Long-term results of surgical treatment of pelvic organ prolapse using prosthetic mesh
Objective: To analyze postoperative complications in patients after surgical treatment of apical pelvic organ prolapse using prosthetic mesh. Materials and methods: In this study we analyzed complications after surgical implantation of polypropylene (PP) meshes in women with genital prolapse within 18–36 months after surgery. Retrospectively, 732 women were divided into 2 groups depending on the techniques used for surgical treatment of pelvic organ prolapse. Group 1 consisted of patients who underwent laparoscopic sacrocolpopexy using polypropylene mesh prosthesis (n=348). Group 2 consisted of patients who underwent transvaginal bilateral sacrospinous fixation with implantation of a polypropylene mesh prosthesis (n=394). Statistical processing of the obtained results was performed using software packages STATISTICA 10.0 and Eviews 12.0. Results: Recurrence of genital prolapse occurred in 28 women (8.0%) in group 1, while this complication was diagnosed in 62 women (15.7%) in group 2, p<0.001. The rate of vaginal wall erosion after prosthetic mesh implantation was 2.0% and 6.3% in group 1 and 2, respectively. The rate was significantly high among women who underwent sacrospinous fixation (group 2), p<0.001. In premenopause, surgical treatment of women with genital prolapse using bilateral sacrospinous fixation increases the risk of vaginal wall erosion (AUC 0.736, p=0.004, 95% CI: 0.535-0.896). Conclusion: Analysis of postoperative complications showed that laparoscopic sacrocolpopexy is more effective versus bilateral sacrospinous fixation.Berg P.A., Musin I.I., Yaschuk A.G., Naftulovich R.A., Battalova G.Yu.
Keywords
Every year over 300,000 women undergo surgery for genital prolapse, and most commonly for anterior colporrhaphy. This surgical technique is used for reconstruction of pelvic floor using the patient's overstretched tissues, and apical support is not provided. The recent studies reported that the rate of recurrences after anterior colporrhaphy reaches 40% [1, 2].
In search of a method for surgical treatment with the best outcomes, pelvic surgeons began to use transplants to improve the quality of care for women with pelvic organ prolapse (POP). Initially, allotransplants and xenotransplants were used for pelvic floor reconstruction. However, success rates for using these transplants decreased over time due to unpredictable tissue response and reduction in tensile strength. The next step was the decision to use synthetic mesh prosthesis to improve surgical outcomes of genital prolapse.
An updated Cochrane review of 40 studies demonstrated that the use prosthetic mesh for anterior colporrhaphy reduces recurrence of cystocele compared to conventional anterior colporrhaphy [3]. Nevertheless, the quality of life was comparable both using prosthetic mesh and without it. Moreover, with increasing frequency it was reported about complications, which were specific only for mesh prosthesis (deformation, erosion, shortening of vaginal mesh). The rate of complications varies from 2.7% to 20.0% among all women, who underwent surgery, and the average rate reaches 10.8% [4–8]. In such a case, the question arises, which of techniques with the use of mesh implants is more effective and safe.
Maher C. et al. [9] conducted a single-center randomized controlled trial, which compared laparoscopic sacrocolpopexy (LSC) with anterior colporrhaphy using Prolift mesh implant. The authors came to the conсlusion that the rate of objective success of sacrocolpopexy (SC) is higher versus anterior colporrhaphy using Prolift mesh implant, and the rates of reoperation and perioperative morbidity is lower.
Also worth noting is transvaginal sacrospinous fixation (SSF) performed using polypropylene mesh prosthesis. The study by Solomon E.R. et al. was devoted to investigation of the safety and efficacy of bilateral sacrospinous ligament fixation (BSSLF) for surgical repair of apical prolapse [10]. The researchers concluded that the number of complications after surgery is minimal, and this surgical technique is safety and effective.
Other pelvic surgeons [11] also proved that performance of BSSLF for reinforcement of the anterior vaginal wall with mesh prosthesis is a safety method for surgical treatment of genital prolapse, especially in women not having sexual activity.
Thus, this transvaginal method for apical support is most acceptable, effective, safe and well tolerated by women with anterior apical prolapse. Other researchers concluded [12] that sacrospinous ligament fixation with prosthetic mesh reduces the number of recurrences of genital prolapse. But complications still occur, including the specific complications associated with prosthetic mesh implantation.
