Sexual functioning, psycho-emotional status and quality of life in patients with extragenital endometriosis and insomnia
Objective: To investigate sexual function, psychoemotional status, and quality of life (QoL) in patients with extragenital endometriosis (EGE) and insomnia.Gumenyuk L.N., Gavrilov M.V., Puchkina G.A., Chotchaev R.M., Zaurova M.B., Ivanenko O.I., Lanets I.E., Enzel D.A.
Materials and methods: This cross-sectional study included 323 patients aged 18–45 years who had EGE and insomnia (n=165) and EGE without insomnia (n=158). Sleep quality was evaluated using the Pittsburgh Sleep Quality Index (PSQI), and severity of insomnia was evaluated using the Insomnia Severity Index (ISI). We studied sexual health using the Female Sexual Function Index (FSFI) questionnaire and psycho-emotional status using the Hamilton Anxiety Rating Scale (HARS) and Hamilton Rating Scale for Depression (HDRS). Patient QoL was monitored using the QoL assessment questionnaire (Medical Outcomes Study Short Form-36, MOS SF-36).
Results: Patients with EGE and insomnia had a greater reduction in the quality of their sexual life, a higher prevalence of anxiety-depression spectrum disorders (ADSD), higher levels of depression, and lower QoL than those with EGE alone. There was a negative correlation between the integral value of ISI and the final indicators of FSFI and SF-36 and a positive correlation with the final indicator of HARS.
Conclusion: The existence of a relationship between EGE and insomnia indicates the need for routine diagnosis of insomnia disorders in this category of patients. EGE in combination with insomnia results in sexual dysfunction and ADSD and significantly reduces QoL. Timely targeted correction of insomnia can improve the effectiveness of EGE treatment.
Authors' contributions: Gumenyuk L.N. – conception and design of the study, article writing, Gavrilov M.V. – conception and design of the study; Puchkina G.A., Ivanenko O.I., Lanets I.E., Enzel D.A. – data collection, analysis and interpretation; Chotchaev R.M. – manuscript drafting, Zaurova M.B. – statistical analysis.
Conflicts of interest: The authors have no conflicts of interest to declare.
Funding: There was no funding for this study.
Ethical Approval: The study was reviewed and approved by the Research Ethics Committee of the S.I. Georgievsky Medical Academy, V.I. Vernadsky Crimean Federal University.
Patient Consent for Publication: All patients provided informed consent for the publication of their data.
Authors' Data Sharing Statement: The data supporting the findings of this study are available on request from the corresponding author after approval from the principal investigator.
For citation: Gumenyuk L.N., Gavrilov M.V., Puchkina G.A., Chotchaev R.M., Zaurova M.B., Ivanenko O.I., Lanets I.E., Enzel D.A. Sexual functioning, psycho-emotional status and quality of life in patients with extragenital endometriosis and insomnia.
Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2023; (6): 107-114 (in Russian)
https://dx.doi.org/10.18565/aig.2023.46
Keywords
Extragenital endometriosis (EGE) is one of the most pressing problems in modern gynecology, and has been the subject of active research for many decades. In recent years, data have emerged confirming the close association between EGE and insomnia [1, 2], making treatment more difficult [3]. At the same time, the relationship between existing insomnia and EGE manifestations and its impact on patients' quality of life (QoL) is often underestimated in clinical practice [3].
Insomnia of varying severity is reported in a significant proportion of patients with EGE (up to 64.8% according to some data) [4] and is an independent predictor of disease progression and adverse outcomes [3, 5]. Moreover, the negative impact of insomnia on prognosis is largely due to common pathogenic mechanisms, including pro-inflammatory changes, central sensitization, inversion of the functioning of the hypothalamic-pituitary-adrenal axis, impaired expression of neurotransmitters, and immune response [6–10]. Collectively, these mechanisms may underlie the independent negative impact of insomnia on the development of chronic pain, sexual dysfunction, and psychoemotional disorders of the anxiety-depressive spectrum (ADSD) [6–10]. At the same time, the available literature mainly discusses issues related to the cause-and-effect relationship between insomnia and chronic pain. Of interest in this context are the research data from Maggiore et al. [11] and Arion et al. [5], who described the associations between the severity of insomnia and the severity of pelvic pain and dysuria in patients with EGE. A study by Nunes et al. [12] showed a significant association between insomnia and low pain threshold.
