The risk of developing adhesions after female reproductive organ surgery
Aim. To identify risk factors for the development of pelvic adhesions in women of reproductive age.Dobrokhotova Yu.E., Sulima A.N., Puchkina G.A.
Material and methods. The study retrospectively analyzed 500 clinical records of randomly selected patients who underwent gynecologic pelvic surgery for various indications. Of them, 290 patients diagnosed with pelvic adhesions according to the R-AFS classification system were included in the main retrospective group. A retrospective comparison group was made up of 210 patients without pelvic adhesions. Continuous data were presented as median and the quartiles with differences between unpaired groups assessed by the Mann-Whitney U test. Qualitative variables were summarized as counts and percentages. The odds ratio (OR) and 95% confidence intervals (95% CI) to determine the risk factors for developing adhesions were calculated.
Results. The study identified risk factors for developing postoperative pelvic adhesions. It showed that already known risk factors predisposing to the formation of pelvic adhesions should be added with such factors as non-gynecologic comorbidities (diseases of the cardiovascular and endocrine system), endocrine disorders (estrogen deficiency and hypersecretion of thyroxine), intraoperative blood loss > 1000 ml, and the time from the last surgery > 12 months.
Conclusion. The study results showed that non-gynecologic comorbidities (diseases of the cardiovascular and endocrine system), endocrine disorders (estrogen deficiency and hypersecretion of thyroxine), intraoperative blood loss more than 1000 ml, and the time from the last surgery more than 12 months may be considered as risk factors for the formation of adhesions. These findings must be taken into account when developing preventive and therapeutic measures.
Keywords
The current literature provides available evidence suggesting that 90% of patients undergoing gynecologic pelvic surgery subsequently develop adhesions [1]. According to a SCAR study conducted by the Lower et al. in Scotland, infertility is associated with the adhesions following gynecological procedures, since 40% of pregnancy occurred after surgical adhesiolysis [2].
Despite the widespread use of laparoscopy in gynecology, as well as a significant number of adhesion barriers for abdominal surgery, the incidence of postoperative pelvic adhesions does not tend to decrease [3–7].
This study was aimed to identify risk factors for the development of pelvic adhesions in women of reproductive age.
Material and methods
This study retrospectively analyzed 500 clinical records of randomly selected patients who underwent gynecologic pelvic surgery for various indications between 2017 and 2018. Of them, 290 patients with established pelvic adhesions were included in the main retrospective group (MRG). The patients were enrolled in the MRG under the following inclusion criteria: 1) diagnosed with pelvic adhesions according to the R-AFS classification system; 3) a history of surgical intervention using traditional laparoscopic, fast-track laparoscopic and laparotomy techniques. A retrospective comparison group (RCG) was made up of 210 patients without pelvic adhesions. Source materials included a medical record of a hospitalized patient (form No. 003-у) and protocols of surgical operations (form No. 008 / у-07). A specially designed research card was used, containing 168 descriptors related to 5 thematic modules and covering: 1) general anamnestic information; 2) obstetric and gynecological history; 3) data of endocrine profile; 4) characteristics of previous surgical interventions; 5) information on prior treatments and adhesion prevention measures. Research card information was used to create the study dataset using Microsoft Excel 2018 for subsequent statistical analysis.
Statistical analysis
Continuous data are presented as median and the quartiles, with differences between unpaired groups assessed by the Mann-Whitney U-test. Qualitative variables are summarized as counts and percentages. The odds ratio (OR) and 95% confidence intervals (95% CI) to determine the risk factors for developing adhesions were calculated. The critical level of significance when testing statistical hypotheses were considered at p<0.05. Statistical analysis was performed using MATLAB version R2016b software (MathWorks).
Results
According to our data, the incidence of pelvic adhesions was 58.0%. There were several anamnestic risk factors for developing postoperative pelvic adhesions. MRG patients were statistically significantly more likely (OR=1.65; 95% CI 1.1–2.5) to use intrauterine contraceptives compared to RCG [90 (65.4%) and 45 (28.1%), respectively]. Also, 174 (60.0%) and 183 (87.1%) patients had a history of pregnancy, respectively. The groups did not differ significantly in the rates and structure of pregnancy and childbirth complications. At the same time, MRG patients were statistically significantly more likely to have a history of cesarean delivery [28 (32.6%) cases] (OR=3.10; 95% CI 1.3–7.2). Seventy-two (24.8%) and 56 (26.7%) patients in MRG and RCG groups had a history of induced abortion, respectively. However, the rate of repeat induced abortion (> 2) was statistically significantly higher among MRG patients [26 (36.1%)] (OR=2.49; 95% CI 1.1–5.6).