Comparison between short-term outcomes of LSC and transvaginal SSF using prosthetic mesh was performed by a group of researchers in 2018 [13] and demonstrated that there were no significant differences in the rate of short-terms complications. However, the duration of surgery was slightly longer than in patients who underwent SC. Also, the authors reported that this issue requests further research.
For this reason, the objective of our study was analysis of the effectiveness of LSC and transvaginal BSSLF for treatment of apical pelvic organ prolapse in the context of implant-associated complications.
Materials and methods
The authors of this article analyzed complications after implantation of polypropylene mesh prosthesis for genital prolapse during 18–36 months after surgery. In total, 732 medical histories of patients were retrospectively analyzed. The patients underwent surgery for POP with the use of polypropylene mesh prostheses in the gynecological departments of the Republican clinical hospital named after G.G. Kuvatov, in city clinical hospitals Nos. 8 and 18 in 2015–2021. The women were divided into 2 groups depending on the method for surgical treatment of POP. The patients after LSC using polypropylene mesh prosthesis (n=348) were recruited for group I, and the patients after transvaginal BSSLF using polypropylene mesh prosthesis were recruited into group 2 (n=394). The relationship between the parameters of obstetric and gynecological, somatic anamnesis, surgical protocol, the course of postoperative period, postoperative complications was analyzed in women who participated in the study. Also, the patients were prospectively investigated using valid questionnaires PISQ-12 Pelvic Organ Prolapse and Incontinence Sexual Function [14] (assessment of the symptoms of prolapse and the quality of sexual life) and EQ-5D [15] (assessment of quality of life) in 18–36 months after surgical treatment of POP. The criteria for the effectiveness of surgical treatment of POP were the presence of stage 0–I according to the Pelvic Organ Prolapse Quantification System (POP-Q) and the absence of the symptoms of vaginal wall erosion. The criteria for recurrence of the disease were considered as the presence of stage II–IV according to POP-Q.
Inclusion criteria in the study were: the presence of symptomatic types of POP with ≥ stage II POP-Q requiring surgical treatment; the presence of anterior apical POP; possibility to visit the clinic and undergo diagnostic testing for complications and screening in 18–36 months after surgical treatment.
Exclusion criteria were: posterior vaginal prolapse, previous surgical treatment of POP.
LSC was performed in two steps. The first step was transvaginal hysterectomy; the distal end of mesh prosthesis was fixed to the posterior wall of the vaginal сuff and inserted into pelvis. The second step was laparoscopic fixation of the proximal end of mesh prosthesis to the sacral promontory in the area of the first and second sacral vertebrae bones.
BSSLF procedure included transvaginal hysterectomy, prosthetic mesh fixation to the vaginal cuff and sacrospinous ligament suspension on both sides.
Statistical analysis
Statistical data analysis was performed using statistical software packages STATISTICA 10.0 and EViews 12.0, SPSS. The results were statistically significant at p-value˂0.05. Mann–Whitney U-test was used for quantitative comparison between the groups due to absence of the normal distribution. Pearson's chi-square test (χ2) was used to compare statistical significance of differences between two relative independent parameters. The odds ratio (OR) and 95% confidence interval (CI) were used to measure association. SPSS software was used to assess the associations between the analyzed factors and formation of vaginal wall erosion. The value of the quantitative parameter is shown as median and interquartile range 25–75 – Me (Q25; Q75). Binary logistic regression was used and ROC-curve was created for statistical assessment of the role of surgical technique, the data of gynecological anamnesis for development of the outcome under study – vaginal wall erosion after using prosthetic mesh.
Results and discussion
The age of patients in group I was 51.0 (47.0; 58.0) years and was similar to the age of patients in group II – 52.0 (46.0; 58.0) years, р=0.548.
The analysis of obstetric and gynecological anamnesis showed that there were no significant differences in the parameters of age at menarche, number of pregnancies and births (Table 1).
Analysis of the data regarding the performed surgical treatment showed that blood loss during LSC was 320.0 (250.0; 410.0) ml in group I, while in group II it was 260.0 (190.0; 340.0) ml, and the difference was significant between the groups (р=0.006). Operative duration was significantly higher in group I than in group II and was 162.0 (140.0; 186.0) minutes versus 88.0 (76.0; 112.0) minutes. Thus, performance of LSC was associated with longer surgical intervention, but was comparable with regard to blood loss during BSSLF. Early postoperative period was without complications in all patients. The length of hospital stay was 6 (5; 7) days in group I and 5 (4; 5) days in group 2. The differences were statistically significant (р=0.033) and indicated shorter hospital stay of patients who underwent BSSLF. Therefore, shorter length of hospital stаy and less blood loss were after BSSLF versus LSC.