Despite the prevalence of sexual dysfunction in patients with EGE (approximately 43.3% of cases) [13], which is known to be associated with an increased incidence of cardiovascular pathology [14], psychoemotional disorders [15], problems in interpersonal and marital interactions [16], and a significant decrease in self-esteem [17] and quality of life [18], there is no information on the contribution of insomnia to the development and severity of sexual dysfunction. At the same time, scientific publications in recent years have provided incontrovertible evidence of a link between insomnia and female sexual dysfunction. There is evidence in the literature that insomnia is an independent predictor of decreased sexual desire and response (arousal and orgasm) and dyspareunia in menopausal women [19], fibromyalgia [20], and the general population [21].
In particular, there are limited data on the contribution of insomnia to the development and severity of ADSD in patients with EGE [5], with a prevalence of 57.1% in this group [22]. An important aspect of the impact of ADSD is a significant worsening of the course of the disease, a change in the clinical response to treatment, and a decrease in the effectiveness of treatment and rehabilitation [22]. The impact of insomnia on the quality of life of patients with EGE is relevant.
This study aimed to investigate sexual function, psycho-emotional state, and quality of life in patients with EGE and insomnia.
Materials and methods
A comparative cross-sectional study was conducted in the gynecological department of St Luke's Clinical Multidisciplinary Center in Simferopol. The study comprised 323 patients, including 323 aged 18–45 years with EGE and insomnia (n=165, study group) and EGE without insomnia (n=158, control group). All the patients provided written informed consent to participate in the study.
Inclusion criteria were age 18–45 years, laparoscopically and histologically confirmed diagnosis of EGE according to the 1996 revised American Fertility Society (r-AFS) classification. The exclusion criteria were age <18 or >45 years, body mass index >24.9 kg/m2, pregnancy and lactation, diabetes mellitus type I and II, severe systemic and somatic comorbidities, mental disorders, history of alcoholism or drug addiction, taking psychotropic or other drugs that affect sleep in the last 3 months before study entry, psychocorrective interventions affecting sleep in the last 3 months before study entry, shift work, or time zone changes in the month before study entry.
Insomnia was diagnosed according to the International Classification of Sleep Disorders version 3 (2014) [23]. Sleep quality was assessed using the Pittsburgh Sleep Quality Index (PSQI) [24] and insomnia severity was assessed using the Insomnia Severity Index (ISI) [24]. The Female Sexual Function Index (FSFI) was used to assess the sexual health of patients [25]. Psychoemotional status was studied using the Hamilton Anxiety Rating Scale (HARS) and the Hamilton Rating Scale for Depression (HDRS) [26, 27]. Patients’ QoL was assessed using the QoL assessment questionnaire (Medical Outcomes Study Short Form-36, MOS SF-36) [28].
Statistical analysis
Statistical analysis was performed using STATISTICA 8.0 (StatSoft. Inc., USA). Continuous variables were presented as median (Me) with interquartile range (Q1; Q3). Differences between the two groups were analyzed using the Mann–Whitney U-test. Qualitative variables were summarized as counts and percentages and compared using the chi-squared test (χ2). Correlation analysis was conducted by calculating the Spearman's correlation coefficients. Differences were considered statistically significant at p<0.05.
Results
The clinical characteristics of the patients are summarized in Table 1. The groups were balanced by age, body mass index, prevalence, and form of EGE.
A comparison of the FSFI questionnaire results showed that patients with EGE and insomnia were significantly more likely to have sexual dysfunction than those with EGE alone (152/165 (92.1%) vs. 108/158 (68.4%), respectively (p<0.001). At the same time, in patients with EGE and insomnia, almost all domains of sexual functioning were significantly worse than in those with EGE alone. The only exceptions were domains such as lubrication and pain during intercourse that were comparable between the groups (Table 2).
