Anatomical and functional characteristics of the pelvic floor in women of various age groups
Bezmenko A.A., Zakharov I.S., Bezhenar V.F., Staroverova A.S., Bagramyan E.A., Ivanova O.A., Kapitanova M.V.
Objective: To evaluate the anatomical and functional characteristics of the pelvic floor in women of different age groups.
Materials and methods: This study was conducted at the Military Medical Academy and included 1,546 women who were divided into three age groups. Anatomical characteristics were assessed using the POP-Q system and transperineal ultrasound examinations. Functional characteristics were analyzed with the PERFECT system, and the PFDI-20 and SF-36 questionnaires were utilized. In addition, the Female Sexual Function Index was evaluated.
Results: The study revealed that women in the second group experienced age-related shifts in the locations of points Aa and Ba, along with a statistically significant increase in the angle of urethral inclination and bladder neck displacement (p=0.01). Women in group 3 showed a significant decrease in strength, endurance, and muscle contractions (p=0.001). The PFDI-20 questionnaire results indicated an increase in the severity of pelvic dysfunction symptoms, rising from 9.4 points in group 1 to 144.8 points in group 3 (p=0.001). The increase in prolapse symptoms and severity of pelvic dysfunction correlated with a decrease in both the physical (ρ=-0.56, p=0.001) and psychological components of health (ρ=-0.60, p=0.001).
Conclusion: This study demonstrated that anatomical and functional changes in most women begin long before menopause onset. The data obtained can be used to develop individualized prevention and treatment measures.
Authors’ contributions: Bezmenko A.A., Zakharov I.S., Bezhenar V.F. – conception and design of the study, data analysis and interpretation, drafting and final approval of the manuscript; Bezmenko A.A., Zakharov I.S., Staroverova A.S., Bagramyan E.A., Ivanova O.A., Kapitanova M.V. – data collection and processing, data analysis and interpretation, drafting of the manuscript.
All authors read and approved the final version before submission.
Conflicts of interest: The authors have no conflicts of interest to declare.
Funding: There was no funding for this study.
Ethical Approval: The study was reviewed and approved by the Research Ethics Committee of the 1S.M. Kirov Military Medical Academy.
Patient Consent for Publication: All patients provided informed consent for the publication of their data.
Authors' Data Sharing Statement: The data supporting the findings of this study are available upon request from the corresponding author after approval from the principal investigator.
For citation: Bezmenko A.A., Zakharov I.S., Bezhenar V.F., Staroverova A.S., Bagramyan E.A., Ivanova O.A., Kapitanova M.V. Anatomical and functional characteristics of the pelvic floor in women of various age groups.
Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2025; (6): 131-138 (in Russian)
https://dx.doi.org/10.18565/aig.2025.101
Keywords
Pelvic organ prolapse (POP) is a significant issue in modern gynecology, affecting approximately 30% of the general population. Its prevalence increases with age, exceeding 40% by the age of 65–70, suggesting a connection between POP and age-related changes [1–4]. It is important to note that POP prevalence rates can vary based on the diagnostic methods employed; for instance, a physical examination indicates a higher incidence rate (41.8%) than a questionnaire (25.0%) [5]. Given the aging population, some experts predict an increase in the number of POP patients, which will inevitably place additional strain on the healthcare system [2, 6, 7].
Although POP is more common among the elderly, the influence of predisposing factors on the development of this condition can manifest long before the appearance of clinical symptoms. In contrast to POP, pelvic floor dysfunction can be diagnosed at a younger age, often because of factors such as genetic predisposition, chronic diseases, obstetric injuries, and gynecological surgeries [8–10]. Understanding the role of these factors in POP pathogenesis requires further investigation. Modern studies highlight a lack of knowledge regarding the dynamics of anatomical and functional changes in the pelvic floor throughout the different stages of a woman’s life. The existing conceptual model illustrates how age, vaginal delivery, and high parity affect the morphology of the pelvic floor, underscoring the complexity and multidimensional nature of these processes [11]. Yuan G. (2011) observes that vaginal delivery results in more significant structural changes compared to a planned cesarean section; however, even cesarean sections do not guarantee complete protection against the development of POP and related dysfunctions [12]. This underscores the need for further research into the mechanisms underlying pelvic floor pathology and the dynamic relationship between pelvic floor anatomy and function throughout a woman's life.