Among MRG patients, the rates of chlamydia [48 (27.2%)], chronic salpingo-oophoritis [112 (38.6%)], and extragenital endometriosis [63 (47.7%)] were statistically significantly higher than among RCG patients (OR=2, 25; 95% CI 1.3–4.0; OR=3.81; 95% CI 1.7–8.3 and OR=2.96; 95% CI 1.7–5.2, respectively). Infertility was diagnosed in 116 (39.9%) and 27 (12.9%) patients in MRG and RCG groups, respectively; MRG patients predominantly had secondary infertility (OR=2.76; 95% CI 1.4–5.2).
As for non-gynecologic comorbidities, MRG patients had a statistically significantly higher incidence of cardiovascular diseases [38 (33.3%)] (OR=3.37; 95% CI 1.6–7.1) and the endocrine disorders [40 (35.1%)] (OR=3.20; 95% CI 1.6–6.6).
Endogenous-exogenous risk factors for the development of pelvic adhesions are presented in Table 1.
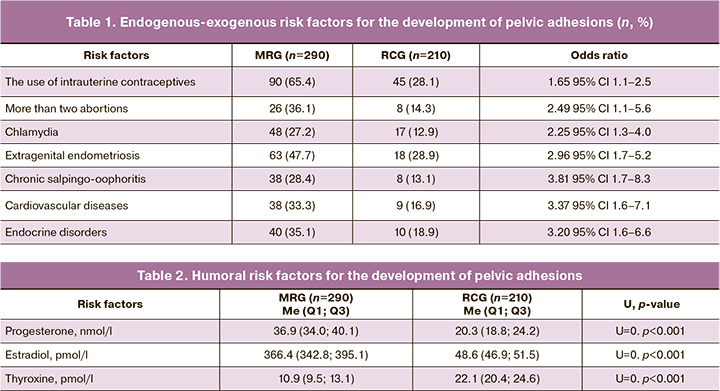
Compared with patients in RCG, MRG patients had significantly lower concentration of progesterone (to 20.3 nmol/L) and estradiol (to 48.6 pmol/L), but higher levels of thyroxine (to 22.1 pmol/L), (p <0.001; p <0.001; p <0.001) (Table 2).
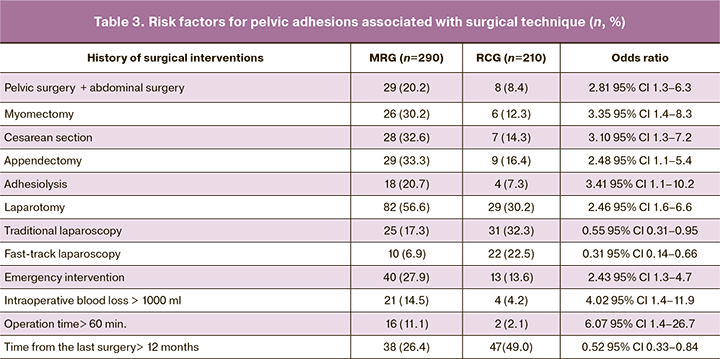
Compared with patients in RCG, MRG patients were statistically significantly more likely to have a history of combined abdominal and pelvic surgery (Table 3). They comprise 29 cases (20.2%) (OR=2.81; 95% CI 1.3–6.3), including adhesiolysis (OR=3.41; 95% CI 1.1–10.2), appendectomy (OR=2.48; 95% CI 1.1–5.4), myomectomy (OR=3.35; 95% CI 1.4–8.3), and cesarean section (OR=3.10; 95% CI 1.3–7.2). Also, MRG patients statistically significantly more often had a history of emergency surgery [40 cases (27.9%)] (p=0.012) (OR=2.43; 95% CI 1.3–4.7) and laparotomic surgery [82 cases (56.6%)] (p <0.001) (OR=2.46; 95% CI 1.6 –6.6). In MRG, there was a statistically significantly higher proportion of patients with blood loss > 1000 ml and operation time > 60 minutes [21 (14.5%) and 16 (11.1%) than in RCG (OR=4.02; 95% CI 1.4–11.9; OR=6.07; 95% CI 1.4–26.7, respectively). Patients in MRG had a more remote history (> 12 months) of surgical interventions in 38 (26.4%) cases (OR=0.52; 95% CI 0.33–0.84).
