женщин постменопаузального возраста.
По данным Ryhammer A.M. и соавт. [13], латентность значительно увеличивается с числом перенесенных родов (от 0 до 6 родов), однако связи между увеличением латентности полового нерва и опущением промежности обнаружено не было.
В работах Jorge J.M. и соавт. [14] (у пациенток с запорами, недостаточностью анального сфинктера (НАС) и с хронической тазовой болью) предпринята попытка выявить взаимосвязь между тазовой дисфункцией, диагностируемой по данным дефекографии, и нейропатией полового нерва, определяемой по результатам стимуляционой электромиографии (ЭМГ) – корреляции выявлено не было.
Нет единого мнения в литературе и о значении пудендальной нейропатии для выбора тактики лечения пациентов.
В исследовании Cooper EA. и соавт. [15] «пудендальная нейропатия, проявляющаяся увеличением латентности полового нерва», по данным анализа карт 398 пациентов с недержанием кала, отмечалась у 79% больных, а полное выпадение прямой кишки выявлено у 31%. При этом, по данным статистического анализа, полное выпадение прямой кишки являлось независимым предиктором хирургического лечения, в то время как пудендальная нейропатия – нет.
А по данным Cannon J.A. и соавт. [16], место PNTML при полном ректальном пролапсе – в прогнозировании частоты анальной инконтиненции в послеоперационном периоде.
Birnbaum E.H. и соавт. [3] также утверждают, что после проведения оперативного лечения выпадения прямой кишки необходимо проводить PNTML с целью прогнозирования НАС в послеоперационном периоде. Данный вывод был получен по результатам собственного исследования, в котором указывалось, что 83% пациентов с билатерально увеличенной латентностью страдали инконтиненцией и в 38% случаев при монолатеральном увеличении латентности также наблюдалась НАС; в то же время только 20% с нормальной латентностью имели признаки недержания. Нейропатия полового нерва способствует, по мнению авторов, возникновению послеоперационной НАС после коррекции ректального пролапса.
Таким образом, следует констатировать, что в настоящее время не существует определенного мнения о роли пудендальной нейропатии в патогенезе анатомо-функциональных нарушений, возникающих у пациенток с синдромом опущения тазового дна.
В связи с этим целью нашей работы было оценить наличие пудендальной нейропатии и ее возможную роль в патогенезе недержания кишечного содержимого у пациенток с пролапсом тазовых органов.
Материалы и методы
За период 2015–2019 гг. в ФГБУ «ГНЦК им. А.Н. Рыжих» Минздрава России были обследованы 52 пациентки с пролапсом тазовых органов. Из ГБУЗ МО «Московский областной НИИ акушерства и гинекологии» были направлены 25/52 (48,1%) больных с генитальным пролапсом.
Все пациентки предъявляли жалобы на выпадение матки и/или стенок влагалища. При этом у 6/25 (24%) женщин, перенесших ранее тотальную/субтотальную гистерэктомию, отмечалось выпадение купола/свода влагалища, у остальных 19/25 (76%) гинекологические операции в анамнезе отсутствовали. Средний возраст пациенток составил 56,1 (10) года, величина распределена нормально. Одни роды были у 6/25 (24%), двое родов – у 17/25 (68%), трое – у 2/25 (8%). Жалобы на недержание различных компонентов кишечного содержимого предъявляли 19/25 (76%) пациенток. Для субъективной оценки жалоб на НАС использовали Шкалу оценки недержания по Wexner [17, 18].
Наружное выпадение прямой кишки (K62.3) имелось у 27/52 (51,9%) обследованных пациенток: средний возраст 58,6 (17,6) года, распределение нормальное, при этом 2 пациентки были ранее оперированы по поводу выпадения прямой кишки, в двух наблюдениях ректальный пролапс сочетался с выпадением матки. В анамнезе 3/27 (11,1%) пациентки перенесли гистерэктомию, 5/27 (18,5%) – промежностные операции по коррекции генитального пролапса. Рожавших женщин было 22/27 (81,5%): 1 роды – 5/22 (22,7%), 2 родов – 14/22 (63,6%), 3 родов и более – 3/22 (13,6%). Жалобы на недержание компонентов кишечного содержимого предъявляли все пациентки данной группы.
