Опухоли относятся к редкой патологии, диагностируемой у плода, и чаще всего они представлены крестцово-копчиковой тератомой. Как правило, диагностика опухолей у плода не вызывает затруднений, однако оценка прогноза для жизни и здоровья плода и новорожденного, рисков акушерских осложнений и, как следствие, выбор тактики ведения беременности и родоразрешения не всегда очевидны.
Мы представляем клиническое наблюдение опухоли шеи плода, выявленное в 32 недели гестации. Родоразрешение проведено с применением мультидисциплинарного подхода, позволившего провести восстановление дыхания новорожденного при продолжающемся плацентарном кровообращении за счет отсроченного клеммирования пуповины, – методики внематочного интранатального лечения (ex-utero intrapartum treatment (EXIT)).
Ультразвуковые исследования (УЗИ) выполнены на аппаратах VOLUSON 730 с использованием трансабдоминального конвексного датчика 5 МГЦ и трансвагинального датчика 7 МГЦ.
Магнитно-резонансная томография (МРТ) выполнена на аппарате Philips Ingenia 1.5T.
Клинический случай
Пациентка Р., 31 год, была направлена для консультации в Республиканский научно-практический центр (РНПЦ) «Мать и дитя» в связи с выявлением опухоли шеи у плода при плановом УЗИ в сроке гестации 32 недели. Беременность вторая. Первая завершилась родоразрешением путем кесарева сечения в сроке 39 недель в связи с вторичной слабостью родовых сил. Ребенок здоров. Вторая беременность наступила самопроизвольно во втором браке. Семейный анамнез не отягощен. Среди перенесенных заболеваний отмечается хронический холецистит. Течение второй беременности осложнилось угрожающим выкидышем с кровянистыми выделениями в сроке 11 недель. При проведении комбинированного скрининга беременных на выявление группы высокого риска по синдрому Дауна установлен риск 1:9 (высокий). Копчико-теменной размер – 39 мм, толщина воротникового пространства – 2,3 мм. В связи с высоким риском по синдрому Дауна проведено медико-генетическое консультирование и предложено выполнить инвазивную пренатальную диагностику. В 16 недель беременности был сделан диагностический амниоцентез и получен нормальный кариотип плода, 46,XY. В 22 недели гестации проведен плановый диагностический ультразвуковой осмотр, и патологических состояний не выявлено.
При контрольном осмотре в III триместре беременности по месту жительства установлено: срок гестации 32 недели, опухоль шеи плода, выраженное многоводие. Семья была направлена в РНПЦ «Мать и дитя».
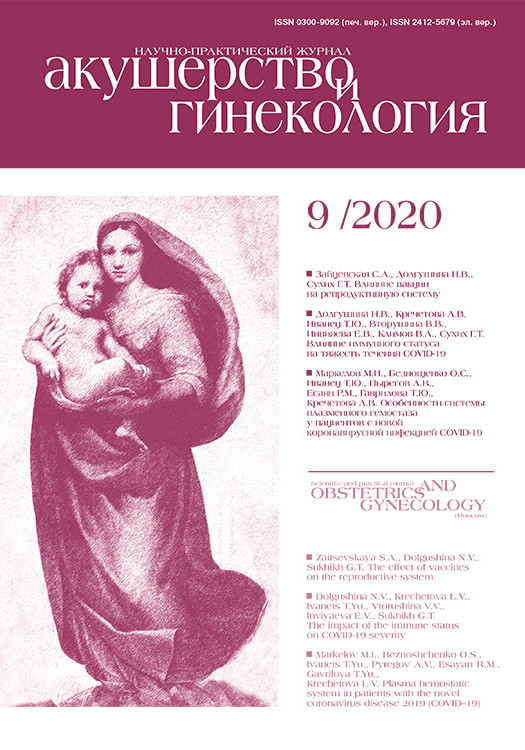
При осмотре в РНПЦ «Мать и дитя» срок беременности по первому дню последней менструации составил 32 недели, по фетометрии – 35 недель. В области шеи плода определялось округлое эхонеоднородное образование размерами 45×35×50 мм, без активного кровотока (рис. 1). В плевральной полости визуализировалась свободная жидкость, индекс амниотической жидкости 358, максимальный пакет вод – 120 мм. Стенки сердца утолщены, гиперэхогенные, определяется регургитация на трикуспидальном клапане II степени. Установлен диагноз: беременность 32 недели, тератома шеи плода, выраженное многоводие, вторичная кардиомиопатия. Проведен лечебный амниоцентез и удалено 3000 мл светлых амниотических вод.
