На сегодняшний день эпидуральная анальгезия (ЭА) является наиболее эффективным методом обезболивания родов, что объясняет ее широкое применение. В действующих клинических рекомендациях по нейроаксиальным методам обезболивания родов от 2018 г. отмечено, что постановка ЭА не влияет на частоту оперативного родоразрешения и перинатальных осложнений у матери и плода и возможна без учета степени раскрытия шейки матки [1]. Однако стоит отметить, что характер влияния последней на течение родов и перинатальные исходы до сих пор остается предметом дискуссии. Так, в новейшем ретроспективном анализе историй 21 808 родов 1, 2a, 3, и 4a групп по классификации Робсона, опубликованном Zanfini В.А. et al. в 2022 г., помимо увеличения продолжительности родов на фоне ЭА, была выявлена статистически значимая ассоциация ее проведения с увеличением частоты оперативных вагинальных родов (ВР) и кесарева сечения (КС) (р<0,05) [2]. Согласно результатам многофакторного анализа ретроспективных данных 2726 родов 1 и 2а групп по классификации Робсона, нейроаксиальная анальгезия явилась независимым фактором риска абдоминального родоразрешения (р<0,0001) [3].
Связь проведения ЭА с развитием лихорадки в родах была выявлена еще в конце XX в.; при этом, согласно результатам недавно проведенных исследований, частота повышения температуры (Т) тела до 38°C и более при данном методе обезболивания родов достигает 11–33% [4]. Это привело к появлению в медицинской литературе самостоятельного термина «epidural-related maternal fever» (ERMF), при дословном переводе означающего «лихорадка, ассоциированная с ЭА». В классификации МКБ-10 гипертермия во время родов закодирована как О75.2, в МКБ-11 – JB0D.2; однако критерии постановки данного диагноза точно не определены. Строгих критериев гипертермии в отечественной литературе не существует; наиболее часто в качестве порогового значения принимается Т в подмышечной впадине, равная 37,5°C и выше, с учетом того, что нормальная Т тела составляет в среднем 36,6–37,0°C с суточными колебаниями, равными 0,5°C, что было подтверждено опытным путем [5,6]. Согласно клиническим рекомендациям Королевского колледжа акушеров и гинекологов (Royal College of Obstetricians and Gynaecologists, RCOG) по бактериальному сепсису у беременных, гипертермию в родах следует определять как Т тела в родах ≥38°C при однократном измерении или 37,5°C и выше при двукратном измерении с интервалом 2 ч [7]. Основываясь на представленных данных, в приведенном ретроспективном анализе гипертермия в родах будет соответствовать Т в подмышечной впадине ≥37,5°C, определяемой как минимум при однократном измерении; Т=37,1–37,4°C будет классифицирована как «тенденция к гипертермии».
Также следует избегать путаницы в терминах «гипертермия» и «лихорадка», в основе которых прежде всего лежат различные патофизиологические механизмы. Под термином «гипертермия» подразумевается пассивное состояние организма, связанное с его перегреванием на фоне снижения эффективности механизмов теплоотдачи и/или срыва механизмов терморегуляции в результате длительного психоэмоционального стресса, при эндокринной патологии, а также под действием внешних причин. Лихорадка определяется как общая неспецифическая реакция организма на действие экзогенного или эндогенного пирогенного фактора [8]. Учитывая, что их проявлением служит повышение Т тела выше нормы, которое в родах обусловлено как действием психоэмоционального фактора, так и воздействием эндогенных пирогенов (в частности, провоспалительных цитокинов интерлейкинов (IL-6 и IL-10), относительно рассматриваемого состояния применимы оба термина.
Цель представленного ретроспективного анализа – выявление связи развития гипертермии в родах с проведением ЭА, поиск факторов риска ее развития, а также анализ влияния ЭА на течение родов и тип родоразрешения.