In 18–36 months after surgical treatment, the patients were invited for gynecological examination and diagnostics of postoperative complications of POP, as well as the patients filled in the valid questionnaires related to the quality of life and the presence of POP symptoms.
In 313/348 (89.9%) women in group I after SC, the surgical treatment was considered effective (stages 0–I POP-Q and the absence of vaginal wall erosion), as well as in 87/394 (77.9%) patients in group II after BSSLF. However, the results of surgical treatment of POP were more successful in group I (р<0.001).
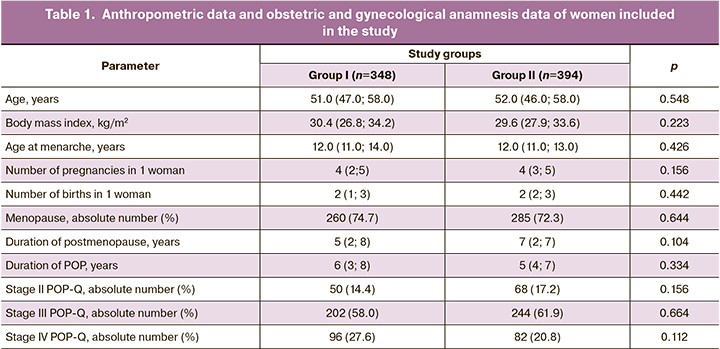
POP recurrence occurred in 28/348 (8.0%) women after LSC (group I); while in women in group II, posthysterectomic prolapse after BSSLF was diagnosed in 62/394 (15.7%) patients, р<0.001. It should be noted that in women with early posthysterectomic prolapse and pronounced deformation of vaginal vault (Fig. 1), surgical treatment was difficult due to the risk of complications associated with reimplantation. A number of unanswered questions that still need to be answered include preparation for surgical treatment, the choice of the technique for surgical correction, rehabilitation of these patient.
In 7/348 (2,0%) women in group I, vaginal was erosion was diagnosed in the postoperative period after using polypropylene mesh prosthesis, as well as in 25/394 (6.3%) patients in group II. The number of women with erosion, who underwent BSSLF (group II), significantly increased, р<0.001. The symptoms of vaginal wall erosion were: purulent discharge or vaginal tract bleeding, perineum pain, discomfort during intercourse. This complication was diagnosed on average in 180.0 (45,0; 630,0) days after surgical treatment of POP. Pelvic examination with speculum revealed the presence of denuded mesh prosthesis in the vaginal wall, often with inflammatory infiltrate in the surrounding area. Also, it should be noted that in 24/32 (75.0%) patients with vaginal wall erosion the recurrence of pelvic organ prolapse was diagnosed. The analysis of gynecological anamnesis found that most of patients 20/32 (62.5%) with vaginal wall erosion had a perimenopausal status during surgical treatment, and this led to the complication.
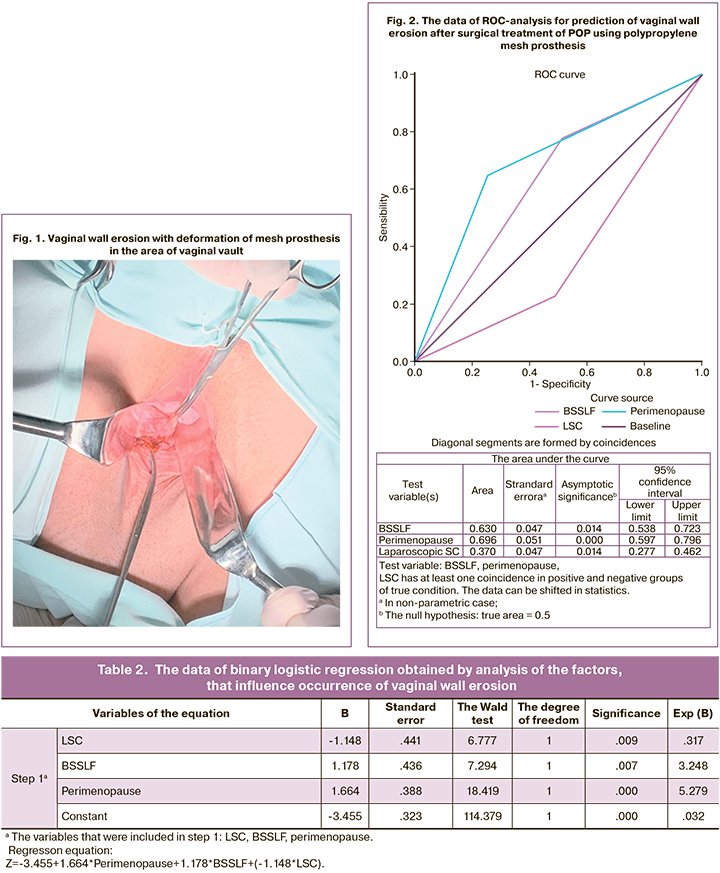
Binary logistic regression and ROC-analysis were used for statistical assessment of the role of the factors that influence the occurrence of vaginal wall erosion after using mesh prosthesis (Table 2, Fig. 2). The presence of erosion of the vaginal wall after reconstructive surgery of the pelvic floor with the use of a mesh prosthesis was considered as a dependent variable, and the surgical correction of POP using transvaginal BSSLF, LSC and treatment of patients with perimenopausal status were considered as predictor variables.
