Current issues in preeclampsia: a ten-year analysis of maternal mortality
Aim. To investigate the implementation of evidence-based guidelines for the prevention of adverse outcomes in preeclampsia.Sidorova I.S., Nikitina N.A., Filippov O.S., Guseva E.V., Ageev M.B., Kokin A.A.
Materials and methods. The study analyzed medical records of 129 maternal deaths from preeclampsia/eclampsia and their complications in Russia's regions from 2010 to 2019. Data for years 2010–2015 (n=63) were compared with that for 2016–2019 (n=66). Between these periods, all Russian Federation regions adopted new terminology, classification, and management strategy for preeclampsia established by new national guidelines.
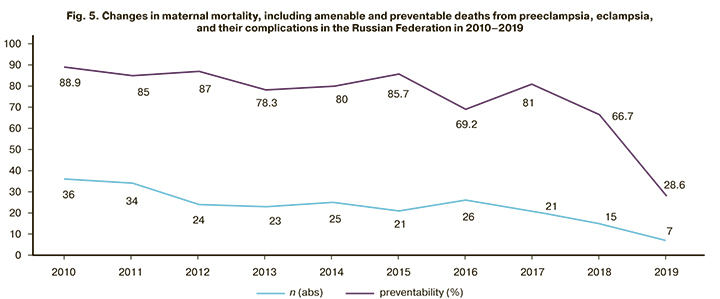
Results. In 2010–2015 amenable and preventable maternal preeclampsia-related mortality reached 89%. There were significant medical errors in patients' management related to inappropriate prevention and treatment in outpatient and inpatient settings. The introduction of new national guidelines for preeclampsia management resulted in improved maternal and perinatal outcomes and sharply reduced amenable and preventable maternal mortality.
Conclusion. Standardization, strict adherence to approved protocols, and continuous maternal health care quality assessment is an effective and promising way to reduce preeclampsia-related maternal mortality.
Keywords
According to WHO estimates, while maternal mortality has decreased significantly over the past decades across the world, it is still unacceptably high. Approximately 830 women die worldwide every day from preventable causes related to pregnancy and childbirth. The vast majority of these deaths occurred in low-resource settings, and most could have been prevented [1]. From 1990 to 2015, the global maternal mortality rate has declined by only 2.3% per year. However, since 2000, it has been declining with higher rates [1].
The changes in the maternal mortality rate in the Russian Federation (RF) (according to the Ministry of Health of Russia) are presented in Fig. 1, which also shows a global trend [2–4].

According to official WHO data, the main complications that account for two thirds (75%) of all maternal deaths worldwide are massive obstetric hemorrhage (mainly postpartum), sepsis, hypertensive disorders, and complicated abortions [5]
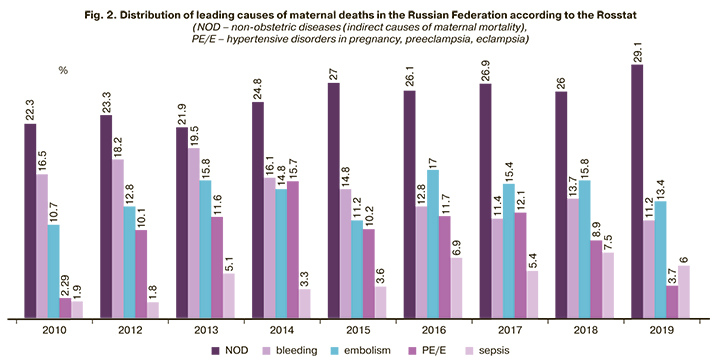
Distribution of leading causes of maternal deaths in the Russian Federation from 2007 to 2019 is shown in Fig. 2 and is broadly consistent with global indicators [2–4]. The top five causes include non-obstetric diseases, bleeding, hypertensive disorders including preeclampsia/eclampsia, sepsis, and embolism.
According to the Global Strategy for Women’s and Children’s Health adopted during the 2015 UN General Assembly in New York, one of the most essential modern health care goals is to reduce global maternal mortality to less than 70 per 100,000 live births. By 2030, no country should have a maternal mortality rate greater than 140 maternal deaths per 100,000 live births, a number twice the global target [6].
In the Russian Federation, a long-term state demographic program has been launched. Its main directions were outlined in the “Concept for a demographic policy for the Russian Federation for the period up to 2025,” sanctioned by presidential decree of 9 October 2007, No. 1351.
The Russian Federation's demographic policy for the period up to 2025 aims to overcome depopulation, increase the birth rate, and reduce mortality, including maternal and infant mortality, at least by half.