Материалы и методы
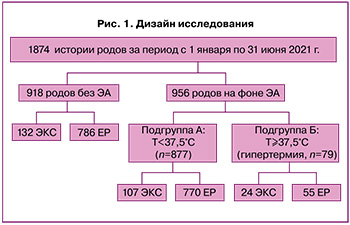
Исследование проведено на базе родильного дома ГКБ им. Д.Д. Плетнева (Москва). В ретроспективный анализ было включено 1874 истории родов за период с 1 января по 31 июня 2021 г.; из них 956 родов велись на фоне ЭА, а 918 – в отсутствие нейроаксиального обезболивания. В рамках исследования была проведена диверсификация по типу родоразрешения (ВР и оперативные роды путем операции КС в экстренном порядке (ЭКС)). По степени повышения Т тела в группе родов на фоне ЭА было выделено 2 подгруппы: подгруппа А, включившая рожениц с Т<37,5°C (877/956), и подгруппа Б, объединившая роды с Т≥37,5°C (79/956). С целью оценки степени повышения Т при проведении нейроаксиального обезболивания и в его отсутствие в основных группах сравнивались частота тенденции к гипертермии (Т≥37°C и <37,5°C) и гипертермия (Т≥37,5°C). Плановые операции КС из анализа были исключены ввиду отсутствия у беременных родовой деятельности на момент начала оперативного вмешательства, а также их обезболивания путем спинномозговой анальгезии, реализующей свои эффекты через другие патогенетические механизмы. Дизайн данного ретроспективного исследования представлен на рисунке 1. В группе пациенток, рожавших на фоне ЭА, были проведены сравнительный анализ их анамнестических данных, однофакторный корреляционный и дисперсионный анализы, направленные на выявление факторов, предрасполагающих к развитию гипертермии.
Статистический анализ
Медицинские данные заносились в индивидуальные регистрационные карты родильниц, на основании которых была сформирована база данных в Microsoft Excel 2019. Статистический анализ проводился с использованием пакета статистических программ IBMSPS Statistics 22.0. 95% доверительные интервалы (ДИ) к частотам были рассчитаны на основании биномиального распределения. Статистическую значимость различий между частотами определяли с помощью точного варианта критерия «хи-квадрат». Для числовых характеристик были рассчитаны величины среднего арифметического M, минимального (Min) и максимального (Max) значений, а также стандартного (среднеквадратичного) отклонения σ; данные представлялись в виде M (σ); полученная по фактическим данным оценка σ обозначалась как s. Значимость различий среднего в двух группах определяли при помощи t-критерия (вариант без использования предположения о равенстве дисперсий). Корректность применения методов параметрической статистики определяли в соответствии с [9]. Для подтверждения корректности применения методов параметрической статистики при сравнении распределения числовых характеристик в двух группах также применяли непараметрический критерий Манна–Уитни, результаты применения которого во всех случаях не противоречили результатам t-критерия. При множественных сравнениях для определения статистической значимости различий использовали поправку Холма–Бонферрони. Различия считали статистически значимыми при р<0,05.
Результаты
Для оценки возможного влияния ЭА на риск гипертермии и оперативного родоразрешения в первую очередь был проведен статистический анализ встречаемости тенденции и собственно гипертермии, а также дистресса плода и ЭКС в группах пациенток, рожавших на фоне ЭА и без нейроаксиального обезболивания.
В группе родов без ЭА (918/1874) тенденция к гипертермии была отмечена у 13 пациенток (1,4% (13/918): у 1,4% (12/854) – при ВР и 1,6% (1/64) – при ЭКС), гипертермия – лишь у 2 пациенток (0,2% (2/918): 1 случай при естественных родах, 1 – при ЭКС). 7% родов (64/918) в данной группе были завершены путем ЭКС; при этом одним из наиболее частых показаний к оперативному родоразрешению служил дистресс плода с изменением частоты сердечных сокращений (ЧСС) плода и/или выходом мекония в амниотическую жидкость, выставленный у 20 пациенток (2,2% (20/918)), 10 из которых было проведено ЭКС (15,6% (10/64) всех ЭКС в данной группе), 6 – вакуум-экстракция плода (ВЭП).