Thus, the analysis of the data obtained from women with vaginal wall erosion showed that surgical treatment of patients with POP in the perimenopausal period (AUC 0.696, р<0.001, 95%, 95% CI 0.597–0.796) using BSSLF (AUC 0.630, р=0.014, 95%, 95% CI 0,538–0,723) increases the risk of this complication. The model was not validated.
All women, participating in the study were surveyed in 18–36 months after surgical treatment with the use of valid questionnaires. The number of scores obtained by women in group I after they answered the questions of PISQ-12 questionnaire was 22.0 (14,0; 29,0) out of possible 48 points, while in women in group II, the average score was 15.0 (8.0; 24.0) points and was significantly lower, р=0.002. This result indicated a lower quality of sexual life in patients who underwent BSSLF with the use of polypropylene mesh prosthesis versus the group of women, who underwent LSC. This could be due to the presence of POP symptoms, as well as dyspareunia and erosion of the vaginal mucosa in these women. The analysis of the answers to another valid EQ-5D questionnaire оn health-related current quality of live showed the following results. In group I, the number of scores was 5.0 (5.0; 6.0) out of 15 possible points. This indicated a high quality of life, while in women in group II, the value of this parameter was higher (р=0,023) and the score reached 6.0 (6.0; 8.0) points. This was associated with postoperative complications, which significantly reduced the quality of live (in this group, vaginal wall erosion and recurrence of pelvic organ prolapse occurred more often).
In our opinion, the increased number of postoperative complications, such as recurrence of pelvic organ prolapse and vaginal wall erosion after using polypropylene mesh prosthesis in women, who underwent transvaginal BSSLF, was associated with several factors.
First of all, LSC is an operation of a higher level of complexity. As a rule, it is performed by the surgeon, who has extremely high level of training. In this case, incorrect placement of mesh prosthesis, which can lead to deformation, erosion of the vaginal wall and recurrence of pelvic prolapse, are less likely.
Secondly, with transvaginal access, the blind passage of the needle can lead to pelvic nerve injury, pelvic pain, and dyspareunia, and worsen the surgical outcomes. Moore R.D. et al. came to similar conclusion. They reported in the article [16] that elimination of blind passages of the trocar-based needle reduces the risk of bleeding, pain and deformation of mesh prosthesis.
It is also likely, that prosthetic mesh fixation to the patient’s sacrospinous overstretched ligaments contributes to recurrence of the disease, especially in patients with hereditary disorders of connective tissue.
Conclusion
Surgical treatment of patients with POP using prosthetic mesh led to occurrence of implant-associated complications, and their pathogenesis is understudied. Assessment of the effectiveness of different surgical techniques in the context of reduction of the frequency of these complications is extremely important. In this regard, LSC is more advantageous versus BSSLF. In addition, this method of surgical treatment for pelvic organ prolapse demonstrated a higher quality of life in women in late postoperative period. This was associated with surgical treatment satisfaction. Formation of risk group of women with implant-associated complications and surgical correction to minimize these risks will improve the quality of care for women with POP.
