Perinatal outcomes of twin pregnancies with single fetal demise and different types of placentation
Relevance: Multiple pregnancies carry a higher risk of perinatal morbidity and mortality. In pregnancies complicated by intrauterine death of one of the co-twins, the perinatal outcome of the surviving fetus depends on the type of placentation. Objective: To investigate the impact of dichorionic and monochorionic twin pregnancies complicated by single fetal demise on perinatal outcomes. Materials and methods: A retrospective study was conducted at V.I. Kulakov NMRC for OG&P from 2014 to 2022, analyzing 113 twin pregnancies and neonatal outcomes of 99 newborns. The study subjects were divided into groups of dichorionic and monochorionic twin pregnancies. The groups were compared in terms of the course of the antenatal period and outcomes of the neonates. Results: The study analyzed 20 dichorionic and 93 monochorionic twin pregnancies. Pregnancy rates resulting from assisted reproductive technologies were higher in dichorionic twins (40%) compared to monochorionic twins (18.3%; p<0.05). The mean gestational age at intrauterine death of one co-twin was significantly lower in monochorionic twins (21.9 weeks) compared to dichorionic twins (29.6 weeks; p<0.01). Discordance in body weight of newborns was more prevalent in monochorionic twins (51.6%) compared to dichorionic twins (25%; p<0.05). Low Apgar scores in the 1st minute were more common in monochorionic twins (24%) than in dichorionic twins (10%; p=0.03). However, there was no statistically significant difference in overall morbidity between the two groups (p=0.61). Conclusion: Monochorionic placentation, compared to dichorionic placentation, is associated with specific complications in twin pregnancies complicated by single fetal demise. In monochorionic twins, the occurrence of single fetal demise happened much earlier than in dichorionic twins. Furthermore, monochorionic placentation was associated with cases of second fetal death and spontaneous demise of one of the co-twins in uncomplicated pregnancies. Neonatal mortality and morbidity rates were similar between the two groups. However, monochorionic placentation was characterized by severe central nervous and cardiovascular complications, as well as sepsis. Authors' contributions: Kostyukov K.V. – conception and design of the study, statistical analysis, manuscript drafting; Nikitina A.T., Cherepanova A.E. – data collection and analysis, review of the relevant literature; Gladkova K.A. – manuscript editing. Conflicts of interest: The authors have no conflicts of interest to declare. Funding: There was no funding for this study. Ethical Approval: The study was reviewed and approved by the Research Ethics Committee of the V.I. Kulakov NMRC for OG&P, Ministry of Health of Russia. Patient Consent for Publication: All patients provided informed consent for the publication of their data. Authors' Data Sharing Statement: The data supporting the findings of this study are available on request from the corresponding author after approval from the principal investigator. For citation: Kostyukov K.V., Nikitina A.T., Cherepanova A.E., Gladkova K.A. Perinatal outcomes of twin pregnancies with single fetal demise and different types of placentation. Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2023; (7): 40-46 (in Russian) https://dx.doi.org/10.18565/aig.2023.45Kostyukov K.V., Nikitina A.T., Cherepanova A.E., Gladkova K.A.
Keywords
Multiple pregnancies carry a greater risk of adverse outcomes than singleton pregnancies. Among the complications associated with multiple pregnancies, antenatal death of one of the co-twins is particularly concerning. According to the literature, the occurrence of intrauterine single fetal demise after 20 weeks of pregnancy ranges from 2.6% to 6.2% in all twin pregnancies [1].
Multiple pregnancies are classified into two types based on placentation: monochorionic and dichorionic, with incidences of 30% and 70%, respectively [2]. The death rate among fetuses in monochorionic twins is 15%, while it is no more than 3% in dichorionic twins [1]. Specific complications arise from the structural characteristics of the monochorionic placenta, such as the presence of vascular anastomoses and uneven division of the placenta between twins. These complications include fetofetal transfusion syndrome (FFTS), twin anemia-polycythemia sequence (TAPS), and selective intrauterine growth restriction (sIUGR). Additionally, congenital malformations and other pregnancy complications are risk factors for the death of one or both fetuses during multiple pregnancies [3]. Maternal risk factors for fetal death include preeclampsia, placental abruption, uterine scar defects after previous surgical interventions, thromboembolic and infectious complications, and spontaneous fetal death of unclear etiology [2].