The insufficient study of age-related changes in pelvic floor pathology and lack of comprehensive research in this field highlight the need for an in-depth analysis of these changes from anatomical and functional perspectives. Such analysis will enhance our understanding of the mechanisms behind pelvic dysfunction and genital prolapse at various stages of a woman’s life.
This study aimed to evaluate the anatomical and functional characteristics of the pelvic floor in women of different age groups.
Materials and methods
This cross-sectional study involved 1,546 women from various age groups and was conducted at the Obstetrics and Gynecology Clinic of the Military Medical Academy. Participants were categorized into three age groups: group 1 included patients aged 18–35 years (n=519), group 2 included patients aged 36–50 years (n=532), and group 3 included patients aged 51 years and older (n=495).
Inclusion criteria for the study were age 18 years and older, Caucasian race, and signed informed consent to participate. Exclusion criteria included age under 18 years, pregnancy at the time of the study, women whose pregnancy ended less than 24 months prior, history of surgical treatment for gynecological diseases, malformations of the genitals, presence of acute gynecological diseases at the time of the study, absence of signed informed consent, and any patient refusal to participate at any stage.
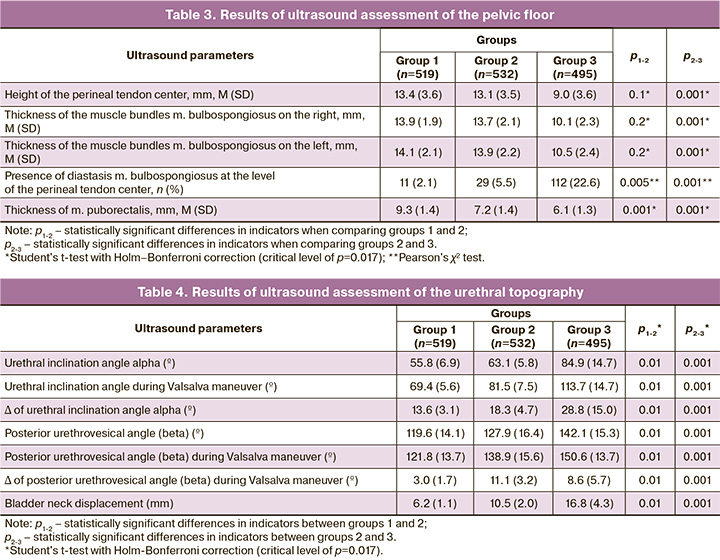
The anatomical characteristics of the pelvic floor were assessed using the Pelvic Organ Prolapse Quantification System (POP-Q, 1996), a standardized method developed by the International Continence Society (ICS) and the International Urogynecology Association (IUGA) [13]. Ultrasound evaluation of the pelvic floor was performed using a Mindray DC-8 ultrasound machine equipped with a convex probe operating at a frequency of 4–8 MHz. The bladder was filled to a volume of 150–200 ml and monitored using transabdominal ultrasound. Patients were placed in the lithotomy position to facilitate optimal access during the study, which was conducted in the sagittal plane with the pubic symphysis serving as a fixed anatomical landmark. The following parameters were measured: the anterior urethral angle (α), defined as the angle between the axis of the proximal urethra and the longitudinal axis of the pubic symphysis; the posterior urethrovesical angle (β), measured between the axis of the proximal urethra and the posterior wall of the bladder; and the displacement of the neck of the bladder relative to the pubis during the Valsalva maneuver, quantified as the distance from the neck of the bladder to a horizontal line drawn through the distal edge of the pubic symphysis. The rotation angles (Rα and Rβ) were calculated as the difference between the angles at rest and during straining. The Valsalva maneuver was performed after patients received preliminary training using the correct technique. Dynamic changes were recorded in the cine-loop mode to enhance the accuracy of the analysis. Additionally, measurements were taken of the height of the tendinous center of the perineum (mm), the thickness of the bulbospongiosus muscle (mm), and the thickness of the puborectalis muscle (mm) to comprehensively assess the condition of the pelvic floor muscles [14].