В группе родов на фоне ЭА (956/1874) тенденция к гипертермии выявлялась у 14,2% (136/956) пациенток (у 11,1% (106/956) – при ВР и 3,1% (30/956) – при ЭКС), гипертермия была зарегистрирована у 8,2% (79/956) пациенток (5,7% (55/956) – при ВР, 2,5% (24/956) – при ЭКС). ЭКС на фоне ЭА было проведено в 13,7% (131/956) случаев, что практически в 2 раза выше, чем в группе родов без ЭА – 7% (64/918). Диагноз дистресса плода с изменением ЧСС плода и/или выходом мекония в амниотическую жидкость был выставлен у 13,3% пациенток (124/956); при этом 63% (78/124) из них были родоразрешены путем ЭКС, 18,5% (23/124) – путем ВЭП. Из приведенных данных следует, что дистресс плода после проведения нейроаксиального обезболивания развивался в 6 раз чаще (13% (124/956) против 2,2% (20/918)); при этом его доля в структуре показаний к ЭКС была значительно выше – более половины случаев.
Из таблицы 1 также следует, что повышение Т тела в родах до 37,0°C и более значительно чаще отмечалось на фоне нейроаксиального обезболивания (p<0,001); при этом гипертермия при ЭА регистрировалась в 40 раз чаще – в 8,2% случаев (79/956, 5,7% (55/956) – при ВР, 2,5% (24/956) – при ЭКС), чем в отсутствие данного вида обезболивания (лишь в 0,2% случаев (2/918), 1 – при ВР, 1 – при ЭКС). Таким образом, для подтверждения актуальности проведения ретроспективного анализа была получена достоверность связи повышения Т тела роженицы с проведением ЭА.

Для дальнейшей оценки влияния данного метода регионарной анальгезии на развитие гипертермии и факторов, предрасполагающих к ее развитию, в группе родов с обезболиванием родового акта путем проведения ЭА были выделены 2 подгруппы: подгруппа А – пациентки с родами на фоне ЭА и Т<37,5°C (877/956); подгруппа Б – пациентки с родами на фоне ЭА и Т≥37,5°C (79/956). При сравнительном анализе анамнестических данных обеих групп было отмечено, что средние арифметические значения возраста (в подгруппе А – 30 лет, в подгруппе Б – 29 лет), срока беременности (в обеих подгруппах 40 недель), прибавки веса за период беременности (в подгруппе А – 14,2 кг, в подгруппе Б – 14,9 кг), паритета (в подгруппе А – 0,47, в подгруппе Б – 0,14) значительно не отличались, что свидетельствует об однородности исследуемой выборки и повышает достоверность анализа.
Рассмотрим подробнее данные о течении настоящих родов и их связь с развитием гипертермии на фоне эпидурального обезболивания (табл. 2).
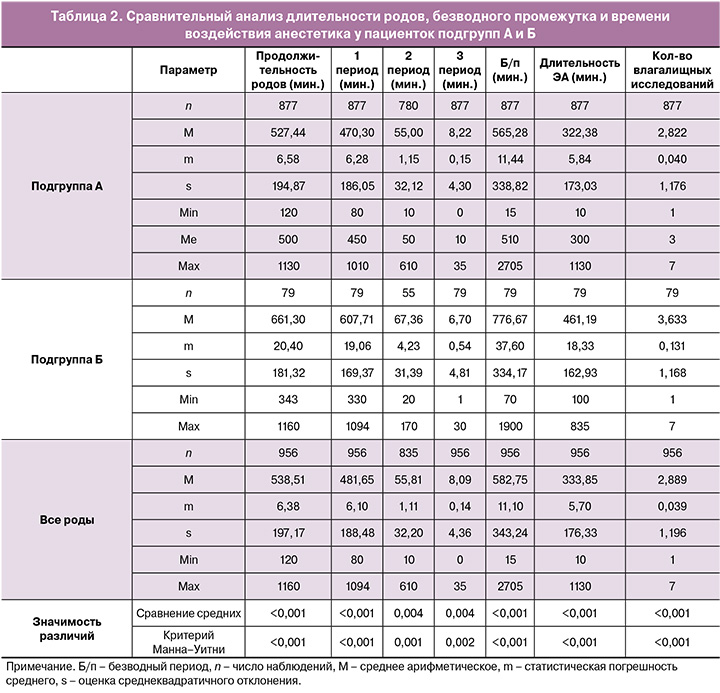
Данные сравнения средних при помощи критерия Стьюдента свидетельствуют о том, что гипертермия на фоне ЭА сопровождается достоверно более высокими показателями продолжительности родов, безводного периода, времени воздействия анестетика, а также количества влагалищных исследований.