References
- Ищенко А.И., Александров Л.С., Ищенко А.А., Хохлова И.Д.,Гаврилова Т.В., Горбенко О.Ю., Джибладзе Т.А., Брюнин Д.В.,Гадаева И.В., Малюта Е.Г. Усовершенствованный хирургический подход к лечению пациенток с полным выпадением матки. Вопросы гинекологии, акушерства и перинатологии. 2020; 19(1): 32-9. https://dx.doi.org/10.20953/1726-1678-2020-1-32-39. [Ishchenko A.I.,Aleksandrov L.S., Ishchenko A.A., Khokhlova I.D., Gavrilova T.V.,Gorbenko O.Yu., Dzhibladze T.A., Bryunin D.V., Gadaeva I.V., Malyuta E.G. An improved surgical approach to treatment of patients with complete uterine prolapse. Issues of Gynecology, Obstetrics and Perinatology. 2020; 19(1): 32–9. (in Russian)]. https://dx.doi.org/10.20953/1726-1678-2020-1-32-39.
- Аполихина И.А., Дикке Г.Б., Бычкова А.Е. Консервативное лечение пролапса половых органов. Акушерство и гинекология. 2019; 6 (Приложение): 22-4. [Apolikhina I.A., Dikke G.B., Bychkova A.E. Conservative treatment of pelvic organ prolapse. Obstetrics and gynecology. 2019; 6 Suppl: 22-4.(in Russian)].
- Maher C.M., Feiner B., Baessler K., Glazener C.M. Surgical management of pelvic organ prolapse in women: the updated summary version Cochrane review. Int. Urogynecol. J. 2011; 22(11): 1445-57. https://dx.doi.org/10.1007/s00192-011-1542-9.
- Deng T., Liao B., Luo D., Shen H., Wang K. Risk factors for mesh erosion after female pelvic floor reconstructive surgery: a systematic review and meta-analysis. BJU Int. 2016; 117(2): 323-43. https://dx.doi.org/10.1111/bju.13158.
- Ganer H.H., Raz N., Gold E., Bar J., Condrea A., Ginath S. Risk of mesh erosion after pelvic organ prolapse repair with or without concomitant vaginal hysterectomy. Isr. Med. Assoc. J. 2019; 21(6): 399-403.
- MacCraith E., Cunnane E.M., Joyce M., Forde J.C., O'Brien F.J., Davis N.F. Comparison of synthetic mesh erosion and chronic pain rates after surgery for pelvic organ prolapse and stress urinary incontinence: a systematic review. In.t Urogynecol. J. 2021; 32(3): 573-80. https://dx.doi.org/10.1007/s00192-020-04612-x.
- Kim T.Y., Jeon M.J. Risk factors for vaginal mesh erosion after sacrocolpopexy in Korean women. PLoS One. 2020; 15(2): e0228566. https://dx.doi.org/10.1371/journal.pone.0228566.
- Ерема В.В., Буянова С.Н., Мгелиашвили М.В., Петракова С.А., Пучкова Н.В.,Юдина Н.В., Глебов Т.А. Mesh-ассоциированные осложнения при коррекции пролапса тазовых органов и стрессовой формы недержания мочи. Российский вестник акушера-гинеколога. 2021; 21(3): 748. https://dx.doi.org/10.17116/rosakush20212103174. [Erema V.V., Buyanova S.N.,Mgeliashvili M.V., Petrakova S.A., Puchkova N.V., Yudina N.V., Glebov T.A.Mesh-associated complications in the correction of pelvic organ prolapse and stress urinary incontinence. Russian Bulletin of Obstetrician-Gynecologist. 2021;21(3):748. (in Russian)]. https://dx.doi.org/10.17116/rosakush20212103174.
- Maher C.F., Feiner B., DeCuyper E.M., Nichlos C.J., Hickey K.V.,O'Rourke P.. Laparoscopic sacral colpopexy versus total vaginal mesh for vaginal vault prolapse: a randomized trial. Am. J. Obstet. Gynecol. 2011; 204: 360e1-e7. https://dx.doi.org/10.1016/j.ajog.2010.11.016.
- Solomon E.R., St Marie P., Jones K.A., Harmanli O. Anterior bilateral sacrospinous ligament fixation: a safe route for apicalepair. Female Pelvic Med. Reconstr. Surg. 2020; 26(8): e33-6. https://dx.doi.org/10.1097/SPV.0000000000000857.
- Zhu Q., Shu H., Du G., Dai Z. Impact of transvaginal modified sacrospinous ligament fixation with mesh for the treatment of pelvic organ prolapse-before and after studies. Int. J. Surg. 2018; 52: 40-3. https://dx.doi.org/10.1016/j.ijsu.2018.02.021.
