Тазовое дно представляет собой совокупность мягких тканей (мышц, фасций и связок), которые занимают нижнюю апертуру таза, составляя опорную конструкцию, и обеспечивают нормальное положение органов малого таза: прямой кишки, мочевого пузыря, мочевыводящего канала, а также влагалища и матки у женщин [1].
Повреждения опорных структур тазового дна могут способствовать возникновению дисфункции тазового дна.
Дисфункция тазового дна - это комплекс нарушений функции мышц тазового дна и связочного аппарата, который приводит к нарушению работы и опущению/выпадению (пролапсу) органов малого таза.
Клиническими проявлениями дисфункции тазового дна могут быть: стрессовое недержание мочи, синдром хронической тазовой боли, сексуальная дисфункция, формирование кубитальных язв, инфекционные осложнения и др. Наличие дисфункции тазового дна существенно снижает качество жизни женщины, приводит к развитию психоэмоциональных расстройств, социальной изоляции и т.д.
По данным клиники Mayo, 33% всех женщин страдают опущением органов малого таза и недер-жанием мочи в разные периоды своей жизни. Распространенность пролапса гениталий увеличива-ется с возрастом. Согласно демографическим пока-зателям, отмечено увеличение продолжительности жизни женщины, в том числе длительности периода менопаузы у женского населения, ассоциированного со снижением уровня эстрогенов и ухудшением качества соединительной ткани, что способствует форми-рованию дисфункции тазового дна. Следовательно, выпадение гениталий становится все более распро-страненным явлением. Высказываются предположения, что в ближайшие 30 лет частота пролапса гениталий удвоится [2-4]. В настоящее время проблема пролапса гениталий названа «скрытой эпидемией».
Общепринятой в мире является современная кли-ническая классификация пролапса тазовых органов POP-Q (Pelvic Organ Prolapse Quantification).
Принцип стадирования пролапса тазовых органов, согласно системе POP-Q, заключается в определении выраженности опущения с помощью измерения стан-дартных точек, обозначающих положение и размеры структур тазового дна. Точки, расположенные выше границы половой щели, обозначаются знаком «-» (минус), а точки, расположенные ниже, - знаком «+» (плюс). Все измерения осуществляются в сантиметрах.
Исследование выполняется на высоте пробы Вальсальвы. В случае ношения пессария исследование производится не ранее чем через сутки после его удаления. Исследование должно проводиться сначала с наполненным мочевым пузырем (для исключения оккультного недержания мочи), затем - после опорожнения (для исключения ложноотрицательных показателей).
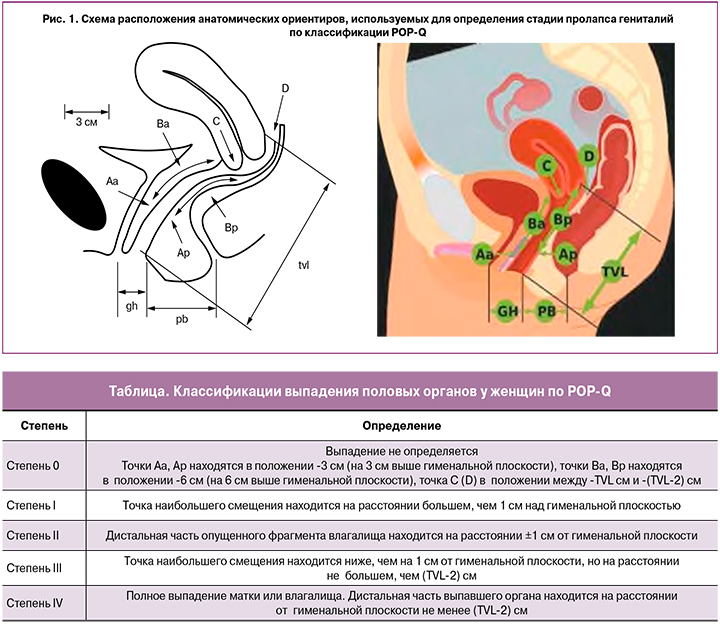
Количественная оценка степени пролапса гениталий основана на измерении 9 параметров (рис. 1):
- Aa - точка на передней стенке влагалища на 3 см проксимальнее гименального кольца;
- Ba - наиболее низко расположенная точка на участке передней стенки влагалища между точками Аа и С;
- C - передняя губа шейки матки (или купол влага-лища);
- Ap - точка на задней стенке влагалища на 3 см проксимальнее гименального кольца;
- Bp - наиболее низко расположенная точка на задней стенке влагалища между точками Ap и D;
- D - задний свод (после гистерэктомии - отсутствует);
- Gh - расстояние от наружного отверстия уретры до заднего края гимена;
- Pb - расстояние между задним краем гимена и анальным отверстием (промежность);
- TVL — расстояние между краем гимена и куполом влагалища (длина влагалища).