All ultrasound measurements were conducted by highly qualified specialists with extensive experience in urogynaecological diagnostics. To eliminate bias, the operators were not provided access to clinical information about the patients. Consequently, all studies were conducted in a blinded manner, ensuring objective assessment of ultrasound parameters. The functional characteristics of the pelvic floor were evaluated using the PERFECT system, which measures key parameters of pelvic floor muscle contractility, including strength (P), endurance (E), number of repetitions (R), rapid contractions (F), and counting each contraction (ECT). The technique developed by Laycock D. and Jerowod D. was chosen for its simplicity, noninvasiveness, and ease of use in clinical practice. The reliability and validity of the system have been confirmed by numerous studies demonstrating a high correlation between the results obtained using this system and objective measurement methods such as perineometry, indicating the reproducibility of the technique for objectively assessing the functional state of the pelvic floor muscles [15].
Additionally, diagnoses of POP and bladder and bowel dysfunction were assessed using the Pelvic Floor Distress Inventory Questionnaire (PFDI-20). The Female Sexual Function Index (FSFI) and quality of life (SF-36) were assessed.
Statistical analysis
Statistical analysis was conducted using the StatSoft Statistica 12. The normality of distribution was assessed using the Kolmogorov–Smirnov criterion with the Lilliefors correction. Continuous variables with normal distribution are presented as arithmetic means (M) and standard deviations (SD); for non-normally distributed samples, medians (Me) and interquartile ranges [Q1; Q3] are reported. Student’s t-test was used to compare the mean values between two samples; for three or more groups, analysis of variance (ANOVA) was employed, along with the Holm-Bonferroni method for multiple comparisons. Non-normally distributed variables were compared using the non-parametric Mann–Whitney test. For three or more independent groups, the nonparametric Kruskal–Wallis H-test was applied. Categorical variables were reported as counts and proportions (%) and compared using the Pearson χ² test. Correlation analysis was conducted by calculating Spearman's rank correlation coefficients (ρ), with strength assessed using the Chaddock scale: 0.1–0.3 – weak correlation; 0.3–0.5 – moderate correlation; 0.5–0.7 – noticeable correlation; 0.7–0.9 –strong correlation; and 0.9–0.99 – very strong correlation.
Results and discussion
Clinical and demographic characteristics were collected and analyzed as part of the cross-sectional study (Table 1).
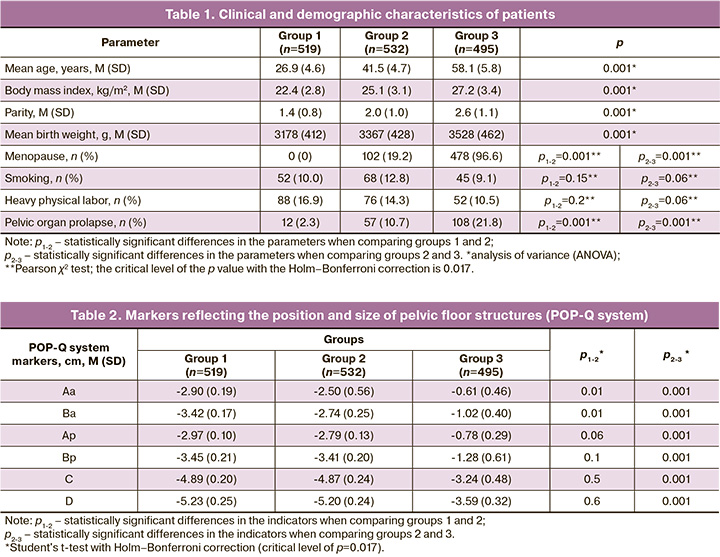
The assessment of the anatomical characteristics reflecting the position and size of the pelvic floor structures using the POP quantitative assessment system (POP-Q) yielded the following results (Table 2).
