По данным международных исследований, бесплодием страдает около 186 млн мужчин и женщин по всему миру [1]. Основными причинами бесплодия у женщин являются: нарушения менструального цикла, заболевания эндокринной системы, овуляторная дисфункция, повреждения маточных труб и др. Основные факторы мужского бесплодия – аномалии сперматогенеза, генетические факторы и сосудистые заболевания. Следует отметить, что примерно в 30% случаев диагностический поиск причин бесплодия оказывается безуспешным, и этиология потери фертильности остается неустановленной [2].
Бесплодие и эндометриоз
Женское бесплодие часто ассоциировано с эндометриозом [1, 3], но механизмы этой связи до настоящего времени не вполне ясны. Завершив серию масштабных научных изысканий для установления связи бесплодия и эндометриоидной болезни, исследователи заключили, что к нарушению фертильности при эндометриозе могут приводить различные механизмы, включая изменения анатомии и локальной микросреды, что отрицательно сказывается на созревании ооцитов, оплодотворении, транспорте зиготы и имплантации [2, 4–6].
При прогрессировании и распространении эндометриоза (rAFS III/IV, классификация распространенности эндометриоза Американского общества по репродуктивной медицине), анатомические изменения, такие, как перитубарные и периовариальные сращения, могут оказывать негативное влияние на захват ооцита фимбриями маточной трубы, отрицательно влиять на взаимодействие гамет и пассаж эмбриона по трубе [2]. Также описаны случаи уменьшения овариального резерва при прогрессировании эндометриоза [4], особенно в случаях формирования эндометриом [5, 6]. Некоторые авторы сообщают о том, что эндометриомы самостоятельно могут снижать овариальный резерв [7]. Считается, что яичниковая ткань повреждается под действием токсических субстанций, содержащихся в эндометриомах, которые диффундируют в окружающие ткани и оказывают отрицательное воздействие на функциональный резерв яичников [5].
Между тем, бесплодие наблюдается и у пациенток с малыми формами эндометриоза (rAFS I/II), при которых не наблюдаются изменения анатомии малого таза, что говорит о наличии и других механизмов нарушения фертильности [8, 9]. Предполагается, что у пациенток с эндометриозом нарушается перитонеальная, фолликулярная и эндометриальная микросреда, что приводит к дефектам фолликулогенеза, нарушению овуляции, патологии ооцитов, снижению рецептивности эндометрия и, даже, опосредованно, к угнетению функции сперматозоидов [10, 11].
Проблемы диагностики эндометриоза
Эндометриоз – изнуряющая гинекологическая патология, характеризующаяся появлением эндометриальных желез и стромы эктопической локализации. Особенности этиопатогенеза данной патологии до сих пор недостаточно изучены, но принято считать, что основной причиной эндометриоза является ретроградная менструация. У большинства женщин часть менструальной крови вытекает в брюшную полость через маточные трубы, но далеко не у всех развивается эндометриоз, что достигается элиминацией клеток эндометрия макрофагами [12].
Поражая 6–10% пациенток репродуктивного возраста, заболевание достоверно ассоциировано с болевым синдромом и бесплодием [13]. Клинические проявления эндометриоза варьируются от бессимптомных до дисменореи, диспареунии, болевого синдрома в малом тазу, аномальных маточных кровотечений и др. [14, 15]. Одним из самых неблагоприятных клинических проявлений эндометриоза является бесплодие.
Для эффективной диагностики эндометриоза неивазивными методами важно знать факторы риска, при которых следует заподозрить наличие данной патологии. На сегодняшний день в практике врача отсутствуют общепринятые унифицированные неинвазивные тесты для диагностики эндометриоза, поэтому решение вопроса о выполнении лапароскопии основывается на клинической оценке анамнеза, данных объективного осмотра и результатах ультразвукового исследования (УЗИ) [16]. У пациенток с эндометриомами УЗИ является точным методом предоперационной диагностики, но его возможности существенно ограничены при исключительно перитонеальном поражении [17]. Исследования демонстрируют, что точность диагностики эндометриоза без вовлечения яичников, основанная только на сочетании симптомов, данных объективного осмотра и результатов УЗИ, составляет не более 38% [18].
