The impact of Fast Track Surgery technology on the outcomes of laparoscopic non‑hysterectomy interventions
Volkov O.A., Shramko S.V., Marchenko E.E., Karapetyan A.J., Vlasenko A.E.
Minimally invasive laparoscopic surgery and Fast Track Surgery (FTS) program for patients have had a significant impact on perioperative management and have practically replaced the practice of traditional management. This raises the question of whether long-term inpatient treatment is required.
Objective: To evaluate the protective effect of FTS technology in laparoscopic non-hysterectomy interventions in elective patients.
Materials and methods: This prospective cohort study included gynecological patients who underwent elective laparoscopic organ-preserving surgery for benign neoplasms (uterine fibroids, benign ovarian neoplasms, endometriosis, and chronic salpingitis). The study included 312 operated patients: 247 – in the Fast Track Surgery program (FTS, main group) and 65 – in traditional care (TC, control group). Data for the study were obtained from the electronic databases of the full-cycle medical information systems "Ariadna" and "Medialog" for the years 2021–2023. The primary criteria for evaluating the effectiveness of FTS technology were complications in the early postoperative period and time of patient discharge. Additionally, the dynamics of some laboratory parameters in the study groups were analyzed.
Results: The use of FTS technology led to a decrease in the length of hospital stay (RR=0.06, 95% CI: 0.03–0.11), frequency of nausea and vomiting in the postoperative period (RR=0.04, 95% CI: 0.002–0.69), and surgical site infections (RR=0.05, 95% CI: 0.002–1.00).
Conclusion: The use of FTS program in combination with minimally invasive laparoscopic gynecologic surgery for elective patients who underwent surgery for benign neoplasms of the uterus and appendages significantly reduced the incidence of postoperative complications and the duration of inpatient treatment, without increasing the frequency of rehospitalization.
Authors' contributions: Volkov O.A. – conception and design of the study; Volkov O.A., Marchenko E.E., Karapetyan A.J. – material collection and processing; Vlasenko A.E. – statistical analysis; Volkov O.A., Shramko S.V. – drafting of the manuscript; Shramko S.V. – editing of the manuscript.
Conflicts of interest: The authors have no conflicts of interest to declare.
Funding: There was no funding for this study.
Ethical Approval: The study was reviewed and approved by the Research Ethics Committee of the Novokuznetsk State Institute of Advanced Medical Training, Branch of Russian Medical Academy of Continuing Professional Education of the Ministry of Health of the Russian Federation on 2024-06-29.
Patient Consent for Publication: All patients provided informed consent for the publication of their data.
Authors' Data Sharing Statement: The data supporting the findings of this study are available upon request from the corresponding author after approval from the principal investigator.
For citation: Volkov O.A., Shramko S.V., Marchenko E.E., Karapetyan A.J., Vlasenko A.E. The impact of Fast Track Surgery technology on the outcomes of laparoscopic non-hysterectomy interventions.
Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2024; (9): 99-107 (in Russian)
https://dx.doi.org/10.18565/aig.2024.155
Keywords
The introduction of the Fast Track Surgery (FTS) program, along with minimally invasive laparoscopic surgery and multicomponent pain relief, has prompted reassessment of perioperative patient management and the need for long-term inpatient treatment [1–3]. The approach to patient management was successfully changed in cardiac surgery by Krohn B.G. et al. (1990) and Engelman R.M. et al. (1994) marked a significant milestone in this regard. Effective control of postoperative pain, nausea, and vomiting, as well as activating patients early and initiating oral nutrition promptly, can reduce the body's stress response and shorten hospital stays without increasing the risk of rehospitalization or postoperative complications [4, 5].
The core concept of the Fast Track Surgery program involves establishing a preoperative council of specialists (comprising anesthesiologists, gynecological surgeons, and therapists) to enhance patient awareness and optimize preoperative medical care [6]. By using carbohydrate drinks to prevent starvation, initiating oral nutrition early, foregoing routine bowel preparation, and minimizing sedative use, a significant positive impact on patient well-being was achieved, reducing the likelihood of bowel dysfunction and stress related to the procedure. Additionally, the use of laparoscopic access allows the avoidance of narcotic drugs in the postoperative phase and facilitates earlier patient activity [7, 8].
