Characteristic features of sexual function in patients with pelvic organ prolapse
Objective. To evaluate the quality of sexual life in patients with pelvic organ prolapse (POP). Materials and methods. The study included 64 sexually active women. The main group consisted of 32 patients with POP, and the control group included 32 patients without POP and urinary incontinence. The research methods were analysis of complaints, POP-Q (Pelvic Organ Prolapse Quantification) system, questionnaires FSFI-19 (Female Sexual Function Index) and PFDI-20 (Pelvic Floor Distress Inventory). The patients of the main group who underwent surgical treatment for POP were assessed 6 months after the operation. Results. During the study, we were able to identify a correlation between PFDI-20 and FSFI-19 scores (r=-0.6, p=0.00002), which confirms the relationship between the severity of POP and sexual disorders in women. After the treatment, 27 patients with POP stage II, III and IV were absolutely cured, and 5 patients showed regression of POP to stage I (p<0.001). The number of patients with dyspareunia decreased by 5 times (p<0.001). There was an improvement in the scores of the questionnaires FSFI-19 and PFDI-20, POPDI-6 (Pelvic Organ Prolapse Distress Inventory) and UDI-6 (Urinal Distress Inventory). The questionnaire CRADI-8 (Colorectal-Anal Distress Inventory) did not show a statistical difference. Conclusion. POP negatively affects many aspects of intimate life. Comprehensive treatment can manage the condition of most patients and improve the quality of their sexual life.Dobrokhotova Yu.E., Kamalov А.А., Slobodyanyuk B.А., Nagieva Т.S., Khlynova S.А., Dimitrova V.I.
Keywords
Pelvic organ prolapse is one of the main clinical manifestations of pelvic floor dysfunction and is often associated with such disorders as urinary and/or anal incontinence [1]. The incidence of pelvic organ prolapse varies widely (30–76%) and increases with age [2]: it is 6% among women 20–29 years old, 31% among women 50–59 years old, and up to 50% among women 80 years old and older [3]. This problem is becoming more relevant due to the increase in life expectancy. Sexual dysfunction caused by vaginal relaxation syndrome is also a serious problem in the postpartum period [4].
Many researchers confirm that women are less likely to have sex when they have pelvic organ prolapse [5]. Since sexuality is an important part of life, it leads to a significant decrease in quality of life. The analysis of 535 women who were treated in Urogynecology Department found that 28% of sexually inactive women avoid sexual activity due to the prolapse of pelvic organs and pelvic floor dysfunction [6].
Prolapse is also characterized by a change in the perception of one’s own body [7], which is an important and insufficiently studied phenomenon. In one case-control study, Jelovsek J.E. et al. compared patients with advanced forms of prolapse (stages III–IV). The control group included patients with prolapse stage 0–I without urinary incontinence; the patients were comparable in demographic parameters. It was found that women with prolapse are 4.7 times more likely to be uncomfortable with their appearance, 11 times more likely to feel less attractive, and 4 times less likely to feel feminine; however, there was a significant change in their intimate life including its absence [8].
Sexual dysfunction in patients with pelvic floor disorders is observed in 50–83% of cases [9]. The scientific literature presents data on the correlation between pelvic disorders and the intimate life of patients with this pathology [10, 11]. The researchers focus on the results of the FSFI-19 (Female Sexual Function Index) questionnaire, including the results obtained before and after surgical correction of pelvic organ prolapse and/or urinary incontinence [12–18]. Besides, it is not always possible to take into account the level of sexual activity of perimenopausal and postmenopausal patients, the refusal of patients to be engaged in sexual activity due to the severe prolapse of pelvic organs, and the nature of the relationship between the symptoms of pelvic organ prolapse and the degree of sexual dysfunction.
The aim of the study is to evaluate the quality of sexual life in patients with pelvic organ prolapse.
