Uterine ruptures in modern obstetrics
Objective. To provide the current classification of spontaneous uterine ruptures, which is based on the features of their etiopathogenesis and clinical presentations, and to prove the feasibility of organ-sparing surgery for uterine injury.Savelyeva G.M., Kurtser M.A., Breslav I.YU., Konoplyannikov A.G., Latyshkevich O.A.
Materials and methods. A total of 281 histories of labor complicated by uterine rupture were retrospectively analyzed. Births occurred in the obstetric facilities of the Moscow Healthcare Department in 1997 to 2018.
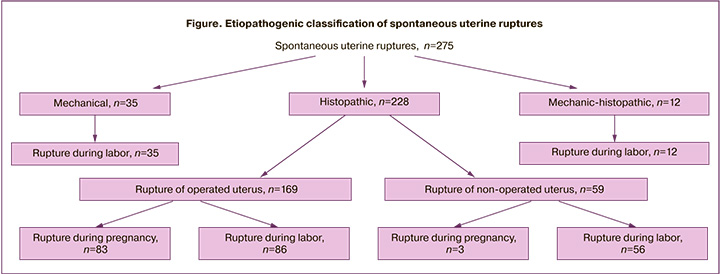
Results. In accordance with the proposed classification, the investigators identified patients with violent
(n = 6) and spontaneous (n = 275) uterine rupture; among the latter, there were patients with mechanical rupture (n = 35), histopathic rupture along the scar (n = 169), histopathic rupture of the unoperated uterus (n = 59), and mechanohistopathic rupture (n = 12).
Conclusion. The leading cause of rupture is a uterine scar after cesarean section and endoscopic myomectomy. The rupture of the operated uterus has clear step-by-step symptoms that a physician of any specialty should know in order to timely save the fetus’s life and to promote the mother’s health. In case of uterine rupture of any etiology, organ-sparing surgery is shown to be expedient during instrumental autoerythrocyte suspension reinfusion that makes it possible not only to reduce operative blood loss, but also to preserve a woman's reproductive function.
Keywords
Uterine rupture (UR) is a serious complication threatening the life and health of both the mother and the fetus.
According to the WHO, the incidence of UR in the world is 0.053–0.07% on average, or 5.3–7 per 10,000 labors, with rather low rates in the developed countries: ini Australia – 8,6, Canada – 3, Ireland – 2,3, Singapore – 1,6, USA – 0,67–1,3 per 10 000 labors, and high rates in the developing countries: Nigeria, Ephiopia, Pakistan, Yemen – 50–263 per 10 000 labors [1–3].
According to Rosstat, in Russia in 2018, the incidence of UR was 1,6 per 10 000 labors [4]. According to the data obtained in Division of Organization and Methodology of Moscow Healthcare Department, the incidence of UR in 2018 was 3,2 per 10 000 labors.
Since the appearance of publications on obstetrics in the world, many authors noted, that a change in the uterus wall along with the disparity between the size of the fetus and the mother's pelvis is of great importance in the occurrence of UR. Deliveries with UR were mainly through the vaginal birth canal (even if the insertion of the fetus into the abdominal cavity was total or partial). Destructive operations on the fetuses were widely used, and the maternal mortality rate was almost 100% [5].
In 1875, L. Bandel described in detail the stages and symptoms of UR that occur during childbirth when the size of the pelvis and the presenting part do not match (or due to the transverse position of the fetus). He used 13 personal observations and 26 autopsy results. The symptoms complex described by the author was called «Bandelevsky rupture», and subsequently, UR was called «mechanical» in Russia [6].
Many obstetricians believed that UR may occur only if the uterine wall is pathologically changed due to some reason, considering such ruptures to be asymptomatic [7].
Evaluation of the results in 262 patients with UR conducted by L.S. Persianinov (1952) were of great importance for the obstetricians in Russia. He was the first to create a clear classification of URs and divided them by pathogenesis into forced and spontaneous, and the latter, depending on the predominance of one or another etiological factor, into mechanical ruptures (discrepancy between the sizes of the presenting part and the pelvis); histopathic (morphological changes in the uterine wall); and mechanical-histopathic (in presence of both adverse factors). Besides, in his classification the author specifies uterine ruptures in accordance with the clinical course into threatening, ongoing and completed; uterine fissure; partial and complete (full-thickness); in accordance with localization: in fundus, body, lower segment; separation of the uterus from the vaginal vaults [6].