The data presented show that an age-related shift in the localization of points Aa and Ba towards the vaginal entrance was already noted in women of group 2, with this trend continuing in those examined in group 3. At the same time, no statistically significant differences in the location of points Ap, Bp, C, and D were found in patients in groups 1 and 2. Comparative evaluation of the specified topographic markers of POP in groups 2 and 3 revealed a significant shift towards hymen in women in group 3.
Along with clinical verification of anatomical features in women of different age groups, an ultrasound assessment of the pelvic floor was performed (Tables 3 and 4).
The results of transperineal ultrasound examination demonstrate that women of groups 1 and 2 do not have statistically significant differences in the height of the perineal tendon center – 13.4 (3.6) mm and 13.1 (3.5) mm, respectively, and the thickness of m. bulbospongiosus (p=0.1). However, in women of the late reproductive period, diastasis of m. bulbospongiosus was more often recorded – 29/532 (5.5%) and a decrease in the thickness of m. puborectalis – 7.2 (1.4) mm, as initial manifestations of age-related changes. In women of the 3rd group, ultrasound markers (height of the perineal tendon center – 9.0 (3.6) mm, thickness of m. puborectalis – 6.1 (1.3) mm, frequency of diastasis of m. bulbospongiosus – 22.6%) statistically significantly differed from similar indicators in patients of the 1st and 2nd groups (p=0.001), which emphasizes more pronounced structural changes in the pelvic floor. These data confirm the results of the study by Asfour V. et al. (2020), where the height of the perineal tendon center in prolapse was 16.9 (8.7) mm, and the area was less than 2.4 cm², which is associated with the loss of its supporting function [16]. Zhou M. et al. (2023) noted that the thickness of the perineal tendon center changes under the influence of increased abdominal pressure [17]. According to Chechneva M.A. (2016), an unchanged pelvic floor is characterized by a height of the perineal tendon center of at least 1.0 cm, a width of the muscle bundles of m. bulbospongiosus from 1.0 to 1.5 cm, the absence of diastasis of m. bulbospongiosus in the area of the tendon center and a thickness of the puborectalis muscle of at least 7 mm [14]. These indicators correlated with our observations, which showed a significant decrease in these parameters in patients in the 3rd group.
Ultrasound assessment of urethral topography confirmed the significant influence of age on the parameters associated with mobility of the anatomical structures of the pelvic floor. Our study revealed that women in Group 2 showed significant changes in angle α (Δ inclination angle α = 18.3 (4.7)°; in Group 3, angles α and β demonstrated more pronounced changes: Δ angle α was 28.8 (15.0°), and angle β during the Valsalva maneuver increased to 150.6 (13.7°) (Fig. 1).
Similar data are presented in the work of Al-Saadi W.I., where the angle α in women with stress urinary incontinence (SUI) increased from 58° at rest to 83° during straining, while in the control group, it changed less significantly. Angle β in patients with POP reached 153° during the Valsalva maneuver, which significantly exceeded the values in the control group [18]. Such changes indicate a loss of support for the urethrovesical junction, which was confirmed by an increase in the displacement of the bladder neck. The displacement of the bladder neck in the 2nd group was 10.5 (2.0) mm, and in the 3rd group it reached 16.8 (4.3) mm. According to Turkoglu A. (2020), the threshold value for the development of SUI is a displacement of the bladder neck relative to the pubis of more than 11.2 mm [19], in contrast to the study of Naranjo-Ortiz C. et al. (2016), which proposed a threshold of 25 mm [20]. Additionally, Hajebrahimi S. et al. (2009), 15.6 mm is indicated as the threshold value for bladder neck displacement [21]. Thus, an increase in bladder neck displacement, comparable to changes in the α and β angles, confirms the relationship between anatomical changes and clinical manifestations and the importance of their comprehensive assessment. At the same time, the presented data indicate the absence of universal normative values for the α and β angles as well as for the magnitude of bladder neck displacement, which is associated with individual anatomical variability. For example, as noted in the studies of Hajebrahimi S. et al., in healthy women, the values of the angles and displacement of the bladder neck may overlap with the range characteristic of patients with pathology [21]. This reduces diagnostic specificity and raises questions about the need for the clinical correlation of changes with symptoms of SUI. Despite these difficulties, the value of ultrasound examination remains high. Transperineal ultrasonography allows for noninvasive and objective assessment of the pelvic floor, detection of anatomical and functional changes, and analysis of the dynamics of parameters during treatment [22]. To improve the accuracy of diagnosis, it is important to standardize ultrasound examination protocols, including the degree of bladder filling, patient position, and performance of the Valsalva maneuver, which minimize methodological variability and provide a more accurate assessment of anatomical and functional changes.