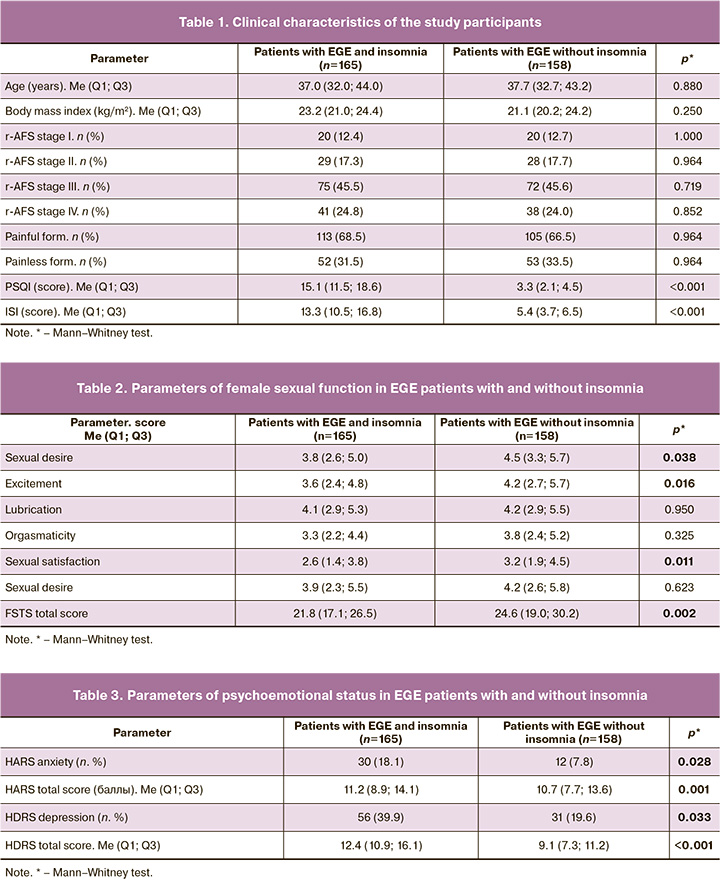
A comparison of psychoemotional status according to the HARS and HDRS scales showed a higher prevalence of ADSD disorders in patients with EGE and insomnia than in those with EGE alone:86/165 (52.1%) versus 43/158 (27.2) (p=0.014). The severity of depression was significantly higher in patients with EGE and insomnia than in those with EGE alone (p<0.001) (Table 3).
Comparison of the SF-36 questionnaire results showed that patients with EGE and insomnia had significantly lower scores for all components of the physical and psychological aspects of QoL than those with EGE alone (p=0.038 and p=0.001) (Table 4).
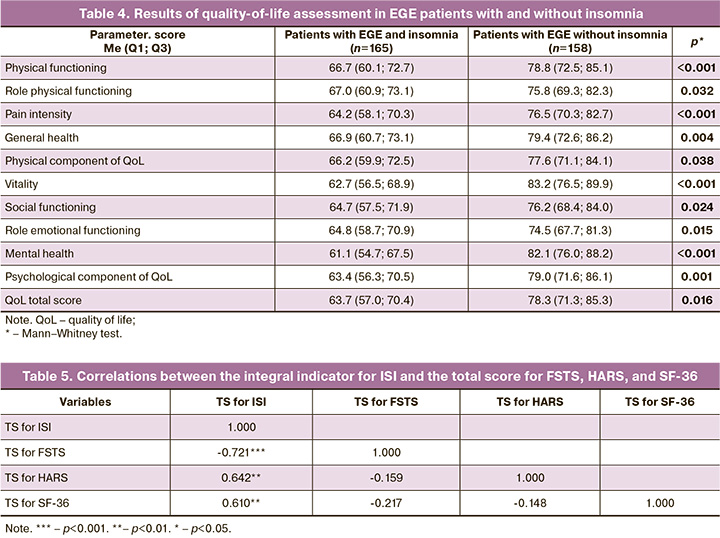
Statistically significant correlations were observed between the integral indicator for ISI and the total scores for FSFI (r=-0.721; p<0.001), HARS (r=0.642; p=0.001), and SF-36 (r=-0.610; p=0.001) (Table 5).