Intrauterine death of one fetus can occur during any trimester of pregnancy, with varying consequences depending on the timing of death. In the first trimester, the death of one twin fetus, known as "vanishing twin syndrome," occurs in 29% of cases and typically does not affect the prognosis of the second fetus. However, fetal loss in the second and third trimesters is associated with a high rate of complications in the surviving fetus. Complications may include death of the second twin, fetal growth restriction, severe brain damage, and the development of irreversible neurological disorders.
Research indicates that in the case of antenatal death of one fetus in monochorionic twins, the risk of neurological morbidity in the surviving fetus significantly increases compared with the death of a fetus in dichorionic twins. The frequencies of neurological disorders in monochorionic and dichorionic twins are 26% and 2%, respectively [1]. This disparity is attributed to the redistribution of blood flow to the deceased fetus through placental anastomoses when one of the monochorionic twins dies. As a result, the surviving fetus experiences acute hypotension and anemia, leading to centralization of the blood circulation, ischemic damage to the central nervous system (CNS) and kidneys, and subsequent multiple organ failure. This often results in death of the second twin within the first day [3]. Surviving twins have been reported to exhibit various structural anomalies, including optic nerve hypoplasia, hypoxic-ischemic white matter lesions, microcephaly, ventriculomegaly, porencephaly, white matter hemorrhagic lesions, and post-hemorrhagic hydrocephalus [3]. Consequently, a higher incidence of cerebral palsy is observed among surviving children from twin pregnancies than in cases in which both twins survive. According to Luu T.M. and Vohr B., the probability of developing cerebral palsy is 9.5% [4].
Considering the antenatal death of one twin fetus and the likelihood of death or the development of perinatal complications in the surviving fetus, this topic holds great relevance.
This study aimed to investigate the impact of dichorionic and monochorionic twin pregnancies complicated by the death of one fetus on perinatal outcomes.
Materials and methods
This retrospective study included 113 pregnant women and 99 newborns who were examined and treated at V.I. Kulakov NMRC for OG&P in 2015–2022.
The inclusion criteria were monochorionic diamniotic and dichorionic diamniotic twin pregnancies complicated by the death of one fetus. The exclusion criteria were higher-order multiple pregnancies (triplets, quadruplets), monochorionic monoamniotic twins, and unknown chorionicity.
Gestational age was calculated from the data of the first day of the last menstruation or the crown-rump length of the larger fetus measured by ultrasound at 10–14 weeks of gestation. The types of chorionicity and amnionicity of multiple pregnancies were determined by ultrasound in the period of up to 14 weeks. The presence of the T-sign confirmed monochorionic diamniotic twins, whereas the presence of the λ-sign confirmed dichorionic diamniotic twins.
Estimated fetal weight discordance was calculated using the following formula: larger estimated weight – smaller estimated weight)/larger estimate weight) × 100. A difference of > 25% was considered clinically significant.
To assess perinatal outcomes, the study participants were divided into dichorionic and monochorionic twin pregnancies. Taking into account the data on the term and method of delivery, clinical groups that are fundamentally important for the study were also identified: preterm birth, full-term birth, physiological birth, operative delivery; in cases of caesarean delivery, the urgency (emergency or planned), as well as indications (fetal or maternal), and antenatal course of pregnancy.
Neonatal outcomes were assessed according to the following criteria: anthropometric data of the newborn (body length and birth weight), gestational age, Apgar score at 1 and 5 minutes after birth, hospitalization and duration of stay in the neonatal intensive care unit (NICU), occurrence of respiratory disorders, damage to the central nervous system, and cardiovascular and other system complications. This study did not assess the long-term outcomes after hospital discharge.
Statistical analysis
Statistical analysis and plotting were performed using Microsoft Excel spreadsheets and the GraphPad Prism 8 software package (GraphPad Software, USA). The generalized D'Agostino–Pearson test was used to determine the normality of the distribution. Normally distributed data are presented as the mean (standard deviation), and t-tests were used to compare them. Non-normally distributed data are presented as median (interquartile range) and were compared using the Mann–Whitney test. Qualitative data are presented as counts (n) and percentages (%), and were compared using Fisher's exact test. Differences were considered statistically significant at p<0.05.