В настоящее время эндометриоидная болезнь может быть объективно диагностирована только при визуальной оценке брюшной полости и малого таза с обязательной гистологической верификацией операционного материала [19]. Несмотря на малую инвазивность и относительную безопасность лапароскопии, она, тем не менее, сопровождается хирургическим риском. Кроме того, лапароскопия является дорогостоящей манипуляцией и временно снижает трудоспособность пациенток. Необходимость в инвазивной хирургии для диагностики эндометриоидных очагов в брюшной полости приводит к тому, что временной интервал от первых симптомов до постановки диагноза составляет 6,7 года [20]. Поздняя диагностика имеет неблагоприятные последствия, так как болезнь со временем прогрессирует [21].
Принимая во внимание связь эндометриоза с хорошо изученными болевыми симптомами, клиницисты вынуждены констатировать –почти у половины женщин с синдромом хронической тазовой боли эндометриоидные очаги во время операции не обнаруживаются [22, 23]. Указанные ограничения отражают важность исследований, направленных на дооперационное выявление пациенток с эндометриозом. Выявление клинических предикторов эндометриоза позволит определить группу пациенток с бесплодием и высоким риском эндометриоза, что ускорит проведение лапароскопии. Между тем, до настоящего времени проведено не так много исследований, направленных на поиск клинических предикторов эндометриоза у пациенток с бесплодием [24– 26]. Это приводит к тому, что в международном медицинском сообществе отсутствует единая позиция по вопросу: каким пациенткам с бесплодием следует предложить лапароскопию [27, 28]. Таким образом, поиск нехирургических триггеров эндометриоза нам представляется важным направлением исследований в обсуждаемой области.
Целью данного обзора является описание известных предикторов эндометриоза, которые помогут заподозрить обозначенную патологию у пациенток с бесплодием. Вместе с тем, приобретенные новые знания позволят практикующим врачам эффективно выявлять женщин с высоким риском эндометриоза и своевременно диагностировать и лечить заболевание, что у многих пациенток поможет не допустить развитие такого грозного осложнения, как бесплодие.
Дизайн исследования
С целью обзора литературы по изучаемой проблеме, проведен поиск результатов исследований в электронной базе данных PubMed MEDLINE (https://www.ncbi.nlm.nih.gov/pubmed) до марта 2021 г. Ключевые слова для поиска: «endometriosis» (эндометриоз), «infertility» (бесплодие), «prognosis» (прогноз), «predictive factors» (предиктивные факторы). Использовались различные комбинации слов и словосочетаний. Для выявления потенциально пропущенных работ дополнительно оценивался список литературы каждой из найденных работ.
Основные предикторы эндометриоза при бесплодии
В ходе двух изученных крупных исследований оценивалось множество факторов риска, которые могут быть связаны с эндометриозом при бесплодии [29, 30]. Полученные данные помогли сделать промежуточные выводы об основных предикторах эндометриоза при утрате фертильности.
В исследование A. Moini et al. [29] были включены 403 пациентки с бесплодием. Среди них у 250 пациенток был диагностирован эндометриоз (62% – исследуемая группа), у 153 пациенток патологии органов малого таза выявлено не было (38% –контрольная группа). I стадия эндометриоза наблюдалась у 52 (20,8%) пациенток, II стадия – у 70 (28%), III стадия – у 82 (32,8%), IV стадия – у 46 (18,4%). По тяжести эндометриоза пациентки были разбиты на 3 группы: контрольная группа (норма –38%); группа эндометриоза легкой степени (I и II стадии – 30,3%); группа тяжелого эндометриоза (III и IV стадии – 31,7%). Между сформированными группами наблюдалась значимая разница по следующим показателям: продолжительность бесплодия, индекс массы тела (ИМТ), продолжительность менструации, продолжительность менструального цикла, продолжительность кровомазания, возраст сексуального дебюта (ANOVA анализ). Анализ хи-квадрат (χ2) показал значимую разницу (р<0,05) по следующим показателям между тремя группами: статус образования, профессиональная деятельность, характер менструации, тяжесть дисменореи, объем менструальной кровопотери, кровомазание, диспареуния, использование оральных контрацептивов, тазовая боль, уплотнения в малом тазу при осмотре, семейный анамнез по эндометриозу (табл. 1, 2).