Accepting L.S. Persianinov’s classification, M.A. Repina (1984) made some amendments to it: she rejected the concept of uterine fissure and suggested to consider the histopathic rupture as typical. She insisted on the absence of a specified clinical picture of the ongoing rupture, distinguishing between «the risk of rupture», «threatening rupture» and «completed uterine rupture» [8].
Currently, the terms rupture of an unscarred uterus and rupture of the scarred uterus are used abroad – uterine rupture of unoperated and operated uterus, respectively. Williams Obstetrics (2018) proposes to distinguish primary uterine rupture (primary, in unoperated uterus) and secondary uterine rupture (secondary, in operated uterus) [9].
Specifying uterine ruptures exclusively in operated and unoperated uterus, does not allow to diagnose UR in cases of: 1) mismatch in size between pelvis and birth canal; 2) changes in the uterine wall, but without surgical intervention (high parity, curettage, metroendometritis, etc.).
Which classification is expedient for the use in Russia? The attitude to the symptoms of UR is ambiguous. Some authors believed that in patients with a scar on the uterus, the rupture is asymptomatic, others assumed that there are symptoms, but they can be identified only in a targeted survey, which requires the knowledge about them [8, 10, 11].
There is no common point of view among the obstetricians regarding the volume of surgery for UR. According to a number of foreign authors, until present, a high percentage (51–87%) of hysterectomies still remain in a number of countries and regions. [12]. Recent researches conducted in Moscow, which were initiated by M.A. Kurtser – Head Specialist of Moscow Healthcare Department, who participated in performing surgery in different maternity hospitals from 2003 to 2013, showed expediency of organ-sparing interventions [10, 13–15].
The purpose of this work is to assess the expediency of URs classification adopted in Russia, basing on the analysis of 275 births with UR, our country and to show the priority importance of organ-sparing surgeries.
Materials and methods
A retrospective analysis of 281 births in women with UR history, which took place in maternity hospitals of Moscow Healthcare Department from 1997 to 2018; 5 women were followed for long-term results.
Results and discussion
We consider to keep the terms «mechanical» and «histopathic» ruptures to distinguish different forms of spontaneous ruptures.
We have excluded forced URs from the proposed scheme, as they differ in pathogenesis from the spontaneous ruptures. Forced ruptures include traumatic URs, caused by non-operative trauma, and iatrogenic URs resulting from the performance of obstetric surgery without appropriate observation conditions. Such ruptures occurred in 6 patients: in 3 patients where obstetric forceps were applied to the head located over the narrow part of the pelvic cavity, and in 3 patients with vacuum extraction. In all patients, the rupture was localized along the edge of lower uterine segment, in 2 of them it extended to the uterine body. Full-thickness rupture was diagnosed in 3 women, partial – in 3.
Etiopathogenic classification of spontaneous URs worked out on the base of analysis of 275 labors in women with in Moscow from 1997 to 2018, is shown on the figure.
As follows from the above presented data, fewer observations refer to the mechanical type of rupture. According to the Moscow Healthcare Department, their number decreased from 23.8% in 2005 г. to 5.1% in 2018 г. The occurrence of mechanical ruptures is explained by the late diagnosis of an obstructed pelvis and inability of manual estimation of fetal weight (the doctors rely only on the results of ultrasound fetometry, which are not always accurate). Among the patients with mechanical UR, fetus weight was ≥4000g in 31 women (88.6%), 4500–4999 g in 4 cases, 5000–5420 g – in 4 patients. In all patients with large or giant fetuses, pelvic size was normal. In patients with fetal birth weight 4500 g and more, the estimated fetal weight according to ultrasound parameters was not indicated in the case record.
According to many authors, starting from K. Bandel, the clinical picture of UR of any genesis comprises the following stages: threatening, ongoing and completed rupture (partial or full-thickness) [6, 8, 10].
In prevention of any type of UR the identification of symptoms of threatening and ongoing ruptures, which nature is determined by etiology, is of great importance.
Mechanical uterine rupture
The symptoms of threatening UR are determined by overstretching of the lower uterine segment:
- complaints on painful contractions, if epidural anesthesia was not administered, difficulty in urinating;
- on examination: high, oblique arrangement of the contraction ring, asymmetric location the round ligaments, overstretched palpable bladder above the uterine bed;
- in vaginal examination the cervix is edematous, cervical dilatation is almost complete, big labor tumor is on fetal head.
Some obstetricians thought, that hematuria may be present in case of threatening UR [11]. This is really possible if the fetal head stays for a long time in the same plane of the pelvis due to the clinical discrepancy between the pelvis and the head size and compression of the urethra, but at present, such expectant management of labor is rare.
