ACUM (Accessory and Cavitated Uterine Mass) – это редкая форма аномалии развития мюллеровых протоков, чаще наблюдаемая у подростков или молодых женщин, и представляющая собой не сообщающуюся с основной добавочную полость матки, окруженную тканью миометрия (uterine-like masses (ULM), маточно-подобные массы), как правило, расположенную в толще самой матки или в месте крепления круглой связки матки.
Кистозный аденомиоз матки представляет собой кистозную структуру, выстланную эндометрием и окруженную тканью миометрия, в большинстве случаев с геморрагическим содержимым.
Термины, используемые в литературе для описания кистозной формы аденомиоза и ACUM, вызывают значительные разногласия. В исследовании Takeuchi H. et al. (2010) [1] описали 30 молодых пациенток с «кистозной аденомиомой» (JCA, Juvenile cystic adenomyoma, ювенильная кистозная аденомиома) на основании следующих критериев: 1) возраст ≤30 лет; 2) наличие кистозного поражения диаметром ≥10 мм, которое не сообщалось с просветом матки и которое было окружено гипертрофированным миометрием при диагностической визуализации; 3) ассоциация с тяжелой дисменореей. Cucinella G. et al. (2013) [2], Takeda H. et al. (2007) [3] предложили вместо термина «аденомиома» использовать термин «ювенильная аденомиотическая киста» или JCA, в зависимости от возраста. Acién P. et al. (2010) [4] и Bedaiwy M.A. et al. (2013) [5] предположили, что описанные ранее клинические случаи изолированной дополнительной полости матки или изолированной кистозной аденомиомы, а также в некоторых случаях ULM, на самом деле, относятся к одной и той же патологии – ACUM, особенностью которого является наличие функционирующего эндометрия. В отличие от случаев диффузного и узлового аденомиоза, ACUM представляет собой изолированную добавочную полость с «шоколадным» содержимым, выстланную функционирующим эндометрием нормального строения, окруженную концентрически организованным миометрием. Авторы подчеркивают, что порок развития ACUM необходимо также дифференцировать от случаев пороков развития с удвоением матки и наличием замкнутого рудиментарного маточного рога [4, 6, 7].
 Было предложено выделение ACUM в отдельную патологию и введение в классификацию в качестве нового варианта порока развития мюллеровых протоков [8].
Было предложено выделение ACUM в отдельную патологию и введение в классификацию в качестве нового варианта порока развития мюллеровых протоков [8].
Развитие аномалий мюллеровых протоков связано с особенностями эмбриогенеза (рис. 1).
Уточнение особенностей эмбриогенеза женских половых органов было проведено в исследованиях Адамян Л.В., Макияна З.Н. и соавт. на основании оценки данных выборки 434 пациентов с различными пороками развития матки [9, 10].
Существует три теории развития ACUM: (1) теория врожденных аномалий, (2) теория гетеротопий и (3) теория метаплазии [4].
Теория врожденных аномалий подтверждается сосуществованием нарушений развития в нижних отделах желудочно-кишечного тракта и мочевыводящих путей у пациентов с ULM. Rosai J. предположил, что ULM являются результатом дефекта слияния мюллеровых протоков или частичного дублирования мюллеровой системы [11].
Теория гетеротопии была предложена Peterson C.J. et al. [12] в которой сообщалось о наличии ULM в подвздошной области у пациентки с множественными аномалиями развития мочеполовой системы и кишечного тракта, а также с крестцово-копчиковой аномалией.
Acién P. et al. [4] предположили, что развитие ACUM может быть обусловлено дубликатурой и персистированием протоковой мюллеровой ткани в критической области, а именно в месте прикрепления круглой связки; аномалия развития мюллерового протока, в литературе называемая JCA, ULM или добавочная полость матки в настоящее время переименованы в один термин – ACUM.
Дифференциальная диагностика ACUM проводится с кистозным аденомиозом и пороками развития внутренних половых органов при наличии функционирующего маточного рудимента.
Клинические проявления ACUM и узловой формы аденомиоза очень сходны, что определяет сложность дифференциальной диагностики этих состояний. К основным клиническим проявлениям ACUM относят дисменорею, хроническую тазовую боль спастического характера, прогрессирующую после менархе и устойчивую к анальгетическим препаратам [1, 3, 4]. Основным клиническим проявлением у пациенток с аденомиозом также является боль в нижних отделах живота и пояснице, интенсивность которой меняется в зависимости от фазы менструального цикла, усиливаясь перед менструацией и в первые дни. По мере прогрессирования патологического процесса боль теряет связь с менструацией, становится относительно постоянной [13].
Из-за типичной клинической картины и редкости ACUM пациентам часто устанавливается диагноз порока развития половых органов, полного удвоения матки с наличием функционирующего маточного рудимента. В дифференциальной диагностике между ACUM и наличием маточного замкнутого функционирующего рога важное значение имеют данные ультразвукового исследования (УЗИ) и гистероскопии. При пороке развития по типу удвоения матки характерна продолговатая однорогая полость матки и наличие одного устья маточной трубы, а по данным УЗИ, магнитно-резонансной томографии (МРТ) и лапароскопии визуализируется дополнительный маточный замкнутый функционирующий рудимент. Тогда как ACUM обнаруживается в матке, имеющей нормальную правильную треугольную форму с двумя устьями маточных труб [14].