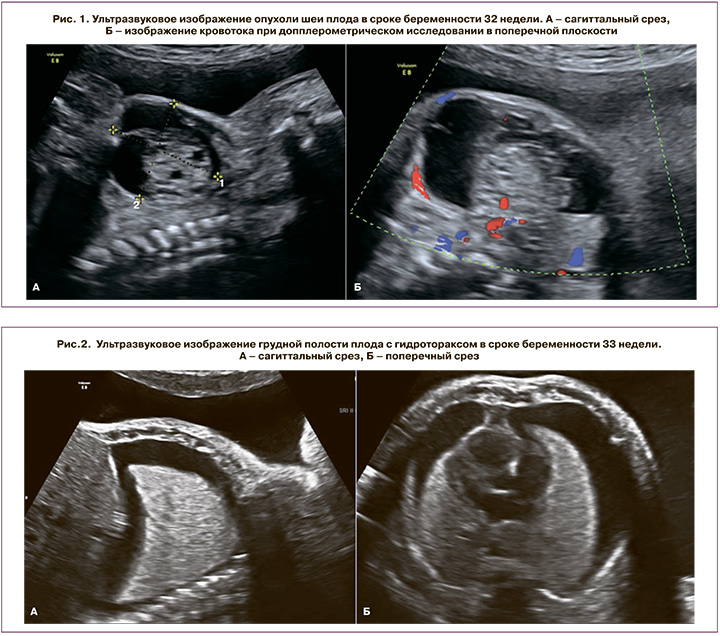
Повторное УЗИ выполнено через неделю. Диагноз тератомы шеи плода подтвержден. Гидроторакс (рис. 2). Многоводие. Четко определяется эхографическая тень желудка размерами 37×14×15 мм.
Проведено медико-генетическое консультирование, в ходе которого определены риски и прогноз для жизни и здоровья плода. Так, риск по множественным врожденным порокам составил 1–2% (низкий), риск обструкции верхних дыхательных путей за счет сдавления трахеи опухолью – 80% (высокий), риск по преждевременной отслойке нормально расположенной плаценты – 10–12% в связи с нарастающим многоводием из-за сдавления пищевода опухолью. В целом прогноз для жизни плода оценен как неблагоприятный (как правило, в связи с интранатальной гибелью), для здоровья – сомнительный. Рекомендовано пролонгировать беременность до доношенного срока с проведением динамического контроля за состоянием плода с использованием ультразвукового мониторинга и повторных лечебных амниоцентезов. В сроке беременности 34–36 недель рекомендовано выполнить МРТ для оценки состояния верхних дыхательных путей.
В 34 недели по первому дню последней менструации проведено контрольное УЗИ. По фетометрии срок беременности – 36 недель (макросомия). Размер опухоли шеи составил 52×39×54 мм, локализация ее – спереди, больше слева. Гидроторакс и многоводие – без положительной динамики. Эхографическая тень желудка не определялась. Проведен амниоцентез, удалено 3500 мл амниотических вод для ограничения подвижности плода при проведении МРТ.
При анализе результатов МРТ установлено, что просвет трахеи визуализируется не на всем протяжении, а прерывается за счет компрессии последней опухолью шеи (рис. 3). Таким образом, риск интранатальной гибели плода высок, и для обеспечения интубации новорожденного при родоразрешении необходимо провести EXIT с целью обеспечения реанимационных мероприятий, ларингоскопии, бронхоскопии или/и постановки трахеостомы при сохраненном кровоснабжении плода через неклеммированную пуповину в ходе кесарева сечения.

Родоразрешение проведено в 35–36 недель гестации. Операционная бригада включала, помимо акушеров-гинекологов, детских реаниматологов, детского отоларинголога, детского эндоскописта, неонатолога.