Discussion
Given the multifactorial etiology and the universal nature of adhesiogenesis, we analyzed a wide range of possible risk factors for developing adhesions, based on patients’ history.
Our findings showed that in addition to already known risk factors predisposing to the formation of pelvic adhesions [8–10], it is necessary to take into account such factors as estrogen deficiency, increased levels of thyroxine, endocrine and cardiovascular comorbidities, intraoperative blood loss > 1000 ml, and the time from the previous operation> 12 months. In a retrospective analysis, these risk factors were observed statistically significantly (p <0.05) more often in MRG than in RCG patients.
Estrogen deficiency indirectly reduces the secretion of vasoactive peptides and the intensity of local metabolic processes, increases in the resistance of arterial vessel walls, which leads to impaired microcir- culation in peritoneal and pelvic tissues thus promoting remodeling of the vascular bed in the focus of inflammation.
The role of hypersecretion of thyroxine can be explained by the fact that its increased level through binding to membrane and nuclear thyroid hormone sites can increase the expression of vascular endothelial growth factor (VEGF), fibroblast growth factor (bFGF), a hypoxia-induced factor -α (HIF-1α), which, in turn, leads to the activation of neo-angiogenesis and patho- logical cell proliferation. Besides, the hyper-production of thyroxine is manifested by a pronounced systemic pro-inflammatory and immunosuppressive effect due to a decrease in the number of antibody-forming cells, which changes the course of physiological inflammation towards a hyperergic reaction and promotes adhesiogenesis. This fact suggests that hypersecretion of thyroxine increases the risk of developing pelvic adhesions.
Considering the role of endocrine and cardiovascular comorbidities, it should be noted that regardless of the specific nosology, they are characterized by a universal mechanism of damage (oxidative stress, endothelial dysfunction, excessive production of pro-inflammato- ry cytokines and, as a consequence, local hyperergic inflammatory reaction). Given that angiogenic, inflam- matory stress is one of the critical elements in the for- mation of the adhesions, it reasonable to conclude that systemic ischemic reperfusion injuries in cardiovascular pathology and changes in intracellular signaling in the case of systemic endocrine dysfunction can contribute to pathological adhesionogenesis in pelvic organs and tissues.
The role of blood loss as a significant risk factor for developing adhesions may be explained by the adverse adhesiogenic effect when whole blood enters the abdominal cavity resulting in impaired regional hemodynamics in the postoperative period. Our results are consistent with the data from a series of experiments performed by K.K. Mailova et al. (2012), in which the adhesion process is proved to depend on the volume of injected blood and its components [11].
Regarding the role of operations lasting more than 60 minutes, it should be noted that this fact should be taken into account to understand the strategy for choos- ing the means of limiting the formation of the adhesions of the pelvic organs, which is consistent with the cur- rent research evidence, which suggests that a surgical technique or instrument that shortens operative time, minimizes the trauma of the peritoneum and, as a result, reduces the extent of adhesion formation [12].
The influence of time from previous surgical interven- tion on the formation of adhesions, in our opinion, is due to the chronic activation of the immune response associated with the cardiovascular and endocrine comor- bidities. The chronic inflammatory process in the body, inducing an imbalance of cytokine regulatory systems, contributes to microcirculatory dysfunctions, including in the peritoneal tissues, initiation of cascade reactions that form the basis of angiogenic-inflammatory stress, and further to the formation of a hyperergic pathological response and the development of adhesions. Our results emphasize the importance of the degree and severity of inflammatory reactions in the development of adhesions and contradict the data of previous studies, which show that the time from the last operation does not affect the formation of adhesions [13].
Conclusion
In our study, the incidence rate of pelvic adhesions in patients who had a history of gynecologic pelvic surgery for various indications was 58.0%. Of them, 36.9% were women of active reproductive age with tubal-peritoneal infertility.