Эндометриома яичника вблизи широкой связки матки может также имитировать ACUM с геморрагическим содержимым в сочетании с циклической болью в области таза. Однако, эндометриома находится в яичнике, что подтверждается при оценке кровотока в яичнике, а также наличием фолликулов в здоровой паренхиме яичника и, кроме того, не имеет толстого периферического кольца мышечной ткани.
В некоторых случаях лейомиома с большой центральной кистозной дегенерацией может по радиологическим признакам иметь схожесть с ACUM, но она чаще встречается у женщин старшего репродуктивного возраста и отличается по клинической картине, поскольку миомы редко сопровождаются циклической менструальной болью [15].
МРТ позволяет уточнить расположение ACUM в матке, его морфологию, структуру, включая наличие или отсутствие центральной полости и периферического мышечного кольца. МРТ признаками ACUM являются: сходство с несообщающимся функционирующим маточным рудиментом в пределах нормальной матки, чаще всего округлой формы; наличие полости с геморрагическим содержимым, не сообщающейся с полостью матки, с повышенным МР-сигналом на T2 взвешенном изображении (соответствующий сигналу от эндометриальной ткани), которая окружена внутренней оболочкой с низким МР-сигналом на T2 изображении и высоким МР-сигналом на Т1 изображении.
Таким образом, диагноз ACUM ставится на основе данных в основном МРТ и подтверждается, когда выделенную дополнительную полость иссекают из матки с неизмененной основной полостью и придатками. Наличие дополнительной полости, выстланной эдометриальным эпителием с соответствующими железами и стромой, заполненной шоколадно-коричневой жидкостью, являются важными признаками ACUM. Размер полости, как правило, 2–4 см, чаще располагается у боковой стенки матки на уровне прикрепления круглой связки. По данным гистологического исследования для ACUM характерна концентрическая организация гладких мышц вокруг эндометрия дополнительной полости, чаще наблюдается у подростков и при микроскопическом исследовании напоминает матку. Основная полость матки и миометрий при данном состоянии не изменены, однако в миометрии самого ACUM в редких случаях может развиться аденомиоз из-за повышенного внутриполостного давления.
Узловая форма аденомиоза представляет из себя самый редкий вариант, характеризующийся кистозными образованиями, заполненными продуктами распада крови за счет постоянных локальных кровоизлияний. При морфологическом исследовании очаг аденомиоза обычно появляется в миометрии в виде скоплений небольших кистозных пространств, заполненных кровью, которые имеют диаметр обычно менее 5 мм. При гистологическом исследовании кистозная аденомиома состоит из желез эндометрия, окруженных стромой эндометриального типа и гладкой мускулатурой, но не имеет подобной матке организации, которая обнаружена при ACUM [4].
Все рассмотренные состояния требуют оперативного лечения. Пациентам с маточным рогом, узловой формой аденомиоза и ACUM рекомендовано удаление образования лапароскопическим доступом. Peters A. et аl. была описана лапароскопическая резекция ACUM с использованием двух различных методов в зависимости от желания пациентки сохранить фертильность. В обоих случаях первоначально производили инъекцию вазопрессина в серозную оболочку ACUM с гемостатической целью. У пациентов, желающих сохранить фертильность, с помощью монополярного коагулятора производили разрез вдоль серозной оболочки ACUM, тем самым облегчая его расслоение. Следующим этапом по окружности вдоль ACUM и на границе эндометрий-миометрий c использованием моно- и биполярной коагуляции производили энуклеацию ACUM. В отличие от лейомиом, где расслоение происходит вдоль псевдокапсулы, ACUM имеет плохо очерченные границы с дезорганизованными мышечными волокнами, что затрудняет его выделение. На последнем этапе ACUM пересекается от места его прикрепления к миометрию матки. В случае, если пациентка не была заинтересована в сохранении фертильности, авторами представлен ход операции путем проведения сальпингэктомии и освобождения ACUM из листьев широкой связки с использованием монополярного электрода с L-образным крюком для отделения ACUM от оставшегося тела матки [16].
Kiyak H. et al. [17] описали лапароскопическое удаление узловой формы аденомиоза в правом трубном углу матки. При лапароскопии была выявлена полость с шоколадно-коричневой жидкостью внутри. Изначально это образование («масса») было диагностировано как внематочная беременность, но при более тщательном осмотре выглядела как узел миомы с дегенерацией. Поскольку вокруг образования не было псевдокапсулы, был поставлен диагноз «очаговый узловой аденомиоз». Очагов эндометриоза не наблюдалось. Образование было рассечено по середине на две половины до слоя здорового миометрия. Далее полостное маточное образование было полностью резецировано, ложе ушито.