When studying the functional characteristics of the pelvic floor using the PERFECT system, the following data were obtained (Table 5): strength (P) was measured by digital palpation of the pelvic floor muscles using the modified Oxford scale (0–5 points), reflecting the tone and strength of muscle tissue contraction. Endurance (E) was assessed as the time it took to maintain a maximum voluntary contraction without a significant decrease in strength (up to 10 s). The number of repetitions (R) was recorded as the number of consecutive maximum contractions that the patient performed with a rest interval (up to 10 times). This parameter is important for assessing muscle fatigue. Rapid contractions (F) represent the number of maximum rapid contractions (up to 10 per approach), reflecting the ability of the muscles to respond to sudden loads such as coughing.
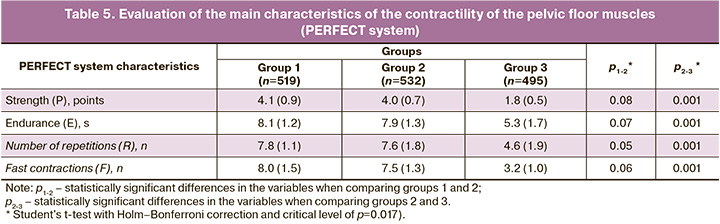
No statistically significant differences were observed in the comparative assessment of pelvic floor muscle contractility in women in the 1st and 2nd groups. However, women in group 3 showed significant changes in the contractility of the pelvic floor muscles in the form of a decrease in the strength of contractions, decreased endurance and the number of repetitions.
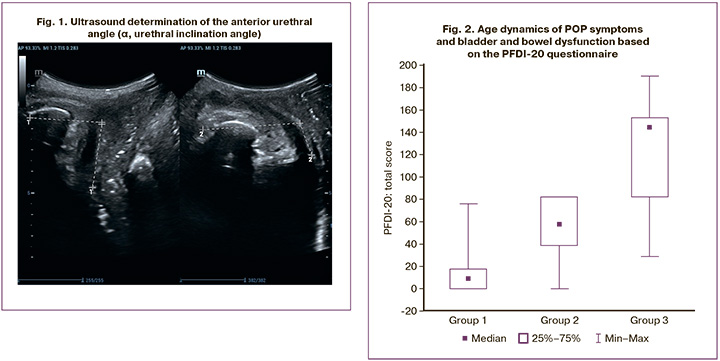
Evaluation of POP symptoms and bladder and bowel dysfunction based on the PFDI-20 questionnaire is shown in Figure 2. In group 1, the median score was 9.4 [0.0; 17.7]; in group 2, the median was 57.3 [38.5; 82.3]; and in the 3rd group – 144.8 [82.3; 153.1]. A statistically significant increase in the final score was observed when studying the dynamics of the obtained indicators. The Kruskal–Wallis criterion (H) was 1143.87 (p=0.001) and 2 =840.2 (p=0.001).
