Non-penetrating uterine rupture along the scar after cesarean section and dehiscence/aneurysm of the uterine scar in the second half of pregnancy and during childbirth
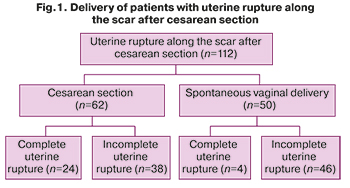
Aim. To provide scientific substantiation of the distinction between the notions “incomplete uterine rupture after surgery” and “dehiscence/aneurysm of the uterine scar during pregnancy and childbirth”. Materials and methods. A retrospective analysis of 112 birth histories with uterine rupture along the scar after cesarean section, 44 birth histories of patients with dehiscence/aneurysm of the uterine scar after cesarean section and myomectomy was carried out. The births took place in maternity hospitals of Moscow Department of Healthcare, clinical hospital MD Group in the period from 1999 to 2018. Results. Out of 112 patients with uterine rupture along the scar after cesarean section, delivery by re-surgery was in 62 patients, spontaneous delivery was in 50. Out of 62 patients with abdominal delivery, the risk symptoms of uterine rupture were in 53, and the incipient uterine rupture was in 48 women. Out of 50 patients, uterine rupture after spontaneous delivery was in 49 women in early postpartum period. Out of 112 babies, 5 were born dead, 3 – with severe asphyxia, and 6 – with moderate asphyxia. In 29 patients, the total blood loss volume was more than 1000 ml. Dehiscence/aneurysm of the uterine scar had common signs: the patients had no complaints, ultrasound examination detected very thin lower uterine segment (<1 mm), pregnancy was prolonged to full-term or almost full-term pregnancy, the intraoperative scar dehiscence was seen as a translucent bulging into the gestational sac and blood loss during cesarean section was within the typical range for the blood loss. Conclusion. The notion “dehiscence/aneurysm of the uterine scar” should be distinguished from “incomplete uterine rupture”, since the concept of commonality of these notions will justify the doctors and contribute to their incompetence. The doctors should know both the symptoms of the risk for uterine rupture and the incipient uterine rupture.Savelyeva G.M., Kurtser M.A., Breslav I,Yu., Karaganova E.Ya., Neklyudova Yu.G.
Keywords
Uterine rupture (UR) remains a serious problem for obstetricians in all countries, as it is a dangerous complication for both mother and baby. In Russia (according to the data of the Ministry of Health of RussiaВ России), 4 women died due to UR in 2015, 2 in – 2016, 0 – in 2017, 4 – in 2018, 5 – in 2019. For the recent 20 years (1999-2018), perinatal outcomes based on the analysis of 281 birth histories with UR in various maternity hospitals of Moscow Department of Healthcare were as follows: the rate of ante- and intranatal fetal deaths was 14.9%, 13.2% of infants were born with severe asphyxia [1, 2].
It is believed, that probability of severe complications for the mother and fetus due to UR is an indicator of unsatisfactory work performance in a healthcare setting. In the latter circumstance, some doctors, instead of the diagnosis of “incomplete uterine rupture along the scar”, interpret the situation as “uterine scar dehiscence”. On the one hand, inaccurate terms definition leads to delayed diagnosis of incomplete UR and sometimes initial signs of complete UR, on the other hand, to underestimation of this serious complication.
Both in our country and abroad, incomplete (or non-penetrating) uterine ruptures include the ruptures without disrupting the integrity of the vesicouterine peritoneal fold and/or the leaves of the broad ligament. Complete (or penetrating) UR implies rupture into the peritoneal cavity, including visceral peritoneum with occurrence of blood, amniotic fluid, and sometimes fetal parts or the whole body of the fetus in the peritoneal cavity.
All researchers point out, that complete UR is not difficult to diagnose, since it is accompanied by pain and hemorrhagic shock, severe asphyxia or fetal death.