Таким образом, несмотря на различия в структуре ACUM и узлового аденомиоза, сохраняются трудности в дифференциальной диагностике образований. В литературе с 1998 г. описаны 25 случаев JCA у подростков, из них только 2 случая с образованиями более 5 см в диаметре [18–20].
Мы представляем серию клинических наблюдений дифференциальной диагностики и ведения пациенток подросткового возраста с различными вариантами аномалии мюллеровых протоков: ACUM и полного удвоения матки с наличием маточного рудимента.
Клиническое наблюдение № 1
В кабинет гинеколога детей и подростков научно-поликлинического отделения ФГБУ «НМИЦ АГП им. В.И. Кулакова» Минздрава России в марте 2019 г. обратилась девочка 17 лет с жалобами на резкую боль с 1-го по 5-й день менструации, с нарастанием интенсивности болевого синдрома в последние 6 месяцев.
Из анамнеза пациентки известно, что менархе наступило в 12 лет, через два года менструации стали болезненными. В связи с выраженным болевым синдромом находилась в стационаре по месту жительства с диагнозом: подострый сальпингоофорит. Порок развития половых органов с нарушением оттока менструальной крови – замкнутый функционирующий рудиментарный маточный рог справа диаметром 5 см. Для проведения оперативного лечения была рекомендована госпитализация в плановом порядке в Центр.
При поступлении в стационар состояние оценено как удовлетворительное. Девочку беспокоит боль внизу живота больше справа. Физическое и половое развитие соответствует возрасту. Наружные половые органы сформированы соответственно возрасту и полу. Клитор не увеличен. Уретра расположена типично. Гимен бахромчатый, цел. При ректо-абдоминальном исследовании тело матки в anteflexio, увеличено до 5 см, деформировано в области правого ребра, чувствительное при пальпации. Придатки матки слева без пальпаторных изменений, справа область придатков болезненная при пальпации. Точки выхода тазовых нервов при пальпации безболезненны.
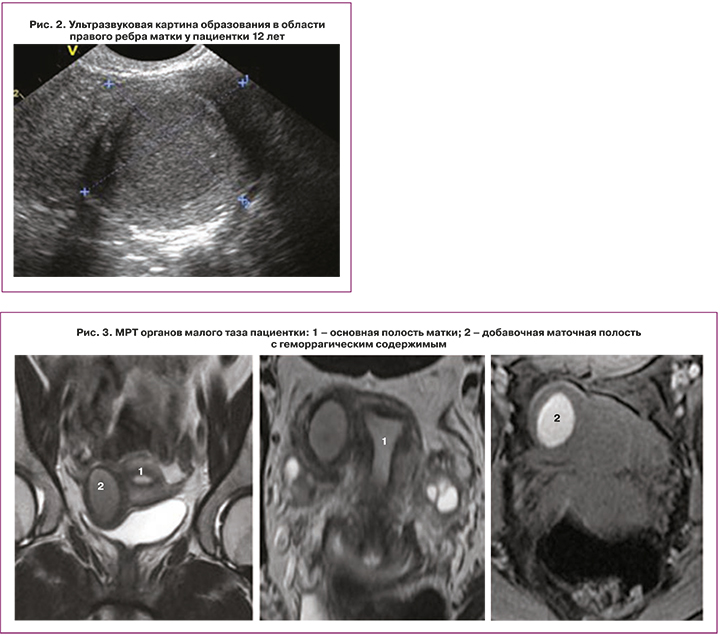
По данным УЗИ органов малого таза (рис. 2) матка расположена срединно, положение anteflexio, контуры ровные, четкие. Размер тела матки составляет 38×29×32 мм, шейки – 30×27 мм. Шеечно-маточный угол выражен. Эхо-структура миометрия не изменена. Эндометрий 7,5 мм, однородный. Яичники расположены в углах матки. Правый яичник размерами 35×17×24 мм, V=7,5 см3, эхо-структура не изменена, содержит фолликулы диаметром 7–8 мм, а также кистозную структуру округлой формы 19х15 мм с однородным мелкодисперсным изоэхогенным аваскулярным содержимым. Левый яичник размерами 26×17×21 мм, V=4,86 см3, эхо-структура не изменена, содержит фолликулы диаметром 5-7 мм, 6–8 в срезе. К правому ребру матки интимно прилежит образование округлой формы, диаметром 55×37×35 мм, с утолщенной до 6,2 мм изоэхогенной стенкой и полостью до 28 мм в диаметре с достаточно однородным содержимым. Эхографическое заключение: Эхо-картина функционирующей двурогой матки с замкнутым рогом справа. Эндометриоидная киста яичника справа.
По данным МРТ (рис. 3) органов малого таза визуализировано объемное образование 5–6 см в диаметре с полостью в области правого ребра матки, не сообщающееся с полостью матки, наиболее соответствует ACUM, следует дифференцировать с кистозным очагом аденомиоза. Кроме того, обнаружено кистозное включение в правом яичнике 1,5 см в диаметре, которое наиболее соответствует кисте желтого тела с кровоизлиянием.