Упрощенная схема классификации выпадения половых органов у женщин по POP-Q приведена в таблице.
К развитию дисфункции тазового дна может приво-дить сочетанное воздействие различных факторов. По мнению большинства исследователей, повреждение тазового дна в ходе осложненных влагалищных родов, в том числе травма мышцы, поднимающей задний проход (m. levator ani), является ведущим фактором в формировании дисфункции тазового дна. Согласно статистическим данным, повреждение m. levator ani происходит в 15—30% случаев (20% после первых родов). Травма m. levator ani является основным фак-тором, способствующим патофизиологии пролапса гениталий. Наиболее высокий риск развития дис-функции тазового дна обнаружен у пациенток с дву-сторонним отрывом m. levator ani; при одностороннем отрыве вероятность патологических изменений ниже.
Кроме того, выявлены прямая зависимость между степенью повреждения мышц и степенью опущения, а также более высокий риск рецидива пролапса [5, 6].
При повреждении мышц в ходе естественных родов возможна денервация тазового дна, которая может приводить к нарушению сократительной способности поперечно-полосатой мускулатуры тазового дна, а также к заторможенности нервной релаксации гладкой мускулатуры уретры, мочевого пузыря и т.д. с последующим формированием гиперактивного моче-вого пузыря, ургентной инконтиненции.
Кроме того, отягощенный наследственный анамнез пролапса гениталий с наличием синдрома дисплазии соединительной ткани являются факторами риска развития дисфункции тазового дна.
Основным методом лечения пролапса гениталий в настоящее время является хирургическая коррекция. Однако возможность рецидива состояния после проведенного лечения не исключена. Самая высокая частота рецидивов отмечена после оперативного лечения пролапса гениталий в переднем компартменте таза.
Выделяют следующие причины неэффективности оперативного лечения при пролапсе гениталий:
- нет четкого стандарта обследования и унифици-рованных технологий для диагностики данного состояния;
- в ряде случаев отсутствует возможность приме-нения персонализированного подхода с учетом индивидуальных особенностей пациентки;
- отсутствуют комплексный подход к проблеме и преемственность послеоперационных реабили-тационных мер;
- редко практикуется предоперационная диагно-стика «скрытого» недержания мочи при выра-женном опущении органов малого таза; таким образом, зачастую после оперативного лечения у женщины проявляется недержание мочи;
- нет золотого стандарта оперативного лечения пролапса.
В последние годы изменился хирургический подход к коррекции пролапсов: ранее в качестве «стандарта» широко применялись сетчатые импланты, которые поддерживали как каркас переднюю или заднюю стенку влагалища. Накопленный опыт и анализ данных периода наблюдения пациентов после операций с применением сетчатых имплантов показали большое количество осложнений (эрозии, язвы, смещение сеток, и др.), в связи с чем современная урогинекология ставит под сомнение применение сетчатых имплантов при опущении, заменяя их пластикой собственными тканями пациента, а FDA (Food and Drug Administration) предупреждает о приостановлении и снятии с производства некоторых видов таких имплантов.
Поэтому выбор вида операции должен проводиться после комплексного подхода в оценке состояния тазового дна, которое включает такие методы, как:
- анкетирование пациентки и подробный сбор анамнеза;
- визуальная оценка состояния тазового дна при осмотре на гинекологическом кресле;
- применение пробы Вальсальвы (пробы с натужи- ванием);
- пальцевое исследование — эффективный и про-стой метод выявления надрыва и отрыва m. levator ani.
Трансперинеальное и трансвагинальное ультраз-вуковое исследование (УЗИ) в режиме визуализации 2D позволяет определить и дифференцировать не только макротравмы (отрыв) m. levator ani, но и микротравмы (перерастяжение). Режимы визуализации 3D/4D применяются для объемной реконструкции всех структур тазового дна.