Detection of completed UR indicates that the threatening diagnosis was established untimely and the incidence of catastrophic outcome [1, 2].
In the last decade, a significant number of publications described uterine scar dehiscence after cesarean section [3–6]. According to the authors, this condition is most commonly found during the repeated cesarean section and is considered as a “finding”. Sometimes, scar dehiscence forms the so-called "uterine windows" that may allow the fetal parts to be seen. It should be noted that the patients had no complaints, and cardiotocography showed, that fetal condition was satisfactory. Williams Obstetrics (2018) noted, that the integrity of the visceral peritoneum is a distinctive feature of uterine scar dehiscence.
In our professional activity, it was not uncommon and it is still actual that during repeated cesarean section we find protrusion formation in the area of the scar covered by peritoneum, muscle tissue is absent or visible along the edges. The visceral peritoneum is intact. In our practice, for such conditions, we first used the term "hernia", which did not correspond to the essence of the case, and then we have chosen another term – "aneurysm" by analogy with locally mediated vasodilation.
There is reason to believe, that some obstetricians in our country classify incomplete URs as uterine scar dehiscence in their medical reports.
Due to the fact that the issue of differential diagnosis between incomplete UR and uterine scar dehiscence/aneurysm after cesarean section is insufficiently covered in the domestic literature, the aim of this article is defined as follows: in conformity with recommendations of the Ministry of Health of the Russian Federation to provide scientific rationale for separation of the notions “incomplete uterine rupture after surgery” and “uterine scar dehiscence/aneurysm during pregnancy and childbirth”.
Materials and methods
A retrospective analysis of 112 birth histories with uterine rupture along the scar after cesarean section was carried. In all women under study, UR was confirmed during repeated cesarean section or abdominal incision in the early postpartum period. The births took place in maternity hospitals of Moscow Department of Healthcare, clinical hospital MD Group in the period from 1999 to 2018.
43 birth histories of patients with uterine scar dehiscence/aneurysm after cesarean section, who gave birth in Center for Family Planning and Reproduction and in clinical hospital MD Group, were studied. Inclusion criterion was confirmation of the presence of aneurysm with the intact visceral peritoneum in repeated cesarean section. Exclusion criteria were: placenta accreta and placenta previa to the wall of the aneurysm without accretion. One patient had scar dehiscence after myomectomy, and her case was described separately.
 Results and discussion
Results and discussion
As it follows from the data below (Fig.1), out of 112 patients, UR was found before delivery in 62 women (24 of them had complete UR, and 38 – incomplete UR), due to this they underwent repeated cesarean section. Spontaneous vaginal delivery was in 50 women. Complete UR (blood in the peritoneal cavity) in the early postpartum period was in 4 women, and incomplete UR (blood under the vesicouterine peritoneal fold) was in 46 women. The total number of imcomplete URs was 84.
These data indicate an untimely diagnosis of UR, both in those operated before delivery and in those who had a rupture only after delivery (the selected method can hardly be considered correct).
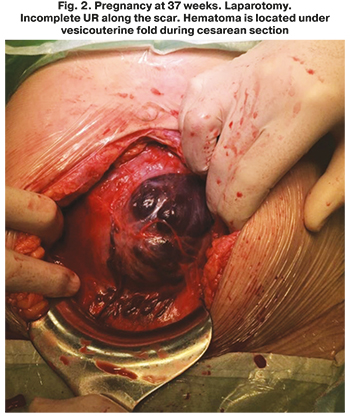 Fig. 2 shows incomplete uterine rupture, when the fetus is in the womb. It is characterized by overstretched vesicouterine fold and hematoma of significant size, which is clearly seen.
Fig. 2 shows incomplete uterine rupture, when the fetus is in the womb. It is characterized by overstretched vesicouterine fold and hematoma of significant size, which is clearly seen.