Выполнена операция: Лапароскопия, иссечение образования ACUM без вскрытия полости матки, метропластика. Иссечение и коагуляция очагов наружного генитального эндометриоза (рис. 4). В ходе лапароскопической операции визуализировалось тело матки размерами 8,0×4,5×4,0 см, деформированное ближе к правому трубному углу большим образованием 5×6 см, исходящим из передне-боковой стенки матки. Правая маточная труба просматривалась на всем протяжении нормальной окраски, фимбриальный отдел свободен, фимбрии выражены, труба проходила по задней стенке аденомиозного узла. Правый яичник без видимой патологии размерами 3,0×4,0×3,4 см, имелось желтое тело со стигмой. Левая маточная труба просматривалась на всем протяжении нормальной окраски, фимбриальный отдел свободен, фимбрии выражены. Левый яичник был размерами 3,5×2,7×3,3 см с капсулой белесоватой окраски. На правой и левой крестцово-маточных связках, в Дугласовом пространстве, на брюшине пузырно-маточного углубления обнаружены множественные очаги эндометриоза 0,2–0,5 мм.
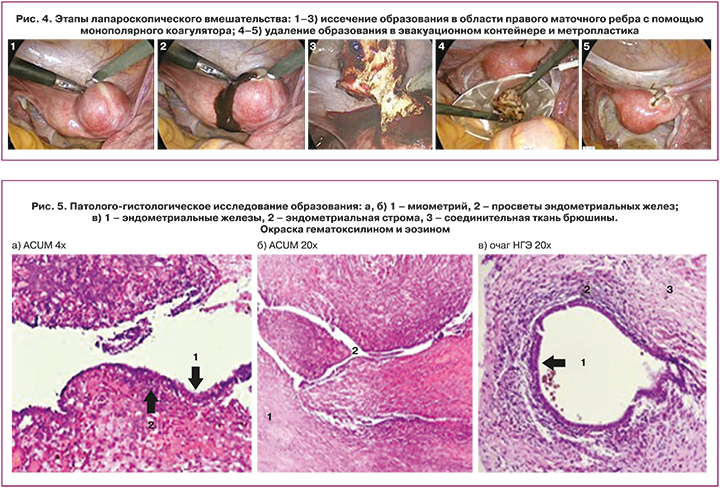
После предварительной коагуляции ткань матки над образованием рассечена, излилось 20 мл шоколадного содержимого, тупо и остро образование ACUM иссечен в пределах визуально здоровых тканей без вскрытия полости матки, удален через левое троакарное отверстие. Произведена метропластика с ушиванием ложа узла нитью «Велок» и иссечение, коагуляция очагов эндометриоза крестцово-маточных связок слева и справа, ретроцервикальной области и пузырно-маточного пространства.
Хирургический диагноз: ACUM. Наружный генитальный эндометриоз.
По результатам патоморфологического исследования в очагах НГЭ выявлены железы эндометриального типа с окружающей цитогенной стромой в фиброзно-жировой ткани (рис. 5). В узле ACUM описаны железы эндометриального типа с окружающей цитогенной стромой и гипертрофией окружающей гладкомышечной ткани. Патологогистологическое заключение (диагноз): ACUM. Инфильтративный эндометриоз мягких тканей малого таза.
Пациентка выписана в удовлетворительном состоянии.
Рекомендовано проведение повторного УЗИ спустя 30 дней после операции, указана необходимость контроля менструального цикла и консультации гинеколога. При контрольном визите через месяц с данными УЗИ патологии матки и ее придатков не обнаружено, менструация возобновилась через 30 дней от наблюдаемой в стационаре после операции, безболезненна.
Клиническое наблюдение № 2
В июле 2020 г. в Центр поступила девочка 17 лет с жалобами на боль в нижних отделах живота в течение 2 лет, резко болезненные менструации, требующие приема анальгетиков. По месту жительства проводилось лечение комбинированным оральным контрацептивом «Силуэт» в течение 5 месяцев в непрерывном режиме, однако пациентка отмечала усиление болей на фоне лечения.
В ходе анализа медицинской документации по данным МРТ по месту жительства в матке выявлено шаровидное образование с центральной полостью с четкими контурами, заполненное геморрагическим содержимым, диаметром 22,4×26,0×24,9 мм, не сообщающееся с основной полостью матки. Представленные данные наиболее свидетельствуют о наличии порока развития мюллеровых протоков ACUM, дополнительная маточная полость, что требует дифференциальной диагностики с рудиментарным функционирующим маточным рогом и узловой формой аденомиоза.
При поступлении пациентки в стационар состояние оценено как удовлетворительное. Наружные половые органы сформированы соответственно возрасту и полу. Клитор не увеличен. Уретра расположена типично. Гимен бахромчатый. При ректальном осмотре тело матки увеличено в размерах, плотно-эластической консистенции, умеренно подвижное. Придатки матки слева не пальпируются. Справа придатки увеличены в размерах до 6 см, туго-эластической консистенции, подвижные. Область выхода тазовых нервов безболезненна.