Despite the extensive evidence base and continuous advancements in surgical and anesthetic technologies, the practice of enhanced recovery, including Fast Track Surgery, has not yet been widely adopted. Many physicians still prefer the traditional approach of prolonged postoperative hospitalization, pointing to potential negative outcomes during the perioperative period.
This study aimed to determine the protective effect of Fast Track Surgery technology in laparoscopic non-hysterectomy interventions in elective patients.
Materials and methods
This prospective cohort study included 312 gynecological patients who underwent elective laparoscopic organ-preserving surgery for benign neoplasms (uterine fibroids, benign ovarian neoplasms, endometriosis, and chronic salpingitis) with 247 in the Fast Track Surgery program (FTS, study group) and 65 in traditional care (TC, control group).
Data for the study were obtained from the electronic databases of the full-cycle medical information systems "Ariadna" and "Medialog" for the years 2021–2023. The size of the groups was not calculated, and all the information available in the database was used.
The inclusion criteria were women over 18 years of age. The study group included laparoscopic non-hysterectomy surgical interventions for uterine fibroids, benign ovarian tumors, and fallopian tubes performed in the FTS program, and the control group included similar surgical interventions performed with TC patients. The exclusion criteria were age <18 years and the presence of a malignant neoplasm.
The primary criteria for assessing the effectiveness of the FTS technology were complications in the early postoperative period and the time of discharge of the patient from the hospital (early discharge, over 3 days, and over 7 days). All complications and the risk of developing individual complications were analyzed, including nausea and vomiting, infectious complications, bleeding, and phlebitis of the saphenous vein.
Additionally, analysis of the dynamics of laboratory parameters in the study groups was conducted, including erythrocytes, hemoglobin, hematocrit, leukocytes, leukocyte intoxication index (LII), glucose, and fibrinogen. All parameters were determined in women in both study groups immediately before the operation and on the day after the operation.
Statistical analysis
The normality of the distribution of continuous variables was tested using the Shapiro-Wilk test. Continuous variables were not normally distributed and were reported as median (Me) and interquartile range (Q3; Q1). Continuous variables between the two groups were compared using the nonparametric Mann–Whitney test (for unpaired samples) and the Wilcoxon test (for paired samples). When analyzing the dynamics of indicators, the delta of the indicator was also calculated, which was described by the median and its 95% confidence interval (CI). Categorical variables were compared using Pearson’s chi-squared (χ2) criterion. Fisher’s exact test was used when the expected frequency of one or more cells was less than five. To identify table cells that made a non-random contribution to the criterion statistics, Haberman's consistent standardized residuals with the Holm-Bonferroni correction were calculated [9]. As a measure of effect size, relative risks and their 95% CI were calculated; the effect size was calculated only in the case of statistically significant differences between the groups. In the presence of zero cells in the contingency table, Haldane–Anscombe correction was applied. Multivariate analysis and calculation of the adjusted relative risk were performed using modified Poisson regression [10]. Results were considered statistically significant at p<0.05. All calculations were performed using the R statistical environment (v.3.6, GNU GPL2 license).