The analysis of birth histories showed that the symptoms of UR along the scar during pregnancy and delivery were in 53 women out of 62: nausea, vomiting, epigastric pain with subsequent localization in the area of the scar, pain in the lower right abdomen. It should be noted that similar symptoms, when pain is localized in the lower abdomen often mimics acute appendicitis. Despite the symptoms of UR, labor contractions did not stop. 48 out of 62 patients subsequently had a combination of initial symptoms of UR: uterine hypertonus and fetal bradycardia; 13 women had bloody vaginal discharge; 6 women had discoordinated and week labor.
There were no records of the presence of signs and symptoms of UR in birth histories of 5 women, as well as there were no records of their absence. The latter may indicate that some doctors lack the knowledge of small but very important UR manifestations, and their absence or presence should be obligatory mentioned in the records of birth histories.
The condition of babies born to 38 mothers with incomplete rupture of the uterus, who underwent uterine surgery during pregnancy and childbirth was as follows: 4 babies were stillborn, 3 were born with severe asphyxia, 6 – with moderate asphyxia, 14 – with mild asphyxia, and 11 babies had a satisfactory condition. The amount of blood loss was 600–1000 ml in 17 women, 1001–2000 ml in 14 women and 2001–4000 ml was in 7 women.
Small hematomas and the scar defects of 2–4 cm length were observed in 11 patients with incomplete UR. But, despite a small size of the scar defect, out of 11 newborns, two babies were born with moderate asphyxia, and one baby was born with severe asphyxia. Therefore, perinatal outcomes are defined not by the length of the scar defect, but by the reaction of the uterus to the stretching of the scar by a hematoma, resulting in hypertonic uterine. [1].The amount of blood loss associated with UR was defined not only by impaired integrity of the vascular wall, but possibly by detachment of the normally situated placenta, as well as by uterine hypotonia.
 As was mentioned above, in 46 women out of 50, who had spontaneous delivery, incomplete UR was detected in the early postpartum period. In order not to miss a possible UR after spontaneous childbirth, Previously, manual examination of the postpartum uterus was required not to overlook UR after spontaneous delivery, and even then UR was not always detected. According to our data, in all 49 parturient women, who underwent manual examination of the uterys, UR was not overlooked. Currently, (in compliance with recommendations of the Ministry of Health of Russia) ultrasound is a method of choice for evaluating and monitoring of patients with uterine rupture after vaginal delivery on a 24 hour per day basis (especially during the first hours). Regardless of ultrasound evaluation and manual uterine examination, emergency laparotomy is indicated for all women with uterine scar, who gave birth by vaginal delivery, and whose general condition worsened, and the symptoms of intra-abdominal bleeding (skin pallor, hypotension, tachycardia) appeared.
As was mentioned above, in 46 women out of 50, who had spontaneous delivery, incomplete UR was detected in the early postpartum period. In order not to miss a possible UR after spontaneous childbirth, Previously, manual examination of the postpartum uterus was required not to overlook UR after spontaneous delivery, and even then UR was not always detected. According to our data, in all 49 parturient women, who underwent manual examination of the uterys, UR was not overlooked. Currently, (in compliance with recommendations of the Ministry of Health of Russia) ultrasound is a method of choice for evaluating and monitoring of patients with uterine rupture after vaginal delivery on a 24 hour per day basis (especially during the first hours). Regardless of ultrasound evaluation and manual uterine examination, emergency laparotomy is indicated for all women with uterine scar, who gave birth by vaginal delivery, and whose general condition worsened, and the symptoms of intra-abdominal bleeding (skin pallor, hypotension, tachycardia) appeared.
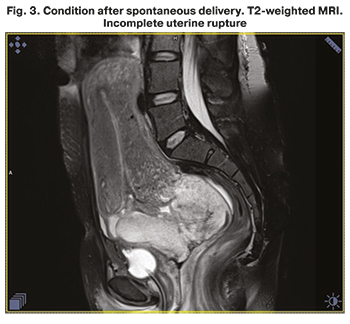
Among all women in the study, only 1 patient underwent ultrasound examination in the early postpartum period, which did not show uterine rupture, and manual vaginal examination was not carried out. Based on the worsening of the parturient woman’s condition, 3 hours after delivery repeated ultrasound revealed the risk of uterine rupture. Magnetic resonance imaging (MRI) confirmed the uterine wall defect (Fig. 3).
