The indicators of acid-base balance and the gas composition of umbilical cord arterial and venous blood in health and fetal hypoxia
Objective. To compare the indicators of acid-base balance in the neonatal umbilical cord artery and vein in health and fetal hypoxia.Prikhodko A.M., Romanov A.Yu., Shuklina D.A., Baev O.R.
Material and methods. A prospective observational study was performed using 98 umbilical cord blood samples.
Results. The pH value was lower in the umbilical artery (7.252 ± 0.100 than that in the umbilical vein (7.297 ± 0.097) (p < 0.0001). The lactate level did not differ and was 5.929±2.807 mmol/l in the umbilical artery and 5.661 ± 2.898 mmol/l in the umbilical vein (p = 0.1074). The partial pressure of carbon dioxide was predictably higher in the umbilical artery (47.56 ± 12.68 mm Hg) than that in the umbilical vein (39.69 ± 9.70 mm Hg) (p < 0.0001); the partial pressure of oxygen was higher in the umbilical vein (17.56 ± 6.134 mm Hg) than that in the umbilical artery (23.36 ± 10.09 mm Hg) (p < 0.0001).
Conclusion. When pH values are determined, the source of umbilical cord blood sampling is critically important, whereas when lactate levels are measured, any umbilical vessel may be used. It is important to take into account the found patterns in clinical practice.
Keywords
The assessment of lactate and pH cord blood levels is of crucial importance for predicting such neonatal complications as transient tachypnea of the newborn, metabolic disorders, hypoxic-ischemic encephalopathy [1–6]as an early predictor of significant consequences and/or a fatal outcome in term neonates after a perinatal asphyxia. BACKGROUND Severe perinatal asphyxia can generate multiple organ dysfunction and neonatal mortality. METHODS In routine clinical practice, after an admission to the Intensive Care Unit, lactate concentration was determined in capillary blood samples during the first one to six hours after birth in 55 term newborns with the post-asphyxial hypoxic-ischemic encephalopathy. The control group consisted of 36 healthy term neonates randomly selected in the maternity ward at the Gynecology and Obstetrics Clinic. RESULTS Significantly higher concentrations of lactate (p 8.7 mmol/L with 80 % sensitivity and 82% specificity indicated the development of the hypoxic-ischemic encephalopathy stage II/III, while the lactate level>9.95 mmol/L was a predictor of death, with 75% sensitivity and 74.4% specificity. CONCLUSION Determination of lactate concentrations in serum of term newborns associated with risk factors -for the perinatal asphyxia is a useful tool in diagnosing metabolic disorders and ischemic damage, particularly severe clinical forms (Tab. 2, Fig. 3, Ref. 34. Fetal venous blood flows through the umbilical cord arteries to the placenta, where it becomes saturated with oxygen and nutrients and where it loses carbon dioxide. Then, through the umbilical cord vein arterial blood returns to the fetus. According to some authors, lactate level in venous and capillary blood samples is higher than in arterial ones [4]. Kruse O. et al. (2011) consider that these differences are not clinically significant [7]. Others indicate that blood sampling source does not affect the result of the analysis [8, 9]with respect to measurements of pH, bicarbonate, base excess and lactate, in critically ill term and premature newborns. METHODS Arterial blood samples (0.5-1 mL).
Despite the high accuracy of laboratory diagnostics, the pre-analytical procedures can vary significantly. Blood sampling source and method are not always clearly described [1, 2, 10], which may lead to difficulties in comparison with the results of different researches.
The aim of this study was to compare the indicators of acid-base balance (pH, lactate, base excess (ВЕ), oxygen partial pressure (pO2) and carbon dioxide partial pressure (pCO2) in the umbilical cord artery and vein blood of newborns after uncomplicated labor and labor complicated with hypoxia.
Materials and Methods
The study was conducted in the First Maternity Department of the National Medical Research Center for Obstetrics, Gynecology and Perinatology named after Academician V.I.Kulakov, Moscow. A prospective observational study was performed using 98 umbilical cord blood samples, which were obtained immediately after delivery. Three clamps were placed on the umbilical cord. The umbilical cord was cut between the first and second clamps. Blood was taken from the umbilical artery (n = 49) and vein (n = 49) between the 2-nd and 3-rd clamps. The gas analyzer ABL800 FLEX (Radiometer Medical ApS, Denmark) was used to assess pH, lactate, ВЕ, pO2 and pCO2 levels within 10 minutes after sampling.
