The role of bulbocavernosus reflex in the diagnosis of neuropathy in patients with pelvic organ prolapse and pelvic pain syndrome
Aim. To investigate the clinical value of testing bulbocavernosus reflex (BCR) and the M-response during pudendal nerve stimulation electroneuromyography (ENMG) in patients with pelvic organ prolapse and neurogenic pain syndrome.Fomenko O.Yu., Poryadin G.V., Martynov M.Yu., Kashnikov V.N., Shkoda A.S., Kozlov V.A., Belousova S.V., Rumyantsev A.S., Achkasov S.I.
Materials and methods. The study included 56 patients with pelvic organ prolapse and chronic neurogenic pelvic pain managed from 2019 to 2020. The mean age of patients was 50.1 ± 11.6 years. The patients had pelvic organ prolapse in the form of rectocele [25/56 (44.6%)] and rectocele combined with internal rectal intussusception [31/56 (55.4%)]. All patients underwent comprehensive examination, including physical examination, colonoscopy (to exclude organic pathology), defecography (to diagnose rectocele and internal rectal intussusception), neurophysiological study (stimulation ENMG) to measure the M-response and BCR. The statistical analysis was performed using Stata 14.2 (StataCorp).
Results. Among patients with pelvic organ prolapse and neurogenic pelvic pain, 66.1% had abnormal M-response latency. Changes in BCR parameters were observed in 33.9% of patients with pelvic organ prolapse and neurogenic pelvic pain with normal M-response. In a clinical context, this observation can be interpreted as a sign of pudendal neuropathy. BCR latency was evoked in all patients and was abnormal in 92.9% of them. In 7.1% of cases of normal BCR latency, M-response latency was changed.
Conclusion. Assessment of pelvic floor muscles innervation requires testing for both M-response and BCR, which allows identification of pudendal neuropathy in all patients with pelvic organ prolapse and neurogenic pelvic pain.
Keywords
Speaking about disorders of the pelvic floor muscle innervation, including pelvic organ prolapse ("genital prolapse is a disease in which the pelvic organs prolapse through the vagina" [1]), we mean pudendal nerve dysfunction, that is, neuropathy. Causes of neuropathy in women with genital prolapse can be obstetric injury and nerve overstretching, which mechanically occurs in the perineal prolapse [2–4]. In this case, neuropathy can manifest both as sensitive (chronic neurogenic pelvic pain) and motor (impaired bowel holding and emptying functions, voiding disorders, sexual dysfunctions), and their combination [5, 6].
In the literature, pudendal neuropathy is often referred to as pudendal nerve entrapment, Alcock's canal syndrome, and pudendal neuralgia as synonyms.
In pudendal nerve entrapment (PNE) syndrome, chronic pain is caused by compression of the pudendal nerve in Alcock’s canal [7]. The pain is usually aggravated by sitting. Other symptoms include sensory (genital numbness) and motor disorders in the form of fecal and urinary incontinence [8–15].
 The term pudendal neuralgia is often used interchangeably with a pudendal nerve entrapment or Alcock's canal syndrome. However, a 2009 survey study found no direct evidence to support equating pudendal neuralgia and Alcock's canal syndrome because the 2008 Nantes criteria suggest that all neuralgia symptoms can occur without pudendal nerve entrapment [16–18]. In our opinion, the term "neuropathy," also called "peripheral neuropathy," as a collective term, can refer to any condition that affects the normal activity of peripheral nerves. The causes can be both hereditary and acquired. Speaking about neuropathy of the pudendal nerve, we mean its axonopathy and/or impaired myelination, i.e., demyelination.
The term pudendal neuralgia is often used interchangeably with a pudendal nerve entrapment or Alcock's canal syndrome. However, a 2009 survey study found no direct evidence to support equating pudendal neuralgia and Alcock's canal syndrome because the 2008 Nantes criteria suggest that all neuralgia symptoms can occur without pudendal nerve entrapment [16–18]. In our opinion, the term "neuropathy," also called "peripheral neuropathy," as a collective term, can refer to any condition that affects the normal activity of peripheral nerves. The causes can be both hereditary and acquired. Speaking about neuropathy of the pudendal nerve, we mean its axonopathy and/or impaired myelination, i.e., demyelination.