Results
This study retrospectively analyzed the course of pregnancy and childbirth in 113 patients who were examined and treated at V.I. Kulakov NMRC for OG&P from 2014 to 2022. This study found that intrauterine fetal death in one twin was much more common in monochorionic placentation than in dichorionic placentation (93/113 (82.3%) vs. 20/113 (17.4%), p<0.01). The most common causes of antenatal death in one of the monochorionic twins included the combination of FFTS and sIUGR in 30/113 (32%) cases, isolated sIUGR in 17/113 (18.3%), FFTS in 16/113 (17%), and TAPS in 6/113 (6.5%). In 25/93 (26.9%) pregnant women with monochorionic twins, spontaneous fetal death occurred in an uncomplicated pregnancy. Growth restriction was the main cause of fetal death in dichorionic twins 5/20 (25%).
There were no significant differences between the groups in terms of the age of the pregnant women, body mass index, and parity.
The study groups differed significantly in the rate of pregnancies resulting from assisted reproductive technology, which was significantly higher in dichorionic twins -8/20 (40%), whereas in monochorionic twins, it was 17/93 (18.3%), p=0.04.
The clinical characteristics of the study groups are presented in Table 1.
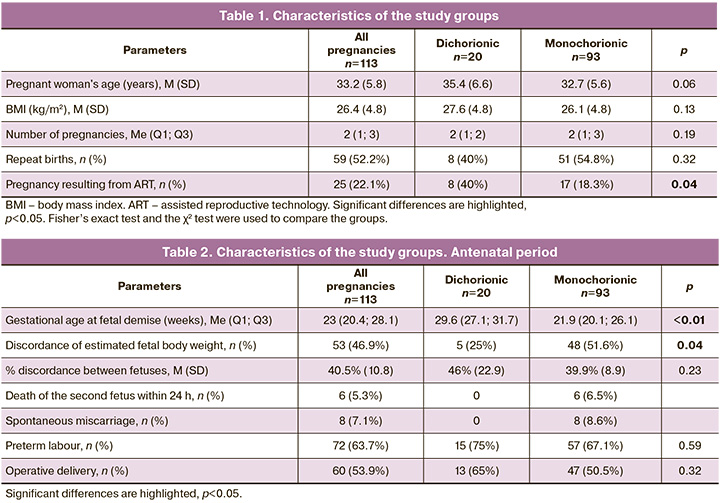
The gestational ages at single fetal demise with different types of placentation were analyzed. The gestational age at death of monochorionic and dichorionic twins was 21.9 weeks (20.1; 26.1) and 29.6 (27.1; 31.7) weeks, respectively, p<0.01.
In addition, the incidence of discordant fetal growth was statistically different. Significant discordance in the estimated weight of the fetus (more than 25%) was significantly more common in monochorionic placentation, amounting to 48/93 (51.6%), while only 5/20 (25%) in dichorionic twins (p=0.04). At the same time, the severity of discordant fetal growth in the study groups did not differ statistically and averaged 40.5 (10.8%).
In the monochorionic twin group, there were 6 cases of death of the co-twin within 24 h after the death of the first, as well as 8 cases of spontaneous miscarriage at a gestational age of less than 22 weeks.
Most pregnant women gave birth prematurely (72/113 (63.7%) patients). Preterm birth rates in the study groups did not differ significantly (57/93 (67.1 %) and 15/20 (75 %), respectively; p=0.59).
Surgical abdominal delivery was performed in 60/113 pregnant women (53.9%); the rates did not differ significantly, amounting to 47/93 (50.5%) and 13/20 (65%) in monochorionic and dichorionic twins, respectively, p=0.35.
Clinical characteristics of the antenatal period in the study groups are presented in Table 2.
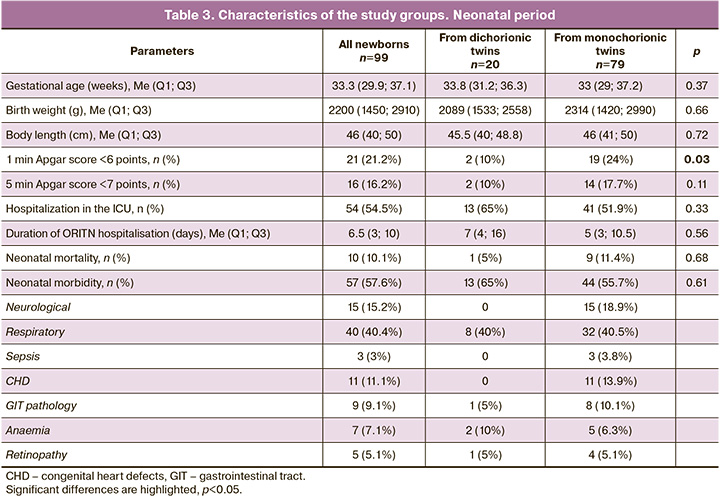
A comparison of the gestational age of the newborns showed no significant difference between the study groups. The median gestational age was 33.8 and 33 weeks in dichorionic and monochorionic twins, respectively (p=0.37).