Results
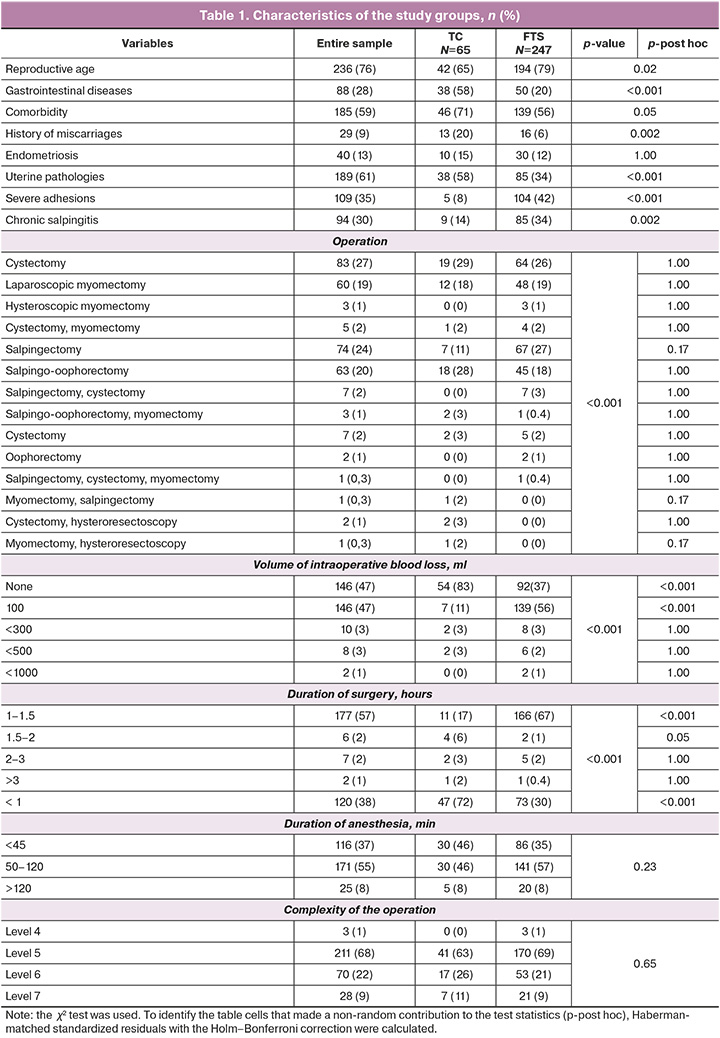
Patients in the FTS group were more likely to be of reproductive age (FTS – 194/247 (79%); TC – 42/65 (65%); p=0.02). They were less likely to have gastrointestinal diseases (FTS – 50/247 (20%); TC – 38/65 (58%); p<0.001), comorbidity (FTS – 139/247 (56%), TC – 46/65 (71%); p=0.05), uterine pathology (FTS – 85/247 (34%), TC – 38/65 (58%); p<0.001), and history of miscarriages (FTS – 16/247 (6%); TC – 13/65 (20%); p=0.002). Chronic salpingitis (FTS – 85/247 (34%); TC – 9/65 (14%); p=0.002) and severe adhesions (FTS – 104/247 (42%); TC – 5/65 (8%); p<0.001) were registered significantly more often than in the control group. The groups were comparable in terms of the complexity of surgical interventions. The most frequently performed operations were levels 6 and 7 (TC – 17/65 (26%); FTS – 53/247 (21%); p=0.65, and TC – 7/65 (11%), FTS – 21/247 (9%); p=0.65, respectively) (Table 1).
In the TC group, there was a statistically significant decrease in erythrocyte (p<0.001) and hemoglobin (p=0.001) levels after surgery; in the FTS group, these parameters remained unchanged (Table 2). It should be noted that the distribution of the variables relative to the reference range in the study groups did not differ before or after surgery; in most cases, the parameters were within the reference range (RR) in both groups (Table 3).
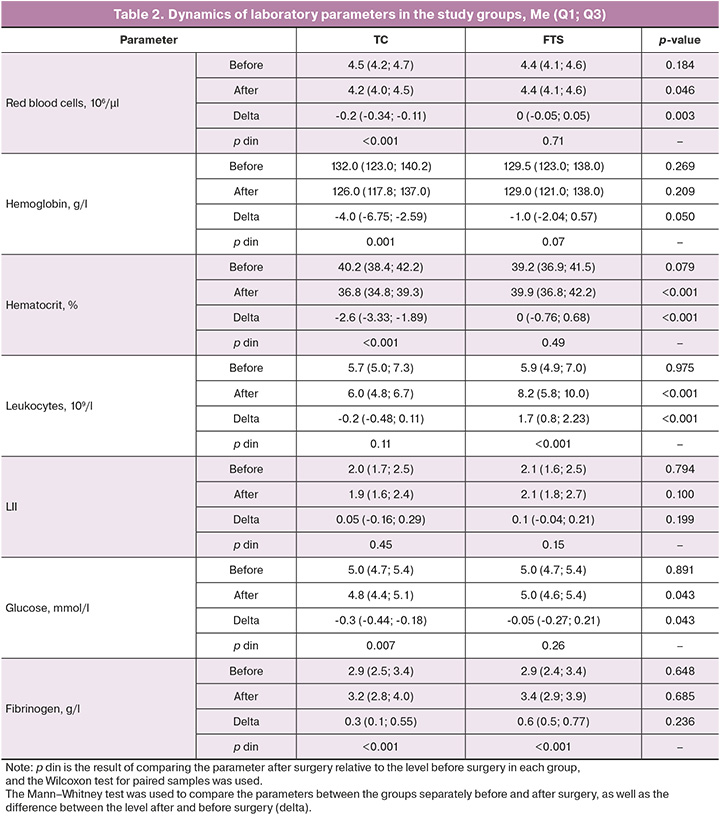
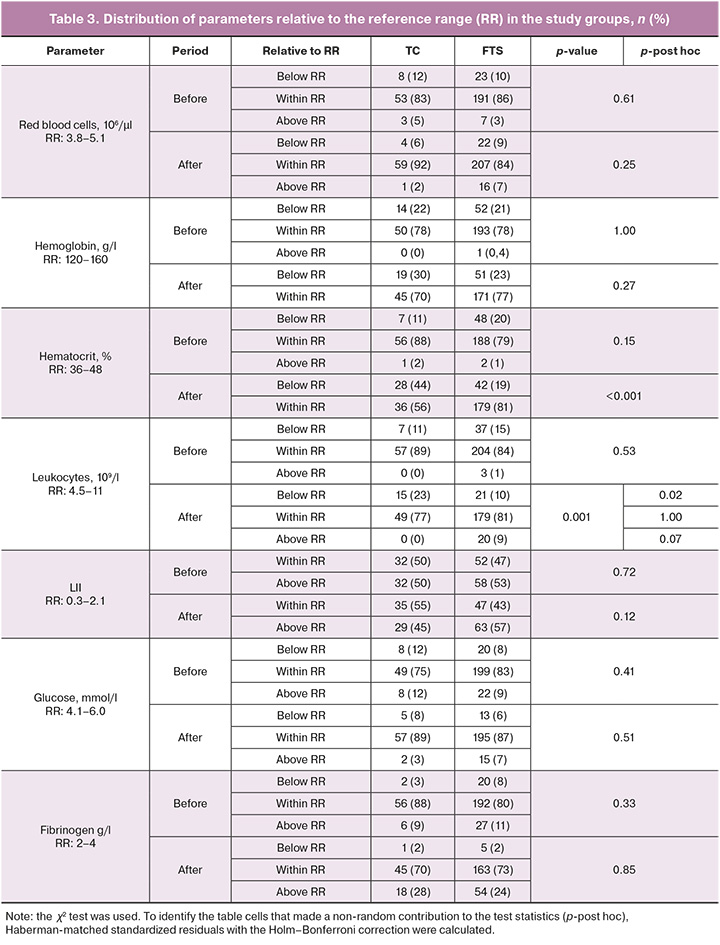