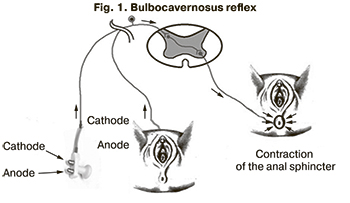
Electroneuromyography (ENMG) using a St Mark's electrode is used to diagnose pudendal nerve injury, its demyelination. Usually, this technique is used to assess the latency of the M-response. However, according to the methodology of Contreras Ortiz O. et al. St. Mark's electrode can also be used to examine the bulbocavernosus reflex (BCR) [19–22], which is a physiological reflex of contraction of the bulbous-spongy muscle elicited with compression of the glans penis or clitoris [23] (Fig. 1).
 According to the Atlas of anatomy, the pudendal nerve (n. Pudendus), together with the internal genital vessels, travels into the perineal region via the piriform opening, bending around the spina ischiadica, goes into the lesser sciatic foramen, lies between the sacrospinous ligament and obturator internus muscle, being in the cleavage of the fascia obturatoria, which is called the pudendal canal (canalis pudendalis, Alcock's canal). Pudendal nerve, branching out in the perineal region, innervates the muscles of the perineum (external anal sphincter; levator ani muscle; sciatic-cavernous and bulbous-spongy muscles; the superficial and deep transverse perineal muscles; external urethral sphincter), the skin of the perineum and external genital organs [24].
According to the Atlas of anatomy, the pudendal nerve (n. Pudendus), together with the internal genital vessels, travels into the perineal region via the piriform opening, bending around the spina ischiadica, goes into the lesser sciatic foramen, lies between the sacrospinous ligament and obturator internus muscle, being in the cleavage of the fascia obturatoria, which is called the pudendal canal (canalis pudendalis, Alcock's canal). Pudendal nerve, branching out in the perineal region, innervates the muscles of the perineum (external anal sphincter; levator ani muscle; sciatic-cavernous and bulbous-spongy muscles; the superficial and deep transverse perineal muscles; external urethral sphincter), the skin of the perineum and external genital organs [24].
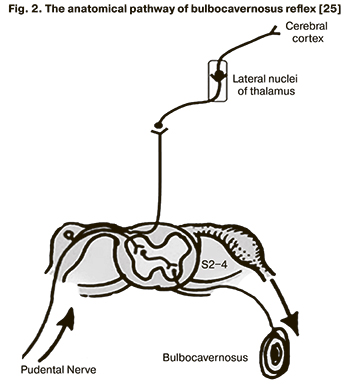
BCR causes the contraction of the bulbocavernosus muscles by stimulating the pudendal nerve through the sacral reflex arc. Objectively, the conduction time of the pudendal nerve and the sacral reflex arc can be measured, and its latency reflects the function of the peripheral pudendal nerve and the sacral reflex arc [25] (Fig. 2).
In previous studies, we have shown that neuropathy can be diagnosed in 65.9% of patients based on increased M-response latency. It is noteworthy that in 34.1% of patients, neuropathy was diagnosed only by impaired latency of late phenomena of the deep pudendal reflex and/or BCR [26]. It should be noted that testing for only the deep pudendal reflex does not provide information on the state of the afferent innervation of the pelvic floor muscles. Consequently, the BCR examination may be a promising method for assessing the activity of the pelvic floor muscles in connection with the possibility of determining neuro-reflex reactions. However, to date, the role of BCR in ENMG remains unclear regarding assessing the M-response latent period arising from the conduction of excitation along the distal parts of the pudendal nerve motor fibers for the diagnosis of pudendal neuropathy.
Based on the above consideration, the present study aimed to investigate the clinical value of testing BCR and the M-response during pudendal nerve stimulating ENMG in patients with pelvic organ prolapse and neurogenic pain syndrome.
Materials and methods
The study included 56 patients with pelvic organ prolapse and chronic neurogenic pelvic pain managed at the A.N. Ryzhikh National Medical Research Center of Coloproctology, Ministry of Health of Russia from 2019 to 2020. All participants gave written informed consent to take part in the study. The mean age of patients was 50.1 ± 11.6 years. The patients had pelvic organ prolapse in the form of rectocele [25/56 (44.6%)] and rectocele combined with internal rectal intussusception [31/56 (55.4%)].