Несмотря на то что всего было проведено 7 сравнений для каждого из двух используемых критериев, максимальная величина p составила 0,004 для первого критерия (сравнение средних) и 0,002 для второго критерия (Манна–Уитни), то есть при уровне значимости р=0,05 и использовании поправки Холма–Бонферрони все найденные различия статистически значимы.
Также видно, что уровни значимости различий, полученные при помощи параметрических методов статистики и непараметрического критерия Манна–Уитни, близки друг к другу.
При оценке влияния степени раскрытия шейки матки на момент проведения ЭА с повышением Т тела в родах до 37,5°C и более было выявлено, что раскрытие шейки матки 5 см и более ассоциировано с наиболее низким уровнем гипертермии (1,27% (1/142), 95% ДИ: 0,31–4,56%, р<0,001, табл. 3). Данная тенденция вполне закономерна ввиду того, что раскрытие маточного зева до 5 см знаменует начало активной фазы родов, длительность которой, как правило, в 2–3 раза короче длительности предшествующей ей латентной фазы.

Сравнение структуры качества околоплодных вод в исследуемых подгруппах показало, что гипертермия наиболее часто отмечалась при светлом их характере, что, вероятно, связано со значительно большей встречаемостью светлых околоплодных вод в представленной выборке (83,9% (727/877) и 67% (53/79)) и не позволяет исключить наличие патогенетической взаимосвязи развития гипертермии на фоне ЭА и дистресса плода с выходом мекония в амниотическую жидкость (табл. 4).
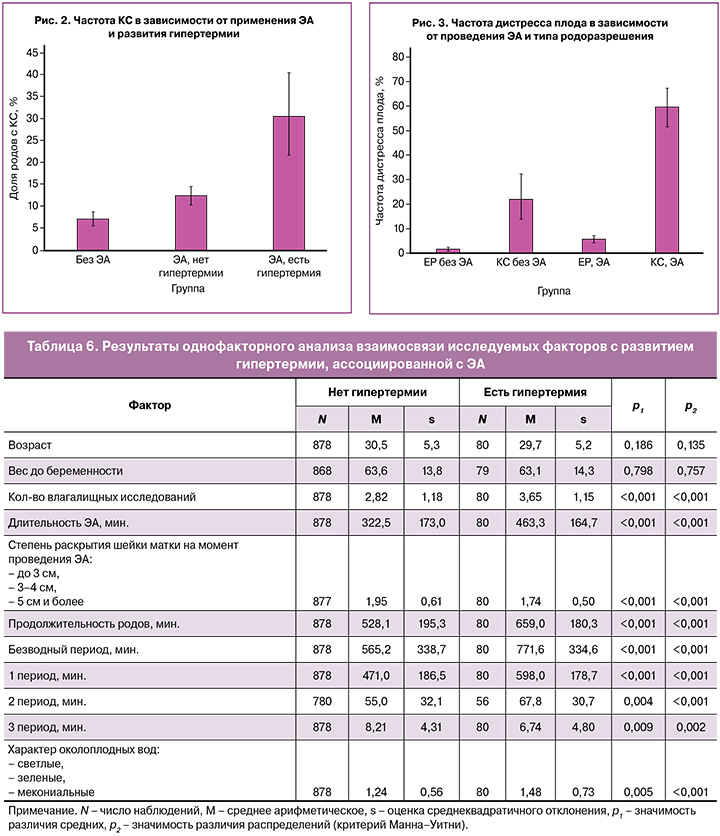
В ходе анализа типов родоразрешения в исследуемых подгруппах было отмечено, что гипертермия сопровождалась более высокой частотой оперативного родоразрешения: ЭКС в подгруппе Б проводилось в 2,5 раза чаще (30,4% (24/79) и 12,2% (107/877), р<0,001, рис. 2), ВЭП – в 2,9 раза чаще (10,1% (8/79) и 3,5% (31/877), р=0,003), чем в подгруппе А (рис. 2); при этом наиболее распространенным показанием к вмешательству был дистресс плода (при повышении Т тела до 37,5°C и более на фоне ЭА частота дистресса плода была в 2,6 раза выше, чем при Т тела ниже 37,5°C (29,1% (23/79) и 11,4% (100/877), р<0,001, рис. 3).
