Prediction of and a risk group for delayed labor
Objective. To assess the features of somatic, obstetric and gynecologic histories and the course of pregnancy in order to determine factors and to identify a risk group for delayed labor.Tysyachnyi O.V., Baev O.R., Chausov A.A., Krechetova L.V., Chernukha E.A.
Subjects and methods. The study included 957 healthy primiparas and secundiparas and their newborns. The data of family, somatic and obstetric/gynecologic histories were analyzed to clarify differences in the course of pregnancy and childbirth during timely and delayed childbirth.
Results. Post-term pregnancy was found to be more common in some types of extragenital pathology, such as diseases of ENT (p = 0.01), urinary system (p = 0.01), and visual organs (p = 0.01), and a male fetus (p = 0.0001). The significant risk factors of post-term pregnancy included the birth of a pregnant woman herself (OR = 4.6; 2.5-8.3; p < 0.0001) or that of the father of the child (OR = 3.8; 1.7–8.1; p = 0.0005) due to delayed labor, a history of post-term pregnancy (OR = 2.2; 1.2–4.1; p = 0.01), and birth canal unreadiness for childbirth in primiparas at 284 days or more (p < 0.0001) and in secundiparas at 283 days or more (p < 0.0001). Taking into account the gender of a fetus and medical history data, a prognostic model was created using the binary logistic regression method.
Conclusion. The most significant risk factors for post-term pregnancy are diseases of ENT, urinary system, and visual organs, a male fetus, birth of parents from delayed labor, a history of post-term pregnancy, birth canal unreadiness for childbirth in primiparas at 284 days or more and in secundiparas at 283 days or more.
Keywords
Postterm pregnancy is a pressing problem of modern obstetrics due to the fact that it is associated with increased risk of obstetric complications and adverse neonatal outcomes [1]. The primary research goal is finding etiological and risk factors of postterm pregnancy in order to reduce the whole range of complications.
There is an array of well-known risk factors for postterm pregnancy in modern specialized literature [2, 3], but in most cases the etiology of postterm labour is unclear. It leads to myriad difficulties in developing preventive measures.
Therefore, studying risk factors seems to be essential to define patients who are at risk of this complication, and to develop management of postterm pregnancy and labor.
The aim of this study is to assess patients’ histories and pregnancy complications for determining the risk factors and groups of women who are at risk of postterm labor.
Materials and Methods
The study included 957 healthy nulliparous and multiparous patients and their newborns. Inclusion criteria were maternal age 18–40 years, spontaneous singleton pregnancy, spontaneous onset of labour, gestational age 38–42 weeks and more, written informed consent of patients. Exclusion criteria were extragenital pathology, pregnancy after in vitro fertilization, congenital uterine abnormalities, fetal abnormalities.
The data of family and medical histories were analysed to define differences in the pregnancy complications and delivery process in patients with term and postterm pregnancies.
They were divided into two groups: the first (control) group included 751 women with term pregnancy; the second (comparison) group included 206 women with postterm pregnancy.
Gestational age was estimated using the first day of the last menstrual period and data from ultrasound scans according to Guidelines for the Management of Council of the Society of Obstetricians and Gynaecologists of Canada (2017) [4]. The main factor for date of birth calculation was ultrasound measurements performed between 11 and 14 weeks. In the absence of this data we used ultrasound finding at 7–8 weeks gestation or not later than 24 weeks.
The cervix in pregnancy was assessed using Bishop score (Modified Bishop scale) [5]. Postterm pregnancy was confirmed after delivery of a baby with at least two signs of postmaturity syndrome (Ballantyne–Runge Syndrome) [6].
Statistical analysis was performed using «MedCalc Statistical», «IBM SPSS Statistics 22 for Windows». Mean value (M), standard deviation (δ), and 95% confidence interval (CI) were determined for each quantitative parameter. Frequency(%) was determined for qualitative data. Mann–Whitney U test was used to compare continuous variables with a non-normal distribution. χ2 test was used for categorical variables. Statistical significance was defined as p<0.05. The association of different independent variables on the development of one characteristic was evaluated by multivariable logistic regression analysis. Usage of this method allowed to predict the probability of occurrence of the event and was calculated by the formula:
Р = 1/(1+e-z)
Р – the probability of occurrence of the event,
e – the base of the natural logarithm is equal to 2.718281828,
z – control of a linear regression.