All 56 women complained of pain localized to the anus or rectum, radiating to the coccyx, genital and perineal area, not associated with emptying. At the same time, 11/56 (19.6%) patients reported concurrent dyspareunia, and 10/56 (17.9%) patients complained of soreness, numbness, paresthesia in the external genital area, inner thigh, and perineum. Fecal incontinence and intestinal gas leakage were observed in 48/56 (85.7%) patients. Difficulty in bowel emptying and incomplete defecation were reported by 44/56 (78.6%) patients. Stress urinary incontinence and straining to continue urinating were observed in 16/56 (28.6%) and10/56 (17.9%) women, respectively. Therefore, according to the totality of clinical complaints, we had patients with pelvic prolapse and pudendal neuropathy.
Baseline clinical evaluation included physical examination, colonoscopy (to rule out organic pathology), defecography (to diagnose rectocele and internal rectal intussusception along with physical examination), neurophysiological examination in the form of stimulating ENMG to study the M response and BCR [27]. A urologist and gynecologist consulted all patients; findings of magnetic resonance imaging of the lumbosacral spine were obtained to rule out organic (not caused by pelvic organ prolapse) gynecological and urological pathology as well as neurosurgical diseases.
In a neurophysiological study, a standard stimulating ENMG was first performed to investigate the latent period of the M-response resulting from the conduction of potentials along the distal parts of the motor fibers of the pudendal nerve. Normally, pudendal nerve latency is 1.8–2.2 and 1.55–2.54 ms with the rectal and vaginal electrode positions, respectively [28, 29]. This method allows for identifying neuropathy in the distal part of the pudendal nerve. Next, the BCR was tested using a bridge electrode placed vertically over the clitoris. The normal values are 25–42 ms [19–22].
Statistical analysis
Statistical analysis was performed using Stata 14.2 (StataCorp) statistical software. The critical level of significance (p) was considered at 5%. Based on the normality of the data assessed by the Shapiro–Wilk test, quantitative variables were expressed as means (M) and standard deviation (SD). For scores (which cannot be considered normally distributed) on the VAS, Wexner, and rectal emptying scales, the median (Me) and the quartiles Q1 and Q3 in the Me (Q1; Q3) format were reported. Statistical significance of the differences between two indicators (BCR and M-response) was estimated by Fisher's exact test (since the expected frequencies in several cells were less than 5) using contingency tables. Correlation analysis was conducted by calculating Spearman's rank correlation coefficients (r), indicating the statistical significance of the result in the form of p. Comparing numerical data with non-normal distribution was performed with nonparametric Mann–Whitney tests.
Results
According to the questionnaire analysis, all patients had pain syndrome; the median score was 6.0 (4: 8) (VAS, maximum 10 points [30, 31]). All patients also complained of difficulties during bowel emptying [7.0 (5:10) points (Scoring system for disorders of colon emptying, maximum 22 points [32])]. Fecal incontinence (anal sphincter insufficiency (ASI) was reported by 48 (85.7%) patients, their score was 8.0 (2.25: 11.75) (Wexner scale, maximum 20 points [33]) Eight (14.3%) patients had no complaints of ASI (0 points on the Wexner scale).