Discussion
This study clarified the characteristics of sexual functioning, psychoemotional status, and QoL in EGE patients with insomnia.
Our study showed a higher incidence of sexual dysfunction in patients with EGE and insomnia than in those with EGE alone. It was also found that patients with EGE and insomnia had lower scores in areas of sexual functioning, such as sexual desire, arousal, satisfaction, and orgasmic intensity, compared to those with EGE alone. We found a possible explanation for the results in the literature. It is generally accepted that the development of insomnia is based on excessive activation of the hypothalamic-pituitary-adrenal system and hypercortisolemia [29]. In turn, an increase in cortisol levels potentiates the endocrine imbalance necessary for a successful sexual response [8]. Significant data indicate a significant role of increased activity of inhibitory neurotransmitter systems, in particular, the GABAergic system (GABA), in the development of insomnia [10]. At the same time, GABA hyperactivation is known to be closely associated with decreased libido and anorgasmia. Although the mechanisms of this relationship are poorly understood, it is assumed that the cause may be the general inhibitory effect of GABA on exploratory behavior and the reduced sensitivity to stimuli [30]. It has been shown that during insomnia, there is a high dominance of the sympathetic tone of the central nervous system, which is an important predictor of impaired sexual desire, arousal, and orgasm [31], as it causes insufficient relaxation of smooth muscles and impedes blood flow to the cavernous tissues [32]. There is evidence that a significant pathogenetic component of the comorbidity of insomnia and sexual dysfunction is central and peripheral hyperalgesia [33], the negative consequences of which are recognized as a lower level of sexual desire and satisfaction [34]. It is likely that the imbalance between the inhibitory and activating systems of somatic and cortical regulation contributes to the development of sexual dysfunction in patients with EGE and insomnia. The association between the severity of insomnia and higher FSFI scores found in this study may be the basis for considering insomnia as a predictor of sexual dysfunction progression in patients with EGE. This also suggests that the treatment of insomnia disorders will contribute to its improvement; however, further research with an appropriate design is required to confirm this hypothesis.
The higher prevalence of ADSD disorders in patients with EGE and insomnia compared to those with EGE alone can be explained by the general mechanisms of their development, the main component of which is hyperactivation of the sympathetic nervous system [35]. Our results are partially consistent with the study by Arion K. et al. [5], which found that patients with EGE and insomnia had a higher frequency of depressive, but not anxiety, disorders. The contrasting results may be due to the fact that firstly, unlike the above authors, we included patients with EGE without insomnia who were comparable to those with EGE and insomnia in terms of body mass index, as this factor has been shown to influence the prevalence and severity of ADSD disorders. Second, some differences in methodology, namely, the use of objective psychometric scales for ranking ADSD disorders, could also affect the results of the study. This approach is not a limitation of the present study but, on the contrary, confirms the position of other authors on the need to use psychometric scales that best meet the requirements of the "comparison standard.” In addition, in our study, the severity of insomnia was positively correlated with the severity of depression, whereas no association was found between insomnia and anxiety.
Although our data do not allow us to draw unambiguous conclusions, based on data on causal relationships between insomnia and depression [36], it can be assumed that the following sequential transformations can be observed during EGE, contributing to the creation of a vicious circle: insomnia activation of the nuclear factor kappaB increased the transcription of interleukin-6 and tumor necrosis factor alpha increased cellular inflammation (these effects are more evident in women [11]) depressive disorder progression of EGE severity aggravation of depressive disorder. In general, our results can be the basis for classifying patients with EGE and insomnia into subgroups with an increased risk of developing ADSD. Early detection and treatment of insomnia in patients with EGE may reduce the risk of developing ADSD and be effective in alleviating the severity of the disease. However, additional studies with appropriate designs are required to confirm this hypothesis.