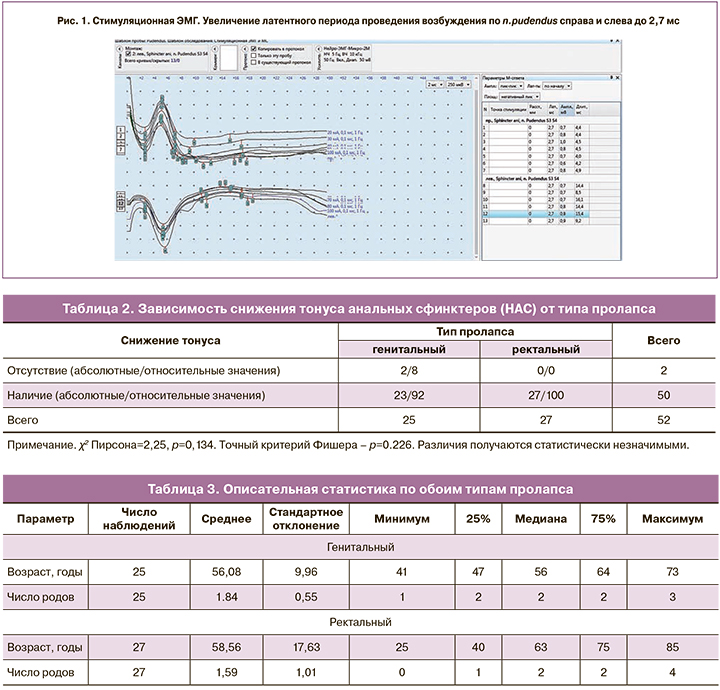
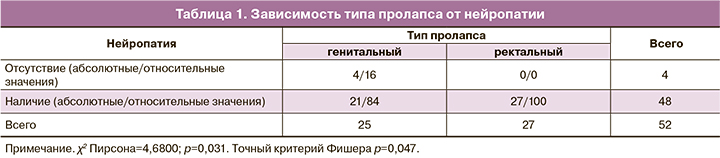
Для диагностики пудендальной нейропатии использовали метод стимуляционной интравагинальной ЭМГ с помощью электрода Св. Марка на электромиографе «Нейро-ЭМГ-Микро», «Нейрософт», Россия. Данный метод нейрофизиологической оценки состояния мышц тазового дна заключается в регистрации моторного ответа мышц тазового дна и/или наружного сфинктера в ответ на электрическую стимуляцию полового нерва с определением латентного периода проведения возбуждения по двигательным волокнам n. pudendus. Норма при интравагинальном расположении электрода Св. Марка составляет 1,54–2,55 мс, при интраректальном – 1,8–2,2 мс [12, 19].
Увеличение латентности свидетельствовало о патологии нерва и, по нашему мнению, было обусловлено процессами частичной демиелинизации нервных структур.
Для диагностики НАС использовали разработанный в ФГБУ «ГНЦК им. А.Н. Рыжих» Минздрава России метод комплексной сфинктерометрии (Патент РФ № 2576445 от 05.02.2016) на аппарате WPM Solar (MMS, Голландия), при котором обращали внимание на значение показателей давления в покое и при волевом сокращении сфинктера [20–23].
Для статистического анализа данных использовали статистический пакет Stata 11.2 (StataCorp). Для оценки влияния наличия нейропатии на развитие ректального или генитального пролапса в работе использовался критерий χ2 Пирсона для четырехпольных таблиц сопряженности, который позволяет оценить статистическую значимость различий двух относительных показателей (встречаемости нейропатии в случае с ректальным и генитальным пролапсом). Был применен данный непараметрический метод, так как сопоставляемые показатели были измерены в номинальной шкале (тип пролапса: ректальный или генитальный, наличие или отсутствие нейропатии – в обоих случаях переменные принимали только 2 возможных значения). В связи с тем что наши выборки были довольно малочисленными, дополнительно в работе использовался двусторонний точный критерий Фишера для оценки статистической значимости упомянутых выше различий, так как в медицинской статистике данный критерий применяется в случае значений ожидаемого явления менее 5 хотя бы в 1 ячейке.
Для сравнения групп пациенток с ректальным и вагинальным пролапсом по возрасту и количеству родов (другими словами, для оценки возможной связи возраста и числа родов с развитием ректального или генитального пролапса) в работе использовали U-критерий Манна–Уитни. Дело в том, что в условиях небольшого числа наблюдений использование непараметрического теста и, как следствие, отказ от предположения о нормальности распределения и одинаковых дисперсий (условие для применения t-критерия Стьюдента для проверки равенства средних значений в двух выборках) в пользу U-критерия представляется разумным предположением.