Магнитно-резонансная томография (МРТ) при-меняется с 1990-х гг. Метод способствует иден-тифицированию всех мышц тазового дна; однако МРТ имеет ограниченное клиническое применение при оценке дисфункции тазового дна из-за высокой стоимости и сложности доступа.
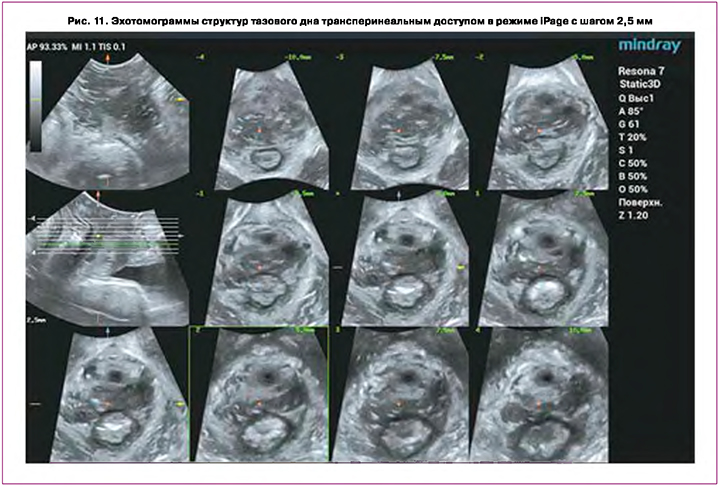
В связи с усовершенствованием трехмерных уль-тразвуковых технологий, объемная эхография стала новым инструментом в диагностике состояния тазового дна. Визуализация в режиме 3D позволяет определить осевую плоскость с хорошим пространственным и временным разрешением. Мультислайс технология (режим томографических срезов), подобно МРТ способствует послойной оценке всех структур и дифференцировке микротравм мышц тазового дна.
Объемная эхография демонстрирует ряд преиму-ществ при исследовании тазового дна:
- доступность в клинической практике;
- простой доступ для исследования зоны интереса;
- возможность применения метода во время беременности и в родах, что особенно актуально в настоящее время в связи с развитием предиктив-ного акушерства и дает возможность врачу оценить сокращение мышц тазового дна во время схватки и вовремя предотвратить разрыв про-межности.
В ультразвуковой диагностике дисфункции тазового дна важное значение имеет стандартизация технологии, операционных систем оборудования и автоматизация измерений при проведении исследо-вания.
Производители ультразвуковых сканеров предла-гают современные технологии для оценки состояния тазового дна. В НМИЦ АГиП им. В.И. Кулакова применяется современная ультразвуковая система Resona 7 (Mindray), позволяющая выполнять весь спектр технологий мультипараметрической эхографии, включая разметку и измерения в полуавтоматическом режиме с помощью опции Smart Pelvic Floor.
Технология Smart Pelvic Floor
Функция Smart Pelvic реализуется при гине-кологических исследованиях с помощью транс-вагинального (внутриполостного 3D/4D) DE10- 3WU с частотой 3—9 МГц и трансперинеального (конвексного) датчика объемного сканирования D8-4U с использованием диапазона частот 2,3— 6,8 МГц или 2-й гармоники на частоте 5 МГц (Н5) (рис. 2).

Сканирование тазового дна проводится в положении пациентки лежа на спине, ноги согнуты в коленных суставах. Исследование может быть выполнено в любой день менструального цикла.
Алгоритм исследования тазового дна.
1. Определяется максимальный обзор в 2D-режиме при умеренно наполненном мочевом пузыре (угол обзора 90°, при низкой частоте и высоком разре-шении).
2. Выстраивается плоскость минимальных размеров отверстия промежности — линия, соединяющая точки нижнего края лобкового симфиза и аноректального угла.
3. Объемная реконструкция с применением тех-нологии Smart Pelvic Floor.
При трансвагинальном доступе датчик устанав-ливается в нижней трети влагалища. Референсная линия проходит через центральную часть лобковой кости под углом 135° к центральной оси лобкового сочленения через его задний нижний край.
На первом этапе получается 2D изображение, и с помощью опции Smart Pelvic в полуавтоматическом режиме выстраивается система координат по точкам: S — нижняя часть лобкового симфиза, Р — верхняя часть лобкового симфиза, SP — лобковый симфиз, U — шейка мочевого пузыря, Е — проксимальная часть уретры, R — задняя стенка мочевого пузыря, наиболее близко расположенная к уретре, V — нижняя часть задней стенки мочевого пузыря (рис. 3А), позволяющая получить расчеты следующих показателей:
- BSD — расстояние между шейкой мочевого пузыря и симфизом;
- PVA — лонно-пузырный угол;
- PUA — лонно-уретральный угол;
- RVA — позадипузырный угол;
- BND — опущение задней стенки мочевого пузыря;
- UTA — угол наклона уретры;
- URA - угол поворота уретры.