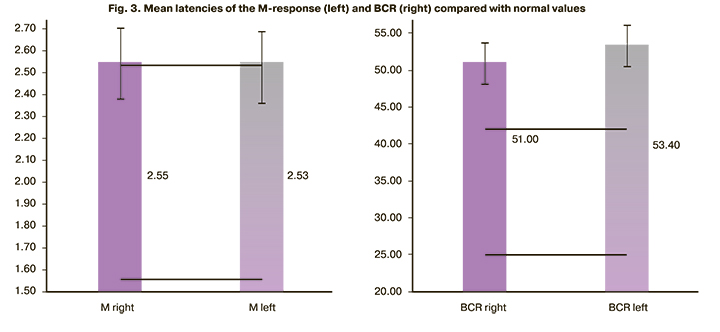
The M-response latency was normal on both sides in 19/56 (33.9%) patients (mean 2.03 (0.22) ms on the right and 2.01 (0.25) ms on the left). An increase in latency from at least one side was detected in 37/56 (66.1%) cases (mean 2.81 (0.60) ms on the right and 2.8 (0.61) ms on the left). At the same time, a simultaneous increase in latency on both sides was recorded in 16/37 (43.2%) women, only on one side in 21/37 (56.8%) patients. Based on an increase in the latency of the M-response from at least one side in patients with pelvic organ prolapse, pain syndrome, and dysfunction of the pelvic floor muscles (ASI) and/or obstructive defecation), we diagnosed the neuropathy of n. pudendus.
BCR was invoked in all of our observations. BCR latency within normal values on both sides was simultaneously observed only in 4 (7.1%) patients [(28.6 (4.0) ms on the right, 25.7 (3.9) ms on the left)] (table). BCR was increased at least on one side in 6 (10.7%) patients [up to 52.4 ms on the right in one, on average up to 54.3 (6.4) ms on the left in 5]. In the remaining 46 (82.2%) patients, BCR latency was increased on both sides up to 54.9 (6.4) ms on the right and 56.1 (4.9) ms on the left.
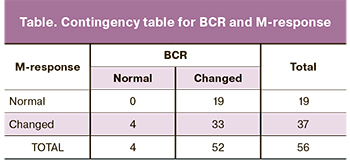
As shown in the table, there were no patients with normal BCR and M-response among the study participants. Thirty-three/56 (58.9%) patients had abnormal latency of both BCR and M-response, of which 13/33 (39.4%) patients had both responses changed on both sides. The contingency table analysis showed no significant relationship between BCR and M-response (Fisher's exact test = 0.287).
Latencies of M-response and BCR on the right and left sides are shown in Figure 3. The mean values of the M-response slightly exceed the normal values, while mean BCR values were significantly higher than the normal.
Among four patients with normal BCR, the latency of the M-response was from in 2 on the right and in 2 on the left (the values of the M-response were at the level of 2.7 on the left and 2.8 on the right). It should be noted that the age of the patients in most cases was over 50 years (above the sample mean), and the M-response usually increases with age [29].
Among 19 patients with normal M-response, BCR was abnormal, at least on one side. At the same time, they had a slightly higher VAS score: the median value was 7.0 (4: 8) versus 6.0 (4: 8), but the differences were not statistically significant (p=0.58).
The relationship between BCR latency and M-response was analyzed using Spearman's correlation coefficient (hereinafter referred to as r)
As expected, the M-response on the left and on the right were significantly correlated with r=0.32 (p=0.017); similarly, BCR values on the left and right correlate significantly with r=0.42 (p=0.001). We suggest that in case of abnormal latency violation, on the one hand, it is likely to be at least increased on the other hand.
However, there was no relationship between latencies of BCR and M-response. The BCR value on the left practically did not correlate with that of the M-response on the right with the correlation coefficient r=0.02 (0.91) and on the left r=-0.09 (0.52); BCR on the right had slightly higher, but statistically insignificant values, respectively: r=0.15 (p=0.27) and r= -0.14 (p=0.32).
The relationship between the M-response indicators presented as binary variables (1 – changed, 0 – normal) on the left and right and similar BCR binary variables on the left and right also were statistically non-significant (for all four combinations, p > 0.5).
There was no relationship between the M-response and BCR scores and the Wexner scale, VAS, and patient age. Correlation coefficients between the indicators of the M-response and the Wexner scale: 0.17 (p=0.21) on the right and 0.17 (p=0.22) on the left, for the VAS scale: -0.02 (p=0.91) on the right and 0.003 (p=0.98) on the left. Correlation coefficients for BCR and Wexner scale was 0.15 (p=0.26) on the right and -0.07 (p=0.61) on the left, for the VAS scale 0.14 (p=0.29) on the right and -0.17 (p=0.22) on the left. Correlation coefficients between the M-response and age was 0.16 (p=0.24) on the right and 0.08 (p=0.56) on the left, and BCR and age 0.14 (p=0.3) on the right and 0.03 (p=0.85) on the left. Patients with a normal M-response were statistically significantly (p=0.03) younger than patients with an impaired M-response [45.4 (2.58) versus 52.5 (1.84)] years. For BCR, no such differences were observed.