Состояние при рождении ребенка оценено как очень тяжелое и обусловлено врожденным пороком развития, дыхательной недостаточностью третьей степени. Кожные покровы – бледные, цианотичные. В области шеи определялось новообразование. При прямой ларингоскопии установлено смещение трахеи вправо. После рождения ребенка сразу выполненыэкстренная интубация трахеи и перевод ребенка на искусственную вентиляцию легких (дыхание проводилось симметрично по всем легочным полям). После интубации проведена бронхоскопия для оценки состояния дыхательных путей. Поставлен желудочный зонд, катетеризирована периферическая вена, начата интенсивная терапия. В 1-е сутки жизни выполнен торакоцентез слева и получено около 60 мл, справа – около 45 мл транссудата. Повторно проводился торакоцентез справа на 3-и (35 мл) и на 6-е сутки (80 мл). Слева на 2-е сутки выполнено дренирование плевральной полости.
В возрасте 9 дней ребенок был переведен в РНПЦ «Детской хирургии» МЗ Республики Беларусь, где ему была выполнена успешная операция по удалению опухоли. При гистологическом исследовании установлено: доброкачественная зрелая кистозная тератома, представленная соединительной тканью, многочисленными кистами, выстланными преимущественно муцинпродуцирующим, местами мерцательным эпителием, мелкими островками панкреатической и печеночной ткани, островками гемопоэза и участками зрелой и незрелой нейроглии (последняя составляет 5–7% от общей площади тератомы). Проводился анализ уровня альфа-фетопротеина (АФП) в динамике. На 5-е сутки он был 991 Ме/мл, в возрасте 2 месяцев – 4900 Ме/мл. Учитывая рост АФП, ребенок проконсультирован детскими онкологами в РНПЦ «Детской онкологии, гематологии и иммунологии» МЗ Республики Беларусь. При УЗИ шеи ребенка обнаружено изоэхогенное образование размерам 10×7×6 мм, расположенное между щитовидной железой и трахеей. Принято решение о проведении химиотерапии. При контрольном исследовании после 3 курсов химиотерапии уровень АФП оказался 780 Ме/мл, образование в области шеи при проведении УЗИ и компьютерной томографии не определялось. В возрасте 4 месяцев ребенок развивается с опережением, масса его 5600 г, косметических дефектов в области рубца нет (рис. 4).

Обсуждение
Опухоли плода встречаются в практике пренатального консультирования редко. Чаще всего они представлены доброкачественными образованиями, однако описаны и злокачественные опухоли плода, метастазирующие в другие органы плода и в плаценту. В доступной литературе мы не встретили информации об отдаленных метастазах у матери в связи со злокачественной опухолью плода. Наличие опухоли часто сопровождается таким осложнением беременности, как многоводие, как правило, многоводие резко выраженное и агрессивное, что, в свою очередь, может привести к преждевременной отслойке нормально расположенной плаценты. Поэтому особое значение приобретает медико-генетическое консультирование с оценкой не только прогнозов для жизни и здоровья плода, но и рисков акушерских осложнений и выбора тактики ведения беременности.
Опухоли в области шеи представлены тератомами, лимфангиомами, кистозными гигромами, опухолью щитовидной железы, гемангиомами, кистами протока щитовидной железы, кистами жаберной щели, нейробластомами шеи.
Для тератом шея является вторым по частоте регионом локализации. При УЗИ тератома описывается, как образование эхонеоднородной структуры, чаще расположенное на передней поверхности шеи. В состав опухоли может вовлекаться щитовидная железа, и рост опухоли может идти в сторону средостения. При МРТ за счет солидного и кистозного компонентов опухоли регистрируются сигналы различной интенсивности, что демонстрирует рисунок 3. Практически в половине случаев в составе тератомы есть кальцификаты, однако при проведении МРТ у плода внутриопухолевые кальцификаты определить сложно. Считается, что проведение МРТ в подобных ситуациях целесообразно для детальной характеристики опухолевого образования шеи, оценки смещения и компрессии органов дыхания и планирования мультидисциплинарного подхода при родоразрешении и оказании помощи новорожденному [1, 2].
Тератома шеи плода ассоциируется с многоводием, которое возникает за счет обструкции пищевода, что не позволяет плоду проглатывать околоплодные воды, и при УЗИ эхографическая тень желудка становится не видна, что и установлено нами при проведении контрольного УЗИ в 34 недели. Кроме того, тератома шеи может приводить к вычурному положению головки плода, сердечной недостаточности, водянке плода, а также смещению и/или компрессии гортани, трахеи, глотки.
Как правило, тератома шеи при выявлении обструкции дыхательных путей имеет плохой витальный прогноз. Снизить смертность новорожденных можно при применении EXIT – процедуры, позволяющей провести интубацию или трахеостомию новорожденному при продолжающем кровоснабжении последнего через нелигированную пуповину.