По данным УЗИ органов малого таза матка расположена срединно, положение anteflexio, контуры ровные, четкие. Размеры матки: тело 47×31×41 мм, шейка 32×21 мм. Шеечно-маточный угол выражен. Эхо-структура миометрия не изменена. Эндометрий 8,2 мм, однородный. Яичники расположены в углах матки. Правый яичник размерами 33×20×18 мм, V=9,6 см3. Эхо-структура не изменена, содержит желтое тело диаметром 20×19 мм. Левый яичник размерами 30×16×18 мм, V=4,5 см3. Эхо-структура не изменена, содержит фолликулы диаметром 5–7 мм, 6–8 в срезе. В проекции левого ребра матки определяется образование округлой формы диаметром 23×20×16 мм с полостью диаметром до 7,8 мм – замкнутый рог. Свободной жидкости не выявлено. Картина соответствует двурогой матке с замкнутым функционирующим левым рогом.
По данным МРТ органов малого таза в левом ребре матки, в области отхождения круглой связки определяется образование округлой формы с четкими контурами, размерами 2,6×2,3×2,5 см, с наличием в центральных отделах замкнутой полости размером 1,5×1,4×1,3 см, заполненной неоднородным геморрагическим содержимым. Толщина интактного миометрия левого ребра матки (между вышеописанным образованием и полостью матки) 0,5 см. Истмический отдел левой маточной трубы расположен по верхнему контуру данного образования. На остальном протяжении левая маточная труба не визуализируется. Картина соответствует пороку развития мюллеровых протоков ACUM.

Пациентке было проведено хирургическое вмешательство под эндотрахеальной анестезией в объеме: лапароскопия, иссечение образования ACUM без вскрытия полости матки, метропластика (рис. 6). В ходе лапароскопической операции визуализировалось тело матки размерами 6,0×4,5×4,0 см, деформированное образованием ACUM размера 3×3 см ближе к левому трубному углу, которое исходило из передне-боковой стенки матки. После предварительной эндокоагуляции было произведено рассечение ткани матки над образованием, излилось 10 мл шоколадного содержимого, тупо и остро очаг аденомиоза был иссечен в пределах визуально здоровых тканей без вскрытия полости матки, удален через левое троакарное отверстие. Ложе узла было тщательно коагулировано. На конечном этапе операции произведена метропластика с ушиванием ложа узла викриловыми швами.
Хирургический диагноз: порок развития внутренних половых органов. Аномалия развития мюллеровых протоков ACUM.
По результатам патоморфологического исследования узел ACUM размером 2×2×1 см, плотной консистенции, белесовато-серого цвета, на наружной поверхности с признаками коагуляции. Узел представлен фрагментами миометрия с наличием эндометриоидных гетеротопий, представленных эндометриоидной стромой и эндометриоидным эпителием. По результатам иммуногистохимичсекого исследования выявлена экспрессия эстрогеновых рецепторов (SP1, VENTANA): в строме – 6 баллов, в эпителии – 5 баллов. Экспрессия прогестероновых рецепторов (1E2, VENTANA): в строме – 6 баллов, в эпителии – 2 балла (по Allred). Патологоанатомическое заключение: ACUM. Эндометриоз матки.
Пациентка выписана в удовлетворительном состоянии под наблюдение гинеколога поликлиники по месту жительства. Родителям девочки даны рекомендации проведения повторного УЗИ органов малого таза через 1 и 3 месяца по месту жительства. Повторный прием в Центре через 3 месяца с результатами УЗИ органов малого таза и анализа крови на СА-125 натощак в Центре.
Клиническое наблюдение № 3
В сентябре 2020 г. поступила девочка 13 лет для оперативного лечения с жалобами на тянущие боли внизу живота.
По результатам обследования у пациентки с 11 лет по данным УЗИ сформировано подозрение на объемное образование тела матки, состоящее из жировой ткани, подозрение на лейомиому или миому матки с вторичными изменениями в узле. На МРТ от 28.05.2019 выявлено кистозное образование малого таза с кровоизлиянием, присутствие характерного МР-сигнала эндометриоидного внутреннего содержимого. На УЗИ от 07.07.2020 по задней стенке мочевого пузыря визуализируется гиперэхогенное образование 15×14 мм с кровотоком при цветовом допплеровском картировании, подозрение на очаговый эндометриоз, подозрение на миому матки.
При поступлении в стационар состояние оценено как удовлетворительное. Физическое и половое развитие соответствует возрасту.
Наружные половые органы сформированы соответственно возрасту и полу. Оволосение по женскому типу. Клитор не увеличен. Уретра расположена типично. Гимен бахромчатый, цел. Выделения слизистые, скудные. При ректальном осмотре тело матки увеличено в размерах до 7 см, плотное, подвижное, чувствительно при пальпации и тракции. Придатки матки слева не пальпируются. Придатки матки справа не пальпируются. Область выхода тазовых нервов безболезненна.