Analysis of birth weight and body length of newborns also showed no statistically significant difference between monochorionic (2314 g, 45.5 cm) and dichorionic (2089 g, 46 cm) twins (p=0.66) and (p=0.72), respectively.
The newborns’ overall condition was evaluated using the Apgar score. In each group, the number of children with a score of 6 or less at 1 min after birth and 7 or less at 5 minutes after birth was calculated. In monochorionic twins, the number of babies with low Apgar scores was significantly higher than that in dichorionic twins (24% vs. 10% at minute 1 (p=0.03) and 17.7% vs. 10% at minute 5 (p=0.11]).
The severe course of the early neonatal period, which required hospitalization of the newborn in the NICU, was observed in 65% of dichorionic twins and 51.9% of monochorionic twins (p=0.33). The length of stay of newborns in the NICU was comparable between the study groups and amounted to 7 days for dichorionic twins and 5 days for monochorionic twins (p=0.56).
The early neonatal mortality rate in the study cohort was 10.1%. The analysis of neonatal mortality in the groups showed no statistically significant difference between dichorionic and monochorionic placentation 1/20 (5%) vs. 9/93 (11.4%), p=0.68).
The overall incidence of neonatal morbidity in the study cohort was 57.6%. Comparison of neonatal morbidity in the groups showed no significant difference: dichorionic twins, 65%; monochorionic twins, 55.7%; p=0.61).
A detailed analysis of the structure of neonatal morbidity revealed a predominance of respiratory and neurological disorders. In the study groups, the respiratory morbidity rates in dichorionic and monochorionic placentation groups were 40% and 40.5%, respectively (p>0.99). Neurological morbidity was observed only in monochorionic placentation (18.9 %). In addition, the surviving fetus from monochorionic twins is characterized by the presence of anomalies of the cardiovascular system, gastrointestinal tract, and congenital sepsis.
The detailed clinical characteristics of the newborns and the course of the neonatal period in the study groups are presented in Table 3.
Discussion
A meta-analysis of 10 studies of multiple pregnancies and their complications found that intrauterine death of one fetus occurred in 6% of twins, most of whom were monochorionic [5]. In the present study, the fetal death rate in monochorionic twins was also higher than that in dichorionic twins. The most common causes of single fetal death in monochorionic twins are specific complications. According to Morris R.K. et al., 47% and 6% of fetal deaths are caused by FFTS and sIUGR, respectively. However, in 27% of cases of intrauterine death of one fetus in monochorionic twins, the cause of death could not be determined [2]. Our study also established the predominance of specific complications of monochorionic multiple pregnancies among the causes of fetal death. The most common were FFTS (32%) and sIUGR (18.3%). The spontaneous intrauterine fetal death rate without established causes in the study cohort was 26.9%. In dichorionic pregnancies, 25% of fetal deaths were caused by fetal growth restriction.
It has also been found that the risk of death and morbidity in surviving twin is three–four times higher in monochorionic pregnancies than in dichorionic pregnancies. According to Livnat E.J. et al. [6], antenatal mortality of the second fetus in monochorionic twins is 12%, whereas that of dichorionic twins is 4%. A similar frequency was demonstrated in this study: intrauterine death of the second fetus or termination of pregnancy occurred in 15% of monochorionic twin pregnancies. However, these complications did not occur in dichorionic twins. The probable cause of death of the second twin in monochorionic twins is placental anastomoses, which cause sharp redistribution of blood flow.
Death of one of the fetuses in a twin pregnancy can occur at any gestational age. It is known that the death of a fetus in the first trimester does not have a negative effect on the second fetus or the course of pregnancy. Fetal death in the second and third trimesters often results in preterm delivery, growth restriction of the surviving twin, and increased twin morbidity and mortality [5]. At the same time, if antenatal death of one twin fetus occurs after the 32nd week of pregnancy, the risk of adverse outcomes for the surviving twin is reduced. In the course of this study, a statistically significant difference was found in the timing of death of one of the fetuses, with monochorionic twins, it was 21.9 (20.1; 26.1) weeks, and with dichorionic twins - 29.6 (27.1; 31.7] weeks, p<0.01). The earlier gestational age of reproductive losses in monochorionic twins can be explained by the fact that the most common cause of fetal death was FFTS, which occurred from the 16th to the 26th week of gestation. In dichorionic twins, a later gestational age at the time of fetal death is characteristic. In this study it was 29.6 weeks, which is explained by the later manifestation of growth restriction and decompensation of the fetal condition. This is supported by data from a study by Burgess J.L. et al. [7], who analyzed 768 multiple pregnancies and found that antenatal death in one of the fetuses after 34 weeks was observed only in dichorionic twins.