Materials and Methods
The study included 64 sexually active women who gave an informed consent to participate in the study. They received treatment in Gynecology Department of the F.I. Inozemtsev City Clinical Hospital, Moscow, Russia. The main group included women with diagnosed pelvic organ prolapse; the control group consisted of patients without pelvic organ prolapse who came for a routine check-up to the Clinical Diagnostic Center. The exclusion criteria were pregnancy, severe gynecological and extragenital pathology, abnormalities of the genitourinary system, symptomatic uterine fibroids and endometriosis, acute pelvic inflammatory diseases and the diseases of urogenital tract, oncological diseases, neuropsychiatric disorders (including psychogenic sexual disorders).
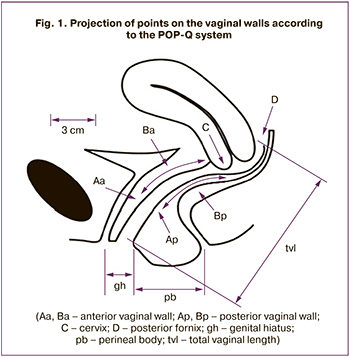 The research methods included taking the patient’s history, the analysis of complaints, gynecological examination, and standard clinical and laboratory data. In order to determine the stage of pelvic organ prolapse, the Pelvic Organ Prolapse Quantification system (POP-Q) was used which is based on the assessment of the position of the vaginal and cervical walls in relation to the hymenal ring (Fig. 1) [19].
The research methods included taking the patient’s history, the analysis of complaints, gynecological examination, and standard clinical and laboratory data. In order to determine the stage of pelvic organ prolapse, the Pelvic Organ Prolapse Quantification system (POP-Q) was used which is based on the assessment of the position of the vaginal and cervical walls in relation to the hymenal ring (Fig. 1) [19].
Taking into account the inclusion and exclusion criteria, the main group consisted of patients with pelvic organ prolapse, stages II–IV; this group is characterized by the lowering of the vaginal or cervix walls by one centimeter or more from the hymen. Distance measurement was performed using a graduated uterine probe and a ruler.
To assess the impact of pelvic floor dysfunction symptoms on the quality of life of patients with pelvic organ prolapse, the results of the PFDI-20 (Pelvic Floor Distress Inventory) questionnaire were used. The questionnaire includes 20 questions divided into three blocks: POPDI-6 (Pelvic Organ Prolapse Distress Inventory) for the analysis of complaints associated directly with pelvic organ prolapse, CRADI-8 (Colorectal – Anal Distress Inventory) for the assessment of anorectal symptoms, and UDI–6 (Urinal Distress Inventory) for the detection of urinary disorders.
The FSFI-19 questionnaire was used to determine the level of quality of sexual life, taking into consideration such parameters as desire, arousal, lubrication, orgasm, satisfaction and pain. The range of scores was from 0 to 36.
Statistical analysis
Statistical processing of the data was performed using the statistical software package Office Excel (Microsoft 2016) and Statistica version 12.0 (StatSoft). Data distribution was analyzed using the Kolmogorov– Smirnov criterion. For a normal distribution, parametric methods of statistical analysis were used; in other cases, nonparametric methods were applied. The nonparametric Mann-Whitney test was used to determine the significance of quantitative differences for two independent groups. The analysis of qualitative features was carried out using the Chi-square criterion. The relationship between the results of the PFDI-20 and FSFI-19 questionnaire was determined on the basis of the Spearman correlation and scatter diagram was constructed. Dependent features were evaluated using nonparametric criteria of McNemar and Wilcoxon tests. The value of p=0.05 is considered as the critical significant level.