The symptoms of ongoing UR are related to the damage of the uterine wall and a hematoma formation, and are similar to the abruption of normally located placenta (hypertonic uterine dysfunction, impaired cardiac activity of the fetus, vaginal bleeding). The pressure the fetal bruising head on the sacrum and the pelvic diaphragm result in expulsive contractions. In case of an ongoing UR, there may be no vaginal bleeding (this symptom is not obligatory), but the occurrence of vaginal bleeding always indicates the ongoing UR.
According to the obtained data, in the presence of the above described symptoms of an ongoing UR, the following diagnoses were made as an indication for emergency operative delivery: obstructed pelvis – in 4 patients, premature abruption of normally located placenta – in 4 patients, acute fetal hypoxia – in 4 patients. URs were detected intraoperatively, and this confirms the untimely and incorrect diagnosis of the incipient uterine rupture in 12 women in labor.
Full-thickness completed rupture (in 16 patients) was not difficult to diagnose:
- Labor contractions stopped, the «silence» sets in (unfortunately, in case records this symptom is documented only in 2 patients in labor).
- The signs of a pain shock combined with hemorrhagic shock were present in all women in labor.
In case of partial rupture (19 patients), the hematoma was formed either under the plica vesico-uterina (7 cases), or between the broad ligaments of the uterus (12 cases, including 2 cases of retroperotoneal hematoma spread to the kidney).
The clinical symptoms of partial UR were:
- pain in the lower abdomen in the 3rd and/or early postpartum period (7 patients);
- weakness, dizziness, tachycardia, hypotension (6 patients);
- vaginal bleeding (9 patients);
- diagnosis may be confirmed by palping or ultrasound.
Palpation of the uterus is an important test increasing the likelihood of the correct diagnosis of UR. Of 23 patients, who gave birth spontaneously, manual examination of the uterine cavity was performed in 20 women in labor; UR was detected in 13 (65%) patients, not detected in 7 (35%).
In patients with an unidentified UR before surgery, the indication for laparotomy was: vaginal bleeding not responding to conservative therapy – in 4 women, deterioration of the general condition and the signs of intra-abdominal hemorrhage – 4, echographic signs of hematoma in the parametria – in 2.
The above data prove that it is not always possible to detect PM by manual examination, therefore it should be carried out by a highly qualified obstetrician and only once.
The newborns’ health at birth was estimated as satisfactory in 9 (25.7%) babies, mild birth asphyxia in 13 (37.1%), moderate asphyxia in – 4 (11.4%), heavy asphyxia in 5 (14.3%), intranatal death was in 4 (11.4%).
Histopathic uterine ruptures
Most of the observations were histopathic ruptures; 169 (61.5%) of these occurred along the uterine scar, in 71 (25.8%) the rupture affected an unoperated uterus.
Of 169 patients with rupture after uterine surgery, 112 (66.3%) had a scar after cesarean section, 43 (25.4%) – after myomectomy, 12 (7.1%) after the uterine tube excision, and 2 (1.2%) – after deep infiltrative endometriosis excision.
Previous uterine surgery is a prevailing cause of rupture in many countries of the world. There is an obvious direct correlation between the increase in the incidence of UR in the scar and the widespread progressive increase in the frequency of caesarean section already being performed in more than 25% of women in Russia, Europe, and the United States. In China and some countries in South America the rate reaches 50–70% [16–18].
According to Zharkin (2018) [19], Y.X. Li (2019) [20], the UR in the scar after cesarean section occur in 70–90% of all the ruptures of the operated uterus. In our study UR along the scar after cesarean section occurred in 40 (35,7%) women, in labor – in 72 (64,3%) .
Expansion of indications for organ-sparing surgery for uterine myoma resulted in an increase of the UR along the scar after laparoscopic myomectomy hysteroresectoscopy. Intramural (types 2–5 according to FIGO classification) myoma removal, the use of electrocoagulation, inadequate suturing result in the formation of an insufficient scar with the risk of UR in subsequent pregnancy. In 36 (83.8%) out of 43 patients with uterine rupture along the scar after myomectomy, the rupture occurred during pregnancy in the absence of labor. In 7 (16.2%) patients, the rupture occurred during labor.
Among 15 patients with uterine scar after uterine tube excision (12 patients with ectopic pregnancy) and excision of deep infiltrative endometriosis (2 patients), UR during pregnancy occurred in 7 (50%) patients, during labor – in 7 (50%).