GraphPad Prism (GraphPad Software, USA) statistical software package and R statistical programming language with RStudio 1.0.143 (RStudio, USA) were used for statistical analysis and plotting. We used a paired t-test to compare the related parametric data and Wilcoxon test to compare the related nonparametric data. Value of p < 0.05 was considered as statistically significant. The study was approved by the local institutional review board.
Results
Mean patient age was 31.4 ± 5.3 years, mean body mass index was 24.3 ± 6.3 kg/m2. Twenty-seven (55.1%) patients were primiparous and twenty-two (44.9%) were multiparous. No severe somatic diseases or pregnancy complications were observed. All deliveries were vaginal and term (39.3 ± 1.2 gestation weeks). Newborns weight ranged from 2540 g to 4320 g (3298 ± 380 g) and height ranged from 46 cm to 56 cm (51.4 ± 2.0 cm). Apgar score ranged from 5 to 9 points (95% CI: 6 – 8 points) at 1 minute and from 7 to 9 points (95% CI: 7 – 9 points) at 5 minutes.
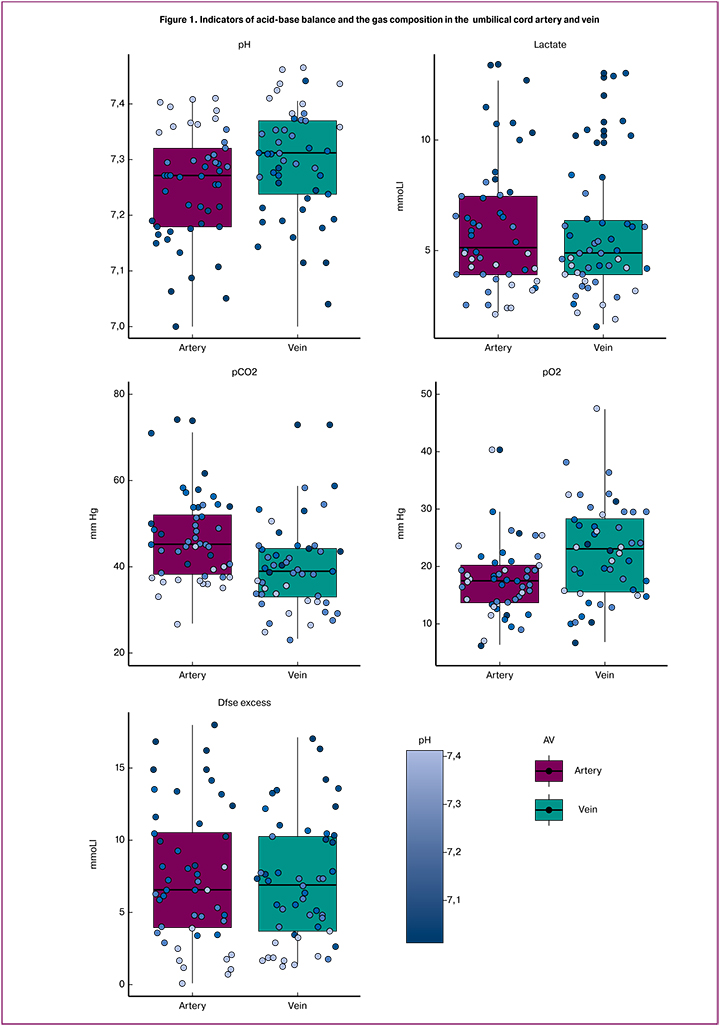
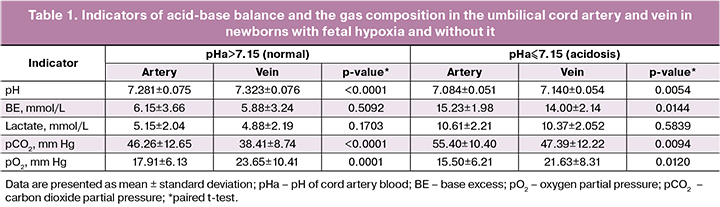
In seven (14.3%) cases arterial cord blood pH was ≤7.15. The pH level was significantly lower in the umbilical cord artery (7.252 ± 0.100) than in the umbilical cord vein (7.297 ± 0.097), p < 0.0001.