A significant aspect of the present work was to clarify the effect of insomnia on the QoL of patients with EGE. In our study, patients with EGE and insomnia had a more significant decrease in all aspects of QoL than patients with EGE without insomnia, mainly due to the emotional component, which may partly be mediated by a higher prevalence of sexual dysfunction and ADSD in the former. It cannot be ruled out that the differences in the QoL level that we identified in patients with EGE and insomnia and those with EGE alone can be largely determined by the direct influence of insomnia on the performance of daily activities [5] and self-perception of satisfaction with their health, professional, and social functioning [37]. In addition, our study confirmed statistically significant correlations between insomnia severity and levels of pain intensity, role-emotional functioning, life activities, social interactions, and lower QoL scores on the SF-36 questionnaire, proving the clinical and psychosocial significance of insomnia in EGE overall. Our data are in good agreement with some literature data regarding the association between the severity of insomnia and QoL. For example, in a study by Arion K. et al. [5] showed that in patients with EGE, poorer sleep quality was independently associated with painful bladder syndrome and worsening QoL. Zammit G.K. et al. [38] showed a relationship between the severity of insomnia and the severity of pelvic pain, the degree of limitation of role functioning due to the physical and emotional state in healthy individuals. In the work of Katz D.A. et al. [39] in 3455 patients with chronic somatic and psychiatric diseases found that the severity of insomnia was independently associated with lower QoL scores on all eight subscales of the SF-36 questionnaire. At the same time, the authors of [40] noted that the effect of insomnia on QoL is comparable to the severity of the effects of chronic heart failure and clinically significant depression.
Conclusion
In patients with EGE, the addition of insomnia leads to the development of sexual dysfunction and ADSD and significantly reduces quality of life. The association between EGE and insomnia suggests the need for routine screening for insomnia. Interventions to improve sleep quality should be considered part of a holistic approach to the management of EGE in this complex cohort of patients.
References
- Maggiore U.L.R., Bizzarri N., Scala C., Tafi E., Siesto G., Alessandri F. et al. Symptomatic endometriosis of the posterior cul-de-sac is associated with impaired sleep quality, excessive daytime sleepiness and insomnia: a case-control study. Eur. J. Obstet. Gynecol. Reprod. Biol. 2017; 20(9): 39-43.https://dx.doi.org/10.1016/j.ejogrb.2015.11.026.
- Ramin-Wright A., Schwartz A.S.K., Geraedts K., Rauchfuss M., Wölfler M.M., Haeberlin F. et al. Fatigue – a symptom in endometriosis. Hum. Reprod. 2018; 33(8): 1459-65. https://dx.doi.org/10.1093/humrep/dey115.
- Ishikura I.A., Hachul H., Pires G.N., Tufik S., Andersen M.L. The relationship between insomnia and endometriosis. J. Clin. Sleep Med. 2020; 16(8): 1387-8. https://dx.doi.org/10.5664/jcsm.8464.
- Leone Roberti Maggiore U., Bizzarri N., Scala C., Tafi E., Siesto G., Alessandri F., Ferrero S. Symptomatic endometriosis of the posterior cul-de-sac is associated with impaired sleep quality, excessive daytime sleepiness and insomnia: a case-control study. Eur. J. Obstet. Gynecol. Reprod. Biol. 2015; 209: 39-43.https://dx.doi.org/10.1016/j.ejogrb.2015.11.026.
- Arion K., Orr N.L., Noga H., Allaire C., Williams C., Bedaiwy M.A. et al. A quantitative analysis of sleep quality in women with endometriosis. J. Womens Health (Larchmt). 2020; 29(9): 1209-15. https://dx.doi.org/10.1089/jwh.2019.8008.
- Cameron M.J., Kelvin D.J. Cytokines and chemokines — their receptors and their genes: an overview. Adv. Exp. Med. Biol. 2003; 520: 8-32.https://dx.doi.org/10.1007/978-1-4615-0171-8_2.
- Rodenbeck A., Hajak G. Neuroendocrine dysregulation in primary insomnia. Rev. Neurol. (Paris). 2001; 157(11, Pt 2): S57-61.