In total, among the patients with histopathic uterine rupture along the scar, the rupture occurred during pregnancy in 83 (49.1%) patients, during labor – in 86 (50.9%).
It is diffictult to diagnose histopathic UR at the initial stage due to very few symptoms, and it is necessary to know them in order actively to detect threatening UR.
The symptoms of histopathic uterine rupture along the scar during pregnancy
The analysis of 83 cases of rupture of operated uterus (along the scar), in 52 (62.7%) there were signs of a threatening UR. The patients complained of nausea, vomiting, epigastric pain and lower abdominal pain: in 1 of them, the above symptoms made the doctors suggest acute appendicitis; in 1 patient after past story of laparoscopic myomectomy, a differential diagnosis of renal colic was questioned. The rest 31 (37.3%) patients had no complaints of this kind or these were ignored (not mentioned in the medical records).
The ongoing UR is defined as a rupture of the uterine wall along the scar with hematoma formation in the rupture area, leading to uterine hypertonus and fetal hypoxia (bradycardia). Vaginal bleeding is decisive for the diagnosis in 100% of cases. All patients had abdominal pain. In 13 (15.7%) patients, vaginal bleeding was noted.
Many authors join the symptoms of a threatening and ongoing UR. It should be assumed that identification of the symptoms of a threatening UR in patients with a scar accelerates the decision to perform a caesarean section. [21–23].
The signs of a completed UR depend on the scar localization and the character of the uterine injury: full-thickness or partial rupture.
Histopatic uterine rupture along the scar during labor
Histopathic UR usually occurs in the process of spontaneous labor, labor induction or activation. According to I. Al-Zirqi et al. (2019), C. Vachon– Marceau (2016), the use of prostaglandins and oxytocin in patients with uterine scar is associated with a doubled risk of UR [24, 25].
The symptoms of a threatening UR along the scar during labor are similar to those during pregnancy and include nausea, vomiting, abdominal pain and painful scar. These complaints in various combinations were in 79 (91.9%) of 86 patients. A specific sign of a threatening UR along the scar is weakness or discoordination of labor contractions [26, 27].
Among the analyzed cases, weak contractions were seen in 7 (8,1%) patients, discoordination – in 2 (2,3%). With ongoing UR along the scar during labor, abdominal pain increases, the uterus remains hypertonic accompanied by impaired placental blood flow, fetal hypoxia; these events were documented in medical records of 47 (54.7%) patients, but uterine rupture was suspected only in 28 of them. They underwent a caesarean section, during which UR was discovered. The symptoms of UR were: an impairment of fetal cardiac function alone (in 4 women), or a combination of pain in the scar area, vaginal bleeding and poor contractions.
Spontaneous labor occurred in 19 (40.4%) patients; in 16 of these late and variable decelerations occurred at the end of the second stage of labor, and the babies were born with mild asphyxia. Uterine wall defect was detected in the early postpartum period during manual examination of the uterus.
The completed uterine rupture along the scar during pregnancy and labor may be full-thickness or partial. In our study 73 (43,2%) women had a full-thickness rupture, 96 (56,8%) – a partial rupture.
The completed partial UR along the scar is characterized by formation of hematoma under vesicouterine fold or between the broad ligaments of the uterus. If this happens during pregnancy, there is abdominal pain, hypertonic uterus and fetal hypoxia. The cessation of labor contractions is added to the listed symptoms during labor. The volume of hematoma and the speed of its growth determine the intensity of the symptoms: weakness, pain in the lower abdomen, skin pallor, low blood pressure.
In full-thickness uterine rupture the severity of clinical picture is determined by the volume of blood loss. 25 patients developed hemorrhagic shock with complete UR; the blood loss varied from 1000 to 3200 ml. The scar after cesarean section was in 17 out of 25 patients, the scar after myomectomy – in 8.
Health condition in babies (173 babies, out of them 4 twins) born in women with operated uterine rupture was satisfactory in 61 (35.3%) newborns, mild asphyxia in 52 (30.1%), moderate asphyxia – in 18 (10.4%), severe asphyxia – 13 (7.5%), antenatal and intranatal deaths were in 29 (16.7%).
Histopathic ruptures of unoperated uterus usually occurred during labor (56 patients). In 3 patients the rupture at 23, 24 and 27 weeks of gestation were associated with the pregnancy in the rudimentary uterine horn.