On the other hand, the lactate level was the same in both vessels (5.929 ± 2.807 vs. 5.661 ± 2.898 mmol/L, respectively; p = 0.1074) as well as the BE level (7.449 ± 4.713 vs. 7.037 ± 4.214 mmol/L, respectively; p = 0.2596).
As we expected, the pCO2 level was significantly higher in the umbilical cord artery (47.56 ± 12.68 vs. 39.69 ± 9.70 mm Hg, respectively; p < 0.0001) and the pO2 level was significantly higher in the umbilical cord vein (17.56 ± 6.134 vs. 23.36 ± 10.09 mm Hg, respectively; p < 0.0001).
Then depending on the umbilical cord artery pH (pHa) we analyzed the same parameters. We used the pHa = 7.15 parameter as a threshold since it is most commonly used in practice [11–15]we analyzed 226 women with term pregnancies complicated by severe neonatal acidosis (umbilical artery pH less than 7.00. The pHa≤7.15 parameter was classified as acidosis subgroup; the pHa > 7.15 parameter was classified as uncomplicated labour subgroup (control).
The umbilical cord artery pH level was significantly lower in both subgroups (Table 1). As in the general sample, the pCO2 level in acidosis was higher in the umbilical artery, and the pO2 level was higher in the umbilical cord vein. The lactate level was the same in umbilical cord artery and vein in both subgroups.
The BE level was significantly higher in the umbilical cord artery in the acidosis subgroup (15.23 ± 1.98 vs. 14.00 ± 2.14 mmol/L, respectively; p = 0.0144) and was the same in the uncomplicated labor subgroup (6.15 ± 3.66 vs. 5.88 ± 3.24mmol/L, respectively; p = 0.5092).
Discussion
The umbilical cord vein had significantly higher levels of pH and pO2, while the umbilical cord artery had a significantly higher level of pCO2. Lactate and BE levels were the same in both vessels. These differences correspond to the fetal-placental circulation physiology [6, 8]with respect to measurements of pH, bicarbonate, base excess and lactate, in critically ill term and premature newborns. METHODS Arterial blood samples (0.5-1 mL. In addition, a decrease in the pCO2 blood level after passing through the placenta can lead to the decrease in blood acidity in the umbilical cord veins because of the carbonic acid decomposition reaction (H+ + HCO3- CO2 + H2O) [8]with respect to measurements of pH, bicarbonate, base excess and lactate, in critically ill term and premature newborns. METHODS Arterial blood samples (0.5-1 mL.
The above mentioned differences were present both in the acidosis subgroup (pHa ≤ 7.15) and in the control subgroup (pHa > 7.15). However, in acidosis the BE level was significantly higher in the umbilical cord artery, which indicates the exhaustion of the blood buffer resources [8, 11]with respect to measurements of pH, bicarbonate, base excess and lactate, in critically ill term and premature newborns. METHODS Arterial blood samples (0.5-1 mL.
Conclusion
The umbilical cord vein has higher levels of pH and pO2, and the level of pCO2 is higher in the umbilical artery both in healthy newborns and in newborns with metabolic acidosis. The lactate level does not depend on the umbilical cord blood sampling source (artery or vein). Thus, the source of the cord blood collection is critically important in the pH level assessment, whereas any umbilical cord vessel can be used to assess the lactate level. If pH level is normal, the BE level does not differ in umbilical cord artery and vein. However, in acidosis, the BE level increases in the umbilical cord artery more dramatically than in the vein. The revealed patterns should be taken into account in clinical practice, as well as when comparing the results of different studies.
References
- Simovic A., Stojkovic A., Savic D., Milovanovic D.R. Can a single lactate value predict adverse outcome in critically ill newborn? Bratisl. Lek. Listy. 2015; 116(10): 591-5.
- Ozkiraz S., Gokmen Z., Boke S.B., Kilicdag H., Ozel D., Sert A. Lactate and lactate dehydrogenase in predicting the severity of transient tachypnea of the newborn. J. Matern. Fetal Neonatal Med. 2013; 26(12):1245-8.
- Приходько А.М., Киртбая А.Р., Романов А.Ю., Баев О.Р. Биомаркеры повреждения головного мозга у новорожденных. Неонатология. 2018; 7(1): 70-6. [Prikhodko A.M., Kirtbaya A.R., Romanov A.Yu., Baev O.R. Biomarkers of brain damage in newborns. Neonatology. 2018; 7 (1): 70-6. (in Russian)]
- Fine-Goulden M.R., Durward A. How to use lactate. Arch. Dis. Child. Educ. Pract. Ed. 2014; 99(1): 17-22.