Results
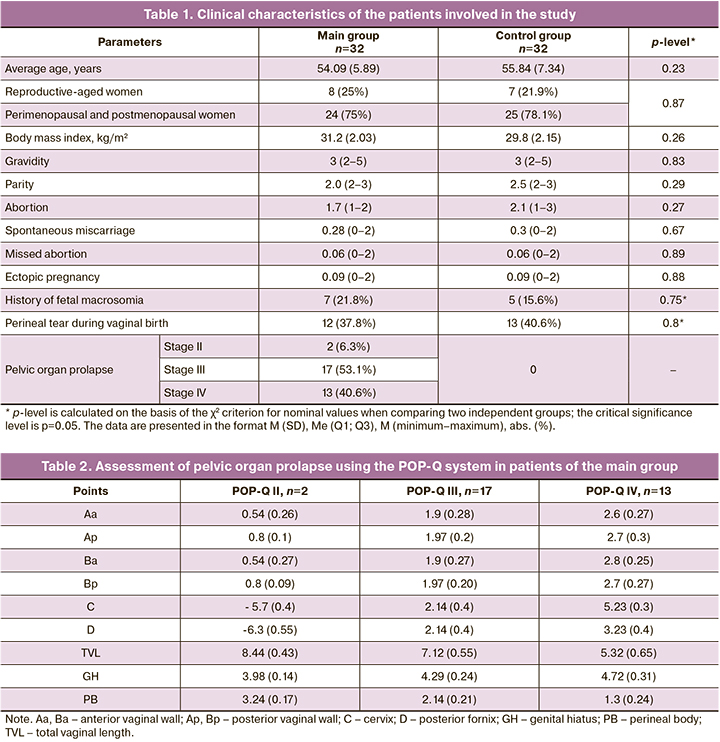
The age of the patients who took part in the study ranged from 37 to 66 years. Data on body mass index, average age, characteristics of obstetric history in patients of both groups, and the prevalence of pelvic organ prolapse in patients of the main group are presented in Table 1.
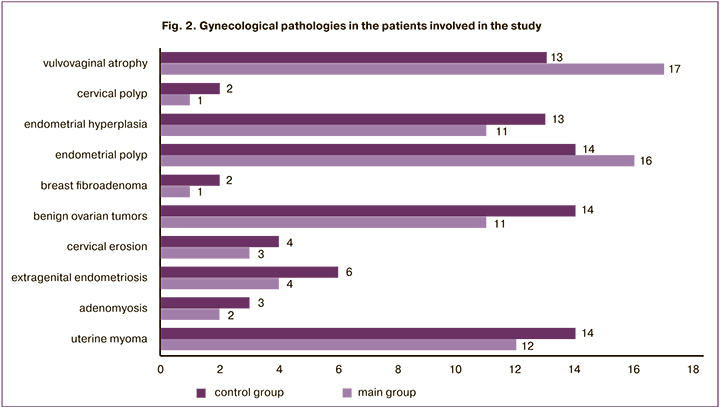
The analysis of patients’ gynecological history revealed the absence of statistically significant differences in individual diseases in patients of the main and control groups (p>0.05). The data are presented in Fig. 2.
According to the POP-Q classification, we measured the vaginal points, as well as the length of the genital hiatus (GH) and the perineal body (PB) (Table 2). As the stage of prolapse progressed, the length of the genital hiatus significantly increased in the patients of the main group, while the length of the perineal body decreased by almost 1.5 times (p<0.05).
During the survey of patients with pelvic organ prolapse, the following results were obtained: women with stage II pelvic organ prolapse had POPDI-6 value 21.3 (11.26; 34.8) scores, CRADI-8 – 15.9 (9.6; 19.2) scores, and UDI-6 – 18.1 (10.7; 23.3) scores; women with stage III pelvic organ prolapse had POPDI-6 value 34.1 (19.8; 45.4) scores, CRADI-8 – 19.8 (11.3; 23.6) scores, and UDI-6 – 23.4 (16.4; 28.2) scores; women with stage IV pelvic organ prolapse had POPDI-6 value 47.2 (33.2; 59.6) scores, CRADI-8 – 22.1 (14.2; 25.5) scores, and UDI-6 – 33.3 (23.5; 41.7) scores.