Therefore, no statistically significant relationship was found between the M-response and BCR scores.
Discussion
Findings of this study suggest that examination of pelvic floor muscle innervation requires testing for both M-response and BCR. In patients presenting with symptoms of pudendal neuropathy (neuralgia) and normal M-response, an additional examination is needed not only of late phenomena [26] but also BCR. We have shown that abnormal BCR is present in almost all patients with pelvic organ prolapse and neurogenic pelvic pain and maybe the only marker of impaired innervation.
An increase in the latency of the M-response was observed in 66.1% of patients with pelvic organ prolapse and neurogenic pelvic pain. In 33.9% of cases, the latency of the M-response remained normal. BCR was changed in 92.9% of patients. At the same time, all women with a normal M-response had abnormal BCR. On the other hand, in all cases of unchanged BCR, there was an increased latency of the M-response. Thus, examination of BCR and assessing the latent period of the M-response allows for identifying pudendal neuropathy in all patients with pelvic organ prolapse and neurogenic pelvic pain.
Conclusion
1. The latency of the M-response in patients with pelvic organ prolapse and neurogenic pelvic pain was impaired in 66.1% of patients.
2. Among patients with pelvic organ prolapse and complaints of neurogenic pelvic pain with normal M-response, 33.9% had abnormal BCR, which in the presence of clinical manifestations can be interpreted as a sign of pudendal neuropathy.
3. BCR latency was evoked in all cases and was changed in 92.9% of patients.
4. In 7.1% of cases of normal BCR latency, the M-response latency was changed.
References
- Пушкарь Д.Ю., Раснер П.И., Гвоздев М.Ю. Пролапс гениталий. РМЖ. 2013; 34: 11. [Pushkar D.Yu., Rasner P.I., Gvozdev M.Yu. Genital prolapse. Russian medical journal. 2013; 34: 11. (in Russian)]. https://my.clevelandclinic.org/health/diseases/14737-neuropathy
- Antolak S.J., Antolak C.M. Chronic pelvic pain: neurogenic or non-neurogenic? Warm detection threshold testing supports a diagnosis of pudendal neuropathy. Pain Physician. 2018; 21(2): E125-35.
- Извозчиков С.Б. Механизмы формирования и диагностика туннельных пудендонейропатий. Журнал неврологии и психиатрии им. С.С. Корсакова. 2019; 119(11): 98-102. [Izvozchikov S.B. Mechanisms of formation and diagnostics of tunnel pudendoneuropathies. Journal of neurology and psychiatry named after S.S. Korsakov. 2019; 119(11): 98-102. (in Russian)]. https://dx.doi.org/10.17116/jnevro201911911198.
- Коган М.И., Белоусов И.И., Шорников П.В. Нейрофизиологическая оценка пациентов с хроническим простатитом (синдром хронической тазовой боли III Б). Урология. 2012; 4: 37-43. [Kogan M.I., Belousov I.I., Shornikov P.V. Neurophysiologic evaluation of patients with chronic prostatitis (chronic pelvic pain syndrome III B). Urology. 2012; 4: 37-43 (in Russian)].
- Зайцев А.В., Шаров М.Н., Пушкарь Д.Ю., Ходырева Л.А., Дударева А.А. Хроническая тазовая боль. Методические рекомендации. М.: Издательский дом «АБВ-пресс»; 2016. [Zaitsev A.V., Sharov M.N., Pushkar D.Yu., Khodyreva L.A., Dudareva A.A. Chronic pelvic pain. Methodological recommendations. M.: Publishing house "ABV-press"; 2016. (in Russian)].
- Antolak S.J., Hough D.M., Spinner R.J. Anatomical basis of chronic pelvic pain syndrome: the ischial spine and pudendal nerve entrapment. Med. Hypotheses. 2002; 59: 349-53. https://dx.doi.org/10.1016/s0306-9877(02)00218-9.