Помимо особенностей течения родов, в анализ факторов, потенциально взаимосвязанных с развитием гипертермии на фоне эпидурального обезболивания, были включены различные осложнения течения настоящей беременности, инвазивные вмешательства в процессе родов, такие осложнения родов, как послеродовые кровотечения, нарушение целостности последа, аномалии родовой деятельности, а также отклонения в лабораторных анализах, полученных при поступлении на роды (табл. 5).
Достоверные связи вероятности развития гипертермии были обнаружены лишь для дистресса плода и ВЭП. Так как статистическая значимость полученных различий р≈0,0000378, а при поиске различий было проведено 16 сравнений, то и при использовании поправки Бонферрони различия значимы с р<0,001. Относительный риск развития дистресса плода при наличии гипертермии составил 2,829 (95% ДИ: 1,807–4,429).
Ниже представлены суммарные результаты однофакторного анализа, оценивающего силу и достоверность связи с вероятностью развития гипертермии представленных выше параметров (табл. 6).
Помимо этого, у пациенток с ЭА при сравнении подгрупп с гипертермией и без нее не было выявлено статистически значимых различий в частоте лейкоцитурии (р=0,135), лейкоцитоза (р=0,171) и кольпита (р=0,126).
Таким образом, в ходе однофакторного анализа были установлены следующие факторы, оказывающие значимое влияние на возникновение гипертермии в родах: длительность воздействия анестетика (р<0,001), продолжительность родов (р<0,001), продолжительность безводного периода (р<0,001), количество влагалищных исследований (р<0,001), степень раскрытия шейки матки на момент постановки анальгезии (р<0,001), а также характер околоплодных вод (р=0,005), что подтверждает необходимость проведения проспективного исследования с целью более детальной оценки динамики повышения Т рожениц после проведения ЭА и изучения возможных патогенетических механизмов развития гипертермии путем оценки лабораторных показателей и данных гистологического анализа плацент.
Обсуждение
Впервые связь обезболивания родов посредством ЭА с развитием лихорадки отметили Fusi L. et al. более 30 лет назад; при этом они выявили прямую корреляционную связь между Т тела роженицы и длительностью анальгезии [8]. С тех пор было проведено множество клинических исследований, подтверждающих влияние ЭА на развитие гипертермии в родах, однако более ранние публикации подвергались критике за отсутствие поправок на предрасполагающие к развитию лихорадки факторы, такие как паритет, продолжительность родов, Т роженицы при развитии родовой деятельности и т.д. В последующем были опубликованы результаты исследований, учитывающих смешивающие факторы, в которых была доказана статистически значимая ассоциация проведения ЭА с последующим проградиентным ростом Т тела роженицы, при этом скорректированное соотношение шансов, по данным разных авторов, составило 2,9–14,5 [10].
Исследователями выдвигались различные гипотезы ЭА-ассоциированной лихорадки: развитие хориоамнионита, модуляция терморегуляции под действием нейроаксиальной анальгезии и др. Однако на сегодняшний день представлены убедительные доказательства главенствующей роли в повышении Т тела роженицы на фоне ЭА неинфекционного воспалительного процесса, инициируемого или потенцируемого воздействием эндогенных провоспалительных пирогенных цитокинов [11]. Примечательно, что при постановке ЭА с целью обезболивания в ходе оперативного вмешательства у небеременных, как правило, отмечается обратный эффект – развитие гипотермии, которая может сопровождаться снижением насыщения тканей кислородом и их микроперфузии, например, после циторедуктивной операции по поводу рака яичников, в связи с чем было предложено предварительное согревание пациенток воздухом при Т=43°C в течение 30 минут перед вмешательством [12]. Такой эффект объясняется сочетанным влиянием на терморегуляцию одновременно применяемых ингаляционных анестетиков [13] и опиоидов [14].