When determining the correlation between the PFDI-20 score and functional tests assessing the condition of the pelvic floor using the PERFECT system, the following results were obtained: an increase in POP symptoms and bladder and bowel dysfunction was statistically significantly associated with a decrease in the strength of pelvic floor muscle contractions (ρ=-0.60 (p=0.001] ), a decrease in endurance (ρ=-0.45 (p=0.01] ), and the number of repetitions during contraction of these muscles (ρ=-0.45 (p=0.01] ). Additionally, a statistically significant correlation was found between the Female Sexual Function Index (FSFI) and functional tests (PERFECT). PFSI was positively correlated with strength (ρ=0.51 (p=0.006), endurance (ρ=0.39 (p=0.01), and number of repetitions during contraction of the pelvic floor muscles (ρ=0.34 (p=0.01). A connection was noted between PFSI and the markers reflecting the position and size of the pelvic floor structures (POP-Q). In age-related migration of points Aa, Ba, Ap, Bp, C and D, a statistically significant decrease in the pelvic floor function index was observed: ρ(Aa)=-0.5 (p=0.01), ρ(Ba)=-0.57 (p=0.001), ρ(Ap)=-0.44 (p=0.01), ρ(Bp)=-0.49 (p=0.01), ρ(C)=-0.4 (p=0.01), ρ(D)=-0.45 (p=0.01). The quality of life of the subjects depended on the severity of prolapse symptoms and the degree of pelvic organ dysfunction (according to the results of the PFDI-20 questionnaire). An increase in these symptoms was associated with a decrease in both the physical (ρ=-0.56, p<0.001) and psychological (ρ=-0.60, p<0.001) components of health, as assessed using the SF-36 questionnaire.
Conclusion
Prolapse and dysfunction of pelvic organs in women represent a multifactorial pathology. The study results underscore the importance of comprehensive assessment of the pelvic floor, which includes both anatomical and functional parameters. This approach aids in identifying early signs of pathology, enabling a more accurate evaluation of the pelvic floor, its dynamic changes associated with aging, and the influence of predisposing factors.
This study revealed that the onset of anatomical and functional changes in most women occurs long before menopause. These findings can be used to develop individualized preventive and therapeutic programs aimed at strengthening the pelvic floor muscles, minimizing the effects of obstetric trauma, and enhancing the overall quality of life of patients.
References
- Гилядова А.В., Ищенко А.А., Решетов И.В., Ищенко А.И., Аполихина И.А., Саидова А.С., Пучкова Е.Н., Петровичев В.С., Мершина Е.А., Новрузалиева М.Ф. Роль динамической магнитно-резонансной томографии в диагностике пролапса тазовых органов. Акушерство и гинекология. 2023; 4: 28-39. [Gilyadova A.V., Ishchenko A.A., Reshetov I.V., Ishchenko A.I., Apolikhina I.A., Saidova A.S., Puchkova E.N., Petrovichev V.S., Mershina E.A., Novruzalieva M.F. The role of dynamic magnetic resonance imaging in the diagnosis of pelvic organ prolapse. Obstetrics and Gynecology. 2023; (4): 28-39 (in Russian)]. https://dx.doi.org/10.18565/aig.2023.1
- Wang B., Chen Y., Zhu X., Wang T., Li M., Huang Y. et al. Global burden and trends of pelvic organ prolapse associated with aging women: An observational trend study from 1990 to 2019. Front. Public Health. 2022; 10: 975829. https://dx.doi.org/10.3389/fpubh.2022.975829
- Yuk J.S., Lee J.H., Hur J.Y., Shin J.H. The prevalence and treatment pattern of clinically diagnosed pelvic organ prolapse: a Korean National Health Insurance Database-based cross-sectional study 2009-2015. Sci. Rep. 2018; 8(1): 1334. https://dx.doi.org/10.1038/s41598-018-19692-5