- Insola A., Granata G., Padua L. Alcock canal syndrome due to obturator internus muscle fibrosis. Muscle Nerve. 2010; 42(3): 431-2. https://dx.doi.org/10.1002/mus.21735.
- Possover M. Laparoscopic management of endopelvic etiologies of pudendal pain in 134 consecutive patients. J. Urol. 2009; 181(4): 1732-6. https://dx.doi.org/10.1016/j.juro.2008.11.096.
- Itza Santos F., Salinas J., Zarza D., Gómez Sancha F., Allona Almagro A. Update in pudendal nerve entrapment syndrome: an approach anatomic-surgical, diagnostic and therapeutic. Actas Urol. Esp. 2010; 34(6): 500-9. https://dx.doi.org/10.1016/s2173-5786(10)70121-9.
- Ramsden C.E., McDaniel M.C., Harmon R.L., Renney K.M., Faure A. Pudendal nerve entrapment as source of intractable perineal pain. Am. J. Phys. Med. Rehabil. 2003. 82(6): 479-84. https://dx.doi.org/10.1097/00002060-200306000-00013.
- Durante J.A., Macintyre I.G. Pudendal nerve entrapment in an Ironman athlete: a case report. J. Can. Chiropr. Assoc. 2010; 54(4): 276-81.
- Filler A.G. Diagnosis and treatment of pudendal nerve entrapment syndrome subtypes: imaging, injections, and minimal access surgery. Neurosurg. Focus. 2009; 26(2): E9. https:/dx./doi.org/10.3171/FOC.2009.26.2.E9.
- Гусев Е.И., Коновалов А.Н., Скворцова В.И., Гехт А.Б., ред. Неврология. Национальное руководство. М.: ГЭОТАР-Медиа; 2018. . [Gusev E.I., Konovalov A.N., Skvortsova V.I., Gecht A.B., ed. Neurology. National leadership. M.: GEOTAR-Media, 2018; 880 p. (in Russian)].
- https://my.clevelandclinic.org/health/diseases/14737-neuropathy Ссылка активна на 27.07.2020.
- Stav K., Dwyer P.L., Roberts L. Pudendal neuralgia. Fact or fiction? Obstet. Gynecol. Surv. 2009; 64(3): 190-9. https://dx.doi.org/10.1097/ogx.0b013e318193324e.
- Labat J.J., Riant T., Robert R., Amarenco G., Lefaucheur J.P., Rigaud J. Diagnostic criteria for pudendal neuralgia by pudendal nerve entrapment (Nantes criteria). Neurourol. Urodyn. 2008; 27(4): 306-10. https://dx.doi.org/10.1002/nau.20505.
- Аполихина И.А., Миркин Я.Б., Эйзенах И.А., Малинина О.Ю., Бедретдинова Д.А. Тазовые дисфункции и болевые синдромы в практике уролога. Экспериментальная и клиническая урология. 2012; 2: 84-90. [Apolikhina I. A., Mirkin Ya. B., Eisenach I.A., Malinina O.Yu., Bedretdinova D.A. Pelvic dysfunctions and pain syndromes in the practice of a urologist. Experimental and clinical urology (Neurology). 2012; 2: 84-90. (in Russian)].
- Contreras Ortiz O., Bertotti A.C., Rodriguez Nuñez J.D. Pudendal reflexes in women with pelvic floor disorders. Zentralbl Gynakol. 1994; 116(10): 561-5.
- Contreras Ortiz O., Bertotti A.C., Rodríguez Núnez J.D. Deep pudendal reflex. Medicina (B Aires). 1994; 54(5, Pt 1): 407-10.
- Contreras Ortiz O., Bertotti A.C., Rodriguez Nuñez J.D. Female pelvic floor reflex responses. Int. Urogynecol. J. 1994; 5: 278-82. https:/dx./doi.org/10.1007/BF00376240.
- Contreras Ortiz O., Coya Nuñez F. Dynamic assessment of pelvic floor function in women using the intravaginal device test. Int. Urogynecol. J. Pelvic Floor Dysfunct. 1996; 7(6): 317-20. https://dx.doi.org/10.1007/BF01901106.