В данной работе мы останавливаемся на 5% уровне значимости для определения значимости различий (р<0,05).
Форматы описательной статистики представлены следующим образом:
- для количественных данных, имеющих нормальное распределение, используется формат М (SD), где М – среднее арифметическое; SD – стандартное отклонение;
- для количественных данных с распределением, отличающимся от нормального, представлены медиана (Me) и квартили первый (Q1) и третий (Q3) в формате Me (Q1; Q3).
Результаты
В результате проведенной стимуляционной ЭМГ у 25/52 пациенток с генитальным пролапсом мы установили, что латентность была увеличена с двух сторон (рис. 1) у 16/25 (64%) пациенток: в среднем до 3,7 (1,36) мс справа и 3,7 (1,0) мс слева, однако справа распределение ненормальное, следовательно, медиана 3,1 (2,5; 3,7). При этом 15/16 пациенток отмечали жалобы на недержание кишечного содержимого – 5,6 (2,0) балла по шкале Wexner (нормальное распределение по тесту Шапиро–Уилка, р=0,07), а показатели сфинктерометрии у них составили в среднем 32,7 (4,5) и 104,9 (36,7) мм рт. ст. В то же время 1/16 пациентка не имела жалоб на НАС (0 баллов по шкале Wexner), однако ее показатели давления в покое оказались сниженными до 37 мм рт. ст. (латентная форма анальной инконтиненции).
Увеличение латентности с одной из сторон было отмечено у 5/25 (20%) пациенток. При этом 2 из них не имели жалоб на недержание – 0 по шкале Wexner, однако у 1 из них отмечались сниженные показатели тонуса до 31 мм рт. ст., что можно расценивать как латентную форму анальной инконтиненции. У 3 пациенток были жалобы на недержание – 3–5 баллов по шкале Wexner, и их сфинктерометрические показатели в покое и при волевом сокращении были также снижены (в пределах 29–28 мм рт. ст. и 46–105 мм рт. ст. соответственно).
У 4/25 (16%) показатели латентного периода проведения возбуждения по двигательным волокнам n. pudendus были в пределах нормы: 2,3 (2,13; 2,48) мс справа и 2,2 (2,05; 2,35) слева (рис. 2). При детальном анализе было установлено, что 1 пациентка имела жалобы на периодическое недержание газов (4 балла по шкале Wexner). По данным сфинктерометрии ее показатели в покое составили 39 мм рт. ст., что соответствует I степени анальной инконтиненции; у 3 пациенток жалоб на недержание не было – 0 баллов по шкале Wexner, однако только у одной из них показатели сфинктерометрии были в пределах физиологических норм, в то время как у 2 других снижены в покое до 34 и 35 мм рт. ст., что говорило о латентной форме анальной инконтиненции.
Среди пациенток с выпадением прямой кишки с обеих сторон латентность была увеличена у 24 (88,9%) женщин – справа до 3,2 (0,5) мс, слева – до 3,6 (0,9) мс.
Манометрические показатели в покое были значительно снижены у всех пациенток и составили в среднем 21,5 (6,6) мм рт. ст. Все они имели жалобы на недержание компонентов кишечного содержимого. Средний балл по шкале Wexner составил 15,0 (4,6) баллов.
Увеличение латентности с одной из сторон выявлено у 3 (11,1%) пациенток. При этом показатели сфинктерометрии у них были снижены в покое до 14–31 мм рт. ст. Оценка по шкале Wexner колебалось от 12 до 20.
Нормальных показателей времени проведения по n. pudendus в этой группе отмечено не было.
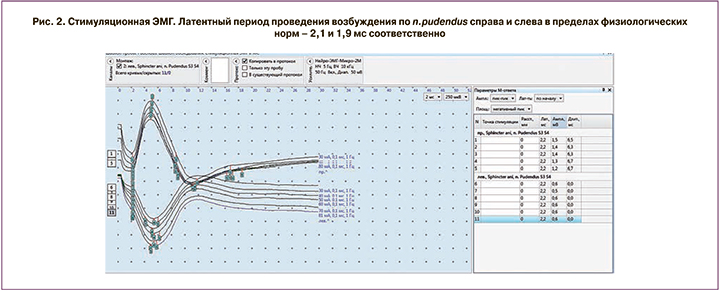
Мы провели сравнительный статистический анализ зависимости наличия нейропатии от типа пролапса (табл. 1). В таблицах приводятся абсолютные (число наблюдений) и относительные (процент наблюдений от данного типа пролапса)
Как показывают результаты статистических тестов, различия значимые. Нейропатия чаще встречается при ректальном пролапсе (во всех 27 случаях наблюдалась нейропатия). При генитальном пролапсе в 16% случаях (4/25) нейропатия отсутствует.