- American College of Obstetricians and Gynecologists and the American Urogynecologic Society; INTERIM UPDATE: This Practice Bulletin is updated as highlighted to reflect the US Food and Drug Administration order to stop the sale of transvaginal synthetic mesh products for the repair of pelvic organ prolapse. Pelvic Organ Prolapse. Female Pelvic Med. Reconstr. Surg. 2019; 25(6): 397-408. https://dx.doi.org/10.1097/SPV.0000000000000794
- Hadizadeh-Talasaz Z., Khadivzadeh T., Mohajeri T., Sadeghi M. Worldwide prevalence of pelvic organ prolapse: a systematic review and meta-analysis. Iran. J. Public. Health. 2024; 53(3): 524-38. https://dx.doi.org/10.18502/ijph.v53i3.15134
- Безменко А.А., Берлев И.В., Скворцов В.Г. Опыт использования синтетических сетчатых имплантов для коррекции пролапса гениталий. Военно-медицинский журнал. 2012; 333(8): 35-7. [Bezmenko A.A., Berlev I.V., Skvortsov V.G. Experience of use of synthetic cellular implants for correction of genitals prolapse. Military Medical Journal. 2012; 333(8): 35-7. (in Russian)]. https://dx.doi.org/10.17816/RMMJ74693
- Эйзенах И.А., Власова В.В., Мозес В.Г., Захаров И.С. Ранние mesh-ассоциированные послеоперационные осложнения при установке синтетических сетчатых имплантов с двумя и четырьмя рукавами у женщин с пролапсом гениталий. Медицина в Кузбассе. 2017; 16(1): 61-4. [Eisenakh I.A., Vlasova V.V., Mozes V.G., Zakharov I.S. Early postoperative mesh-related complications after placing two- and four-sleeved synthetic implants in women with genitals prolapse. Medicine in Kuzbass. 2017; 16(1): 61-4. (in Russian)].
- DaSilva K.A., Lee D.H., Sterling E.K., Hong A.H., Rahman S., Carter-Brooks C.M. Younger age is associated with pelvic floor muscle dysfunction in women with urinary symptoms. Urogynecology (Phila). 2024 Oct 18. https://dx.doi.org/10.1097/SPV.0000000000001557
- Campos N.C., de Carvalho G.M., de Santos R.A., de Brito Oliveira R.D., de Oliveira Sunemi M.M., Figueiredo E.M. Prevalence, bother, and risk factors associated with occurrence of pelvic floor dysfunctions in young women: a cross-sectional survey. Journal of Women's & Pelvic Health Physical Therapy. 2024; 48(3): 194-201. https://dx.doi.org/10.1097/jwh.0000000000000305
- Zhang S., Li B., Liu J., Yang L., Li H., Hong L. The causal effect of reproductive factors on pelvic floor dysfunction: a Mendelian randomization study. BMC Womens Health. 2024; 24(1): 74. https://dx.doi.org/10.1186/s12905-024-02914-6
- DeLancey J.O., Mastrovito S., Masteling M., Horner W., Ashton-Miller J.A., Chen L. A unified pelvic floor conceptual model for studying morphological changes with prolapse, age, and parity. Am. J. Obstet. Gynecol. 2024; 230(5): 476-484.e2. https://dx.doi.org/10.1016/j.ajog.2023.11.1247
- Gao Y., Luo X. Sonographic study on structural and functional impacts on female pelvic floor upon pregnancy, vaginal delivery and elective cesarean delivery. Chinese Journal of Obstetrics & Gynecology and Pediatrics (Electronic Edition). 2011; 07(01): 30-3. https://dx.doi.org/10.3877/cma.j.issn.1673-5250.2011.01.008
- Haylen B.T., de Ridder D., Freeman R.M., Swift S.E., Berghmans B., Lee J. et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Int. Urogynecol. J. 2010; 21: 5-26. https://dx.doi.org/10.1007/s00192-009-0976-9
- Чечнева М.А., Буянова С.Н., Попов А.А., Краснопольская И.В. Ультразвуковая диагностика пролапса гениталий и недержания мочи у женщин. М.: МЕДпресс-информ; 2016. 136c. [Chechneva M.A., Buyanova S.N., Popov A.A., Krasnopolskaya I.V. Ultrasound diagnostics of genital prolapse and urinary incontinence in women. Moscow: MEDpress-inform, 2016. 136p. (in Russian)].