- Приходько А.М., Романов А.Ю., Евграфова А.В., Шуклина Д.А. Определение уровня pH и лактата крови из предлежащей части плода для оценки его состояния в родах. Вопросы гинекологии, акушерства и перинатологии. 2017; 16(6): 96-9. [Prikhodko A.M., Romanov A.Yu., Evgrafova A.V., Shuklina D.A. Determination of pH and blood lactate from the presenting part of the fetus to assess its condition at birth. Issues of gynecology, obstetrics and perinatology. 2017; 16 (6): 96-9. (in Russian)]
- Приходько А.М., Баев О.Р. Определение кислотно-основного состояния пуповинной крови. Показания и техника. Акушерство и гинекология. 2018; 5:127-31. [Prikhodko A.M., Baev O.R. Determination of the acid-base state of umbilical cord blood. Indications and equipment. Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2018; 5: 127-31. (in Russian)]
- Kruse O., Grunnet N., Barfod C. Blood lactate as a predictor for in-hospital mortality in patients admitted acutely to hospital: a systematic review. Scand. J. Trauma Resusc. Emerg. Med. 2011; 19: 74.
- Araujo O.R., Diegues A.R., Silva D.C., Albertoni Ade C., Louzada M.E., Cabral E.A. et al. Agreement and correlation of pH, bicarbonate, base excess and lactate measurements in venous and arterial blood of premature and term infants. Rev. Bras. Ter Intensiva. 2007; 19(3): 322-6.
- Nadeem M., Clarke A., Dempsey E.M. Day 1 serum lactate values in preterm infants less than 32 weeks gestation. Eur. J. Pediatr. 2010; 169(6): 667-70.
- Buijs E.A., Houmes R.J., Rizopoulos D., Wildschut E.D., Reiss I.K., Ince C. et al. Arterial lactate for predicting mortality in children requiring extracorporeal membrane oxygenation. Minerva Anestesiol. 2014; 80(12): 1282-93.
- Maisonneuve E., Audibert F., Guilbaud L., Lathelize J., Jousse M., Pierre F. et al. Risk factors for severe neonatal acidosis. Obstet. Gynecol. 2011; 118(4): 818-23.
Received 15.06.2018
Accepted 22.06.2018
About the Authors
Romanov, Andrey Yu., clinical resident, National Medical Research Center for Obstetrics, Gynecology and Perinatology named after Academician V.I. Kulakovof Ministry of Healthcare of Russian Federation.
117997, Russia, Moscow, Ac. Oparina str. 4. Tel. +79031589400. E-mail: romanov1553@yandex.ru
Prikhodko, Andrey M., PhD, physician of the maternity department, National Medical Research Center for Obstetrics, Gynecology and Perinatology named
after Academician V.I. Kulakov of Ministry of Healthcare of Russian Federation.
117997, Russia, Moscow, Ac. Oparina str. 4 Tel. +74954383047. E-mail: a_prikhodko@oparina4.ru
Shuklina, Daria A., clinical resident, National Medical Research Center for Obstetrics, Gynecology and Perinatology named after Academician V.I. Kulakov
of Ministry of Healthcare of Russian Federation.
117997, Russia, Moscow, Ac. Oparina str. 4 Tel. +79686275987. E-mail: shuk2323@mail.ru
Baev, Oleg R., MD, professor, head of maternity department, National Medical Research Center for Obstetrics, Gynecology and Perinatology named after Academician V.I. Kulakov of Ministry of Healthcare of Russian Federation, professor of the Department of Obstetrics, Gynecology, Perinatology, and Reproductology of I.N. Sechenov
First Moscow State Medical University of Ministry of Healthcare of Russian Federation.
117997, Russia, Moscow, Ac. Oparina str. 4 Tel: +74954381188. E-mail: o_baev@oparina4.ru
For citations: Prikhodko A.M., Romanov A.Yu., Shuklina D.A., Baev O.R. The indicators of acid-base balance and the gas composition of umbilical cord arterial and venous blood in health and fetal hypoxia. Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2019; (2): 93-7. (in Russian)
http://dx.doi.org/10.18565/aig.2019.2.93-97