The study results showed that non-gynecologic comorbidities (diseases of the cardiovascular and endocrine system), endocrine disorders (estrogen deficiency and hypersecretion of thyroxine), intraoperative blood loss more than 1000 ml and the time from the last surgery more than 12 months may be considered as risk factors for the formation of adhesions. These findings must be taken into account when developing preventive and therapeutic measures.
References
- Фетищева Л.Е., Мозес В.Г., Захаров И.С., Мозес К.Б. Эффективность противоспаечного барьера на основе карбоксиметилцеллюлозы 5 мг и натрия гиалуроната 2,5 мг при различных органосохраняющих методиках хирургического лечения внематочной трубной беременности. Гинекология. 2019; 21(2): 71-5. [Fetishcheva L.E., Moses V.G., Zakharov I.S., Moses K.B. The effectiveness of the anti-adhesion barrier based on carboxymethyl cellulose 5 mg and sodium hyaluronate 2.5 mg with various organ-preserving surgical procedures for ectopic tubal pregnancy. Gynecology. 2019 21 (2): 71-5. (in Russian)]. https://dx.doi.org/10.26442/20795696.2019.2.190360
- Diamond M.P., Wexner S.D., diZereg G.S., Korell M., Zmora O., Van Goor H., Kamar M. Adhesion prevention and reduction: current status and future recommendations of a multinationalinter – disciplinary consensus conference. Surg. Innov. 2012; 17(3): 183-8. https://dx.doi.org/10.1177/1553350610379869.
- Ахметзянов Ф.Ш., Егоров В.И., Анхимова Л.Е. Спаечный процесс как проблема абдоминальной оперативной онкологии. Сибирский онкологический журнал. 2018; 17(2): 95-103. [Akhmetzyanov F.S., Egorov V.I., Ankhimova L.E. Adhesions as a problem of abdominal surgical oncology. Siberian Oncology Journal. 2018; 17(2): 95-103. (in Russian)]. https://dx.doi.org/10.21294/1814-4861-2018-17-2-95-103.
- Quah G., Eslick M., Cox R. Laparoscopic versus open surgery for adhesional small bowel obstruction: a systematic review and meta-analysis of case-control studies. Surg. Endosc. 2019; 33(10): 3209-17. https://dx.doi.org/10.1007/s00464-018-6604-3.
- Беженарь В.Ф., Цыпурдеева А.А., Байлюк Е.Н. Спаечная болезнь органов малого таза у гинекологических больных: от патогенеза к практике. Онкогинекология. 2014; 4: 68-74. [Bezhenar V.F., Tsypurdeeva A.A., Bailuk E.N. Adhesive disease of the pelvic organs in gynecological patients: from pathogenesis to practice. Oncogynecology. 2014; 4: 68-74. (in Russian)].
- Луцевич О.Э., Галлямов Э.А., Попов С.В., Биктимиров Р.Г., Санжаров А.Е., Преснов К.С., Орлов И.Н., Кочкин А.Д., Сергеев В.П., Новиков А.Б., Биктимиров Т.Р., Галлямова С.В., Насырова Н.И., Аминова Л.Н., Павлова С.А., Михайликов Т.Г., Харчук А.В., Ерин С.А. Особенности лапароскопических операций в условиях спаечной болезни брюшины и возможности ее лапароскопического лечения и профилактики. Тихоокеанский медицинский журнал. 2017; 1: 69-73. [Lutsevich O.E., Gallyamov E.A., Popov S.V. Specifics of laparoscopic surgeries on peritoneal adhesions and possibilities of laparoscopic treatment and prevention. Pacific Medical Journal. 2017; 1: 69-73. (in Russian)].
- Самарцев В.А., Кузнецова М.В., Гаврилов В.А., Кузнецова М.П., Паршаков А.А. Противоспаечные барьеры в абдоминальной хирургии: современное состояние проблемы. Пермский медицинский журнал. 2017; 34(2): 87-93. [Samartsev V.A., Kuznetsova M.V., Gavrilov V.A., Kuznetsova M.P., Parshakov A.A. Anti-adhesion barriers in abdominal surgery: current problem status. Perm Medical Journal. 2017; 34 (2): 87-93. (in Russian)].
- Mais V. Peritoneal adhesions after laparascopic gastrointestinal surgery. World J. Gastroenterol. 2014; 20(17): 4917-25. https://dx.doi.org/10.3748/ wjg.v20.i17.4917.