In 2018, the national projects "Demography" and "Healthcare" were approved to achieve the main state goals, including preserving the population, health, and well-being of people.
Much has been done in this direction in the last decade, primarily at the state level. Since 2006, the "Birth Certificate" program has been introduced. Its implementation has made it possible to improve the material and technical base of maternity institutions, expand their diagnostic capacities, and improve the quality of obstetric care for pregnant and postpartum women, newborns, and infants.
Starting from the year 2009, additional unprecedented measures have been taken to increase health care system funding, introduce new organizational forms, and improve the material and technical equipment for obstetric care as the most important branch of medicine. Federal laws, Russian government decisions, and orders of the Ministry of Health and the Ministry of Justice have been issued to implement the program outlined in the Presidential Address to the Federal Assembly and the scientific and practical community of specialists.
For each Russian Federation region, plans have been drawn up to reduce maternal and perinatal mortality, and appropriate measures have been developed (“road maps”). A three-tier system was introduced for obstetric and gynecological care. In many Russian regions, modern perinatal centers have been built, and new medical genetics services were created; the delivery of high-tech medical care in obstetrics and gynecology (including the use of IVF) is increasing annually. Twenty-eight training simulation centers have been created to train specialists in obstetrics and gynecology, neonatology, and pediatrics.
In the course of implementing the Concept of Demographic Policy, positive demographic changes have been noted (an increase in the birth rate, a decrease in the death rate, including a reduction of maternal mortality).
As for preeclampsia, new Federal Clinical Guidelines were published in Russia in 2013 [7]. Preeclampsia was isolated from the class "Hypertensive disorders of pregnancy" as a specific and severe complication. Modern terminology, classification of hypertensive disorders, and preeclampsia (moderate, severe) were introduced. Diagnostic criteria for severe and moderate preeclampsia have been substantiated. Mild preeclampsia was excluded based on the absence of evidence-based criteria. The management strategy and therapeutic approaches that meet international standards are regulated. Criteria for predicting severe preeclampsia were proposed.
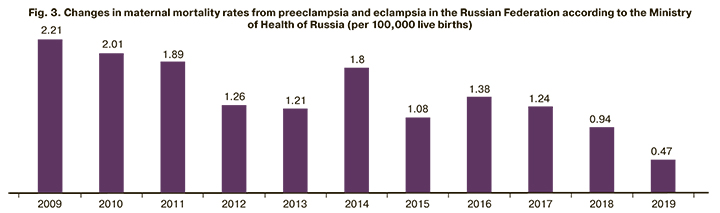
New clinical guidelines were updated in 2016, 2019, and gradually, over 2–3 years, they have been implemented into obstetric practice in all Russian regions. Since then, maternal mortality rates from preeclampsia and eclampsia in Russia have a clear downward trend, but it was initially unstable (Fig. 3). By 2019 the most convincing data were obtained indicating maternal mortality rate reduction by 81% compared to 2014 and 50% compared to 2018.
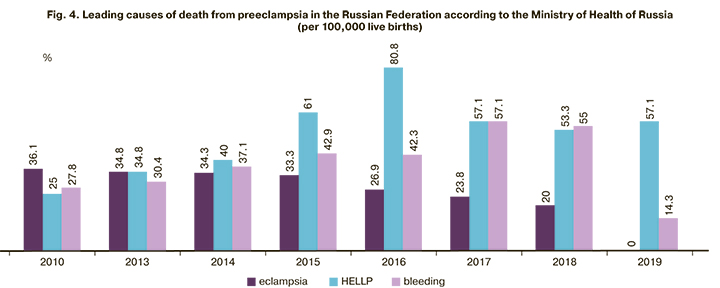
Before 2015, the structure of maternal mortality from preeclampsia remained practically unchanged. The proportion of eclampsia, HELLP syndrome and acute fatty liver, massive obstetric bleeding among all causes of death remained approximately equal. After 2015, among all the complications of preeclampsia that caused death, there was an increase in severe liver and kidney damage rates in parallel with a reduction of the proportion of eclampsia (in 2019, there were no deaths from eclampsia).
These changes in the leading indicators of maternal mortality from preeclampsia/eclampsia in Russia in the last decade were the basis for a detailed comparative analysis of deaths from this pregnancy complication from 2010 to 2019.
The present study aimed to investigate the implementation of evidence-based guidelines to prevent adverse perinatal outcomes in preeclampsia over the past ten years.