RESULTS
First of all, there were no differences found between mean maternal age in both term and postterm labor groups (29.48 ± 3.61 and 31.23 ± 3.99 years, respectively; р = 0.8497).
 Furthermore, the mean maternal age of nulliparous women in the first group was 28.07 ± 3.02, and the same indicator in the second group amounted to 28.63 ± 2.83 years (р = 0.1288), in multiparous patients it was 32.32 ± 3.54 vs. 32.39 ± 3.71 years, respectively (р = 0.8726). More detailed analysis showed that multiparous women younger than 24 years were more prevalent in the postterm labor group (6.97% versus 1.61%, р = 0.04).
Furthermore, the mean maternal age of nulliparous women in the first group was 28.07 ± 3.02, and the same indicator in the second group amounted to 28.63 ± 2.83 years (р = 0.1288), in multiparous patients it was 32.32 ± 3.54 vs. 32.39 ± 3.71 years, respectively (р = 0.8726). More detailed analysis showed that multiparous women younger than 24 years were more prevalent in the postterm labor group (6.97% versus 1.61%, р = 0.04).
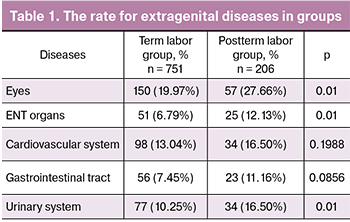
Considering medical history, extragenital diseases were more common in the postterm group with the rate of 83.98%, in comparison with 57.25% in the control group (OR=1.4; 95% CI 1.3–1.5; р < 0.0001 (Table 1). Moreover, no significant differences were found in cardiovascular and gastrointestinal diseases, however, the level of urinary, ENT and eyes disorders were significantly higher (р = 0.01).
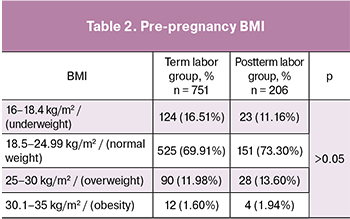 As for pre-pregnancy body mass index (BMI), mean BMI was approximately the same in both groups: 21.60 ± 2.54 kg/m2 versus 21.85 ± 2.42 kg/m2 (р = 0,3685). Table 2 shows characteristics of maternal pre-pregnancy body mass index. In nulliparous women pre-pregnancy BMI was 21.26 ± 3.70 kg/m2 and 21.48 ± 2.98 kg/m2 in term and postterm groups, respectively (р = 0.348), whereas multiparous women had BMI of 21,98 ± 2,82 kg/m2 versus 23,51 ± 3,78 kg/m2, р = 0,091.
As for pre-pregnancy body mass index (BMI), mean BMI was approximately the same in both groups: 21.60 ± 2.54 kg/m2 versus 21.85 ± 2.42 kg/m2 (р = 0,3685). Table 2 shows characteristics of maternal pre-pregnancy body mass index. In nulliparous women pre-pregnancy BMI was 21.26 ± 3.70 kg/m2 and 21.48 ± 2.98 kg/m2 in term and postterm groups, respectively (р = 0.348), whereas multiparous women had BMI of 21,98 ± 2,82 kg/m2 versus 23,51 ± 3,78 kg/m2, р = 0,091.
Moreover, mean weight gain in pregnancy was not significantly different between two groups in this study: 13.56 ± 3.39 kg versus 13.95 ± 3.58 kg (р = 0.5259), as well as there were no distinctions in maternal BMI at the onset of labor that is 26.22 ± 2.60 kg/m2 versus 26.90 ± 2.65 kg/m2 (р = 0.0658).