В представленном ретроспективном анализе данных 1874 родов при проведении ЭА повышение Т тела выше нормальных значений (>37°C) отмечалось почти в 11,5 раза чаще, чем в отсутствие нейроаксиального обезболивания (17,25% (165/956) и 1,5% (14/918) соответственно), что подтверждает возрастание риска развития последней на фоне ЭА (p<0,001). При дальнейшем анализе данных установлена статистически значимая ассоциация проведения ЭА с повышением Т тела рожениц до 37,5°C и более (97,53% (79/81) всех случаев гипертермии регистрировались на фоне ЭА, 95% ДИ: 93,31–99,23, р<0,001). Полученные результаты не согласуются с данными отечественного проспективного исследования от 2008 г., проведенного Шифманом Е.М. и соавт., в ходе которого не было выявлено достоверных статистических различий в частоте встречаемости лихорадки в родах между экспериментальной группой, включившей 342 роженицы, обезболенных методом ЭА при раскрытии шейки матки 3–5 см, и группой сравнения, которую составили 55 пациенток, рожавших в отсутствие нейроаксиального обезболивания [15], Это может быть обусловлено более своевременным проведением анальгезии в экспериментальной группе и иным диагностическим критерием лихорадки (данный диагноз выставлялся при повышении Т тела выше 38°С). Стоит отметить, что средняя Т тела после родов в группе исследования была достоверно выше, чем в группе сравнения (37,3 (0,23) и 36,99 (0,35)°C соответственно, р<0,001).
Предрасполагающими факторами развития гипертермии, согласно данным однофакторного анализа, явились длительность воздействия анестетика (р<0,001), продолжительность родов (р<0,001) и безводного периода (р<0,001), количество влагалищных исследований (р<0,001), степень раскрытия шейки матки на момент постановки анальгезии (р<0,001), а также характер околоплодных вод (р=0,005), что согласуется с недавно опубликованными результатами ретроспективного анализа, согласно которым в качестве основных факторов риска лихорадки, ассоциированной с ЭА, были определены преждевременный разрыв плодных оболочек (относительный риск (ОР)=2,008, 95% ДИ: 1,551–2,600), более 6 влагалищных исследований в родах (ОР=1,681, 95% ДИ: 1,286–2,197), большая продолжительность родов (ОР=1,090, 95% ДИ: 1,063–1,118) и длительный безводный период (ОР=1,048, 95% ДИ: 1,010–1,087) [16].
Оперативное родоразрешение в подгруппе гипертермии на фоне ЭА проводилось в 2,5 раза чаще, чем при Т<37,5°C (30,4% (24/79) и 12,2% (107/877) соответственно, р<0,001); при этом гипертермия была ассоциирована с повышенным риском как абдоминального, так и влагалищного оперативного родоразрешения (ВЭП в подгруппе Б применялась почти в 3 раза чаще, чем в подгруппе А (10,1% (8/79) и 3,5% (31/877)), р=0,003), что также соответствует результатам крупных ретроспективных анализов, упомянутых выше. Представленные данные свидетельствуют о необходимости уточнения утверждений о том, что проведение нейроаксиальной анальгезии с тщательным соблюдением технологии не увеличивает частоту оперативного родоразрешения и может применяться без учета степени раскрытия шейки матки [2]. Отказ от раннего обезболивания, сопряженного с повышением продолжительности родов и времени воздействия анестетика, а также с увеличением длительности безводного периода в случае преждевременного излития вод и проведения амниотомии в рамках программированных родов, возможно, является простым инструментом снижения риска гипертермии и оперативного родоразрешения в отсутствие абсолютных показаний к постановке ЭА.
Заключение
В ходе ретроспективного анализа 1874 историй родов (956 родов на фоне ЭА, 918 – без ЭА) выявлена статистически значимая ассоциация проведения ЭА с повышением Т тела рожениц до 37,5°C и более. По данным однофакторного анализа, с развитием гипертермии ассоциированы такие факторы, как продолжительность воздействия анестетика, родов, безводного периода, число влагалищных исследований, степень раскрытия шейки матки на момент проведения обезболивания, а также характер околоплодных вод. Подтверждена взаимосвязь постановки ЭА с повышенным риском как абдоминального, так и влагалищного родоразрешения, главным образом в случае гипертермии. Более углубленное изучение характера влияния ЭА на возникновение гипертермии и ассоциированных с ней перинатальных осложнений позволит выработать наиболее безопасную тактику обезболивания родового акта и повысить качество оказания акушерской помощи.