Materials and methods
As part of the annual confidential audit conducted jointly with the Department of Child’s Health Care and Maternity Services of Minzdrav of Russia, this study analyzed the primary medical documentation of more than 300 cases of maternal deaths associated with preeclampsia, eclampsia and their complications in the regions of Russia from 2010 to 2019 was analyzed. However, the study included only 129 deceased women for whom a complete set of documents was obtained, including medical outpatient records, antenatal and postpartum care cards, delivery notes, inpatient medical records, medical cards of abortion, and postmortem examination protocols.
Considering the nature of the organizational measures carried out in the country, the analyzed decade was divided into the period from 2010 to 2015 (period I, n=63) and from 2016 to 2019 (period II, n=66). We analyzed the medical, gynecological, reproductive history of each patient, characteristics of pregnancy course, the time of manifestation, development, and progression of preeclampsia and its complications, the timing, mode of delivery, and management strategy.
Statistical analysis
Statistical analysis was performed using Statistica v. 8.0 for Windows. It was found that numerical variables were not normally distributed as indicated by the Lilliefors and Kolmogorov–Smirnov tests, and groups were compared using nonparametric tests. Kruskal–Wallis test and the median test were used for comparing numerical data between groups, followed by pairwise comparison using the Mann–Whitney U-test. Differences were considered statistically significant at p<0.05.
Results
Clinical characteristics of the development and progression of severe preeclampsia.
The age of 129 women who died from preeclampsia ranged from 16 to 44 years. Over the analyzed years, there was a tendency towards an increase in the age of these patients. In 2010–2014, 2015–2017, and 2018–2019 the number of deaths among patients over 30 was 54%, 64.7%, and 84.4%; 7.8% of women were 20 years old and younger.
Worthy of considerable attention is the unsatisfactory status of somatic health of deceased patients during both analyzed periods. Each of them had from 2 to 5 or more comorbidities, including chronic arterial hypertension in 44% and 28.8%, respectively, kidney and urinary tract diseases (33.4 and 27.2%), liver diseases (12.7% and 24.2%), neuro- and endocrine diseases (33.4 and 47.2%), etc. However, during the first period, comorbidities in 54% of the deceased patients were detected by the pathologist posthumously; during the second period, there were 12.1% of such cases (p≤0.001).
For the two analyzed periods, no significant differences were found in changes in development and progression of preeclampsia; however, there were some characteristic features.
In both groups, in the overwhelming number of observations (95.2 and 92.4%, respectively), there were early clinical manifestations up to 34 weeks of pregnancy. More than half of the patients (57.1 and 62.1%) had edema as the first symptom, every third had arterial hypertension (40 and 34.8%), and proteinuria was extremely rare (3.2 and 3%).
However, the duration of severe preeclampsia differed significantly. It was more than 8 weeks in 33.3% for the first analyzed period, and from 2 to 8 weeks in 46.1%. In recent years, in most observations (56%), no more than two weeks passed between the first preeclampsia symptom occurrence and delivery, which explains the lower detection rate of massive proteinuria and severe oliguria. There were no significant differences in the severity of other symptoms.
In both I and II analyzed periods, there was high rates of atypical course of preeclampsia without severe arterial hypertension (31.7 and 42.4%, respectively), massive proteinuria (47.6 and 59.1%, respectively), generalized edema (58.7 and 54.5%, respectively), and the classical triad of symptoms (in 3.2 and 10.6%, respectively).
The primary maternal complications observed in women who died from preeclampsia/eclampsia are presented in Table 1.
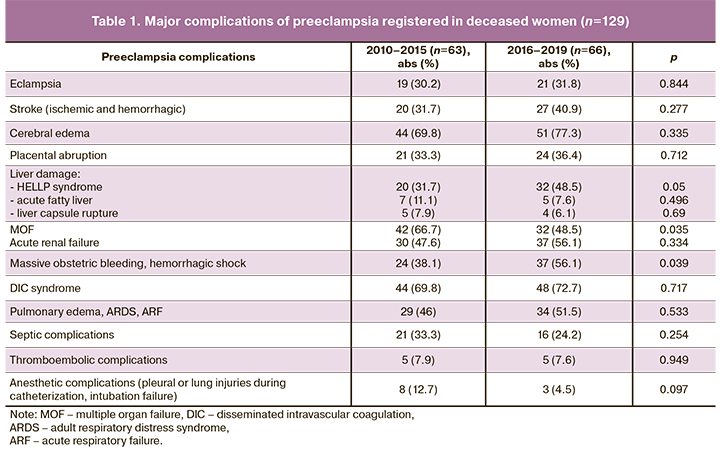
The data presented in Table 1 indicate the absence of positive dynamics in the rates of severe damage to the brain, kidney, liver, lungs, hemostasis system with extensive disseminated intravascular coagulation syndrome and major obstetric bleeding. It is also worth noting a significant increase in proportions of the HELLP syndrome and bleeding with the development of hemorrhagic shock among leading causes of death.