По данным УЗИ от 22.09.2020 на 7-й день первого менструального цикла матка расположена срединно, положение anteflexio, контуры ровные, четкие. Размеры тела матки 40×33×40 мм, шейка – 29×21 мм. Шеечно-маточный угол выражен. Эндометрий 4,3 мм. Яичники расположены в углах матки. Правый яичник размерами 37×20×21 мм, V=8,4 см3. Эхо-структура не изменена, содержит фолликулы диаметром 5–8 мм, 6–8 в срезе. Левый яичник размерами 30×24×34 мм, V=10,8 см3. Эхо-структура не изменена, содержит фолликулы, максимальный диаметром 13,5 мм, 6–8 в срезе. В толще передней стенки миометрия сохраняется включение овальной формы высокой эхогенности общим размером 29×12×26 мм, с четкими зазубренными краями, анэхогенной щелевидной полостью внутри. Кровоток выражен незначительно по периферии. Свободной жидкости не выявлено. Заключение: образование передней стенки миометрия (очаговая форма аденомиоза? ACUM?).

Пациентке была выполнена операция лапароскопия, адгезиолиз, иссечение ACUM, метропластика, диагностическая гистероскопия (рис. 7). В ходе лапароскопической операции тело матки размерами 8,0×4,5×4,0 см шаровидной формы, подпаяно к передней брюшной стенке и мочевому пузырю. Тупым путем произведено разделение спаек между передней поверхностью матки и брюшной стенкой и мочевым пузырем. При разделении спаек вскрылась полость между спайками и образованием, из которого выделяется белесоватая жидкость и детрит, взят посев на микробиологическое исследование. Тупо и остро с помощью гармонических ножниц рассечена брюшина пузырно-маточной складки, мобилизован мочевой пузырь до шейки матки.
Образование деформирует переднюю стенку матки, размерами 4×5 см. С помощью гармонического скальпеля произведено иссечение образования тупо и остро в пределах визуально здоровых тканей без вскрытия полости матки. Ложе узла тщательно коагулировано. Произведена метропластика с ушиванием ложа узла отдельными викриловыми швами.
Образование удалено абластично в эвакуационном контейнере через троакарное отверстие в области пупка. При диагностической гистероскопии обнаружено, что в куполе влагалища визуализируется шейка матки цилиндрической формы с участком эктопии. Полость матки треугольной формы, не увеличена, не деформирована. Эндометрий розового цвета, неравномерной толщины с участками гиперемии и гиперплазии. Устья маточных труб с обеих сторон доступны осмотру.
Хирургический диагноз: порок развития внутренних половых органов. Аномалия развития мюллеровых протоков ACUM. Аденомиоз. Спаечный процесс в малом тазу.
По результатам патологоанатомического исследования фрагмент ткани с маркировкой «маточный рог» 2,0×1,5 см, плотный белесый – 1 кусочек. В присланном материале фрагмент мышечной ткани с признаками коагуляционного воздействия, с инфильтрацией лимфоцитами вокруг сосудов на некоторых участках, без полости.
Патолого-гистологическое заключение: данная морфологическая картина не противоречит клиническому диагнозу «маточный рог».
Пациентка выписана в удовлетворительном состоянии под наблюдение гинеколога поликлиники по месту жительства.
Клиническое наблюдение № 4
Девочка 14 лет поступила с диагнозом: порок развития внутренних половых органов, удвоение матки с замкнутым функционирующим рудиментарным маточным рогом слева. Пациентка жаловалась на выраженные боли, усиливающиеся в дни менструации, неэффективность обезболивающей терапии и терапии по месту жительства.
При поступлении в стационар состояние оценено как удовлетворительное. Физическое и половое развитие соответствует возрасту. Наружные половые органы сформированы соответственно возрасту и полу. Оволосение по женскому типу. Клитор не увеличен. Уретра расположена типично. Гимен бахромчатый. При ректальном осмотре тело матки увеличено в размерах, плотно-эластической консистенции, умеренно подвижное. Придатки матки справа не пальпируются. В области придатков слева пальпируется образование туго-эластической консистенции, подвижное, чувствительное в размерах до 9 см. Область выхода тазовых нервов безболезненна.
По данным УЗИ органов малого таза матка расположена срединно, положение anteflexio, контуры ровные, четкие. Размеры матки: тело 42×23×37 мм, шейка 34×19 мм. Шеечно-маточный угол выражен. Эхо-структура миометрия не изменена. Эндометрий 6,3 мм, однородный. Яичники расположены в углах матки. Правый яичник размерами 32×13×22 мм, V=4,8 см3. Эхо-структура не изменена, содержит фолликулы диаметром 4-7 мм, 4-6 в срезе. Левый яичник размерами 35×14×18 мм, V=4,7 см3. Эхо-структура не изменена, содержит фолликулы диаметром 4–11 мм, 4–6 в срезе. Интимно к ребру матки слева прилежит образование округлой формы 37×29×35 мм, с полостью 18 мм, с неоднородным изоэхогенным содержимым – замкнутый рог.