According to the literature, multiple pregnancies complicated by antenatal death of one of the fetuses are accompanied by a high rate of preterm births [8]. In most cases of multiple pregnancies complicated by fetal death, birth occurs spontaneously in the following weeks, and in about 90% of cases, it occurs within 3 weeks of fetal death [3]. The rate of preterm birth in monochorionic pregnancy with intrauterine death in one fetus is 68%, compared to 54% in dichorionic twins [1]. Analysis of the timing of delivery in the study cohort showed that the incidence of preterm births was 63.7%. At the same time, the influence of the type of chorionicity was not statistically significant: preterm birth rate was 67.1% and 75% in monochorionic and dichorionic pregnancies, respectively (p=0.59). Similar values were demonstrated in a study by DeBolt C.A. [1], in which the frequency of preterm births in monochorionic and dichorionic pregnancies was 68% and 54%, respectively. At the same time, there is evidence of a higher incidence of preterm birth with monochorionic placentation. In a study published by Arinkan S.A. et al. [9], the risk of preterm birth in surviving fetuses was 13 times higher in the group with monochorionic twins than in those with dichorionic twins. This can be explained by the high frequency of monochorionic pregnancies complicated by FFTS. Often, the cause of premature delivery in the death of one fetus from twins is iatrogenic. According to Mackie F.L. et al. [5], the frequency of iatrogenic preterm birth with monochorionic placentation was significantly higher (60.4%) than that with dichorionic placentation (32.4%).
Analysis of newborn condition showed no significant difference between the groups in gestational age, birth weight, and body length. Poor birth conditions according to Apgar scores were more common in the monochorionic group than in the dichorionic twin group.
Our study did not find an association between chorionicity and neonatal outcome. Neonatal morbidity and mortality presented with approximately the same frequency among mono- and dichorionic twins, complicated by the death of one fetus. However, according to Conte G. et al., an increased incidence of neonatal mortality among surviving monochorionic twins was 15% versus 3% for dichorionic twins [10]. In the present study, many newborns were admitted to the NICU, which could be explained by the high percentage of preterm births. This finding was also noted in a study by Morris R.K. et al. [2].
A detailed analysis of neonatal morbidity in the study groups showed a comparable incidence of pathologies caused by prematurity, such as diseases of the respiratory system, gastrointestinal tract, retinopathy, and anemia. At the same time, neurological disorders, pathology of the cardiovascular system and sepsis occurred only in monochorionic twins. Among them, one of the most severe complications of the neonatal period were neurological disorders, which occurred in 18.9% of the newborns. According to a meta-analysis, increased neurological morbidity also occurred in 26% of survivors of monochorionic twins, but only in 2% of dichorionic twins [9]. This finding suggests that the absence of neurological disorders in the surviving fetus during dichorionic pregnancy is due to the presence of the placenta.
Thus, the type of chorionicity in multiple pregnancies complicated by the death of one fetus has a great influence on perinatal outcomes. The monochorionic type has unfavorable prognostic implications, including the risk of death of the second fetus, termination of pregnancy, and the development of irreversible neurological morbidity.
The presence of prematurity-related diseases in newborns from dichorionic twins provides a relatively favorable prognosis compared with that in newborns from monochorionic twins.
The strength of the study is that it included 113 pregnant women and 99 newborns. All the patients in this study were observed and treated at the same center.
The main limitations of this study are its retrospective design and the sample size differences between the groups.
Conclusion
The monochorionic type of placentation, compared to the dichorionic type, is associated with the development of specific complications that increase the risk of adverse pregnancy outcomes. The death of one of the fetuses in monochorionic pregnancy occurs much earlier than that in dichorionic pregnancy. In addition, only with the monochorionic type of placentation were there cases of death of the second fetus and spontaneous death of one fetus from twins in uncomplicated pregnancies. Neonatal mortality and morbidity were comparable in both groups; however, the monochorionic placentation was characterized by severe complications in the central nervous and cardiovascular systems, as well as sepsis. Newborns from dichorionic twins have a relatively favorable prognosis because the incidence is mainly due to prematurity.