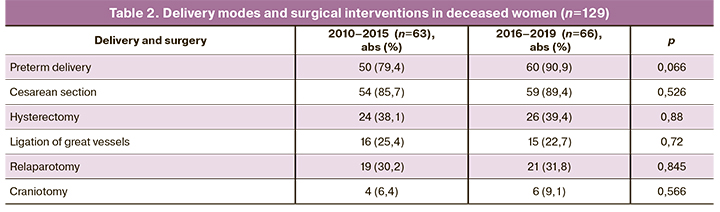
An analysis of the timing and modes of delivery (Table 2) showed that the rates of preterm, operative deliveries and other surgical interventions had not changed significantly in recent years. However, there is still a tendency towards faster and more careful delivery. Nevertheless, late diagnosis and delayed delivery remain essential contributors to maternal mortality, affecting the need for subsequent hysterectomy, repeat relaparotomy, and decompression craniotomy against the background of severe complications.
The distribution of direct causes of death also did not change significantly. In general, in most cases, there was cerebral edema with dislocation syndrome and intracerebral hemorrhages [n=64 (49.6%)], multiple organ failure [n=40 (31%)], massive obstetric bleeding with the development of hemorrhagic shock [n=13 (10, 1%)], obstetric embolism [n=5 (3.9%)], and septic complications [n=7 (5.4%)].
Perinatal outcomes are presented in Table 3. A total of 136 newborns (7 twins) had birthweight of 620 to 4500 g and 98 (72.1%) < 2500 g, including 44 (32.4%) with birthweight < 1500 g and17 (12.5%) with a critically low birthweight < 1000 g.
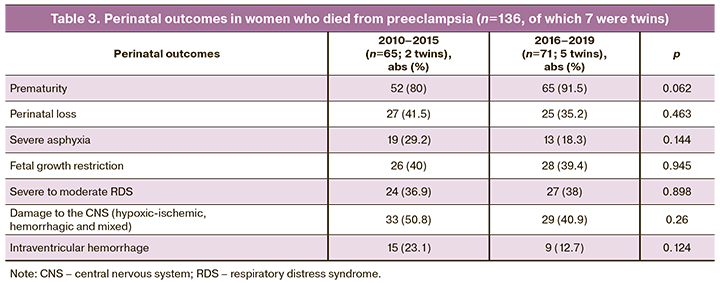
Perinatal mortality was 41.5% and 35.2% for the first and second periods, respectively.
There were no statistically significant differences in the incidence of unfavorable perinatal outcomes over the two analyzed periods. However, there was a decrease in perinatal mortality, severe birth asphyxia, perinatal damage to the central nervous system of various origins, and intraventricular hemorrhages against the background of a natural increase in the number of preterm babies.
Summarizing the above findings, it can be argued that the clinical features of the most severe forms of preeclampsia that ended with maternal death have changed little over the past decade. Patients with multiple comorbidities, early clinical manifestation and a long atypical course of severe preeclampsia, leading to severe multisystem lesions (brain, kidneys, liver, lungs, heart, hemostasis system, fetoplacental complex), still die in the absence of timely delivery.
However, the organizational measures implemented in the country somewhat changed the distribution of causes of maternal mortality from preeclampsia. Against the background of a decrease in the number of deaths from eclampsia (no cases in 2019), there was an increase in the proportion of deaths from severe damage to the liver (HELLP syndrome, acute fatty liver, acute liver failure), kidney (acute renal failure) and massive obstetric bleeding with known subsequent complications.
Comparative analysis of the quality of medical care
Many experts admit that most maternal deaths (up to 89%) from preeclampsia in 2010–2015 were amenable or preventable, which required a complete reassessment of the system for providing medical care to such patients. In 2016–2019 convincing data were obtained on a decrease in the absolute number of women who died from this complication of pregnancy, as well as the number of amenable and preventable deaths (up to 28.6% in 2019) (Fig. 5).
Years from 2010 to 2015
A thorough analysis of professional errors and shortcomings in the management and delivery of patients who died from preeclampsia in 2010–2015 showed numerous medical negligence cases, both in outpatient and inpatient settings, which contributed to such unfavorable outcomes.
The most critical and significant errors in the provision of medical care to such women were the following:
1. 100% of the deceased were entirely unprepared for pregnancy despite multiple comorbidities and complicated reproductive history. Consulting and team management with related specialists were either absent altogether or were formal, occasional, without the necessary recommendations.