Первоначально EXIT была предложена при окклюзии трахеи у пациентов с диафрагмальной грыжей, а затем данная процедура стала использоваться и при других состояниях, сопровождающихся обструкцией дыхательных путей. Lazar D.A. et al. (2011) описали проведение EXIT у 12 беременных при выявлении компрессии трахеи опухолями шеи у плода. Во всех 12 случаях процедура прошла успешно, и в 10 случаях была выполнена интубация с жестким бронхоскопом, в 1 – ларингоскопия, и только в 1 понадобилось проведение трахеостомии [3]. Laje P. et al. (2015) показали опыт ведения и родоразрешения 112 беременных за период 1995–2013 гг. при выявлении опухолей шеи. EXIT применили у 13 (11%) пациенток. Критериями отбора для проведения EXIT были: девиация, компрессия, обструкция дыхательных путей и вовлечение ротовой полости в процесс. Многоводие было в 5 случаях, водянка плода – в 2. Родоразрешение провели в 37–38 недель у 8 (62%), у 5 – в сроке 33–36 недель. В том числе, авторы указали на необходимость проведения экстренной EXIT в 33 и 38 недель. В 12 из 13 случаев удалось провести EXIT: ларингоскопию (n=7), бронхоскопию (n=4), трахеостомию (n=1). В одном случае из-за большого размера опухоли провести трахеостомию не удалось. Из 12 пациентов, успешно прошедших EXIT, в 5 случаях в последующем пришлось выполнять трахеостомию [4]. В нашем клиническом случае мы также провели досрочное родоразрешение в 35 недель из-за нарастающего многоводия и гидроторакса. В целом, несмотря на то, что многие авторы отмечают успешное проведение процедуры EXIT, перинатальная смертность высока и составляет от 17% до 33% [5, 6].
При обсуждении EXIT важными моментами являются время и сопряженные с продолжительностью медицинских манипуляций акушерские осложнения. Ряд авторов установили, что среднее время, затраченное на интубацию новорожденного, составило 8 минут при средней кровопотере со стороны матери 800 (300–1000) мл. В 13,3% случаев понадобилось восполнить кровопотерю у роженицы [4, 7]. Другие авторы указали среднее время от момента вскрытия матки до момента клеммирования пуповины 7–9 минут. Процедуры по обеспечению оксигенации новорожденного включали ларинго-трахео-бронхоскопию или ларингоскопию и интубацию, ларингоскопию-дренирование лимфангиом и интубацию [8]. Продолжительность операции может быть больше и достигать 30,3±14,7 минут (8–66) при сочетании EXIT с экстракорпоральной мембранной оксигенацией, которая применялась у новорожденных с пренатально установленными диагнозами: кистозно-аденоматозный порок легких, односторонняя агенезия легкого, диафрагмальная грыжа в сочетании с врожденными пороками сердца при врожденной обструкции верхних дыхательных путей. Средняя кровопотеря при кесаревом сечении в данной ситуации составила 858,3±574,1 мл [9].
В 2020 г. Novoa R.H. et al. представили систематический обзор, в котором провели анализ 235 случаев применения EXIT, представленных в литературе. Средний срок проведения процедуры, как и в нашем клиническом наблюдении, составил 35,1 недели. В 46,4% случаев показанием для EXIT были тератомы шеи и ротовой полости плода. Интубацией завершились 69,8% операций, трахеостомия выполнена у 21,3% пациентов. Среднее время продолжающегося плацентарного кровообращения составило 28,5 (2–157) минуты. Ни в одном из источников литературы нет данных о материнской смертности после проведения EXIT, а наиболее частым осложнением со стороны матери стали послеродовые кровотечения (4,7%) [5].
Заключение
Таким образом, при пренатальном выявлении опухоли шеи необходимо проведение дополнительной МРТ плода, которая позволяет определить степень смещения и/или обструкции дыхательных путей и запланировать родоразрешение с привлечением специалистов для оказания помощи новорожденному. Оценка типа опухоли, ее анатомической локализации позволяет планировать этапы операции, выделять наиболее критические ее моменты и тем самым предотвращать смерть новорожденного в родах и избежать массивной кровопотери со стороны матери. Только мультидисциплинарный подход и работа команды специалистов могут обеспечить хороший перинатальный исход.