The level of statistical significance of differences between the patients with pelvic organ prolapse stages II and III–IV was calculated using the Mann-Whitney test. According to the results of the analysis, urinary disorders and symptoms associated directly with pelvic organ prolapse were significantly more frequently registered in patients with stage III–IV prolapse, p<0.05. At the same time, there were no statistically significant differences in the frequency of anorectal symptoms in patients with stages II and III–IV pelvic organ prolapse due to the fact that these symptoms are less common without correlation with the stage of pelvic organ prolapse.
The analysis of sexual function in patients of the main and control groups based on the FSFI-19 questionnaire is presented in Table 3.
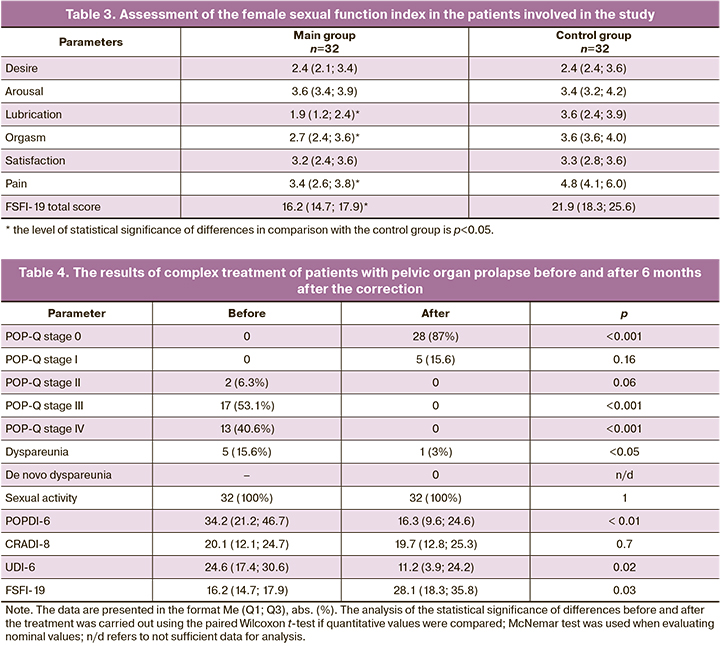
According to the obtained results, the patients of the main group compared to the control group had a statistically significant decrease in the median score of the female sexual function index in such parameters as lubrication (1.9 times), orgasm (1.3 times), and pain (1.4 times) (p<0.05).
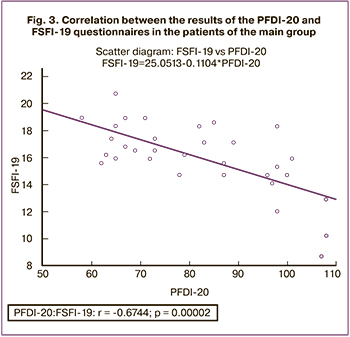 We compared the results of the PFDI-20 and FSFI-19 questionnaires in patients with pelvic organ prolapse using Spearman’s nonparametric correlation analysis. According to the results of the descriptive statistics, the PFDI-20 and FSFI-19 scores in this group of patients were 80.5 (67.0; 97.5) points and 16.03 (14.7; 17.9) points, respectively. At the same time, there was an inverse moderate correlation between the results of the survey using the PFDI-20 and FSFI-19 questionnaires (Fig. 3).
We compared the results of the PFDI-20 and FSFI-19 questionnaires in patients with pelvic organ prolapse using Spearman’s nonparametric correlation analysis. According to the results of the descriptive statistics, the PFDI-20 and FSFI-19 scores in this group of patients were 80.5 (67.0; 97.5) points and 16.03 (14.7; 17.9) points, respectively. At the same time, there was an inverse moderate correlation between the results of the survey using the PFDI-20 and FSFI-19 questionnaires (Fig. 3).
All patients with pelvic organ prolapse received complex treatment: conservative correction (electrical stimulation with a vaginal sensor, pelvic floor muscle training) and surgical intervention. Surgical management of pelvic organ prolapse is done in our practice mainly via vagina. Surgery can be divided into three types:
- Classic technique is applied with the use of local tissues, that is anterior and posterior colporrhaphy combined with hysterectomy and strengthening of the vaginal vault with ligamentous apparatus; it was performed in 4 cases (12.5%).