- Суфияров И.Ф., Хасанов А.Г., Нуртдинов М.А., Самародов А.В., Ямалова Г.Р. Высокий уровень гликозаминогликанов сыворотки крови как независимый предиктор развития спаечной болезни брюшины. Креативная хирургия и онкология. 2017; 7(2): 48-53. [Sufiyarov I.F., Khasanov A.G., Nurtdinov M.A., Samarodov A.V., Yamalova G.R. High glycosaminoglycans in blood serum as an independent predictor of peritoneal adhesions development. Creative Surgery and Oncology. 2017; 7(2): 48-53. (in Russian)]. https://dx.doi.org/10.24060/2076-3093-2017-7-2-48-53.
- Калашников А.В., Дворецкая Ю.А. Спайки брюшной и плевральной полостей – общее и различия. Волгоградский научно-медицинский журнал. 2016; 53(1): 24-8. [Kalashnikov A.V., Dvoretskaya Yu.A. Abdominal and pleural adhesions – similarities and differences. Volgograd Medical Journal. 2016; 53(1): 24-8. (in Russian)].
- Маилова К.С., Осипова А.А., Corona R., Binda M.Ю., Koninckx F., Адамян Л.В. Влияние степени кровотечения на спайкообразование и методы профилактики образования послеоперационных спаек в лапароскопической модели на мышах. Проблемы репродукции. 2012; 18(2): 18-22. [Mailova K.S., Osipova A.A., Corona R. Binda M. Koninckx F., Adamyan L.V. Influence of the extent of hemorrhage on adhesions and methods to prevent post-surgery adhesions in a laparoscopic mouse model. Reproduction problems. 2012; 18(2): 18-22. (in Russian)].
- Луцевич О.Э., Акимов В.П., Ширинский В.Г., Бичев А.А. Спаечная болезнь брюшины: современный взгляд на патогенез и лечение. Хирургия. Журнал имени Н.И.Пирогова. 2017; 10: 100-8. [Lutsevich O.E., Akimov V.P., Shirinsky V.G., Bichev A.A. Peritoneal adhesions: a modern view of pathogenesis and treatment. Surgery. 2017; 10: 100-8. (in Russian)]. https://doi.org/10.17116/hirurgia201710100-108.
- Кондратович Л.М., Козаченко А.В., Коган Е.А., Файзуллина Н.М., Адамян Л.В. Клинико-морфологические особенности спаечного процесса у пациенток с миомой матки. Акушерство и гинекология. 2014; 8: 71-5. [Kondratovich L.M., Kozachenko A.V., Kogan E.A., Fayzullina N.M., Adamyan L.V. Clinical and morphological features of adhesions in patients with uterine myoma. Obstetrics and gynecology. 2014; 8: 71-5. (in Russian)].
Received 12.02.2020
Accepted 14.05.2020
About the Authors
Julia E. Dobrokhotova, MD, PhD, Professor, Head of the Department of Obstetrics and Gynecology, Faculty of Medicine, N.I. Pirogov Russian National Research Medical University, Moscow. E-mail: pr.dobrohotova@mail.ru. ORCID: 0000-0002-9091-4097. 117997, Russia, Moscow, Ostrovityanov str., 1.Anna N. Sulima, Dr.Med.Sci., Professor at the Department of Obstetrics, Gynecology and Perinatology № 1, S.I. Georgievsky Medical Academy of V.I. Vernadsky Crimean Federal University, Simferopol. E-mail: gsulima@yandex.ru. ORCID: 0000-0002-2671-6985. 295051, Russia, Republic of Crimea, Simferopol, Lenin bul., 5/7.
Galina A. Puchkina, Teaching Assistant at the Department of Obstetrics, Gynecology and Perinatology № 1, S.I. Georgievsky Medical Academy of V.I. Vernadsky Crimean Federal University, Simferopol. E-mail: puchkina.g.a@mail.ru. ORCID: 0000-0002-8882-8317.
295051, Russia, Republic of Crimea, Simferopol, Lenin bul., 5/7.
For citation: Dobrokhotova Yu.E., Sulima A.N., Puchkina G.A. The risk of developing adhesions after female reproductive organ surgery.
Akusherstvo i Ginekologiya/ Obstetrics and gynecology. 2020; 7: 105-110 (in Russian).
https://dx.doi.org/10.18565/aig.2020.7.105-110