По данным МРТ органов малого таза по левому ребру тела матки определяется рудиментарный рог матки, размерами 2,9×3,5×3,2 см, с наличием в центре замкнутой эндометриоидной полости максимальным размером 1,6 см, заполненной геморрагическим содержимым. В полости малого таза определяется небольшое количество свободной жидкости. МР-картина соответствует пороку развития внутренних половых органов: однорогая матка с рудиментарным замкнутым функционирующим рогом слева.

Выполнена операция: Лапароскопия, удаление замкнутого функционирующего маточного рога слева, метропластика правой матки (рис. 8). Размеры левого маточного функционирующего рога, исходящего из левой боковой стенки матки, составляют 4,0×3,5×3,0 см, левая маточная труба и яичник без видимой патологии размерами 2,5×1,5×1,4 см. Правая матка шаровидной формы, размерами 5,0×6,0×4,5 см. Левый яичник размерами 2,8×2,1×1,9 см и труба без особенностей. С помощью биполярного коагулятора и ножниц рассечена широкая связка слева, круглая связка и собственная связка яичника коагулированы и отсечены. Рог выделен до предполагаемого цервикса, клиновидно высечен из стенки правой матки и удален. Выполнена пластика стенки матки путем наложения трех Z-образных викриловых швов. Иссеченный рог удален через левое троакарное отверстие. Хирургический диагноз: порок развития внутренних половых органов. Двурогая матка с функционирующим замкнутым рудиментарным левым рогом. Гематометра слева.
По результатам патологоанатомического исследования левая маточная труба размерами 2,5×0,5 см, фимбрии спаяны, у фимбриального отдела гидатида диаметром 0,7 см, маточный рог размерами 4,5×2,5×2 см, на разрезе содержит полость диаметром 2 см, заполнена кровью.
Рудиментарный маточный рог представлен мышечной тканью с расширенными полнокровными сосудами. Миометрий на одном из участков покрыт эндометрием, представленным цитогенной стромой со старыми и свежими кровоизлияниями. Маточная труба атрофичная, складки эндосальпингса сглажены, стенка маточной трубы с рассеянной лимфоидной инфильтрацией. Гидатида с тонкой фиброзной стенкой, выстлана призматическим эпителием.
По результатам иммуногистохимического исследования выявлена экспрессия эстрогеновых рецепторов (SP1, VENTANA): в строме – 5 баллов, в эпителии – негативная (по Allred), экспрессия прогестероновых рецепторов (1E2, VENTANA): в строме – 6 баллов, в эпителии – негативная (по Allred).
Патологоанатомическое заключение: морфологическая картина не противоречит клиническому диагнозу «Замкнутый функционирующий рудиментарный маточный рог слева. Гидатида слева».
Пациентка выписана в удовлетворительном состоянии.
Клиническое наблюдение № 5
В марте 2019 г. во 2-е гинекологическое отделение поступила девочка 16 лет с жалобами на болезненные менструации. По месту жительства наблюдалась с диагнозом: порок развития половых органов, двурогая матка с добавочным рудиментарным рогом справа, гематометра, в связи с чем в декабре 2016 г. была проведена лапароскопическая операция по удалению добавочного рога матки.
При поступлении в стационар состояние оценено как удовлетворительное. Девочку беспокоит боль внизу живота во время менструации. Наружные половые органы сформированы соответственно возрасту и полу. Оволосение по женскому типу. Клитор не увеличен. Уретра расположена типично. Гимен бахромчатый. При ректальном осмотре тело матки увеличено в размерах, плотно-эластической консистенции, умеренно подвижное, чувствительные при пальпации. Придатки матки слева: не пальпируются. Справа придатки увеличены в размерах, туго-эластической консистенции, подвижные. Область выхода тазовых нервов безболезненна.
 По данным УЗИ органов малого таза (рис. 9) матка отклонена влево, положение anteflexio, контуры ровные, четкие. Размеры матки: тело 46×29×32 мм, шейка 22×22 мм. Шеечно-маточный угол выражен. Эхо-структура миометрия не изменена. Эндометрий 10,8 мм, однородный. Яичники расположены в углах матки. Правый 38×20×33 мм, V=12,94 см3. Эхо-структура не изменена, содержит фолликулы 7–8 мм, а также кистозную структуру округлой формы 19×15 мм с однородным мелкодисперсным изоэхогенным аваскулярным содержимым. Левый 38×25×33 мм, V=15,88 см3. Эхо-структура не изменена, содержит фолликулы 5–7 мм, 6–8 в срезе. К правому ребру матки интимно прилежит образование овальной формы размерами 47×31×35 мм, с неравномерно утолщенной до 6,5–14 мм, гипоэхогенной стенкой и полостью до 22×18 мм в диаметре, с несколько неоднородным по структуре содержимым за счет более эхогенного слоя у стенок. Свободная жидкость выявлена в умеренном количестве справа и позади матки. Заключение по данным УЗИ: состояние после удаления замкнутого рога справа (в анамнезе). Эхо-признаки очаговой формы аденомиоза правой стенки матки или нерадикально резецированного правого маточного рога. Окончательный клинический диагноз: Порок развития мочеполовых органов. Двурогая матка с замкнутым функционирующим маточным рогом справа, спаечный процесс в малом тазу, пациентке рекомендовано оперативное вмешательство.