- Laycock J., Jerwood D. Pelvic floor muscle assessment: The PERFECT Scheme. Physiotherapy. 2001; 87(12): 631-42. https://dx.doi.org/10.1016/s0031-9406(05)61108-x
- Asfour V., Digesu G.A., Fernando R., Khullar V. Ultrasound imaging of the perineal body: a useful clinical tool. Int. Urogynecol. J. 2020; 31(6): 1197-202. https://dx.doi.org/10.1007/s00192-019-04166-7
- Zhou M., Shui W., Bai W., Wu X., Ying T. Ultrasonographic study of female perineal body and its supportive function on pelvic floor. Front. Med. (Lausanne). 2023; 10: 1176360. https://dx.doi.org/10.3389/fmed.2023.1176360.
- Al-Saadi W.I. Transperineal ultrasonography in stress urinary incontinence: The significance of urethral rotation angles. Arab J. Urol. 2016; 14(1): 66-71. https://dx.doi.org/10.1016/j.aju.2015.11.003.
- Turkoglu A., Erturk Coskun A.D., Arinkan S.A., Vural F. The role of transperineal ultrasound in the evaluation of stress urinary incontinence cases. Int. Braz. J. Urol. 2022; 48(1): 70-7. https://dx.doi.org/10.1590/S1677-5538.IBJU.2020.1100
- Naranjo-Ortiz C., Shek K.L., Martin AJ., Dietz H.P. What is normal bladder neck anatomy? Int. Urogynecol. J. 2016; 27(6): 945-50. https://dx.doi.org/10.1007/s00192-015-2916-1
- Hajebrahimi S., Azaripour A., Sadeghi-Bazargani H. Clinical and transperineal ultrasound findings in females with stress urinary incontinence versus normal controls. Pak. J. Biol. Sci. 2009; 12(21): 1434-7. https://dx.doi.org/10.3923/pjbs.2009.1434.1437
- Dietz H.P. Ultrasound imaging of the pelvic floor. Part I: two-dimensional aspects. Ultrasound Obstet. Gynecol. 2004; 23(1): 80-92. https://dx.doi.org/10.1002/uog.939
Received 11.04.2025
Accepted 28.05.2025
About the Authors
Alexander A. Bezmenko, PhD, Head of the Department of Obstetrics and Gynecology, Military Medical Academy, 6g, Ac. Lebedev str., St. Petersburg, Russia,194044, bezmenko@yandex.ru, https://orcid.org/0000-0003-2837-1260
Igor S. Zakharov, Dr. Med. Sci., Professor at the Department of Obstetrics and Gynecology, Military Medical Academy, 6g Acad. Lebedev str., St. Petersburg, 194044, Russia, isza@mail.ru, https://orcid.org/0000-0001-6167-2968
Vitaly F. Bezhenar, Professor, Head of the Department of Obstetrics, Gynecology and Neonatology, I.P. Pavlov First St. Petersburg State Medical University,
Ministry of Health of Russia, 6-8 Lva Tolstogo str, St. Petersburg, 197022, Russia, bez-vitaly@yandex.ru, https://orcid.org/0000-0002-7807-4929
Anna S. Staroverova, Head of the Obstetric (Observation) Department of the Clinic of Obstetrics and Gynecology, Military Medical Academy, 6g Acad. Lebedev str.,
St. Petersburg, 194044, Russia, staroverova.anna85@mail.ru, https://orcid.org/0000-0003-0916-4012
Elina A. Bagramyan, Resident at the Clinic of Obstetrics and Gynecology, Military Medical Academy, 6g Acad. Lebedev str., St. Petersburg, 194044, Russia,
elin.bagramian@yandex.ru, https://orcid.org/0009-0009-8650-2426
Olga A. Ivanova, Physician at the Ultrasound Diagnostics Department, Military Medical Academy, 6g Acad. Lebedev str., St. Petersburg, 194044, Russia,
oa_ivanova_63@mail.ru, https://orcid.org/0009-0007-7125-4736
Margarita V. Kapitanova, Physician at the Ultrasound Diagnostics Department, Military Medical Academy, 6g Acad. Lebedev str., St. Petersburg, 194044, Russia,
Lysya08@mail.ru, https://orcid.org/0009-0005-7331-4099
Corresponding author: Igor S. Zakharov, isza@mail.ru