2. Inadequate examination, lack of attention, or misinterpretation of the diagnostic findings (microalbuminuria, proteinuria in a single urine sample, hypoproteinemia, signs of hypovolemia and hemoconcentration, hypercoagulation, low platelet counts, an increase in creatinine, a decrease in urine output), omission of testing for 24-hour proteinuria and renal function, absence of dynamic blood pressure control (daily monitoring of blood pressure), etc.
3. No prediction of severe preeclampsia was utilized in the management of women with high-risk factors. At the same time, they are administered numerous drugs with unproven efficacy (chophytol, riboxin, cocarboxylase, glucose, wobenzym, multivitamins, actovegin, antioxidants, membrane stabilizers, hepatoprotectors, etc.).
4. Diagnosis of severe preeclampsia is erroneous and untimely (no diagnosis until “unexpected” eclamptic seizures).
- Errors in assessing the severity of preeclampsia with the widespread use of scales (Goek, Wittlinger) without considering indicators of the state of the liver, kidneys, cardiovascular system, hemostasis system, fetoplacental complex, followed by an unjustified prolongation of pregnancy and delayed delivery.
- Errors in the diagnosis of atypical (under the guise of "gestational pyelonephritis" with hospitalization in the urology department, "food toxicoinfection" with hospitalization in an infectious diseases hospital, "hepatitis", "cholecystitis", "epilepsy newly diagnosed during pregnancy" with hospitalization in the neurology department, etc.), which delays delivery and leads to irreversible multiple organ injury and death. This situation is due primarily to the lack of knowledge of obstetric pathology among doctors of related specialties, including emergency doctors.
- In all cases, no extended examination was triggered by the manifestation of edema in pregnant women after 20–22 weeks to rule out the onset of preeclampsia.
5. Until 2015, in different regions of Russia, different terminology and classifications were used, including "Mild preeclampsia", "Gestosis I–II", "Edema or arterial hypertension caused by pregnancy", "Preeclampsia of mild or moderate severity", "Arterial hypertension and edema without proteinuria", etc.
6. Hospitalization and routing errors:
- non-observance of the principle "patients with pregnancy complications after 22 weeks of gestation must be hospitalized in the maternity hospital/obstetric department";
- repeat transfers of patients in serious condition from one department to another (surgical, urological, gynecological, intensive care, obstetric, maternity);
- transfers of non-transportable women in critical condition from institutions of groups I–II to institutions of group III in the absence of the possibility of emergency delivery or the provision of highly specialized medical care.
6. The use of magnesium sulfate is delayed or inadequate to the severity of the condition and its administration's discontinuation during delivery. In cases of errors in the diagnosis of preeclampsia, magnesium sulfate was not used at all.
7. Delayed delivery due to incorrect or untimely diagnosis of preeclampsia, underestimating its severity, inadequate examination, a waste of time on transporting patients to second and third-tier hospitals.
8. Inadequate management of massive obstetric bleeding, including incorrect calculation of blood loss followed by inadequate infusion-transfusion therapy; attempts to preserve the uterus at any cost, hysterectomy in the patients in critical condition, relaparotomy in patients with overt disseminated intravascular coagulation.
9. Inadequate surgical skills resulting in uterine incisions followed by a rupture, urinary bladder and bowel wall injury, trauma of the small pelvis vessels with subsequent thrombosis in the postoperative period (particularly the ovarian vein).
10. Inadequate management of the postpartum period with the development of hemorrhagic strokes against the background of unstable hemodynamics, repeat eclamptic seizures, septic and thromboembolic complications.
11. Absence of differential diagnosis of different forms of thrombotic microangiopathy (TMA) with specific therapeutic approaches (severe preeclampsia, HELLP syndrome, atypical hemolytic uremic syndrome (aHUS), thrombotic thrombocytopenic purpura, etc.).
12. In very few cases, medical documentation contained protocols of clinical and anatomic pathology conferences with analysis of maternal and perinatal mortality with relevant comments and conclusions.
Therefore, the analysis from the modern view of maternal mortality from preeclampsia in 2010–2015 showed significant professional errors and shortcomings in managing patients, both in outpatient and inpatient settings, which explains the high rates of amenable and preventable deaths during these years.
Years from 2016 to 2019
A comparative analysis of medical errors in the management of women who died from preeclampsia in 2016–2019 showed fewer significant shortcomings than previous years. However, the following professional and organizational errors persisted:
1. Incomplete examination of pregnant women, especially by consulting specialists including hematologists, urologists, nephrologists, hepatologists, etc. As before, some severe comorbidities are diagnosed with a significant delay or during postmortem examination.