Выявление независимых предикторов
Логистическая регрессия показала, что независимыми предикторами любой формы эндометриоза являются: возраст, продолжительность бесплодия, ИМТ, продолжительность менструального цикла, анамнез по абортам, диспареуния, тазовая боль, семейный анамнез по эндометриозу. Независимыми предикторами тяжелого эндометриоза являются: возраст, образование, продолжительность бесплодия, ИМТ, объем менструальной кровопотери, продолжительность менструации, диспареуния, тазовая боль, семейный анамнез по эндометриозу (табл. 3).
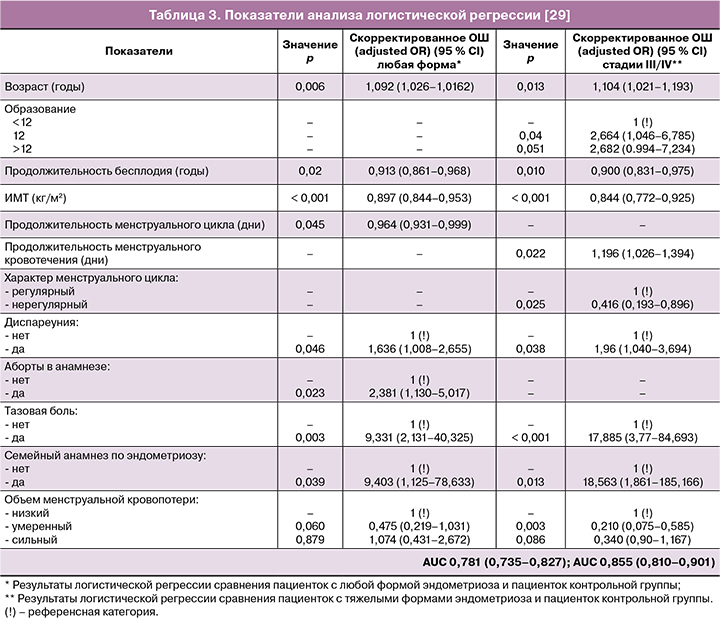
Моделирование показало значение AUC 0,781 с 95 % CI (0,735–0,827) для предположения о любой форме эндометриоза и AUC 0,855 с 95 % CI (0,81–0,901) для предположения о тяжелом эндометриозе. Достоверной разницы не было отмечено по следующим показателям: возраст, вид бесплодия, курение, возраст менархе, дисменорея (наличие или отсутствие), физическая активность, возраст наступления первой беременности и родов, анамнез живорождения, анамнез по эктопической беременности, видам абортов и анамнез по кюретажу полости матки.
Данное исследование показало, что возраст, продолжительность бесплодия, ИМТ, диспареуния, тазовая боль и семейный анамнез могут рассматриваться, как предиктивные факторы не только любого типа эндометриоза, но и тяжелых форм.
Анализ основных предикторов ИМТ показал обратную корреляцию с эндометриозом: пациентки, страдающие ожирением, входили в группу низкого риска по эндометриозу (р<0,001). Представленные данные совпадают с результатами работ S.A. Missmer et al. [31], C. Calhaz-Jorge et al. [30], Итальянской группы [32], M. L. Hediger et al. [33], S. Berube et al. [34]. В настоящем исследовании более низкий ИМТ был значимо связан с тяжестью эндометриоза, что совпадает с данными K.W. Yi et al. [35]. Одним из объяснений полученных результатов может служить тот факт, что ановуляторные и нерегулярные менструации у пациенток с ожирением могут вести к уменьшению объема ретроградной менструации.