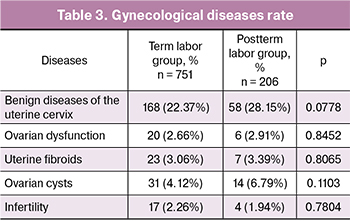 Studying gynecological history did not reveal any substantial differences between two those groups. For instance, the mean age of menarche was 13.15 ± 1.03 and 13.27 ± 1.11 years (р = 0.1616). Moreover, regular periods were more common for the second group (95.64% versus 93.75%), though these figures did not differ significantly (р = 0.3117). Table 3 shows characteristics of gynecological diseases.
Studying gynecological history did not reveal any substantial differences between two those groups. For instance, the mean age of menarche was 13.15 ± 1.03 and 13.27 ± 1.11 years (р = 0.1616). Moreover, regular periods were more common for the second group (95.64% versus 93.75%), though these figures did not differ significantly (р = 0.3117). Table 3 shows characteristics of gynecological diseases.
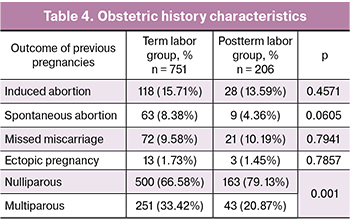
Table 4 shows more common features of obstetric history. For instance, multiparous women gave a birth at term significantly more often that is 251 (33.42%) versus 43 (20.87%), р = 0.001 (Table 4). In contrast, nulliparous patients had a considerably higher level of postterm delivery, in 163 women (79.13%) versus 500 women (66.58%). Furthermore, the analysis of clinical data showed that risk of postterm labor in nulliparous women was about 2 times higher (OR = 1.9; 95%CI 1.3–2.7; р = 0.0006).
 The assessment of previous pregnancies and labour outcomes illustrated that 29 women (3.86%) had postterm labor in the first presented group, whereas their number in the second group was just 17 (8.25%), р = 0.04. Our data showed that previous postterm labor significantly increased the risk of postterm labor in a consecutive pregnancy (OR = 2.2; 95%CI 1.2–4.1; р = 0.01). Taking into account maternal and paternal data analysis, 11.16% women were born postterm in the second group, while only 3.46% patients had the same history in the control group. Therefore, women who were born postterm had 4.6 times higher risk of postterm pregnancy and labor (OR = 4.6; 95%CI 2.5–8.3; р < 0.0001). On top of that, paternal impact on this problem seems to be clear due to the fact that 6.79% of children’s fathers were born postterm in the second group and just 1.86% in the control group. Thus, the risk of postterm labor was considerably higher if the child’s father had this parameter (OR = 3.8; 95% CI 1.7–8.1; р = 0.0005).
The assessment of previous pregnancies and labour outcomes illustrated that 29 women (3.86%) had postterm labor in the first presented group, whereas their number in the second group was just 17 (8.25%), р = 0.04. Our data showed that previous postterm labor significantly increased the risk of postterm labor in a consecutive pregnancy (OR = 2.2; 95%CI 1.2–4.1; р = 0.01). Taking into account maternal and paternal data analysis, 11.16% women were born postterm in the second group, while only 3.46% patients had the same history in the control group. Therefore, women who were born postterm had 4.6 times higher risk of postterm pregnancy and labor (OR = 4.6; 95%CI 2.5–8.3; р < 0.0001). On top of that, paternal impact on this problem seems to be clear due to the fact that 6.79% of children’s fathers were born postterm in the second group and just 1.86% in the control group. Thus, the risk of postterm labor was considerably higher if the child’s father had this parameter (OR = 3.8; 95% CI 1.7–8.1; р = 0.0005).
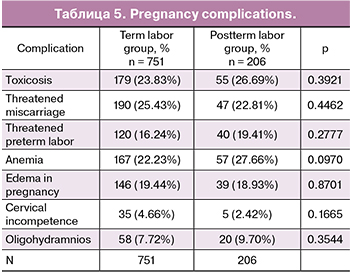 Pregnancy complications are presented in Table 5.
Pregnancy complications are presented in Table 5.
Regarding gestational age at the onset of labor, this parameter varied from 266 days (38 weeks) to 298 (42 weeks and 6 days) in the control group, while the postterm group had a range from 275 (39 weeks and 2 days) to 298 days (42 weeks and 6 days). Therefore, the former had a mean figure of 281.47 ± 5.29 days, whereas the latter had 287.88±2.40 (р < 0.0001). It is worth mentioning that three newborns with a gestational age less than 287 days at birth had signs of postmaturity syndrome.