2. Late diagnosis of severe preeclampsia most commonly due to an atypical course against the background of ongoing therapy (antihypertensive drugs, anticoagulants, antiplatelet agents, and drugs used for various concomitant diseases).
3. Frequent omission of blood pressure monitoring. Extreme fluctuations of blood pressure can lead to acute disorders of cerebral blood flow or cause severe hypoperfusion of organs and tissues, up to necrotic changes.
4. As before, there is a lack of knowledge by doctors of related specialties of the problem of preeclampsia, its severe complications (instead of HELLP-syndrome patients are diagnosed with "acute viral hepatitis", "acute cholecystopancreatitis").
5. Errors in determining the blood loss volume and subsequent inadequate RBC transfusion.
6. Incomplete differential diagnosis omitting other TMA forms (out of 37 deaths with a clinical manifestation of HELLP syndrome and acute fatty liver, only two were examined for aHUS).
7. There were also errors in patients' routing when patients with antenatal fetal death and multiple organ injuries were transported to a third-tier facility.
8. In most regions, the prognosis of severe preeclampsia was omitted; there was no patient-tailored approach in patient’s management and follow-up, especially in the presence of comorbidities.
Discussion
The quality of obstetric and maternity care in the earlier years, before 2015, was insufficient due to many factors. Clinical practice of health personnel of institutions providing obstetric and gynecological care depended on their commitment to a particular scientific school, each of which recommended different approaches to terminology, classification, management, and delivery strategy, including in preeclampsia.
The lack of a unified approach to this problem has resulted in medical errors, discrepancies of opinions, misconceptions, insufficient knowledge of preeclampsia management, and its specific features (it is impossible to cure, a visible improvement – a decrease in edema, normalization of blood pressure – does not mean recovery, etc.).
New clinical guidelines developed jointly by the Russian Society of Obstetricians and Gynecologists and the Association of Obstetric Anesthesiologists and Intensivists and published in 2013 regulates a modern unified approach to terminology, classification, strategies for the management, treatment, delivery, and prevention of preeclampsia.
Implementing these guidelines into clinical practice obstetrics has taken at least three years in different regions of Russia. 2016–2019 – this is a period of a gradual transition to standardization and quality management of obstetric care.
In earlier years, an audit of maternal mortality showed that only a few obstetricians-gynecologists used the results of evidence-based research (both domestic and international). This research evidence includes timely diagnosis of preeclampsia, clear criteria for assessing its severity, the use of drugs with proven efficacy, indications for delivery in severe preeclampsia/eclampsia, the use of magnesium sulfate during childbirth, etc.
In recent years, the latest research evidence has influenced obstetric health care. A unified, systematic approach to the problem helps make the appropriate clinical decision, which naturally affects maternal and perinatal mortality indicators.
Also, there is a problem of underestimating maternal deaths in official statistics, which exists in almost all world countries. Underreporting maternal mortality in Russia is often due to errors in coding the leading cause of death, such as non-obstetric comorbidities or massive obstetric bleeding. The death of women from preeclampsia has often coded the death from arterial hypertension or bleeding. However, only complete identification of all maternal death cases allows assessing the actual maternal mortality rate, distribution of death causes, identifying risk factors, the shortcomings of management and monitoring, and developing prevention methods.
The results of a comprehensive analysis of maternal mortality from preeclampsia and its complications in Russia over the past ten years made it possible to formulate the following provisions.
The most effective way to reduce maternal mortality, including from severe preeclampsia and eclampsia, is constant monitoring of the quality of the examination, the validity of the diagnosis, management, and treatment of each patient, both in outpatient and inpatient settings; maintenance and support of a unified evidence-based approach to the management and delivery of patients with preeclampsia. Medical and diagnostic measures must comply with the legislatively approved national guidelines and be strictly implemented in all Russian regions.
Implementing current clinical guidelines and protocols based on federal laws, considering domestic and international scientific achievements and practical experience, should be constantly monitored by the relevant services. A broader introduction of antenatal care in a woman with comorbidities, individual prediction of the risk of maternal, fetal, and neonatal complications based on an examination, assessing the woman’s somatic and reproductive health, and the state of the fetal-placental unit is necessary.
The earliest symptoms of preeclampsia (in every third) are edema (latent, local, recurrent), signs of hemoconcentration (decreased urine output, increased hematocrit), hypercoagulability, hemodynamic abnormalities in the fetal-placental unit; further "unmotivated" increase in blood pressure, microalbuminuria, abnormal 24-hour proteinuria, fetal growth restriction, oligohydramnios are added.