References
- DeBolt C.A., Mullins J., Borgida A.F. Single fetal demise in twin pregnancy. Topics Obstet. Gynecol. 2018; 38(4): 1-5. https://dx.doi.org/10.1097/01.PGO.0000530584.45244.97.
- Morris R.K., Mackie F., Garces A.T., Knight M., Kilby M.D. The incidence, maternal, fetal and neonatal consequences of single intrauterine fetal death in monochorionic twins: A prospective observational UKOSS study. PLoS One. 2020; 15(9): e0239477. https://dx.doi.org/10.1371/journal.pone.0239477.
- Stefanescu B.I., Adam A.M., Constantin G.B., Trus C. Single fetal demise in twin pregnancy-A great concern but still a favorable outcome. Diseases. 2021; 9(2): 33. https://dx.doi.org/10.3390/diseases9020033.
- Luu T.M., Vohr B. Twinning on the brain: the effect on neurodevelopmental outcomes. Am. J. Med. Genet. C Semin. Med. Genet. 2009; 151C(2): 142-7. https://dx.doi.org/10.1002/ajmg.c.30208.
- Mackie F.L., Rigby A., Morris R.K., Kilby M.D. Prognosis of the co-twin fol-lowing spontaneous single intrauterine fetal death in twin pregnancies: a sys-tematic review and meta-analysis. BJOG. 2019; 126(5): 569-78.https://dx.doi.org/10.1111/1471-0528.15530.
- Livnat E.J., Burd L., Cadkin A., Keh P., Ward A.B. Fetus papyraceus in twin pregnancy. Obstet. Gynecol. 1978; 51(1, Suppl.): 41s-5s.
- Burgess J.L., Unal E.R., Nietert P.J., Newman R.B. Risk of late-preterm still-birth and neonatal morbidity for monochorionic and dichorionic twins. Am. J. Obstet. Gynecol. 2014; 210(6): 578.e1-9. https://dx.doi.org/10.1016/j.ajog.2014.03.003.
- Костюков К.В., Гладкова К.А. Перинатальные исходы при монохориальной многоплодной беременности, осложненной синдромом селективной задержки роста плода. Акушерство и гинекология. 2020; 6: 50-8. [Kostyukov K.V., Gladkova K.A. Perinatal outcomes of monochorionic multiple pregnancies with selective intrauterine growth restriction. Obstetrics and Gynecology. 2020; (6): 50-8. (in Russian)]. https://dx.doi.org/10.18565/aig.2020.6.50-58.
- Arınkan S.A., Arısoy R., Api M. Assesment of pregnancy outcomes among twin pregnancies with single fetal demise regarding chorionicity and fetal death time. J. Turk. Ger. Gynecol. Assoc. 2019; 20: 147. https://dx.doi.org/10.4274/jtgga.galenos.2018.2018.0053.
- Conte G., Righini A., Griffiths P.D., Rustico M., Lanna M., Mackie F.L. et al. Brain-injured survivors of monochorionic twin pregnancies complicated by single intrauterine death: MR findings in a multicenter study. Radiology. 2018; 288(2): 582-90. https://dx.doi.org/10.1148/radiol.2018171267.
Received 16.02.2023
Accepted 28.06.2023
About the Authors
Kirill V. Kostyukov, Dr. Med. Sci., Head of the Department of the Ultrasound and Functional Diagnosis, V.I. Kulakov NMRC for OG&P, Ministry of Health of Russia,+7(926) 214-97-84, kostyukov_k@yahoo.com, https://orcid.org/0000-0003-3094-4013, 117997, Russia, Moscow, Ak. Oparin str., 4.
Kristina A. Gladkova, Ph.D., Senior Researcher at the Fetal Medicine Unit, Institute of Obstetrics, Head of the 1st Obstetric Department of Pregnancy Pathology,
V.I. Kulakov NMRC for OG&P, Ministry of Health of Russia, +7(916)321-10-07, k_gladkova@oparina4.ru, 117997, Russia, Moscow, Ak. Oparin str., 4.
Arina T. Nikitina, student, I.M. Sechenov First MSMU, Ministry of Health of Russia, arinia2000@yandex.ru, 119991, Russia, Moscow, Trubetskaya str., 8-2.
Alina E. Cherepanova, student, I.M. Sechenov First MSMU, Ministry of Health of Russia, acherepanova1@gmail.com, 119991, Russia, Moscow, Trubetskaya str., 8-2.