It deserves a special attention that male newborns were predominant in the postterm group (60.20% versus 39.80%), and they were born postterm 1.5 times more often than female babies (RR = 1.5; 95%CI 1.2–1.8; р = 0.0001).
Using the multiple logistic regression with identified risk factors we calculated the probability of postterm pregnancy by formula:
Р = 1/(1+e-z)
z = 0.441 × the sex of newborn + women who were born postterm × 2.116 + men who were born postterm × 1.934 – 1.947
where: a male newborn was accepted as a number 0, female newborn – a number 1; women and men who were born at term as a number 0, if at postterm – number 1.
For this model, we made a ROC curve with sensitivity 42.0% and specificity 96.0% of postterm labor probability (Figure 1). AUC = 0.697 p = 0.0001.
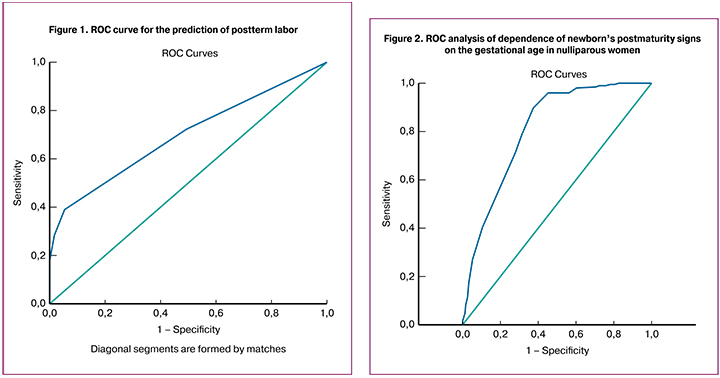
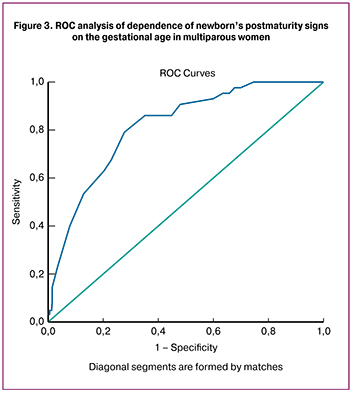
We performed ROC analysis in order to determine the gestational age at birth with a high chance of postmaturity syndrome for both nulliparous (Figure 2) and multiparous (Figure 3) women. As a result, we demonstrated that for nulliparous women with unripe cervix, gestational age was 284 days, sensitivity 89.8% and specificity 62.6%. AUC = 0.810, p < 0.0001, while for multiparous women it was 283 days with sensitivity 86.0% and specificity 64.9%, AUC = 0.817, p < 0.0001.
 Discussion
Discussion
To begin with, the results of the present study highlighted that ENT diseases, urinary and eye disorders were more common in women with postterm pregnancy. According to the existing data from up-to-date medical literature, the connection between maternal medical history and risk of postterm pregnancy has been mentioned only once. Nevertheless, E. A. Chernukha (2008) demonstrated that extragenital diseases play an important role in development of that pregnancy complication [2]. Moreover, J.D. Vucenovic (2007) showed that the risk factors for postterm pregnancy in multiparous women are diseases of the cardiovascular, urinary and digestive systems [7].
According to some literature, increased BMI or obesity can also be related to prolonged pregnancy [3, 8]. This effect could be explained by metabolic and hormone levels changes in obese patients [9, 10]. We have studied the association between BMI and postterm pregnancy. On contrary, our results did not demonstrate a link between such factors as pre-pregnancy BMI and gestational weight gain with an increased risk of postterm pregnancy. However, pre-pregnancy BMI in multiparous women was higher in the postterm group.