Первые измерения проводятся в состоянии покоя, затем следуют измерения с пробой Вальсальвы (при натуживании). Некоторые авторы рекомендуют производить измерения во время проведения пробы Вальсальвы троекратно и указывать среднее значение показателей (рис. 3В). У 21- 40% женщин молодого возраста проведение пробы Вальсальвы может сопровождаться ко-активацией мышц-леваторов - показатель гипертонуса мышц тазового дна, являющийся признаком риска их разрыва и повреждения в родах, т.к. при ко-активации проис-ходит уменьшение площади отверстия промежности и удлинение второго периода родов.
При проведении функциональных проб для диаг-ностики стрессового недержания мочи может визу-ализироваться гипермобильность уретры. При этом показатели PVA, RVA и PUA будут отклонены более чем на 20°.
Определение анатомической длины уретры про-водится в покое и с пробой Вальсальвы. В норме этот показатель может варьировать в пределах от 30 до 42 мм. Кроме того, при гипермобильности уретры может определяться расширение проксимального и среднего отдела уретры в покое и при натуживании.
При трансперинеальном доступе датчик уста-навливается на область промежности вертикально на уровне преддверия влагалища. Референсная линия проходит через центральную часть лобковой кости под углом 90° к центральной оси лобкового сочленения через его задний нижний край (рис. 4).

Трансперинеальное исследование проводится при невозможности использования трансвагинального датчика: наличии девственной плевы, синехий влагалища и вульвы, рубцовой деформации промежности. Выполняется серия параллельных поперечных сканов от уровня анального отверстия по направлению к шейке матки. Сагиттальный срез поможет визуализировать гипермобильность уретры, цистоцеле и ректоцеле, обструкцию при дефекации. Повернув датчик в поперечную плоскость, можно оценить ротацию мочеиспускательного канала и травмы сфинктера, мышцы тазового дна.
Исследование проводят дважды: в покое и с пробой Вальсальвы (рис. 5); на первом этапе — в 2О-режиме, затем — реконструкция тазового дна в ЗО-режиме.
УЗИ тазового дна в режиме 3D с функцией Smart Pelvic
ЗО-визуализация позволяет получить мультипла- новый обзор — сагиттальный срез, перпендикулярный и коронарный (рис. 6).

На первом этапе выполняется получение ЗП-изображения, далее производятся измерения с помощью опции Smart Pelvic в полуавтоматическом режиме (рис. 7, 8).
После получения реконструкции и выбора текущего изображения проводят измерения: U — центральная точка уретры; Bottom — нижняя граница измерения — передняя граница пубо-ректальной мышцы.
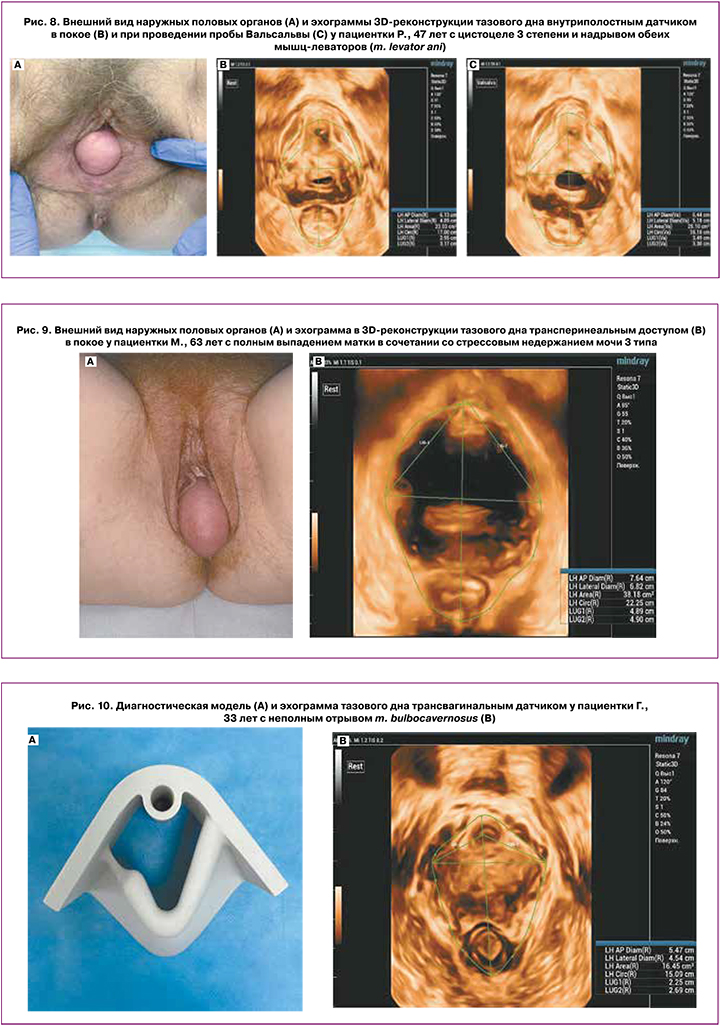
После этого будут автоматически вычислены такие размеры, как levator hiatus (LH) — перед-незадний/боковой диаметр, окружность/площадь levator hiatus, LUG — расстояние между уретрой и т. bulbocavernosus (рис. 9). В норме расстояние между леватором и уретрой — менее 25 мм. Доступно автоматическое определение levator hiatal area при трехмерном сканировании (в норме — менее 25 см2) с возможностью ручной корректировки.