- Benson D.R., Keenan T.L. Evalution and treatment of trauma to the vertebral column. Ints. Course Lect. 1990; 39: 578.
- Шилкин В.В., Филимонов В.И. Анатомия по Пирогову (Атлас анатомии человека). т. 1. Верхняя конечность. Нижняя конечность. М.: ГЭОТАР-Медиа; 2011. 548с.
- Niu X., Shao B., Ni P., Wang X., Chen X., Zhu B. et al. Bulbocavernosus reflex and pudendal nerve somatosensory-evoked potentials responses in female patients with nerve system diseases. J. Clin. Neurophysiol. 2010; 27(3): 207-11. https://dx.doi.org/10.1097/WNP.0b013e3181dd4fca.
- Фоменко О.Ю., Ачкасов С.И., Краснопольский В.И., Мартынов М.Ю., Порядин Г.В., Попов А.А., Салмаси Ж.М., Белоусова С.В., Алешин Д.В., Козлов В.А., Федоров А.А., Некрасов М.А., Ефремова Е.С. Роль комплексного нейрофизиологического исследования в диагностике нейропатии полового нерва у пациенток с пролапсом тазовых органов и болевым синдромом. Акушерство и гинекология. 2020; 6: 72-9. [Fomenko O.Yu.,
- Achkasov S.I., Krasnopolsky V.I., Martynov M.Yu., Poryadin G.V., Popov A.A., et al. The role of complex neurophysiological research in the diagnosis of genital nerve neuropathy in patients with pelvic organ prolapse and pain syndrome. Akusherstvo i Ginekologiya. 2020; 6: 72-9. (in Russian)]. https://dx.doi.org/10.18565/aig.2020.6.72-79.
- Шелыгин Ю.А., Фоменко О.Ю., Николаев С.Г., Ачкасов С.И., Белоусова С.В., Мудров А.А., Алешин Д.В. Патент на изобретение «Способ определения нейрофизиологического состояния мышц тазового дна». Заявка № 2019129221/(057510) от 17.09.2019. https://yandex.ru/patents/doc/RU2708052C1_20191203 Ссылка активна на 27.07.2020. [Patent for an invention "Way of definition of a neurophysiological condition of muscles of a pelvic bottom", application No. 2019129221/(057510) of 17.09.2019. Authors: Shelygin Yu.A., Fomenko O.Yu., Nikolaev S.G., Achkasov S.I., Belousova S.V., Mudrov A.A., Aleshin D.V. https://yandex.ru/patents/doc/RU2708052C1_20191203 Active on 27.07.2020. (in Russian)].
- Jorge J.M., Wexner S.D., Ehrenpreis E.D., Nogueras J.J., Jagelman D.G. Does perineal descent correlate with pudendal neuropathy? Dis. Colon Rectum. 1993; 36(5): 475-83. https://dx.doi.org/10.1007/BF02050014.
- Olsen A.L., Ross M., Stansfield R.B., Kreiter C. Pelvic floor nerve conduction studies: establishing clinically relevant normative data. Am. J. Obstet. Gynecol. 2003; 189(4): 1114-9. https:/dx./doi.org/10.1067/S0002-9378(03)00551-9.
- Fall M., Baranowski A.P., Elneil S., Engeler D., Hughes J., Messelink E.J., Oberpenn F., de C. Williams A.C. Синдром хронической тазовой боли. Перевод Алымов Ю.В. Научное редактирование Коган М.И. Европейская ассоциация урологов; 2011. [Fall M., Baranowski A.P., Elneil S., Engeler D., Hughes J.J., Messelink E.J., Oberpenning F., de C. Williams A.C. Chronic freshness syndrome (transl.). M.I. Kogan, ed. European Association of Urology; 2011.]. (in Russian).
- Tan G., Jensen M.P., Thornby J.I., Shanti B.F. Validation of the brief pain inventory for chronic nonmalignant pain. J. Pain. 2004; 5(2): 133-7.