Histopathic ruptures of unoperated uterus are known to be associated with high parity of women in labor [28]. In our study high parity was noted only in 5 (8.9%) of 56 patients. Abortions by curettage, which took place in 41 (73.2%) patients, seemed to be the most important predisposing factor. Due to this, some authors proposed to consider UR in patients after curettage as the rupture of the operated uterus, since the possibility of partial or complete perforation of the uterus at previous intervention can never be ruled out [29, 30]. 2 patients underwent laparoscopic adnexectomy and ovarian resection. Labor cotranctions were activated by oxytocin in 4 (7.1%) women. Complicated course of previous labor (poor contractions, application of Christaller's maneuver, manual removal of the placenta) was observed in 10 (17.9%) women.
In more than half of patients – in 30 (53.6%) – the rupture was located along the lower uterine segment. In the remaining 26 women, the atypical localization of rupture to some extent suggested possible previous trauma to uterine wall: 24 patients had past history of curettage and scarring of the uterine wall after supposed perforation of the uterus. In 8 patients, UM occurred along the posterior uterine wall, in 8 – in the uterine fundus, in 8 – along the anterior wall. In 2 patients (after adnexectomy and laparoscopic resection of the ovary), localization of the defect allows to suggest previous thermal injury to myometrium when using electrosurgery.
The ruptures of unoperated uterus are very often either asymptomatic or with the signs that mimic another pathology, indicating cesarean section. It is extremely difficult to diagnose a rupture of an unoperated uterus with a predominance of the histopathic component during labor. Often, it manifests itself only in the postpartum period.
In 30 out of 34 patients with vaginal delivery, due to bleeding in the early postpartum period or the birth of a baby with severe asphyxia, a manual examination of the uterine cavity was carried out, and in 20 (66.7%) women in labor a rupture was found, and in 10 (33.3%) it was rejected. Subsequently, due to the continuing uterine bleeding (in 4 women in labor) or a deterioration of general condition (in 6 patients), laparotomy was performed and UR was detected.
In order not to overlook UR, it is necessary to monitor the state of a woman in labor during the first hours.
A rupture with the last bearing-down efforts is typical for UR with no preexisting uterine scar, so a child is born without the signs of asphyxia.
In 22 out of 34 patients under study the babies were born in satisfactory condition.
Delivery in 22 patients was provided by an emergent caesarean section; placental abruption and bleeding were assumed to be an indication for surgery in 12 patients, severe fetal hypoxia – in 8, poor contractions – in 2. URs were detected intraoperatively in all patients.
The diagnosis of histopathic UR after spontaneous labor was set on clinical manifestations and ultrasound data immediately after delivery, and was confirmed during laparotomy.
With the completed UR laparotomy is absolutely necessary.
The condition of babies at birth was considered as satisfactory in 17 (28.8%) newborns, 18 (30.5%) were born with mild asphyxia, 2 (3,5%) - with moderate asphyxia, 12 (20.3%) with severe asphyxia; intranatal deaths occurred in 10 cases (16.9%).
Mechanical-histopathic ruptures
Among the analyzed birth records, a group of mechanical-histopathic URs can be distinguished, in which 12 patients were included, among them 5 (41.7%) women were primiparas, 2 (16.7%) – with high parity. 7 (58.3%) women had past history of abortion and curettage. The symptoms of an obstructed labor could be assumed in 9 (75%) patients, since 5 of these patients gave birth to babies weighing 4000–4200 g; 4 patients were diagnosed with an anatomic obstruction to labor (uniformly narrowed, transversely narrowed pelvis). The labor induction with oxytocin was used in 4 (33.3%) women, preparation of the cervix with prostaglandins was carried out in 3 confirmed the mechanical origin of the rupture in 11 (91.7%) women. Deliveries in 7 (58.3%) women were via caesarean section. The indications for surgery were: acute fetal hypoxia – in 5 women, weak labor strictures – in 1, premature abruption of normally located placenta – in 1. Spontaneous delivery was observed in 5 women, in which UR was detected during manual examination of the uterus for hypotonic bleeding in the early postpartum period.
Health condition in babies at birth was satisfactory in 4 (33,3%) newborns, mild asphyxia was noted in in 3 (25%), moderate asphyxia – in 2 (16,7%), severe asphyxia – in 1 (8,3%), intranatal deaths occurred in 2 (16,7%).