- Site-specific plastic surgery which is aimed at detecting pelvic fascia defects (usually these are high transverse (pericervical) defects of the pubic-cervical and rectovaginal fascia, paravaginal fascia is less common). In this case, the fascial defects are reapproximated to the cervix and the cardinal ligaments are shortened in the form of a duplicate and uterosacral ligaments are also shortened via extraperitoneal access with non-absorbable mono- or multifilament ligatures according to our technique; it was performed in 12 cases (37.5%).
- Hybrid reconstruction which is similar to the second type of operation; however, if there is a severe apical defect or stretchable tissues (determined subjectively), a transsacrospinal sling with a polypropylene Cyrene tape is utilized using the inside-out method. The tape is carried extraperitoneally through the medial middle part of the sacrospinal and sacrotuberal ligaments bilaterally. This tape causes fibrosis along its course and provides reliable long-term apical fixation in 16 cases (50%).
Urethropexy (15.6%), perineoplasty (28%), sphincteroplasty (3%), and Sturmdorf amputation of the uterine cervix (12.5%) were performed according to the indications. The operation time did not exceed two hours, blood loss was 100ml. There were no intraoperative complications.
It should be noted that even sexually active patients with stage IV pelvic organ prolapse are always able to avoid being placed large implants on both the anterior and posterior vaginal walls. We consider it important to maintain the elasticity of the vaginal wall for the proper functioning of adjacent organs and sexual function, especially the posterior vaginal wall and the area of the neck of the bladder. Moreover, pelvic organ prolapse is not considered by us as an indication for hysterectomy. On the contrary, the cervix is used as a «keystone», providing anatomically correct reconstruction, maintaining blood supply. When using site-specific methods, excessive vaginal wall excision is not performed. This approach does not cause protrusion of the mesh in the vagina.
All patients were monitored for 6 months (range of 4-8 months). The results of the patients from the main group before and after the treatment are presented in Table 4. There are positive subjective and objective anatomical outcomes. Stage 0 was observed in 27 patients, and stage I was revealed in 5 patients (cystocele or rectocele with high apical support). There were no complaints about the feeling of a foreign body in the vagina. In addition, there was an improvement in the parameters of the FSFI-19 and PFDI-20 questionnaires (overall score), as well as the questionnaire on prolapse (POPDI-6) and its urological part (UDI-6). The questionnaire on colorectal problems (CRADI-8) did not show a statistical difference due to the fact that the studied patients had no obvious complaints before the operation. All patients resumed sexual activity, and there was no de novo dyspareunia.
Discussion
Female sexuality, especially in this category of patients, is a multi-factor phenomenon, and its study is a complex issue. It is noteworthy that problems of male sexual dysfunction and earlier male mortality often become prevailing. Women may have a sedentary lifestyle, frequent somatic problems (obesity, diabetes, cardiovascular diseases, etc.); however, the impact of pelvic dysfunctions on female sexuality is beyond any doubt. A lot of women are known to keep silent about their problems, despite a direct question from the doctor (for example, about fecal incontinence), which can negatively affect the results of the treatment. The use of questionnaires allows women to answer delicate questions more sincerely, therefore, their use is recommended not only in research, but also in routine clinical work.
This is a complex problem because women without prolapse may also experience problems in the sexual sphere (according to the results of the FSFI-19 questionnaire). When the PFDI-20 questionnaire was used, there was a correlation between the severity of symptoms and the stage of prolapse, which was confirmed by many researchers; it was also possible to identify a correlation between the overall scores of PFDI-20 and FSFI-19 (r=-0.6, p=0.00002), which certainly confirms the connection between the severity of pelvic disorders in prolapse and sexual disorders in women. Conservative treatment (pessaries and electrostimulation) has almost no side effects, but in our study the therapeutic effect was insufficient, and all the patients insisted on surgical treatment. This is a methodological defect of the research, since we did not take into account the patients who refused to receive further treatment in our clinic.