- Yazdany T., Wong K., Bhatia N.N. Sacrospinous ligament fixation for pelvic organ prolapse in the era of vaginal mesh kits. Curr. Opin. Obstet. Gynecol. 2011; 23(5): 391-5. https://dx.doi.org/10.1097/GCO.0b013e32834ac743.
- Biler A., Ertaş İ.E., Tosun G., Hortu İ., Demir A., Taner C.E. et al. Perioperative complications and short-term outcomes of abdominal sacrocolpopexy, laparoscopic sacrocolpopexy, sacrospinous ligament fixation, and iliococcygeus fixation procedures. Turk. J. Med. Sci. 2018; 48(3): 602-10. https://dx.doi.org/10.3906/sag-1712-203.
- Aschkenazi S.O., Rogers R.G., Beaumont J., Botros S.M., Sand P.K.,Goldberg R.P. A valid form of the PISQ-12, the PISQ-9, for use in comparative studies of women with and without pelvic organ prolapse and/or urinary incontinence. Female Pelvic Med. Reconstr. Surg. 2010; 16(4): 218-23.https://dx.doi.org/10.1097/SPV.0b013e3181e4f132.
- Balestroni G., Bertolotti G. L'EuroQol-5D (EQ-5D): uno strumento per la misura della qualità della vita [EuroQol-5D (EQ-5D): an instrument for measuring quality of life]. Monaldi Arch. Chest Dis. 2012; 78(3): 155-9. (in Italian). https://dx.doi.org/ 10.4081/monaldi.2012.121.
- Moore R.D., Mitchell G.K., Miklos J.R. Single-incision vaginal approach to treat cystocele and valut prolapse with an anterior wall mesh anchored apically to the sacrospinous ligaments. Int. Urogynecol. J. 2012; 23(1): 85-91.https://dx.doi.org/ 10.1007/s00192-011-1536-7.
Received 17.06.2022
Accepted 11.10.2022
About the Authors
Polina A. Berg, assistant, Department of obstetrics and gynecology with IPE course, Bashkir State Medical University, Ministry of Health of Russia, +7(917)467-10-64, p.a.berg@mail.ru, 450008, Russia, Bashkortostan, Ufa, Lenin str., 3.Ilnur I. Musin, PhD, Associate Professor, Department of obstetrics and gynecology with IPE course, Bashkir State Medical University, Ministry of Health of Russia,
+7(917)467-10-64, ilnur-musin@yandex.ru, 450008, Russia, Bashkortostan, Ufa, Lenin str., 3.
Alfiya G. Yashchuk, Dr. Med. Sci., Professor, Head of the Department of obstetrics and gynecology with IPE course, Bashkir State Medical University, Ministry of Health
of Russia, +73472649650, alfiya_galimovna@mail.ru, 450008, Russia, Bashkortostan, Ufa, Lenin str., 3.
Raisa A. Naftulovich, PhD, Associate Professor, Department of obstetrics and gynecology with IPE course, Bashkir State Medical University, Ministry of Health of Russia, +79173490472, 450008, Russia, Bashkortostan, Ufa, Lenin str., 3.
Guzel Yu. Battalova, Dr. Med. Sci., Professor at the Department of Obstetrics and Gynecology No. 1, Bashkir State Medical University, Ministry of Health of Russia, +73472649650, 450008, Russia, Bashkortostan, Ufa, Lenin str., 3.
Authors’ contributions: Berg P.A. – writing the article, statistical data processing, material collection; Musin I.I. – the design of the study, material collection; Yaschuk A.G. – the concept of the study, article text editing, approval of the final version of the article; Naftulovich R.A. – article text editing, material collection; Battalova G.Yu. – article text editing, approval of the final version of the article.
Conflicts of interest: The authors declare that they have no conflict of interests.
Funding: The study was carried out without any sponsorship.
Ethical Approval: The study was approved by the local Ethics Committee of Bashkir State Medical University, Ministry of Health of Russia.
Patients’Consent for Publication: The patients have signed informed consent for participation in the study and publication of the results.
Authors' Data Sharing Statement: The data supporting the findings of this study are available on request from the corresponding author after approval from the principal investigator.
For citation: Berg P.A., Musin I.I., Yaschuk A.G., Naftulovich R.A., Battalova G.Yu.
Long-term results of surgical treatment of pelvic organ prolapse using prosthetic mesh.
Akusherstvo i Gynecologia/Obstetrics and Gynecology. 2022; 11: 141-147 (in Russian)
https://dx.doi.org/10.18565/aig.2022.11.141-147