Hematocrit values in the TC group decreased significantly in the postoperative period compared with the preoperative values (p<0.001) and were also significantly lower than those in the FTS group (p<0.001). The delta of hematocrit changes in the study groups was also significantly different: -2.6 (-3.33; -1.89)% in the control group versus 0 (-0.76; 0.68)% in the FTS group (p<0.001). It is also worth noting that in the FTS group, most women (81% (179/221)) had a hematocrit within the normal range in the postoperative period, whereas in the TC group, 44% (28/64) of patients had a hematocrit below the reference values (p<0.001).
The leukocyte count in the FTS group after surgery was significantly higher (p<0.001) than that in the TC group.
When comparing the groups with a breakdown of the leukocyte level in relation to the normative range, it was found that the majority of women in both groups had leukocyte levels within the reference values in the postoperative period (77% (49/64) in the TC group and 81% (179/220) in the FTS group; p=1.00); the differences between the groups were due to a higher proportion of women with a decreased leukocyte count after surgery in the TC group (23% (15/64) vs. 10% (21/220) in the FTS group; p=0.02).
We found a significant decrease in glucose levels in the TC group after surgery (p<0.007), whereas they remained unchanged in the FTS group. The delta of glucose changes between the study groups also showed statistically significant differences (p=0.043).
Fibrinogen levels significantly increased after surgery in both groups. The intensity of the increase (delta of change) did not differ between groups.