- Шелыгин Ю.А., Бирюков О.М., Титов А.Ю., Фоменко О.Ю., Мудров А.А. Существуют ли предикторы результатов хирургического лечения ректоцеле? Колопроктология. 2015; 1: 64-9. [Shelygin Yu.A., Biryukov O.M., Titov A.Yu., Fomenko O.Yu., etc. Are there predictors of the results of rectocele surgery? Сoloproctology. 2015; 1(51): 64-9. (in Russian)].
- Jorge J.M., Wexner S.D. Etiology and management of fecal incontinence. Dis. Colon Rectum. 1993; 36(1): 77-97. https:/dx.doi.org/10.1007/BF02050307.
Received 19.11.2020
Accepted 14.04.2021
About the Authors
Oksana Yu. Fomenko, MD, PhD, Associate Professor, Head of the Laboratory of Clinical Pathophysiology, Ryzhikh National Medical Research Centre for Coloproctology, Ministry of Health of Russia. Tel.: +7(916)481-73-27. E-mail: oksana671@yandex.ru. ORCID: 0000-0001-9603-6988; Scopus Author ID: 16401538300.123423, Russia, Moscow, Salama Adilya str., 2.
Gennady V. Poryadin, Corresponding Member of the RAS, MD, PhD, Professor of the Department of Pathophysiology and Clinical Pathophysiology, Honorary Professor of Pirogov Russian National Research Medical University, Ministry of Health of Russia. Tel.: +7(495)434-14-22. E-mail: rsmu@rsmu.ru. ORCID: 0000-0003-2010-3296;
Scopus AuthorID: 55985271400. 117997, Russia, Moscow, Ostrovityanov str., 1.
Mikhail Yu. Martynov, Corresponding Member of the RAS, MD, PhD, Professor of the Department of Neurology, Neurosurgery and Medical Genetics, Pirogov Russian National Research Medical University, Ministry of Health of Russia. Tel.: +7(495)434-14-22. E-mail: rsmu@rsmu.ru. ORCID: 0000-0003-2797-7877.
117997, Russia, Moscow, Ostrovityanov str., 1.
Vladimir N. Kashnikov, MD, PhD, Deputy Director for scientific and medical work, Ryzhikh National Medical Research Centre for Coloproctology, Ministry of Health of Russia. ORCID: 0000-0002-5385-7898. 123423, Russia, Moscow, Salama Adilya str., 2.
Andrey S. Shkoda, MD, PhD, Professor, Head of L.A.Vorokhobov City Hospital No 67, Moscow Health Department. ORCID: 0000-0002-9783-1796.
123423, Russia, Moscow, Salama Adilya str., 2/44.
Vladimir A. Kozlov, Associate Professor, PhD in economics, Researcher, Ryzhikh National Medical Research Centre for Coloproctology, Ministry of Health of Russia
ORCID: 0000-0003-1788-1484; Scopus Author ID: 55429890300. 123423, Russia, Moscow, Salama Adilya str., 2.
Svetlana V. Belousova, MD, Senior Researcher of the Laboratory of Clinical Pathophysiology, Ryzhikh National Medical Research Centre for Coloproctology,
Ministry of Health of Russia. ORCID: 0000-0003-1475-2599. 123423, Russia, Moscow, Salama Adilya str., 2.
Alexander S. Rumiantsev, traumatologist-orthopedist of L.A. Vorokhobov City Clinical Hospital No 67, Moscow Health Department. ORCID: 0000-0002-1548-5456.
123423, Russia, Moscow, Salama Adilya str., 2/44.
Sergey I. Achkasov, MD, PhD, Professor, Head of the Department of Oncology and Colon Surgery, Ryzhikh National Medical Research Centre for Coloproctology,
Ministry of Health of Russia. ORCID: 0000-0001-9294-5447. 123423, Russia, Moscow, Salama Adilya str., 2.
For citation: Fomenko O.Yu., Poryadin G.V., Martynov M.Yu., Kashnikov V.N., Shkoda A.S., Kozlov V.A., Belousova S.V., Rumyantsev A.S., Achkasov S.I. The role of bulbocavernosus reflex in the diagnosis of neuropathy in patients with pelvic organ prolapse and pelvic pain syndrome.
Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2021; 5: 121-127 (in Russian)
https://dx.doi.org/10.18565/aig.2021.5.121-127