In 9 patients, there were no signs of UR in birth histories. To be sure that the symptoms and signs were not actually present, the doctor should include this information in medical records of birth history and list them all. We are deeply convinced that in some conditions in obstetrics, such as premature separation of the normally situated placenta, risk of uterine rupture or the onset of UR, preeclampsia, after careful questioning the patient, it should be registered in medical records that characteristic symptoms are not present.
 The analysis of all birth histories with incomplete UR along the scar after delivery showed that there were no reasons to believe that the diagnosis of uterine scar dehiscence should be established. One baby was born in the state of clinical death and died, 4 babies were born with mild asphyxia (Apgar score of 6), 8 babies had Apgar score of 7. Satisfactory condition of 33 babies at birth indicated the occurrence of UR at the end the second stage of labor, but agonal state and asphyxia indicated overlooked symptoms of UR. Blood loss in patients of this subgroup makes it impossible to attribute the defects found in uterine integrity to scar dehiscence. In 21 patients, blood loss ranged from 501 to 1000 ml, in 8 patients blood loss was more than 1001 ml. The maximum blood loss was 2500 ml.
The analysis of all birth histories with incomplete UR along the scar after delivery showed that there were no reasons to believe that the diagnosis of uterine scar dehiscence should be established. One baby was born in the state of clinical death and died, 4 babies were born with mild asphyxia (Apgar score of 6), 8 babies had Apgar score of 7. Satisfactory condition of 33 babies at birth indicated the occurrence of UR at the end the second stage of labor, but agonal state and asphyxia indicated overlooked symptoms of UR. Blood loss in patients of this subgroup makes it impossible to attribute the defects found in uterine integrity to scar dehiscence. In 21 patients, blood loss ranged from 501 to 1000 ml, in 8 patients blood loss was more than 1001 ml. The maximum blood loss was 2500 ml.
The data on the condition of newborns and the increased blood loss cannot be attributed to “uterine dehiscence”.
Diagnosis of incomplete UR, as well as all other uterine ruptures can not be an indication for hysterectomy. Most commonly, after opening the peritoneum, hematoma is removed, and if necessary, the wound edges are excised, then the uterine wound is sutured.
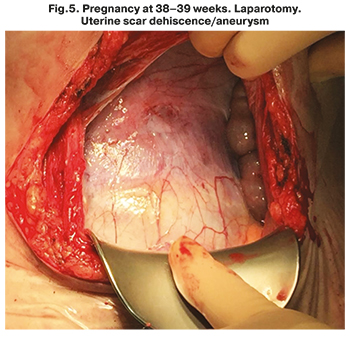 Uterine scar dehiscence/aneurysm has a characteristic picture shown in Figures 4 and 5: scar dehiscence is seen as a translucent bulging into the gestational sac. We have analyzed medical histories of 43 patients with uterine scar dehiscence after lower segment cesarean section. Aneurysm was formed after one cesarean section in 24 women, after 2 CS – in 15, after 3 CS – in 3 and after 4 CS – in 1 woman. Consequently, even after one cesarean section, an inconsistent uterine scar may occur, which manifests itself during repeated pregnancy.
Uterine scar dehiscence/aneurysm has a characteristic picture shown in Figures 4 and 5: scar dehiscence is seen as a translucent bulging into the gestational sac. We have analyzed medical histories of 43 patients with uterine scar dehiscence after lower segment cesarean section. Aneurysm was formed after one cesarean section in 24 women, after 2 CS – in 15, after 3 CS – in 3 and after 4 CS – in 1 woman. Consequently, even after one cesarean section, an inconsistent uterine scar may occur, which manifests itself during repeated pregnancy.