In the surgical treatment of patients, we do not support the opinion of American, English and some European colleagues about a complete ban on the use of synthetic implants inserted vaginally. We call for differentiating sling operations for prolapse from the placement of large vaginal polypropylene prostheses, which are used, for example, in Japan. The presence of pelvic pain and dyspareunia before surgery is a complex pathology that must be diagnosed in order to avoid legal problems later. However, in most cases, patients receiving complex treatment (surgery and physiotherapy) in our series stop suffering from pelvic pains. According to various data, de novo dyspareunia occurs in 2-28% of cases when using mesh prostheses [20] and in 1–15% of cases when using local tissues [21]. Some authors relate its high percentage to the lack of adequate preoperative examination. Factors that cause de novo dyspareunia include shortening and narrowing of the vagina after excision, involvement of nerves in scarring, the use of large synthetic prostheses and their incorrect placement, as well as «shrinkage» of the prostheses. It should be particularly noted that levatorplasty has a very high level of dyspareunia. Being first described by Geghar about 190 years ago, this intervention consists in stitching bundles of m. puborectalis anteriorly from the rectum, where it is not normally located. This intervention does not lead to improved results for rectocele and should not be applied routinely [22].
In our study, there was a significant improvement in sexual activity in the majority of patients (96%), partially due to a positive perception of their body.
Conclusion
When pelvic organ prolapse progresses, it may negatively affect many aspects of intimate life. Comprehensive treatment can manage the condition of most patients and improve the quality of their sexual life. However, during surgical treatment, it is necessary to avoid using large vaginal meshes and performing levatorplasty in patients who are sexually active.
References
- Hong M.K., Ding D.C. Current treatments for female pelvic floor dysfunctions. Gynecol. Minim. Invasive Ther. 2019; 8(4): 143-8. https://dx.doi.org/10.4103/GMIT.GMIT_7_19.
- Good M.M., Solomon E.R. Pelvic floor disorders. Obstet. Gynecol. Clin. North Am. 2019; 46(3): 527-40. https://dx.doi.org/10.1016/j.ogc.2019.04.010.
- Wu J.M., Vaughan C.P., Goode P.S., Redden D.T., Burgio K.L., Richter H.E. et al. Prevalence and trends of symptomatic pelvic floor disorders in U.S. women. Obstet. Gynecol. 2014; 123(1): 141-8. https://dx.doi.org/10.1097/AOG.0000000000000057.
- Доброхотова Ю.Э., Нагиева Т.С., Ильина И.Ю., Карева Е.Н., Кочина Н.А., Зрагус Е.В., Доброва А.Б., Шахмаратова И.А., Краснощок Е.В. Влияние радиочастотного неаблативного воздействия на экспрессию белков соединительной ткани урогенитального тракта у пациенток с синдромом релаксированного влагалища в послеродовом периоде. Акушерство и гинекология. 2019; 8: 119-25. [Dobrokhotova Yu.E., Nagieva T.S.,Ilyina I.Yu., Kareva E.N., Kochina N.A., Zragus E.V., Dobrova A.B., Shakhmaratova I.A. Krasnoshchok E.V. Influence of nonablative radiofrequency on the expression of connective tissue proteins in the urogenital tract in patients with vaginal relaxation syndrome during the postpartum period. Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2019; 8: 119-25. (in Russian)]. https://dx.doi.org/10.18565/aig.2019.8.119-125.
- Handa V.L., Cundiff G., Chang H.H., Helzlsouer K.J. Female sexual function and pelvic floor disorders. Obstet. Gynecol. 2008; 111(5): 1045-52. https://dx.doi.org/10.1097/AOG.0b013e31816bbe85.
- Barber M.D., Visco A.G., Wyman J.F., Fantl J.A., Bump R.C. Continence Program for Women Research Group Sexual function in women with urinary incontinence and pelvic organ prolapse. Obstet. Gynecol. 2002; 99(2): 281-9. https://dx.doi.org/10.1016/s0029-7844(01)01727-6.