- Hamilton L.D., Rellini A.H., Meston C.M. Cortisol, sexual arousal, and affect in response to sexual stimuli. J. Sex. Med. 2008; 5(9): 2111-8.https://dx.doi.org/10.1111/j.1743-6109.2008.00922.x.
- Hurtado-Alvarado G., Dominguez-Salazar E., Pavon L., Velázquez-Moctezuma J., Gómez-González B. Blood-brain barrier disruption induced by chronic sleep loss: low-grade inflammation may be the link. J. Immunol. Res. 2016; 2016(4576012): 1-15. https://dx.doi.org/10.1155/2016/4576012.
- Morgan P.T., Pace-Schott E.F., Mason G.F., Forselius E., Fasula M., Valentine G.W. Cortical GABA levels in primary insomnia. Sleep. 2012; 35(6): 807-21.https://dx.doi.org/10.5665/sleep.1880.
- Irwin M.R., Carrillo C., Olmstead R. Sleep loss activates cellular markers of inflammation: sex differences. Brain Behav. Immun. 2010; 24(1): 54-7.https://dx.doi.org/10.1016/j.bbi.2009.06.001.
- Nunes F.R., Ferreira J.M., Bahamondes L. Pain threshold and sleep quality in women with endometriosis. Eur. J. Pain. 2015; 19(1): 15-20.https://dx.doi.org/10.1002/ejp.514.
- Fairbanks F., Abdo C.H., Baracat E.C., Podgaec S. Endometriosis doubles the risk of sexual dysfunction: a cross-sectional study in a large amount of patients. Gynecol. Endocrinol. 2017; 33(7): 544-51. https://dx.doi.org/10.1080/09513590.2017.1302421.
- Veronelli A., Mauri C., Zecchini B., Peca M.G., Turri O., Valitutti M.T. et al. Sexual dysfunction is frequent in premenopausal women with diabetes, obesity, and hypothyroidism, and correlates with markers of increased cardiovascular risk. A preliminary report. J. Sex. Med. 2009; 6(6): 1561-8.https://dx.doi.org/10.1111/j.1743-6109.2009.01242.x.
- Alonso J., Buron A., Bruffaerts R., He Y., Posada-Villa J., Lepine J.P. et al. World Mental Health Consortium. Association of perceived stigma and mood and anxiety disorders: results from the World Mental Health Surveys. Acta Psychiatr. Scand. 2008; 118(4): 305-14. https://dx.doi.org/10.1111/j.1600-0447.2008.01241.x.
- Beek J.J., Dunselman G.A. Dyspareunia and depressive symptoms are associated with impaired sexual functioning in women with endometriosis, whereas sexual functioning in their male partners is not affected. Hum. Reprod. 2016; 31(11): 2577-86. https://dx.doi.org/10.1093/humrep/dew215.
- McCabe M.P., Althof S.E. A systematic review of the psychosocial outcomes associated with erectile dysfunction: does the impact of erectile dysfunction extend beyond a man’s inability to have sex? J. Sex. Med. 2014; 11(2): 347-63. https://dx.doi.org/10.1111/jsm.12374.
- Бегович Ё., Солопова А.Г., Хлопкова С.В., Сон Е.А., Унгиадзе Д.Ю., Идрисова Л.Э. Оценка сексуальной дисфункции у больных наружным генитальным эндометриозом. Акушерство, гинекология и репродукция. 2022; 16(4): 354-64. [Begovich E., Solopova A.G., Khlopkova S.V., Son E.A., Ungiadze D.Yu., Idrisova L.E. Assessing sexual dysfunction in patients with external genital endometriosis. Obstetrics, Gynecology and Reproduction. 2022; 16(4): 354-364 (in Russian)]. https://dx.doi.org/10.17749/2313-7347/ob.gyn.rep.2022.345.
- Kalmbach D.A., Kingsberg S.A., Roth T., Cheng P., Fellman-Couture C., Drake C.L. Sexual function and distress in postmenopausal women with chronic insomnia: exploring the role of stress dysregulation. Nat. Sci. Sleep. 2019; 11: 141-53. https://dx.doi.org/10.2147/NSS.S213941.