Unlike the foreign researchers [4, 6–10], who found uterine scar dehiscence during cesarean section, in our study we have shown that dehiscence/aneurysm may be formed much earlier. The ground for prenatal diagnosis is an echographic imaging of lower uterine segment thickness < 1 mm in the area of the suspected scar.
Detection of aneurysm at the earlier terms was due to recommendations of the Ministry of Health of Russia on management of normal pregnancy. It was stipulated, that ultrasound should be performed at 11–14, 19–21 weeks of pregnancy [11]. In clinical hospital MD Group the established terms for ultrasound are 11–12 weeks, 16–17 weeks, 20–21 weeks.
The below table shows the weeks of pregnancy at which the scar dehiscence after cesarean section was found.
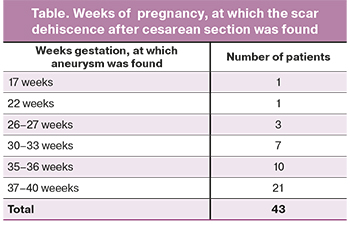 The table shows that scar dehiscence may occur early – at 17 weeks gestation.
The table shows that scar dehiscence may occur early – at 17 weeks gestation.
It should be assumed that identification of aneurysm and initiation of its formation are ambiguous concepts. It is possible that the aneurysm is formed even earlier. Pregnancy in 37 of 43 patients was prolonged to full-term or near-term. None of the patients experienced pain. One patient categorically refused to undergo surgery, and the caesarean section was performed at 40–41 weeks. Figures 4 and 5 show typical examples of uterine scar dehiscence/aneurysm.
Two figures of uterus during pregnancy at 38 weeks gestation demonstrate a possibility to carry pregnancy full term.
Five patients underwent surgery at 35–36 weeks, taking into account the onset of labor.
All babies were born in satisfactory condition. Birth weights were consistent with the gestational age. Blood loos among all patients was not greater than 700 ml.
 Uterine scar dehiscence during pregnancy may occur not only after cesarean section, but also after myomectomy (Fig.6). We followed up a patient with myomectomy in medical history. She underwent laparoscopic myomectomy. She had no complaints during pregnancy. She drove herself to maternity hospital having full-term pregnancy. Ultrasound scan gave the impression of changes in uterine contour, due to this elective caesarean section was performed. There was no blood in the abdominal cavity, but on the posterior and lateral surfaces of the uterus a round-shaped defect of 11x11 cm without damage to the peritoneum was found. Cesarean section was performed in the lower segment. The fetus was removed from the uterus in satisfactory condition, the placenta was removed.
Uterine scar dehiscence during pregnancy may occur not only after cesarean section, but also after myomectomy (Fig.6). We followed up a patient with myomectomy in medical history. She underwent laparoscopic myomectomy. She had no complaints during pregnancy. She drove herself to maternity hospital having full-term pregnancy. Ultrasound scan gave the impression of changes in uterine contour, due to this elective caesarean section was performed. There was no blood in the abdominal cavity, but on the posterior and lateral surfaces of the uterus a round-shaped defect of 11x11 cm without damage to the peritoneum was found. Cesarean section was performed in the lower segment. The fetus was removed from the uterus in satisfactory condition, the placenta was removed.
In this article, we do not dwell on the volume of surgery for UR. According to our point of view, which is supported by the majority of obstetricians in Moscow, organ-sparing surgery reduces overall blood loss and thereby preserves woman’s life and health. It is important, that in maternity hospitals (it is better to hospitalize women to level 3 hospitals), Cell Salvage (Cell-Saver) and additional methods of hemostasis (uterine compression sutures, pelvic surgery on the major arteries of the pelvis, uterine artery embolization) should be used.