- Edenfield A.L., Levin P.J., Dieter A.A., Amundsen C.L., Siddiqui N.Y. Sexual activity and vaginal topography in women with symptomatic pelvic floor disorders. J. Sex. Med. 2015; 12(2): 416-30. https://dx.doi.org/10.1111/jsm.12716.
- Jelovsek J.E., Barber M.D. Women seeking treatment for advanced pelvic organ prolapse have decreased body image and quality of life. Am. J. Obstet. Gynecol. 2006; 194(5): 1455-61. https://dx.doi.org/10.1016/j.ajog.2006.01.060.
- Verbeek M., Hayward L. Pelvic floor dysfunction and its effect on quality of sexual life. Sex. Med. Rev. 2019; 7(4): 559-64. https://dx.doi.org/10.1016/j.sxmr.2019.05.007.
- Стеняева Н.Н., Хритинин Д.Ф., Чаусов А.А, Сухих Г.Т. Распространенность и структура сексуальных дисфункций у женщин при обращении в гинекологическую клинику. Акушерство и гинекология. 2017; 3: 101-7. [Stenyaeva N.N., Khritinin D.F., Chausov A.A., Sukhikh G.T. Prevalence and patterns of sexual dysfunctions in women visiting a gynecology clinic. Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2017; 3: 101-7. (in Russian)]. https://dx.doi.org/10.18565/aig.2017.3.101-7.
- Доброхотова Ю.Э., Нагиева Т.С. Дисфункция тазового дна у женщин репродуктивного периода, синдром релаксированного влагалища – необходимость реабилитации в послеродовом периоде. РМЖ. Мать и дитя. 2017; 15: 1121-4. [Dobrokhotova Yu.E., Nagieva T.S. Pelvic floor dysfunction in women of reproductive age, vaginal relaxation syndrome – necessity of rehabilitation in the postpartum period. RMJ. 2017; 15: 1121-4. (in Russian)].
- Kamińska A., Futyma K., Romanek-Piva K., Streit-Ciećkiewicz D., Rechberger T. Sexual function specific questionnaires as a useful tool in management of urogynecological patients - Review. Eur. J. Obstet. Gynecol. Reprod. Biol. 2019; 234: 126-30. https://dx.doi.org/10.1016/j.ejogrb.2019.01.015.
- Lourenço T.R.M., Pergialiotis V., Durnea C.M., Elfituri A., Haddad J.M., Betschart C. et al. A systematic review of reported outcomes and outcome measures in randomized trials evaluating surgical interventions for posterior vaginal prolapse to aid development of a core outcome set. CHORUS: An International Collaboration for Harmonising Outcomes, Research and Standards in Urogynaecology and Women's Health. Int. J. Gynaecol. Obstet. 2019; Dec. 9. https://dx.doi.org/10.1002/ijgo.13079.
- La Rosa V.L., Ciebiera M., Lin L.T., Sleiman Z., Cerentini T.M., Lordelo P. et al. Multidisciplinary management of women with pelvic organ prolapse, urinary incontinence and lower urinary tract symptoms. A clinical and psychological overview. Prz Menopauzalny. 2019; 18(3): 184-90. https://dx.doi.org/10.5114/pm.2019.89496.
- Liao S.C., Huang W.C., Su T.H., Lau H.H. Changes in female sexual function after vaginal mesh repair versus native tissue repair for pelvic organ prolapse: A meta-analysis of randomized controlled trials. J. Sex. Med. 2019; 16(5): 633-9. https://dx.doi.org/10.1016/j.jsxm.2019.02.016.
- Monti M., Schiavi M.C., Colagiovanni V., Sciuga V., D'oria O., Cerone G. et al. Effectiveness, quality of life and sexual functions in women with anterior compartment prolapse treated by native tissue repair. Minerva Ginecol. 2019; 71(1): 18-24. https://dx.doi.org/10.23736/S0026-4784.18.04305-8.