Medical tactics (surgical treatment of uterine rupture)
Over the last decades, the volume of surgery for UR repair has changed a lot. The mostly used hysterectomy was replaced by organ-sparing surgery: 1) stitching the rupture with separate sutures using absorbable suture material; 2) the crushed tissues can be excised with further suturing to close the defect. In 2004, in obstetric institutions of Moscow Health Department, hysterectomy was performed in 68.7% of patients with UR; in 2018, it was possible to suture the ruptures in all patients. The major reason for the widespread introduction of organ-sparing surgeries was the evidence of the decrease in the volume of blood loss by 2.2 times in suturing a rupture compared to laparotomy [10, 13–15]. Out of 275 analyzed patients with URM, ruptures were sutured in 262 (95.3%). Hysterectomy was performed only in 13 patients. It became possible to save a woman's life with a massive blood loss (sometimes up to 6000 ml), thanks to the introduction of instrumental reinfusion of autologous erythrocytes [13]. In our series reinfusion was carried out in 115 (43.9%) patients, allohemotransfusion was carried out in 128 (48.9%).
The performance of organ-sparing surgeries is aimed at both reducing complications in mothers and preserving their reproductive potential. In our study 5 patients reported of pregnancies after UR and had full-term deliveries by elective cesarean section. Despite the fact that the number of births was not large, none of patients complained on infertility.
Conclusion
To prevent UR, all obstetricians-gynecologists in the outpatient clinics and hospitals should know the pathogenesis of this dangerous complication of pregnancy and labor, its first symptoms, and be ready to perform laparotomy promptly. Timely diagnosis of an obstructed pelvis, careful selection of patients with uterine scar are important for reducing the risk of this life-threatening condition.
Prevention of UR includes the efforts to reduce the number of cesarean sections, especially due to relative indications for surgical delivery.
To avoid insufficient scars after myomectomy it is advisable that nodes of types 2–5 are removed by laparotomy, since this access provide more adequate suturing of the uterine wound.
Organ-sparing surgery is a method for choice for managing UR, and only in extreme situations of crushed edges of the rupture wound, hysterectomy should be considered, as well as in cases of otherwise untreatable hemorrhagic shock.
Surgical interventions in patients with UR should be performed against the background of reinfusion of autologic erythrocytes, which significantly reduces the need for for fresh frozen plasma and for transfusion of donor blood.
References
- Motomura K., Ganchimeg T., Nagata C., Ota E., Vogel J.P., Betran A.P. et al. Incidence and outcomes of uterine rupture among women with prior caesarean section: WHO Multicountry Survey on Maternal and Newborn Health. Sci. Rep. 2007; 7: 44093. https://dx.doi.org/10.1038/srep44093.
- Augustin G. Acute abdomen during pregnancy. Springer; 2018. https://dx.doi.org/10.1007/978-3-319-72995-4_16.
- Fitzpatrick K.E., Kurinczuk J.J., Bhattacharya S., Quigley M.A. Planned mode of delivery after previous cesarean section and short-term maternal and perinatal outcomes: A population-based record linkage cohort study in Scotland. PLoS Med. 2019; 16(9): e1002913. https://dx.doi.org/10.1371/journal.pmed.1002913.
- Основные показатели деятельности акушерско-гинекологической службы в Российской Федерации в 2018 году. М.: Министерство здравоохранения Российской Федерации, Департамент медицинской помощи детям и службы родовспоможения; 2019. [Key performance indicators of obstetric/gynecological service in the Russian Federation in 2018. Ministry of Health of the Russian Federation. Department for Child Care and Obstetric Services. Moscow; 2019 (in Russian)].
- Поповъ Д.Д. Терапiя родовъ при узкомъ тазе. С.-Петербургъ: Издательство «Практическая Медицина»; 1912. [Popov D.D. Therapy for childbirth with a narrow pelvis. Saint Petersburg. Practical Medicine Publishing House; 1912. (in Russian)].
- Персианинов Л.С. Разрывы матки. М.: Медгиз; 1952. [Persianinov L.S. Uterne ruptures. Moscow, Medgiz; 1952. (in Russian)].
- Вербов Я.Ф. Матка женщины, ея нормальная работа и ея разрывы во время родовъ. С.-Петербургъ: Типо-литографiя «ЕВГ. ТИЛЕ пр.» Адмиралтейскiй канн. 17; 1913. [Verbov Ya.F. A woman’s uterus, its normal work and its ruptures during childbirth. Saint Petersburg. Typo-lithography “EVG. TILE pr. "Admiralteyskiy cann. 17; 1913. (in Russian)].
- Репина М.А. Разрыв матки. Л.: Медицина. 1984. [Repina M.A. Uterine rupture. Leningrad. “Meditsina”. 1984. (in Russian)].