Histological examination of the tissue excised during cesarean section (in 25 patients), made it possible to describe the structure of aneurysm, which is composed of the outer layer – a serous membrane, the islets of muscle tissue and stretched fibers of connective tissue, and fetal membranes adjacent to it. In 10 patients who underwent surgery at 37–38 weeks, and in 2 who underwent surgery 36 weeks of pregnancy, small hemorrhages were found in the thickness of the scar.
Conclusion
Non-penetrating UR, both in the second half of pregnancy and during delivery, and uterine scar dehiscence are not the same concept, each of them is determined by specific morphological structure and clinical picture.
Non-penetrating URs along the scar are accompanied by hematomas of different size and defect length, and commonly, by certain clinical symptoms: epigastric pain, nausea, vomiting, unrelaxed uterine tone. During delivery, the precursors of UR may be impaired uterus contractions (weakness, discoordination). Bloody vaginal discharge, fetal bradycardia may occur. The listed symptoms combine the stages of risk and the onset of UR and should be an indication for repeated cesarean section.
Uterine scar dehiscence (aneurysm) is characterized by: a) asymptomatic course; b) carrying pregnancy to term; c) detection during elective cesarean section most often; d) preservation of the visceral peritoneum; e) the fetus does not experience pain; f) the total blood loss does not exceed the average volume.
The notion “uterine scar dehiscence/aneurysm” should be distinguished from “incomplete uterine rupture”, since the concept of commonality of these notions will justify the doctors and contribute to their incompetence. The doctors should know both the initial symptoms of the risk and onset of uterine rupture.
References
- Савельева Г.М., Курцер М.А., Бреслав И.Ю., Коноплянников А.Г., Латышкевич О.А. Разрывы матки в современном акушерстве. Акушерство и гинекология. 2020, 9: 48-55. [Savelyeva G.M., Kurtser M.A., Breslav I.Yu., Konoplyannikov A.G., Latyshkevich O.A. Uterine rupture in modern obstetrics. Obstetrics and gynecology. 2020; 9: 48-55. (in Russian)]. https://dx.doi.org/10.18565/aig.2020.9.48-55. ]
- Бреслав И.Ю. Кровотечения при поздних сроках беременности и во время родов. Возможности органосохраняющих операций. Акушерство и гинекология. 2016; 10: 52-8. [Breslav I.Yu. Bleeding during late pregnancy and during childbirth. Possibilities of organ-preserving operations. Obstetrics and gynecology. 2016; 10: 52-8. (in Russian)]. https://dx.doi.org/10.18565/aig.2016.10.52-8.
- Fox N.S., Gerber R.S., Mourad M., Salzman D.H., Klauser C.K., Gupta S., Rebarber A. Pregnancy outcomes in patients with prior uterine rupture or dehiscence. Obstet. Gynecol. 2014; 123(4): 785-9. https://dx.doi.org/10.1097/AOG.0000000000000181.
- Fox N.S. Pregnancy outcomes in patients with prior uterine rupture or dehiscence: A 5-Year Update. Obstet. Gynecol. 2020; 135(1): 211-2. https://dx.doi.org/10.1097/AOG.0000000000003622.
- Levine E.M. Uterine rupture vs dehiscence. Am. J. Obstet. Gynecol. 2016; 214(3): 415. https://dx.doi.org/10.1016/j.ajog.2015.11.025.
- Di Spiezio Sardo A., Saccone G., McCurdy R., Bujold E., Bifulco G., Berghella V. Risk of Cesarean scar defect following single- vs double-layer uterine closure: systematic review and meta-analysis of randomized controlled trials. Ultrasound Obstet. Gynecol. 2017; 50(5): 578-83. 50(5):557-558. https://dx.doi.org/10.1002/uog.18911.
- Bashiri A., Burstein E., Rosen S., Smolin A., Sheiner E., Mazor M. Clinical significance of uterine scar dehiscence in women with previous cesarean delivery prevalence and independent risk factors. J. Reprod. Med. 2008; 53(1): 8-14.