- Thompson J.C., Rogers R.G. Surgical management for pelvic organ prolapse and its impact on sexual function. Sex. Med. Rev. 2016; 4(3): 213-20. https://dx.doi.org/10.1016/j.sxmr.2016.02.002.
- Rantell A., Srikrishna S., Robinson D. Assessment of the impact of urogenital prolapse on sexual dysfunction. Maturitas. 2016; 92: 56-60. https://dx.doi.org/10.1016/j.maturitas.2016.07.001.
- Bump R.C., Mattiasson A., Bo K., Brubaker L.P., DeLancey J.O., Klarskov P., Shull B.L. The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am. J. Obstet. Gynecol. 1996; 175(1): 10-7. https://dx.doi.org/ 10.1016/s0002-9378(96)70243-0.
- Porter W.E., Steele A., Walsh P., Kohli N., Karram M.M. The anatomic and functional outcomes of defect-specific rectocele repairs. Am. J. Obstet. Gynecol. 1999; 181(6): 1353-8. https://dx.doi.org/10.1016/s0002-9378(99)70376-5.
- Maher C., Feiner B., Baessler K., Adams E.J., Hagen S., Glazener C.M. Surgical management of pelvic organ prolapse in women. Cochrane Database Syst. Rev. 2010; (4): CD004014. https://dx.doi.org/10.1002/14651858.CD004014.pub4.
- Ulrich D., Dwyer P., Rosamilia A., Lim Y., Lee J. The effect of vaginal pelvic organ prolapse surgery on sexual function. Neurourol. Urodyn. 2015; 34(4): 316-21. https://dx.doi.org/10.1002/nau.22569.
Received 11.02.2020
Accepted 15.05.2020
About the Authors
Yulia E. Dobrokhotova, MD, Professor, Head of the Department of Obstetrics and Gynecology, Russian National Research Medical University named after N.I. Pirogov.Tel.: +7(903)722-63-99. E-mail: pr.dobrohotova@mail.ru. 117997, Russia, Moscow, Ostrovityanova str., 1.
Armais A. Kamalov, MD, Professor, Academician of the Russian Academy of Sciences, Director of the Scientific and Educational Center of Moscow State University.
Tel.: +7(495)531-27-27. 119991, Russia, Moscow, Leninskie Gory, 1.
Boris A. Slobodyanyuk, PhD, Associate Professor of the Department of Obstetrics and Gynecology, Russian National Research Medical University named after N.I. Pirogov. Tel.: +7(903)210-98-95. E-mail: borisslo@mail.ru. 117997, Russia, Moscow, Ostrovityanova str., 1.
Tamara S. Nagieva, Assistant of the Department of Obstetrics and Gynecology, Russian National Research Medical University named after N.I. Pirogov.
Tel.: +7(915)155-26-01. E-mail: nagieva.ts@mail.ru. 117997, Russia, Moscow, Ostrovityanova str., 1.
Valentina I. Dimitrova, PhD, Head of the Gynecology Department, obstetrician-gynecologist of the highest qualification category,
Clinical Hospital named after F.I. Inozemtsev. Tel.: +7(916)200-51-91. 105187, Russia, Moscow, Fortunatovskaya str., 1.
Svetlana A. Khlynova, PhD, Associate Professor of the Department of Obstetrics and Gynecology, Russian National Research Medical University named after N.I. Pirogov. Tel.: +7(926)280-63-67. E-mail: doc-khlinova@mail.ru. 117997, Russia, Moscow, Ostrovityanova str., 1.
For citation: Dobrokhotova Yu.E., Kamalov А.А., Slobodyanyuk B.А., Nagieva Т.S., Khlynova S.А., Dimitrova V.I. Characteristic features of sexual function in patients with pelvic organ prolapse.
Akusherstvo i Ginekologiya / Obstetrics and gynecology. 2020; 8: 112-119 (in Russian)
https://dx.doi.org/10.18565/aig.2020.8.112-119