Таким образом, объемная эхография тазового дна является объективным и надежным инструментом оценки функции тазового дна, позволяющим:
- оценить ко-активацию т. levator ani и риск их повреждения;
- оценить мобильность уретры при проведении функциональных проб, состояние сфинктера уретры;
- выдерживать время пробы Вальсальвы не менее 10 секунд, что комфортнее для пациентки в срав-нении с МРТ; при этом проба Вальсальвы стан-дартизируется по времени, а не по давлению натуживания;
- диагностировать образования уретры;
- проводить дифференциальную диагностику сте-пени и типов пролапса, имеющих важное значение в планировании вида оперативного лечения;
- идентифицировать слинги и сетчатые импланты [7-9];
- диагностировать отрыв/разрыв т. levator ani (рис. 10) [10, 11].
Технология Smart Pelvic Floor - автоматизированная функция для исследования переднего ком- партмента таза и т. levator ani. Преимуществами УЗИ тазового дна с применением опции Smart Pelvic Floor являются:
- неинвазивность методики;
- не требует специальной подготовки пациента,
- позволяет нивелировать риск оператор-зависи- мых ошибок и объективизировать полученные данные,
- стандартизация координат измерений, в том числе в режиме iPage (томографическом), для пошагового исследования всех отделов компартмента (рис. 11).
- быстрота получения результата — полуавто-матическое построение линий измерений в 3 раза быстрее позволяет проводить исследование в двухмерном режиме, а сканирование в 3 D-режиме быстрее и эффективнее в 5 раз за счет автоматической трассировки.
Заключение
Дисфункция тазового дна у женщин охватывает ряд распространенных состояний и включает выпадение тазовых органов, недержание мочи и кала, затрудненную дефекацию и сексуальную дисфункцию. В большинстве случаев этиология и патофизиология этих состояний до конца не изучены. Увеличение продолжительности жизни, важность профилактики в более молодом возрасте и роль дисфункции тазового дна не только в постменопаузе, но и в репродуктивном возрасте подчеркивают важность оценки состояния тазового дна.
Из доступных методов диагностики, таких как рентген, компьютерная томография, МРТ и эхография, последний, безусловно, имеет преимущество для визуализации тазового дна. Этот метод безопасен, прост, дешев, легкодоступен и обеспечивает высокое пространственное и временное разрешение.
Метод ультразвуковой визуализации стал важным инструментом для своевременной диагностики дисфункции тазового дна
Внедрение современных ультразвуковых техно-логий, таких как Smart Pelvic Floor для объемной реконструкции тазового дна у женщин и автома-тического анализа результата, позволяет нивелировать риск оператор-зависимых ошибок, объективизировать полученные данные. Это значит, что создаются возможности для стандартизации подобных исследований.
Широкое применение ультразвуковой визуализации может изменить подходы к методам лечения заболеваний тазового дна, таких, как недержание мочи, газов и кала, выпадение тазовых органов и связанных с этим состояний.