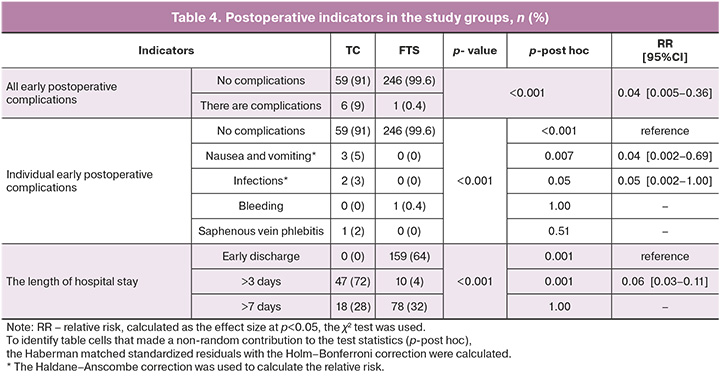
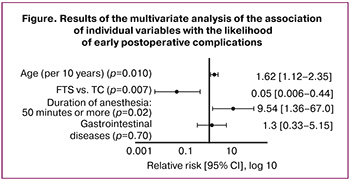
Analysis of the characteristics of the postoperative period showed that nausea and vomiting (3/65 (5%) vs. 0/247 in the FTS group; p=0.007) and surgical site infections (2/65 (3%) vs. 0/247 in the FTS group; p=0.05) were significantly more common in the TC group (Table 4). Patients in the FTS group were significantly more likely to be discharged early (159/247 (64%) vs. 0/65 in the TC group; p<0.001) and less likely to be discharged after three days (10/247 (4%) vs. 47/65 (72%) in the TC group; p<0.001). In addition, the FTS group had fewer postoperative complications than the TC group (1/247 (0.4%) vs. 6/65 (9%); p<0.001). Thus, FTS technology, compared with TC, showed a protective effect against the development of early postoperative complications (RR=0.04 [95% CI: 0.005–0.36]), including nausea and vomiting (RR=0.04 [95% CI: 0.002–0.69]) and infectious complications (RR=0.05 [95% CI: 0.002–1.00]). It was found that FTS technology reduced the frequency of hospital stay by more than 3 days in favor of earlier discharge (RR=0.06 [95% CI: 0.03–0.11]). Adjusted estimates of the relationship between the FTS technology and the risk of developing early postoperative complications were also obtained. The following confounders were considered: patient age, presence of gastrointestinal diseases, and duration of anesthesia (more or less than 50 min) (Figure). The choice of potential confounders was determined by the results of the univariate analysis, considering the literature data and the absence of multicollinearity of the input variables. It was found that the adjusted relative risk of complications (FTS relative to TC) was 0.05 [95% CI: 0.006–0.44]).
Discussion
The FTS program is key to reducing postoperative morbidity by addressing various factors that contribute to surgical stress, such as severe pain syndrome, immobilization, and extended fasting. Surgical trauma activates the sympathetic nervous system and triggers an inflammatory response, indicating the severity of surgical stress. Insulin resistance is a critical factor in determining the severity of surgical treatment and affects the surgical outcome [11]. Changes in insulin sensitivity after surgery affect metabolism, leading to alterations in glucose metabolism, development of hyperglycemia, and loss of protein, muscle mass, and strength [12]. Our study showed a significant decrease in blood glucose levels in the TC group. These changes are the result of traditional restrictive measures regarding nutrition and fluid intake in the perioperative period. The goal of these measures is to reduce the residual volume of gastric contents and acidity, as well as to prevent regurgitation and aspiration during anesthesia. However, this concept is controversial because prolonged fasting before surgery has been associated with a decrease in gastric pH, which increases the risk of aspiration [13].
Fluctuations in inflammatory markers (leukocytes and fibrinogen) can be explained by surgical stress and the release of counter-regulatory hormones (catecholamines, glucagon, cortisol, and growth hormones) and pro-inflammatory cytokines [11]. Although the leukocyte counts and fibrinogen levels in the study groups were within the reference values, further research is needed to study the combined effect of surgical technique, volume of surgical treatment, and anesthesia on the severity of the inflammatory response.
A decrease in erythrocyte count, hemoglobin levels, and hematocrit in the TC group may be partially explained by the inaccuracy of intraoperative blood loss assessment. In both groups, blood loss was estimated using a direct volumetric assessment method (measuring the volume of blood collected in a container on a milliliter scale during surgery). However, this method has a margin of error owing to the absorption of blood in the abdomen [14]. In the FTS group, more attention was given to standardized step-by-step performance of the operation, adherence to the principle of fascial space surgery, and the use of modern energy platforms for vessel ligation.