- Koca T.T., Karaca Acet G., Tanrıkut E., Talu B. Evaluation of sleep disorder and its effect on sexual dysfunction in patients with Fibromyalgia syndrome. Turk. J. Obstet. Gynecol. 2016; 13(4): 167-71. https://dx.doi.org/10.4274/tjod.17047.
- Kalmbach D.A., Arnedt J.T., Pillai V., Ciesla J.A. The impact of sleep on female sexual response and behavior: a pilot study. J. Sex. Med. 2015; 12(5): 1221-32. https://dx.doi.org/10.1111/jsm.12858.
- Laganà A.S., La Rosa V.L., Rapisarda A.M.C., Valenti G., Sapia F., Chiofalo B. et al. Anxiety and depression in patients with endometriosis: impact and management challenges. Int. J. Womens Health. 2017; 16(9): 323-30.https://dx.doi.org/10.2147/IJWH.S119729.
- Sateia M.J. International classification of sleep disorders-third edition: highlights and modifications. Chest. 2014; 146(5): 1387-94. https://dx.doi.org/10.1378/chest.14-0970.
- Buysse D.J., Reynolds C.F., Monk T.H., Berman S.R., Kupfer D.J. The Pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psychiat. Res. 1989; 28: 193-213. https://dx.doi.org/10.1016/0165-1781(89)90047-4.
- Reed S.D., Mitchell C.M., Joffe H., Cohen L., Shifren J.L., Newton K.M.et al. Sexual function in women on estradiol or venlafaxine for hot flushes: a randomized controlled trial. Obstet. Gynecol. 2014; 124(2): 233-41.https://dx.doi.org/10.1097/AOG.0000000000000386.
- Hamilton M.A. The assessment of anxiety states by rating. Br. J. Med. Psychol. 1959; 32(1): 50-5. https://dx.doi.org/10.1111/j.2044-8341.1959.tb00467.x.
- Hamilton M.A. A rating scale for depression. J. Neurol. Neurosurg. Psychiatry. 1960; 23(1): 56-62. https://dx.doi.org/10.1136/jnnp.23.1.56.
- Ware J., Sherbourne C. The MOS 36-item short-form health survey (SF-36). I. Conceptual famework and item selection. Med. Care. 1992; 30(6): 473-83. https://dx.doi.org/10.1097/00005650-199206000-00002.
- Vgontzas A.N., Bixler E.O., Lin H.M., Prolo P., Mastorakos G., Vela-Bueno A. et al. Chronic insomnia is associated with nyctohemeral activation of the hypothalamic-pituitary-adrenal axis: clinical implications. J. Clin. Endocrinol. Metab. 2001; 86(8): 3787-94. https://dx.doi.org/10.1210/jcem.86.8.7778.
- Paredes R.G., Karam P., Highland L., Agmo A. GABAergic drugs and socio-sexual behavior. Pharmacol. Biochem. Behav. 1997; 58(2): 291-8.https://dx.doi.org/10.1016/s0091-3057(97)00268-2.
- Lorenz T.K., Harte C.B., Meston C.M. Changes in autonomic nervous system activity are associated with changes in sexual function in women with a history of childhood sexual abuse. J. Sex. Med. 2015; 12(7): 1545-54.https://dx.doi.org/10.1111/jsm.12908.
- Levin R.J. The physiology of sexual arousal in the human female: a recreational and procreational synthesis. Arch. Sex. Behav. 2002; 31(5): 405-11.https://dx.doi.org/10.1023/a:1019836007416.
- Pluchino N., Wenger J.M., Petignat P., Tal R., Bolmont M., Taylor H.S. et al. Sexual function in endometriosis patients and their partners: effect of the disease and consequences of treatment. Hum. Reprod. Update. 2016; 22(6): 762-74. https://dx.doi.org/10.1093/humupd/dmw031.
- Smith K.B., Pukall C.F., Chamberlain S.M. Sexual and relationship satisfaction and vestibular pain sensitivity among women with provoked vestibulodynia. J. Sex. Med. 2013; 10(8): 2009-23. https://dx.doi.org/10.1111/jsm.12213.