It is evident that nulliparous patients older than 30 years have postterm pregnancy more frequently [11]. Analyzing the age of women with postterm pregnancy, we revealed no age differences in nulliparous women. However, young multiparous patients (younger than 24 years) were prevalent in the postterm labor group (р = 0.04). We also found that risk of postterm pregnancy in nulliparous women were 1.6 times higher than in multiparous pregnant women (р = 0.001). The performed ROC analysis showed, that gestational age of 284 days in nulliparous patients with unripe cervix was a risk factor for the delivery of a baby with postmaturity syndrome (89.8% sensitivity, 62.6% specificity, AUC = 0.810, p < 0.0001). As for multiparous women, this variable was 283 days with 86% sensitivity and 64.9% specificity (AUC = 0.817, p < 0.0001).
It is worth noting that J.C. Kortekas et al. (2015) found the correlation between postterm labor in the first pregnancy and recurrent postterm pregnancy. In particular, the risk of this problem was 15 % higher [12]. Regarding our own results, previous postterm labor significantly increased the risk of postterm labour in a consecutive pregnancy 1.9 times more than in population (р = 0.04). Evaluating the role of hereditary factors, we found that women who were born postterm had 4.6 times higher risk of postterm pregnancy and labor (р < 0.0001), if men were born postterm, they had risk 3.8 times higher (р = 0.0005). These findings support a vital role of genetic factors in postterm pregnancy, such as cytokine gene polymorphism [13].
In assessing labor outcomes in terms of gender differences of babies, we found out that in the postterm group male newborns were predominant and they were born postterm 1.5 times more often than female babies (р = 0.0001). These results correspond to the existing data in literature, which showed that newborn males were born postterm significantly more often than females [14]. That phenomenon might be related to sulfatase deficiency. It is possible that there is a congenital, sex-specific, X-linked defect in that particular placental enzyme, playing a crucial role in the onset of labor. Placental suphatase deficiency was detected in cases of postterm birth of male newborns [15].
Using multiple logistic regression with identified risk factors we calculated the probability of postterm pregnancy by the formula:
Р = 1/(1+e-z),
where z = 0.441 × the sex of newborn + women who were born postterm × 2.116 + men who were born postterm × 1.934 – 1.947.
As a result, we demonstrated that in nulliparous women with unripe cervix, postterm pregnancy gestational age might be 284 days, sensitivity 89.8% and specificity 62.6%. AUC = 0.810, p < 0.0001, while inr multiparous women it might be 283 days with sensitivity 86.0% and specificity 64.9%, AUC = 0.817, p < 0.0001, if this result (Р) is equal to or greater than 50 %.
CONCLUSION
Overall, our study demonstrates that postterm pregnancy is associated with the particular extragenital diseases and male fetuses. There are significant risk factors, including previous postterm births of parents, unripe cervix at the gestational age ≥ 284 days in nulliparous women and ≥ 283 days in multiparous women.
In general, some extragenital diseases are more common in women with postterm pregnancies. However, these diseases are not specific for making risk factor group in postterm pregnancy. We were able to find a range of the significant risk factors: women who themselves were born possterm or had husbands from possterm deliveries, unripe cervix at the gestational age ≥ 284 days in nulliparous women and ≥ 283 days in multiparous women.
The duration of human pregnancy is affected by a variety of different factors, which are extremely important to study with the whole range of modern strategies and methods.
References
1. Wang M., Fontaine P. Common questions about late-term and postterm pregnancy. Am. Fam. Physician. 2014; 90(3): 160-5.
2. Чернуха Е.А. Переношенная и пролонгированная беременность. М.: ГЭОТАР-Медиа; 2007.
3. Ayyavoo A., Derraik J.G., Hofman P.L., Cutfield W.S. Postterm births: are prolonged pregnancies too long? J. Pediatr. 2014; 164(3): 647-51.
4. Delaney M., Roggensack A. No.214-Guidelines for the management of pregnancy at 41+0 to 42+0 weeks. J. Obstet. Gynaecol. Can. 2017; 39(8): e164-74.
5. Calder A., Alfirevic Z., Baxter J. et al. RCOG Clinical guideline. Induction of labour. – 2008. Jul; № 70: 81
6. Karkowski M. The Ballantyne-Runge syndrome. Pediatr. Pol. 1982; 57(1): 63-5.
7. Вученович Ю.Д., Князев С.А., Заякина Л.Б., Хубецова М.Т., Старцева Н.М. Переношенная беременность: влияние паритета. Вестник Российского университета дружбы народов. Серия: Медицина.2007; 5: 44-50.