The FTS group experienced lower rates of postoperative nausea and vomiting than the TC group, owing to a range of patient-focused multimodal technologies that effectively reduce the incidence of these complications in high-risk patients. Uncontrolled nausea and vomiting can delay early discharge after surgery, lead to an early refusal to eat, and hinder mobility.
Conclusion
FTS technology is a reliable protective factor that significantly reduces the incidence of postoperative complications in patients undergoing elective minimally invasive non-hysterectomy surgery. This is achieved by addressing surgical stress, implementing a patient-centered approach to manage postoperative nausea and vomiting, and developing an individualized multicomponent postoperative analgesia strategy.
References
- Доброхотова Ю.Э., Лапина И.А., Тян А.Г., Таранов В.В., Чирвон Т.Г., Глебов Н.В., Кайкова О.В., Малахова А.А., Гомзикова В.М., Клаушук В.И. Программа ускоренного восстановления пациентов после лапароскопической коррекции пролапса тазовых органов. Гинекология. 2023; 25(2): 215-20. [Dobrohotova Yu.E., Lapina I.A., Tyan A.G., Taranov V.V., Chirvon T.G., Glebov N.V., Kaykova O.V., Malahova A.A., Gomzikova V.M., Klaushuk V.I. Accelerated recovery program for the patients after laparoscopic correction of pelvic organ prolapce. Gynecology. 2023; 25(2): 215-20. (in Russian)]. https://dx.doi.org/10.26442/20795696.2023.2.202178.
- Попов А.А., Идашкин А.Д., Тюрина С.С., Будыкина Т.С. Возможности использования программы ускоренного восстановления в коррекции течения послеоперационного периода при хирургическом лечении в гинекологии. Российский вестник акушера-гинеколога. 2019; 19(6): 23-30. [Popov A.A., Idashkin A.D., Tiurina S.S., Budykina T.S. Possibilities of using a fast track recovery program to correct a postoperative course after surgical treatment in gynecology. Russian Bulletin of Obstetrician-Gynecologist. 2019; 19(6): 23-30. (in Russian)]. https://dx.doi.org/10.17116/rosakush20191906123.
- Лисовская Е.В., Хилькевич Е.Г., Чупрынин В.Д., Мельников М.В., Филиппович Г.В. Протоколы ускоренного выздоровления после операции у пациенток с глубоким инфильтративным колоректальным эндометриозом. Акушерство и гинекология. 2019; 1: 34-41. [Lisovskaya E.V., Khilkevich E.G., Chuprynin V.D., Melnikov M.V., Filippovich G.V. Protocols for accelerated postoperative recovery in patients with deep infiltrating colorectal endometriosis. Obstetrics and Gynecology. 2019; (1): 34-41. (in Russian)]. https://dx.doi.org/10.18565/aig.2019.1.34-41.
- Krohn B.G., Kay J.H., Mendez M.A., Zubiate P., Kay G.L. Rapid sustained recovery after cardiac operations. J. Thorac. Cardiovasc. Surg. 1990; 100(2): 194-7.
- Bardram L., Funch-Jensen P., Jensen P., Crawford M.E., Kehlet H. Recovery after laparoscopic colonic surgery with epidural analgesia, and early oral nutrition and mobilisation. Lancet. 1995; 345(8952): 763-4.
- Fischer S.P. Development and effectiveness of an anesthesia preoperative evaluation clinic in a teaching hospital. Anesthesiology. 1996; 85(1):196-206. https://dx.doi.org/10.1097/00000542-199607000-00025.
- Jensen M.B., Houborg K.B., Nørager C.B., Henriksen M.G., Laurberg S. Postoperative changes in fatigue, physical function and body composition: an analysis of the amalgamated data from five randomized trials on patients under-going colorectal surgery. Colorectal Dis. 2011; 13(5): 588-93. https://dx.doi.org/10.1111/j.1463-1318.2010.02232.x.