- Cunningham F.G., Leveno K.J., Bloom S.L., Dashe J.S., Hoffman B.L., Casey B.M.,Spong C.Y. Williams obstetrics. 25th ed. McGraw-Hill; 2018. 132 p.
- Савельева Г.М., Бреслав И.Ю. Разрыв оперированной матки во время беременности и родов. Вопросы гинекологии, акушерства и перинатологии. 2015; 14(3): 22-7. [Savelyeva G.M., Breslav I.Yu. Rupture of the operated uterus during pregnancy and childbirth. Voprosy Ginekologii, Akushertsva i Perinatologii/Problems of Gynecology, Obstetrics, and Perinatology. 2015; 14(3): 22-7. (in Russian)].
- Полякова В.А. Практическое акушерство. Тюмень: Печатник; 2012. 528 с. [Polyakova V.A. Practical obstetrics. Tyumen: OOO “Pechatnik”; 2012. 528 p. (in Russian)].
- Pokhrel Ghimire S.S. Uterine rupture: shifting paradigm in etiology. Kathmandu Univ. Med. J. (KUMJ). 2018; 16(62): 146-50.
- Савельева Г.М., Курцер М.А., Бреслав И.Ю., Бреусенко Л.Е., Латышкевич О.А., Штабницкий А.М. Опыт использования аппарата Haemonetics Cell Saver 5+ в акушерской практике. Акушерство и гинекология. 2013; 9: 64-71. [Savelyeva G.M., Kurtser M.A., Breslav I.Yu., Breusenko L.E., Latyshkevich O.A., Shtabnitsky A.M. Experience with a Haemonetics Cell Saver 5+ device in obstetric practice. Akushertsvo i Ginekologiya/Obstetrics and Gynecology. 2013; 9: 64-71. (in Russian)].
- Савельева Г.М., Бреслав И.Ю. Разрыв неоперированной матки во время родов. Российский вестник акушера-гинеколога. 2016; 16(2): 4-10. [Savelyeva G.M., Breslav I.Yu. Rupture of the unoperated uterus during childbirth. Rossiyskiy Vestnik Akushera-Ginekologa/Russian Bulletin of Obstetrician/Gynecologist. 2016; 16 (2): 4-10 (in Russian)].
- Бреслав И.Ю. Кровотечения при поздних сроках беременности и во время родов. Возможности органосохраняющих операций. Акушерство и гинекология. 2016; 10: 52-8. [Breslav I.Yu. Bleeding during late pregnancy and childbirth. The possibilities of organ-sparing surgery. Akushertsvo i Ginekologiya/Obstetrics and Gynecology. 2016; 10: 52-8 (in Russian)]. https://dx.doi.org/10.18565/aig.2016.10.52-8.
- Euro-Peristat Project with SCPE and EUROCAT. European perinatal health report: The Health and care of pregnant women and babies in Europe in 2010-2013. Available at: http://www.europeristst.com/ Accessed June 4, 2016.
- Chen Y., Han P., Wang Y.J. Risk factors for incomplete healing of the uterine incision after cesarean section. Arch. Gynecol. Obstet. 2017; 296(2): 355-61. https://dx.doi.org/10.1007/s00404-017-4417-6.
- Cox K.J., Bovbjerg M.L., Cheyney M., Leeman L.M. Planned home VBAC in the United States, 2004-2009: outcomes, maternity care practices, and implications for shared decision making. Birth. 2015; 42(4): 299-308. https://dx.doi.org/10.1111/birt.12188.
- Zharkin N., Prohvatilov S., Burova N., Gavrilchuk T., Snigur G. Fertility-preserving surgery for post-Caesarean uterine scar dehiscence in a pregnant patient. Eur. J. Obstet. Gynecol. Reprod. Biol. 2018; 221: 189-90. https://dx.doi.org/10.1016/j.ejogrb.2017.11.023.
- Li Y.X., Long D.J., Wang H.B., Wu Y.F., Reilly K.H., Huang S.R. et al. Predicting the success of vaginal birth after caesarean delivery: a retrospective cohort study in China. BMJ Open. 2019; 9: e027807. https://dx.doi.org/10.1136/bmjopen-2018-027807.
- Eshkoli T., Weintraub A.Y., Baron J., Sheiner E. The significance of a uterine rupture in subsequent birth. Arch. Gynecol. Obstet. 2015; 292(4): 799-803. https://dx.doi.org/10.1007/s00404-015-3715-0.
- Landon M.B. Implications of the rising frequency of uterine rupture. BJOG. 2016; 123(5): 676-7. https://dx.doi.org/10.1111/1471-0528.13482.