По данным УЗИ органов малого таза (рис. 9) матка отклонена влево, положение anteflexio, контуры ровные, четкие. Размеры матки: тело 46×29×32 мм, шейка 22×22 мм. Шеечно-маточный угол выражен. Эхо-структура миометрия не изменена. Эндометрий 10,8 мм, однородный. Яичники расположены в углах матки. Правый 38×20×33 мм, V=12,94 см3. Эхо-структура не изменена, содержит фолликулы 7–8 мм, а также кистозную структуру округлой формы 19×15 мм с однородным мелкодисперсным изоэхогенным аваскулярным содержимым. Левый 38×25×33 мм, V=15,88 см3. Эхо-структура не изменена, содержит фолликулы 5–7 мм, 6–8 в срезе. К правому ребру матки интимно прилежит образование овальной формы размерами 47×31×35 мм, с неравномерно утолщенной до 6,5–14 мм, гипоэхогенной стенкой и полостью до 22×18 мм в диаметре, с несколько неоднородным по структуре содержимым за счет более эхогенного слоя у стенок. Свободная жидкость выявлена в умеренном количестве справа и позади матки. Заключение по данным УЗИ: состояние после удаления замкнутого рога справа (в анамнезе). Эхо-признаки очаговой формы аденомиоза правой стенки матки или нерадикально резецированного правого маточного рога. Окончательный клинический диагноз: Порок развития мочеполовых органов. Двурогая матка с замкнутым функционирующим маточным рогом справа, спаечный процесс в малом тазу, пациентке рекомендовано оперативное вмешательство.
Было выполнено лапароскопическое вмешательство, разделение спаек, удаление нерадикально резецированного функционирующего маточного рога справа, метропластика, диагностическая гистероскопия. Во время лапароскопического вмешательства визуализировалась тело матки размерами 8,0×4,5×4,0 см деформировано ближе к правому трубному углу большим образованием 5×6 см, исходящим из верхне-боковой стенки матки. Правая маточная труба удалена при предыдущей операции по поводу удаления правого маточного рога. Правый яичник без видимой патологии размерами 3,0×4,0×3,4 см. Левая маточная труба просматривается на всем протяжении нормальной окраски, фимбриальный отдел свободен, фимбрии выражены. Левый яичник размерами 3,5×2,7×3,3 см с капсулой белесоватой окраски. В ходе гистероскопического исследования в куполе влагалища визуализируется шейка матки цилиндрической формы, слизистая цервикального канала складчатая, полость матки однорогая, эндометрий бледно-розового цвета, равномерной толщины (тонкий), устье маточной трубы визуализировано слева одно, без особенностей, второе устье трубы не визуализировано.
После предварительной эндокоагуляции ткань матки над образованием рассечена, излилось 7 мл шоколадного содержимого, тупо и остро нерадикально иссеченный маточный рог иссечен в пределах визуально здоровых тканей без вскрытия полости матки, удален через левое троакарное отверстие. Ложе узла тщательно коагулировано. Произведена метропластика с ушиванием ложа узла нитью «Велок». Хирургический диагноз: Порок развития половых органов. Полное удвоение матки. Нерадикально резецированный замкнутый функционирующий маточный рог справа.
По данным гистологического исследования материал представлен фрагментом миометрия с полостью, выстланной эндометрием в фазе поздней секреции. Морфологическая картина соответствует функционирующему маточному рогу.
Пациентка выписана в удовлетворительном состоянии под наблюдение гинекологом поликлиники по месту жительства. Родителям девочки даны рекомендации повторного УЗИ спустя месяц на 5–7-й день менструального цикла, повторный прием в Центре через месяц с результатами УЗИ органов малого таза для решения вопроса о дальнейшем ведении.
Заключение
Таким образом, по мнению многих авторов, дополнительные изолированные полости матки и изолированные кистозные аденомиомы относятся к одной и той же патологии ACUM, важной особенностью которой является нахождение в толще матки, не сообщающейся с основной, добавочной полости. При этом интактная маточная полость правильной формы и устья маточных труб доступны визуализации с обеих сторон. На основе приведенных клинических исследований важное значение имеет дифференцированное ведение таких пациентов, использование МРТ, с помощью которой можно поставить точный диагноз. В то время как аномалия развития мюллеровых протоков с удвоением матки и замкнутым функционирующим маточным рудиментом имеет особенности, как по УЗИ и МРТ, так и при лапароскопическом вмешательстве. По данным визуализации маточный рудимент нередко представлен отдельным образованием у ребра матки или отдельно от матки, маточная полость имеет вид однорогой, визуализируется одно устье маточной трубы, при лапароскопии маточная труба отходит от маточного рудимента. Повышенная осведомленность о диагностике ACUM способствует выбору оптимального лечения и ведения таких пациенток уже на ранних этапах.