- Пучков К.В., Коренная В.В., Подзолкова Н.М. Fast track: хирургические протоколы ускоренной реабилитации в гинекологии. Гинекология. 2015; 17(3): 40-5. [Puchkov K.V., Korennaya V.V., Podzolkova N.M. Fast track: surgical protocols of accelerated rehabilitation in gynecology. Gynecology. 2015; 17(3): 40-5. (in Russian)].
- Agresti A. Categorical data analysis. John Wiley & Sons; 2012.
- Zou G. A modified poisson regression approach to prospective studies with binary data. Am. J. Epidemiol. 2004; 159(7): 702-6. https://dx.doi.org/10.1093/aje/kwh090.
- Schricker T., Lattermann R., Carli F. Physiology and pathophysiology of ERAS. In: Ljungqvist O., Francis N., Urman R., eds. Enhanced Recovery After Surgery (ERAS). A Complete Guide to Optimizing Outcomes. Springer, Cham. 2020: 11-22. https://dx.doi.org/10.1007/978-3-030-33443-7_2.
- Moore F.D., Langohr J.L., Ingebretsen N.M., Cope O. The role of exudate losses in the protein and electrolyte imbalance of burned patients. Ann. Surg. 1950; 132(1): 1-19.
- Manjunath C.P., Pavan V.D., Prajwal B. Ultrasonographic estimation of gastric volume inpatients after overnight fasting and after ingestion of clear fluids two hours before surgery. Anaesthsia, Pain & Intensive Care. 2020; 24(3): 308-13. https://dx.doi.org/10.35975/apic.v24i3.1283.
- Межевикина В.М., Лазарев В.В., Жиркова Ю.В. Интраоперационные методы оценки кровопотери. Обзор литературы. Российский вестник детской хирургии, анестезиологии и реаниматологии. 2022; 12(3): 371-81. [Mezhevikina V.M., Lazarev V.V., Zhirkova Yu.V. Intraoperative methods for assessing blood loss: A review. Russian Journal of Pediatric Surgery, Anesthesia and Intensive Care. 2022; 12(3): 371-81. (in Russian]. https://dx.doi.org/10.17816/psaic991.
Received 04.07.2024
Accepted 09.08.2024
About the Authors
Oleg A. Volkov, MD, Teaching Assistant at the Department of Obstetrics and Gynecology, Novokuznetsk State Institute for Advanced Medical Training, branch of RMACPE, Ministry of Health of Russia, 5 Stroiteley Ave., Novokuznetsk, 654005, Russia, +7(996)332-98-08, volkovoa@icloud.com, https://orcid.org/0000-0002-3271-7167Svetlana V. Shramko, Dr. Med. Sci., Associate Professor, Professor at the Department of Obstetrics and Gynecology, Novokuznetsk State Institute for Advanced Medical Training, branch of RMACPE, Ministry of Health of Russia, Ministry of Health of Russia, 5 Stroiteley Ave., Novokuznetsk, 654005, Russia, +7(3843)324-750,
shramko_08@mail.ru, https://orcid.org/0000-0003-1299-165X
Ekaterina E. Marchenko, Clinical Resident at the Department of Obstetrics and Gynecology, Novokuznetsk State Institute for Advanced Medical Training, branch of RMACPE, Ministry of Health of Russia, 5 Stroiteley Ave., Novokuznetsk, 654005, Russia, +7(900)058-78-05, e.e.marchenko@internet.ru, https://orcid.org/0009-0002-7244-202X
Armine J. Karapetyan, Clinical Resident at the Department of Obstetrics and Gynecology, Novokuznetsk State Institute for Advanced Medical Training, branch of RMACPE, Ministry of Health of Russia, 5 Stroiteley Ave., Novokuznetsk, 654005, Russia, +7(905)908-01-45, karapetyan.armine1102@yandex.ru, https://orcid.org/0009-0003-8508-3625
Anna E. Vlasenko, Specialist at the Department of Medical Statistics and Informatics, Novokuznetsk State Institute for Advanced Medical Training, branch of RMACPE,
Ministry of Health of Russia, 5 Stroiteley Ave., Novokuznetsk, 654005, Russia, +7(3843)32-47-50, vlasenkoanna@inbox.ru, https://orcid.org/0000-0001-6454-4216
Corresponding author: Oleg A.Volkov, volkovoa@icloud.com