Далее мы проанализировали зависимость снижения тонуса анальных сфинктеров (признак НАС) от типа пролапса (табл. 2).
Анализируя полученные результаты, нельзя однозначно сказать, являются ли различия в снижении тонуса сфинктерного аппарата для разных типов пролапса случайными или между показателями существует закономерность. Важно, что ректальному пролапсу всегда сопутствуют нейропатия и снижение тонуса. В случае же с генитальным пролапсом возможно и наличие нормального тонуса.
Относительно наличия нейропатии – различия между типами пролапса получились статистически значимые.
Следующим этапом мы оценили зависимость пролапса разных типов от возраста и числа родов пациенток (табл. 3).
В случае с ректальным пролапсом наблюдается значительно большее стандартное отклонение при небольших различиях в средних как для показателя возраста, так и для показателя числа родов (то есть характеристики пациенток в данном случае более разнородны по сравнению с пациентками с генитальным пролапсом). U-критерий Манна–Уитни, тем не менее, не выявил значимых различий между возрастом пациенток с ректальным и генитальным пролапсом (р=0,36), а также числом родов, наблюдаемым у данных пациенток (р=0,33).
Таким образом, выявленную зависимость нейропатии от типа пролапса нельзя списать на разницу в демографических особенностях пациенток (возраст и число родов). Есть вероятность, что значимых различий получено не было из-за малого числа наблюдений, и именно поэтому полученные нами данные несколько расходятся с результатами Boyle D.J. и соавт. [10], которые установили, что латентность преимущественно левого полового нерва увеличивается с возрастом и при вагинальных родах.
Обсуждение
При анализе мировой литературы, посвященной пролапсу тазовых органов, мы обратили внимание на довольно высокий процент наличия нейропатии как у больных с пролапсом гениталий, так и у пациенток с ректальным пролапсом – до 66% [3].
При этом ранее в наших исследованиях было доказано, что у больных с генитальным пролапсом частота нейропатии достигает практически 100% [24], а у больных только с ректоцеле как вариантом заднего пролапса – от 72,7 до 85,7% [25].
В настоящей работе исследовали частоту встречаемости нейропатии полового нерва и ее связь с НАС у пациенток с крайней степенью пролапса тазовых органов – выраженным опущением и выпадением внутренних половых органов [26] и больных с наружным выпадением прямой кишки. В результате нашего исследования было выявлено, что у всех больных с наружным выпадением прямой кишки имеется и нейропатия, и недостаточность анального сфинктера.
Однако полученные результаты не позволяют четко сформулировать причинно-следственную связь: является ли нейропатия причиной развития анальной инконтиненции или лишь патогенетическим звеном этого процесса наряду с механическим перерастяжением анального сфинктера при выпадении прямой кишки.
В то же время высокая частота встречаемости нейропатии (84%) и признаков анальной инконтиненции у пациенток с генитальным пролапсом даже без механического воздействия на анальный сфинктер склоняет нас к предположению об определенной роли тазовой нейропатии в развитии анальной инконтиненции при выраженном тазовом пролапсе.
Однако для подтверждения данной гипотезы требуется проведение дальнейших исследований с большим числом наблюдений и включением дополнительных сравнительных групп: здоровые добровольцы и пациентки с начальными признаками синдрома опущения мышц тазового дна.
Заключение
У всех пациенток с ректальным пролапсом выявляются наличие нейропатии и клинико-инструментальные признаки недостаточности анального сфинктера;
У больных с генитальным пролапсом увеличение проводимости по половому нерву зарегистрировано в 84% случаев.
Только у 8% женщин с генитальным пролапсом отсутствовали клинико-инструментальные признаки недостаточности анального сфинктера, у 16% – выявлена латентная форма анальной инконтиненции, что подтверждено данными функциональных исследований;
Значительный процент выявления нейропатии у пациенток с опущением и/или выпадением внутренних половых органов ставит вопрос о месте нейропатии в патогенезе тазового пролапса.