- Warzecha D., Szymusik I., Wielgos M., Pietrzak B. The impact of endometriosis on the quality of life and the incidence of depression-a cohort study. Int. J. Environ. Res. Public Health. 2020;17(10): 3641. https://dx.doi.org/10.3390/ijerph17103641.
- Fang H., Tu S., Sheng J., Shao A. Depression in sleep disturbance: a review on a bidirectional relationship, mechanisms and treatment. J. Cell. Mol. Med. 2019; 23(4): 2324-32. https://dx.doi.org/10.1111/jcmm.14170.
- Ishak W.W., Bagot K., Thomas S., Magakian N., Bedwani D., Larson D. et al. Quality of life in patients suffering from insomnia. Innov. Clin. Neurosci. 2012; 9(10): 13-26.
- Zammit G.K., Weiner J., Damato N., Sillup G.P., McMillan C.A. Quality of lifein people with insomnia. Sleep. 1999; 22(l2): 379-85.
- Katz D.A., McHorney C.A. The relationship between insomnia and health-related quality of life in patients with chronic illness. J. Fam. Pract. 2002; 51(3): 229-35.
Received 20.02.2023
Accepted 31.05.2023
About the Authors
Lesya N. Gumenyuk, Dr. Med. Sci., Professor, Department of Psychiatry, Narcology, and Psychotherapy with a Course of General and Medical Psychology,S.I. Georgievsky Medical Academy, V.I. Vernadsky Crimean Federal University, lesya_gymenyuk@mail.ru, https://orcid.org/0000-0002-0944-3591,
295051, Russia, Republic of Crimea, Simferopol, Lenina Blvd, 5/7.
Mikhail V. Gavrilov, Head of the Gynecology and IVF Center, Academician Roitberg Clinic, centr.gyn@yandex.ru, https://orcid.org/0000-0002-3957-2087, 119454, Russia, Moscow, Tverskoy-Yamskoy per., 10.
Galina A. Puchkina, Teaching Assistant at the Department of Obstetrics, Gynecology and Perinatology No. 1, S.I. Georgievsky Medical Academy, V.I. Vernadsky Crimean Federal University, puchkina.g.a@mail.ru, https://orcid.org/0000-0002-8882-8317, 295051, Russia, Republic of Crimea, Simferopol, Lenina Blvd, 5/7.
Robert M. Chotchaev, Student at S.I. Georgievsky Medical Academy, V.I. Vernadsky Crimean Federal University, abdulakh.chotchaev@mail.ru,
https://orcid.org/0000-0002-6728-7822, 295051, Russia, Republic of Crimea, Simferopol, Lenina Blvd, 5/7.
Mariam B. Zaurova, Student at S.I. Georgievsky Medical Academy, V.I. Vernadsky Crimean Federal University, zaurova mariam@bk.ru, https://orcid.org/0000-0002-6378-4987, 295051, Russia, Republic of Crimea, Simferopol, Lenina Blvd, 5/7.
Olga I. Ivanenko, Student at S.I. Georgievsky Medical Academy, V.I. Vernadsky Crimean Federal University, olia.olg.iwanenko2016@mail.ru,
https://orcid.org/0000-0002-7228-2188, 295051, Russia, Republic of Crimea, Simferopol, Lenina Blvd, 5/7.
Irina E. Lanets, Student at S.I. Georgievsky Medical Academy, V.I. Vernadsky Crimean Federal University, irinalanets00@mail.ru, https://orcid.org/0000-0001-9176-7423, 295051, Russia, Republic of Crimea, Simferopol, Lenina Blvd, 5/7.
Daria A. Enzel, Student at S.I. Georgievsky Medical Academy, V.I. Vernadsky Crimean Federal University, darya enzel@yandex.ru, https://orcid.org/0000-0002-0263-6040, 295051, Russia, Republic of Crimea, Simferopol, Lenina Blvd, 5/7.
Corresponding author: Lesya N. Gumenyuk, lesya_gymenyuk@mail.ru