- Abdelazim I.A., Shikanova S., Kanshaiym S., Karimova B., Sarsembayev M., Starchenko T. Cesarean section scar dehiscence during pregnancy: Case reports. J. Family Med. Prim. Care. 2018; 7(6): 1561-5. https://dx.doi.org/10.4103/jfmpc.jfmpc_361_18.
- Sawada M., Matsuzaki S., Nakae R., Iwamiya T., Kakiga-no A., Kumasawa K. et al. Treatment and repair of uterine scar dehiscence during cesarean section. Clin. Case Rep. 2017; 5(2): 145-9. https://dx.doi.org/10.1002/ccr3.766.
- Greenwald S.R., Gonzalez J.M., Goldstein R.G., Rosenstein M.G. Asymptomatic uterine dehiscence in a second-trimester twin pregnancy. Am. J. Obstet. Gynecol. 2015; 213(4): 590.e1-2. https://dx.doi.org/10.1016/j.ajog.2015.06.017.
- Приказ Министерства здравоохранения РФ от 20 октября 2020 г. №1130н «Об утверждении Порядка оказания медицинской помощи по профилю «акушерство и гинекология»». [Order of the Ministry of Health of the Russian Federation dated October 20, 2020 No. 1130n "On Approval of the Procedure for Providing Medical Care in the Profile "Obstetrics and Gynecology"" (in Russian)].
Received 05.05.2021
Accepted 19.05.2021
About the Authors
Galina M. Savelyeva, Dr. Med. Sci., Academician of the RAS, Professor, Professor of the Department of Obstetrics and Gynecology, Pediatric Faculty, N.I. PirogovRussian National Research Medical University, Ministry of Health of Russia. Tel.: +7(495)718-34-72. E-mail: gms@cfp.ru. ORCID: 0000-0001-8735-1281.
117997, Russia, Moscow, Ostrovitianov str., 1.
Mark A. Kurtser, Dr. Med. Sci., Academician of the RAS, Professor, Head of the Department of Obstetrics and Gynecology, Pediatric Faculty, N.I. Pirogov Russian National Research Medical University, Ministry of Health of Russia. Tel.: +7(495)719-78-96. E-mail: m.kurtser@mcclinics.ru. ORCID: 0000-0003-0175-1968.
117997, Russia, Moscow, Ostrovitianov str., 1.
Irina Yu. Breslav, Dr. Med. Sci., Head of the Department of Pathology of Pregnancy, Hospital MD GROUP. Tel.: +7(495)331-44-85. E-mail: irina_breslav@mail.ru.
ORCID: 0000-0002-0245-4968. 111720, Russia, Moscow, Sevastopol Ave., 24/1.
Elena Ya. Karaganova, PhD, Associate Professor of the Department of Obstetrics and Gynecology, Pediatric Faculty, N.I. Pirogov Russian National Research Medical University, Ministry of Health of Russia. Tel.: +7(916)684-95-05. E-mail: karaganova22@gmail.com. ORCID: 0000-0002-3199-4867.
117997, Russia, Moscow, Ostrovitianov str., 1.
Julia G. Neklyudova, resident doctor of the Department of Obstetrics and Gynecology, Pediatric Faculty, N.I. Pirogov Russian National Research Medical University,
Ministry of Health of Russia. Tel.: +7(903)014-40-91. E-mail: yunek95@mail.ru. ORCID: 0000-0001-5353-9569. 117997, Russia, Moscow, Ostrovitianov str., 1.
For citation: Savelyeva G.M., Kurtser M.A., Breslav I,Yu., Karaganova E.Ya., Neklyudova Yu.G. Non-penetrating uterine rupture along the scar after cesarean section and dehiscence/aneurysm of the uterine scar in the second half of pregnancy and during childbirth.
Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2021; 6: 66-72 (in Russian)
https://dx.doi.org/10.18565/aig.2021.6.66-72