Clinical presentation of rapidly progressive severe preeclampsia includes refractory hypertension, sudden onset of edema, proteinuria, hypoproteinemia, thrombocytopenia, elevated enzymes, cytolysis syndrome, signs of TMA, and endothelial dysfunction.
The development of a critical form of preeclampsia is manifested by neurological symptoms (headache, blurred vision, consciousness), pain in the right hypochondrium, dyspeptic symptoms (nausea, vomiting, loose stools), difficulty breathing, polyserositis, multiple organ dysfunction.
It is currently generally recognized that it is impossible to cure preeclampsia to stop its development, and it is difficult to predict the rate of progression. Long-term intensive care is not effective, and polypharmacy and extension of prenatal pharmacology are dangerous.
The clinical characteristics of preeclampsia often do not reflect the actual severity of the ongoing pathological changes, which result in multiple organ failure, TMA, and systemic damage to the systemic vascular endothelium. In this case, the clinical picture often depends on the predominant lesion of target organs (brain-convulsive syndrome, cerebral edema, acute hemodynamic disorders, liver – HELLP syndrome, acute fatty liver, kidney – acute renal failure).
Accurate assessment of preeclampsia severity determines the patient management strategy (severe preeclampsia – delivery, moderate – prolongation of pregnancy up to 34–37 weeks, eclampsia – an absolute indication for "termination of a dangerous pregnancy").
Timely delivery is still the only treatment for severe, early, combined preeclampsia, its critical forms, and complications (regardless of the gestational age). Delivery should be prompt and gentle with adequate pain relief and readiness for a possible more extended intervention, which requires the participation of highly qualified specialists with the necessary level of knowledge and practical experience.
Delivery for patients with severe preeclampsia and its complications is often required to involve allied health specialists (neurosurgeons to remove intracerebral hematomas, abdominal surgeons to suture a ruptured liver capsule, hematologists, transfusiologists to treat hypercoagulability, etc.) Delivery for patients with severe preeclampsia should be carried out in large multidisciplinary hospitals.
Conclusion
Therefore, at present maternal mortality shows a clear downward trend in general, including from preeclampsia. However, there is an alarming steady increase in maternal mortality rates from non-obstetric diseases with concurrent "moderate preeclampsia", according to the reporting documentation.
The standards of care for patients with preeclampsia, eclampsia, HELLP syndrome, and related complications are regulated by clinical guidelines approved by the Ministry of Health of Russia, which is constantly updated and supplemented. A single unified approach to managing this category of patients was associated with decreased amenable and preventable preeclampsia/eclampsia-related deaths in all Russian regions.
Nevertheless, the problems of maternal mortality and the incidence of severe preeclampsia complications in Russia are far from resolved. Professional errors in the management of this category of patients indicate the need to improve quality of specialists' education (both obstetricians-gynecologists and doctors of related medical specialties). Defects in diagnosis, assessment of the severity, and prognosis of severe preeclampsia require measures to improve the quality of care for pregnant women, both in the outpatient and inpatient settings.
Lack of knowledge and understanding of preeclampsia dictates the need for more research that provides insight into the actual cause of this pregnancy complication.
References
- Всемирная организация здравоохранения. Информационные бюллетени. [WHO. Newsletters]. Available at: https://www.who.int/ru/news-room/fact-sheets/detail/maternal-mortality.
- Филиппов О.С., Гусева Е.В. «О материнской смертности в Российской Федерации в 2010 году». Методическое письмо Министерства здравоохранения Российской Федерации № 15-4/3041-07 от 26.09.2011. 41c. [Filippov O.S., Guseva E.V. Methodological letter "On maternal mortality in the Russian Federation in 2010". Methodological letter of the Ministry of Health of the Russian Federation No. 15-4/3041-07 dated 26.09.2011. 41 p. (in Russian)].
- Филиппов О.С., Гусева Е.В., Малышкина А.И., Михайлов А.В., Линде В.А., Зубенко Н.В., Фаткуллин И.Ф., Башмакова Н.В., Артымук Н.В., Пестрикова Т.Ю. Материнская смертность в Российской Федерации в 2015 году. Методическое письмо Министерства здравоохранения Российской Федерации № 15-4/10/2-6810 от 28.10.2016. 85с. [Filippov O.S., Guseva E.V., Malyshkina A.I., Mikhailov A.V., Linde V.A., Zubenko N.V. et al. Maternal mortality in the Russian Federation in 2015. Methodological letter of the Ministry of Health of the Russian Federation No. 15-4/10/2-6810 from 28.10.2016. 85 p. (in Russian)].