- Al-Zirqi I., Daltveit A.K., Forsen L., Stray-Pedersen B., Vangen S. Risk factors for complete uterine rupture. Am. J. Obstet. Gynecol. 2017; 216: 165. e1-8. https://dx.doi.org/10.1016/j.ajog.2016.10.017.
- Vachon-Marceau C., Demers S., Goyet M., Gauthier R., Roberge S., Chaillet N. et al. Labor dystocia and the risk of uterine rupture in women with prior cesarean. Am. J. Perinatol. 2016; 33(6):577-83. https://dx.doi.org/10.1055/s-0035-1570382.
- Al-Zirqi I., Daltveit A.K., Vangen S. Maternal outcome after complete uterine rupture. Acta Obstet. Gynecol. Scand. 2019; 98(8): 1024-31. https://dx.doi.org/10.1111/aogs.13579.
- You S.H., Chang Y.L., Yen C.F. Rupture of the scarred and unscarred gravid uterus: outcomes and risk factors analysis. Taiwan. J. Obstet. Gynecol. 2018; 57(2): 248-54. https://dx.doi.org/10.1016/j.tjog.2018.02.014.
- Islam A., Shah A.A., Jadoon H., Fawad A., Javed M., Abbasi A.U. A two-year analysis of uterine rupture in pregnancy. J. Ayub. Med. Coll. Abottabad. 2018; 30(4, Suppl. 1): S639-41.
- Astatikie G., Limenih M.A., Kebede M. Maternal and fetal outcomes of uterine rupture and factors associated with maternal death secondary to uterine rupture. BMC Pregnancy Childbirth 2017; 17(1): 117-6. https://dx.doi.org/10.1186/s12884-017-1302-z.
- Mourad W.S., Bersano D.J., Greenspan P.B., Harper D.M. Spontaneous rupture of unscarred uterus in a primigravida with preterm prelabour rupture of membranes. BMJ Case Rep. 2015;2015: bcr2014207321. https://dx.doi.org/10.1136/bcr-2014-207321.
- Martin J.A., Hamilton B.E., Osterman M.J., Curtin S.C., Matthews T.J. Births: final data for 2013. Natl. Vital Stat. Rep. 2015; 64(1): 1-65.
Received 29.04.2020
Accepted 07.05.2020
About the Authors
Galina M. Savelieva, MD, PhD, Professor, member of the Russian Academy of Sciences, Professor of the Department of Obstetrics and Gynecology, Pediatric Faculty,N.I. Pirogov Russian National Research Medical University. Tel.: +7(495)718-34-72. E-mail: gms@cfp.ru. ORCID: 0000-0001-8735-1281.
117997, Russia, Moscow, Ostrovitianov str., 1.
Mark A. Kurtser, MD, PhD, Professor, member of the Russian Academy of Sciences, Head of Department of Obstetrics and Gynecology, Pediatric Faculty,
N.I. Pirogov Russian National Research Medical University. Tel.: +7(495)719-78-96. E-mail: m.kurtser@mcclinics.ru. ORCID: 0000-0003-0175-1968.
117997, Russia, Moscow, Ostrovitianov str., 1.
Irina Yu. Breslav, MD, PhD, Head of the Department of Pathology of pregnancy, Hospital MD GROUP.
Tel.: +7(495)331-44-85. E-mail: irina_breslav@mail.ru. ORCID: 0000-0002-0245-4968. 111720, Russia, Moscow, Sevastopol Ave., 24/1.
Alexander G. Konoplyannikov, MD, PhD, Professor of the Department of Obstetrics and Gynecology, Pediatric Faculty, N.I. Pirogov Russian National Research Medical University. Tel: +7(499)723-04-20. E-mail: npo.med@gmail.com. ORCID: 0000-0001-9923-8833. 117997, Russia, Moscow, Ostrovitianov str., 1.
Oleg A. Latishkevich, PhD, Chief of the Center of Family Planning and Reproduction.
Tel: +7(495)718-20-70. E-mail: cpsr@zdrav.mos.ru. ORCID: 0000-0003-1643-7576. 117209, Russia, Moscow, Sevastopol Ave., 24a.
For citation: Savelyeva G.M., Kurtser M.A., Breslav I.Yu., Konoplyannikov A.G., Latyshkevich O.A. Uterine ruptures in modern obstetrics.
Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2020; 9: 48-55 (in Russian).
https://dx.doi.org/10.18565/aig.2020.9.48-55