8. Heslehurst N., Vieira R., Hayes L., Crowe L., Jones D., Robalino S. et al. Maternal body mass index and post-term birth: a systematic review and meta-analysis. Obes. Rev. 2017; 18(3): 293-308.
9. McNamara J.P., Huber K. Metabolic and endocrine role of adipose tissue during lactation. Annu. Rev. Anim. Biosci. 2018; 6: 177-95.
10. Stirrat L.I., O’Reilly J.R., Barr S.M., Andrew R., Riley S.C., Howie A.F. et al. Decreased maternal hypothalamic-pituitary-adrenal axis activity in very severely obese pregnancy: Associations with birthweight and gestation at delivery. Psychoneuroendocrinology. 2015; 63: 135-43.
11. Caughey A.B., Stotland N.E., Washington A.E., Escobar G.J. Who is at risk for prolonged and postterm pregnancy? Am. J. Obstet. Gynecol. 2009; 200(6): 683. e1-5.
12. Kortekaas J.C., Kazemier B.M., Ravelli A.C., de Boer K., van Dillen J., Mol B., de Miranda E. Recurrence rate and outcome of postterm pregnancy, a national cohort study. Eur. J. Obstet. Gynecol. Reprod. Biol. 2015; 193: 70-4.
13. Румянцева В.П., Стрижаков А.Н., Баев О.Р., Донников А.Е., Рыбин М.В., Сухих Г.Т. Полиморфизм генов цитокинов при своевременных родах и перенашивании беременности. Акушерство и гинекология. 2013; 6: 34-40.
14. Torricelli M., Voltolini C., Conti N., Bocchi C., Severi F.M., Petraglia F. Weight gain regardless of pre-pregnancy BMI and influence of fetal gender in response to labor induction in postdate pregnancy. J. Matern. Fetal Neonatal Med. 2013; 26(10): 1016-9.
15. Rabe T., Hösch R., Runnebaum B. Sulfatase deficiency in the human placenta: clinical findings. Biol. Res. Pregnancy Perinatol. 1983; 4(3): 95-102.
Received 20.03.2018
Accepted 20.04.2018
About the Authors
Tysyachnyi, Oleg V., junior scientific researcher of the first maternity departments Federal State Budget Institution «National medical research center of obstetrics,gynecology and Perinatology» of the Ministry of health of Russia. Phone 84954381188. e-mail olti23@mail.ru
Baev, Oleg R., MD, Phd, professor, the head of the first Maternity Department Federal State Budget Institution «National medical research center of obstetrics,
gynecology and Perinatology» of the Ministry of health of Russia. Phone 84954381188, e-mail o_baev@oparina4.ru
FGAOU VO “First Moscow state medical University. I. M. Sechenov” Ministry Of Health Of Russia (Sechenovskiy University). Department of obstetrics,
gynecology, perinatology and reproduction.
Chausov, Andrey A., junior scientific researcher of the Department of medical and social research Federal State Budget Institution «National medical research center
of obstetrics, gynecology and Perinatology» of the Ministry of health of Russia. Phone 84954386948. e-mail a_chausov@oparina4.ru
Krechetova, Lyubov V., Phd., the head of Laboratory of clinical immunology Federal State Budget Institution «National medical research center of obstetrics,
gynecology and Perinatology» of the Ministry of health of Russia. Phone 84954381183. e-mail l_krechetova@oparina4.ru
Chernukha, Evgeniy A., MD, Phd, professor, consultant of the first obstetric physiological Department Federal State Budget Institution «National medical research center
of obstetrics, gynecology and Perinatology» of the Ministry of health of Russia. Phone 84954381188, e-mail e_chernuha@oparina4.ru
For citations: Tysyachnyi O.V., Baev O.R., Chausov A.A., Krechetova L.V., Chernukha E.A. Prediction of and a risk group for delayed labor. Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2018; (11): 36-42. (in Russian)
https://dx.doi.org/10.18565/aig.2018.11.36-42