- Филиппов О.С., Гусева Е.В. Материнская смертность в Российской Федерации в 2019 году. Методическое письмо Министерства здравоохранения Российской Федерации № 15-4/1285-07 от 08.10.2020. 41с. [Filippov O.S., Guseva E.V. Maternal mortality in the Russian Federation in 2019. Methodological letter of the Ministry of Health of the Russian Federation No. 15-4/1285-07 dated 08.10.2020. 41 p. (in Russian)].
- Say L., Chou D., Gemmill A., Tunçalp Ö., Moller A.B., Daniels J.D. et al. Global сauses of maternal death: A WHO systematic analysis. Lancet Glob. Health. 2014; 2(6): e323-33. https://dx.doi.org/10.1016/S2214-109X(14)70227-X.
- WHO. Global strategy for women’s, children’s and adolescents’ health (2016–2030). New York: Every Woman Every Child; 2015.
- Сухих Г.Т., Ходжаева З.С., Филиппов О.С., Адамян Л.В., Краснопольский В.И., Серов В.Н., Сидорова И.С., Баев О.Р., Башмакова Н.В., Кан Н.Е., Клименченко Н.И., Макаров О.В., Никитина Н.А., Петрухин В.А., Пырегов А.В., Рунихина Н.К., Тетруашвили Н.К., Тютюнник В.Л., Холин А.М., Шмаков Р.Г., Шешко Е.Л. Гипертензивные расстройства во время беременности, в родах и послеродовом периоде. Преэклампсия. Эклампсия. Федеральные клинические рекомендации. Методическое письмо Минздрава России № 15-4/10/2-7138 от 23.09.2013. 61с. [Sukhikh G.T., Khodzhaeva Z.S., Filippov O.S., Adamyan L.V., Serov V.N., Sidorova I.S. et al. Hypertensive disorders during pregnancy, in labor and the postpartum period. Preeclampsia. Eclampsia. Federal clinical guidelines. Methodological letter of the Ministry of Health of the Russian Federation No. 15-4/10/2-7138 from 23.09.2013. 61 p. (in Russian)].
Received 04.12.2020
Accepted 11.12.2020
About the Authors
Iraida S. Sidorova, Dr. Med. Sci., Professor, Academician of the RAS, Merited Scholar of the Russian Federation, Department of Obstetrics and Gynecology № 1,N.V. Sklifosovsky Institute of Clinical Medicine, I.M. Sechenov First MSMU, Ministry of Health of Russia (Sechenov University). E-mail: sidorovais@yandex.ru.
ORCID: 0000-0003-2209-8662. 119991, Russia, Moscow, Trubetskaya str., 8-2.
Natalya A. Nikitina, Dr. Med. Sci., Professor at the Department of Obstetrics and Gynecology № 1, N.V. Sklifosovsky Institute of Clinical Medicine, I.M. Sechenov First MSMU, Ministry of Health of Russia (Sechenov University). E-mail: natnikitina@list.ru. ORCID: 0000-0001-8659-9963. 119991, Russia, Moscow, Trubetskaya str., 8-2.
Oleg S. Filippov, Dr. Med. Sci., Professor, Merited Doctor of the Russian Federation, Deputy Director of the Department of Child’s Health Care and Maternity Services, Ministry of Health of Russia. Tel.: +7(495)627-24-00. 127994, Russia, Moscow, GSP-4, Rakhmanovsky per., 3.
Yelena V. Guseva, Deputy Director of the Department – Head of the Department of Reproductive Health and the Implementation of Effective Obstetric and Gynecological Care, Department of Child's Care and Maternity Services, Ministry of Health of Russia. Tel.: +7(495)627-29-00.
127994, Russia, Moscow, GSP-4, Rakhmanovsky per., 3.
Mikhail B. Ageev, Ph.D., Teaching Assistant at the Department of Obstetrics and Gynecology №1, N.V. Sklifosovsky Institute of Clinical Medicine, I.M. Sechenov First MSMU, Ministry of Health of Russia (Sechenov University). E-mail: mikhaageev@yandex.ru. 119991, Russia, Moscow, Trubetskaya str., 8-2.
Albert A. Kokin, Head of the Department of Anesthesiology and Intensive Care, Maternity Hospital affiliated to the V.V. Veresaev Clinical Hospital of Moscow City Health Department. E-mail: Alberkokin@yandex.ru. 127247, Russia, Moscow, 800th anniversary of Moscow str., 22.
For citation: Sidorova I.S., Nikitina N.A., Filippov O.S., Guseva E.V., Ageev M.B., Kokin A.A. Current issues in preeclampsia: a ten-year analysis of maternal mortality.
Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2021; 4: 64-74 (in Russian)
https://dx.doi.org/10.18565/aig.2021.4.64-74