Продолжительность менструального цикла имела обратную корреляцию с риском эндометриоза, в то время как нерегулярный менструальный цикл, продолжительность и объем менструации были связаны только с тяжелым эндометриозом. Нерегулярный цикл имел обратную корреляцию с продолжительностью кровотечения. Полученные результаты могут быть объяснены теорией ретроградной менструации: короткий цикл и больший объем менструации могут потенциально повысить риск ретроградного кровотечения. K. Arumugam и J.M.H. Lim [36], D.W. Cramer и S.A. Missmer [37], S. Berube et al. [34] показали, что у пациенток с циклом короче 27–28 дней риск развития эндометриоза повышается. С другой стороны, C. Calhaz-Jorge [30], R. Hemmings et al. [38], F. Parazzini et al. [32] не нашли достоверной связи между коротким менструальным циклом и эндометриозом.
Возраст пациентки, страдающей бесплодием, обладает прямой корреляционной связью с развитием любой формы эндометриоза, включая тяжелые формы. Частота эндометриоза значительно возрастает с 25–29 лет до 40–44 лет и затем начинает снижаться.
Образование является единственным социально-экономическим фактором, связанным с тяжелыми формами эндометриоза, хотя связи с остальными формами отмечено не было. Исследования Итальянской группы [32] и S. Berube et al. [34] не выявили зависимости между уровнем образования и наличием эндометриоза. Одним из потенциальных объяснений связи уровня образования и развития эндометриоза может являться тот факт, что женщины с более высоким уровнем образования чаще обладают более высоким социально-экономическим статусом и уровнем знаний, поэтому они уделяют больше внимания своему здоровью и чаще обращаются к врачу, соответственно и болезнь диагностируется раньше.
Семейный анамнез по эндометриозу является еще одним независимым фактором, который напрямую связан с любой формой и степенью тяжести эндометриоза. Эти данные подтверждены исследованиями H.M. Mamdouh et al. [39], I.M. Matalliotakis et al. [40], K. Kashima et al. [41]. В ходе исследования A. Moini et al. [29] было показано, что семейный анамнез повышает риск развития эндометриоза в 9,7 раза.
Настоящее исследование показало, что у 48,4% пациенток с эндометриозом наблюдалась диспареуния. Анализ логистической регрессии показал, что диспареуния была фактором риска, связанным с любым видом и тяжестью эндометриоза. I.M. Matalliotakis et al. [40] продемонстрировали, что тазовая боль, дисменорея и диспареуния наблюдались достоверно чаще у пациенток с эндометриозом, по сравнению с пациентками с бесплодием без эндометриоза.
Эндометриоз связан с хронической тазовой болью и бесплодием. Связь между симптомами хронической тазовой боли и эндометриозом не ясна, так как болевой синдром часто наблюдается у пациенток без эндометриоза, а также вследствие наличия безболевых форм эндометриоза. Предполагаемые механизмы боли заключаются в развитии локального воспаления, спаечного процесса и простагландинового каскада, запущенного в эндометриоидных очагах [22]. Настоящее исследование показало, что тазовая боль наблюдалась в 14,8% случаев, в то время как другие авторы [22] показали частоту 79,1%.
Данное исследование показало, что продолжительность бесплодия имеет обратную связь с любым типом эндометриоза и тяжелыми формами. Это кажется логичным, так как «симптомный» эндометриоз заставляет пациентку обращаться за помощью раньше.
Прием оральных контрацептивов связан с повышением риска развития эндометриоза в 2 раза. Подобные результаты были получены и в работе C. Calhaz-Jorge [30]. Связь препаратов с развитием эндометриоза сложно интерпретировать, и авторы не могут предложить четкое патофизиологическое объяснение этому феномену.
Предменструальное кровомазание
Простым для диагностики является показатель предменструального кровомазания. R.J. Heitmann et al. [42] продемонстрировали связь между этим показателем и частотой развития эндометриоза у пациенток с бесплодием. Более того, данный симптом обладает большей специфичностью по сравнению с традиционными проявлениями, такими как дисменорея и диспареуния. В исследовании приняло участие 80 пациенток, которым проводились лапароскопии по поводу бесплодия: 38 пациенток с кровомазанием не менее, чем за два дня до менструации и 42 пациентки без подобных жалоб. Все участницы страдали от бесплодия, что и являлось показанием для проведения лапароскопии. Предменструальное кровомазание расценивалось, как появление кровянистых выделений до начала основного менструального потока. Для исключения нормальных вариантов начала менструации и других состояний, которые могли привести к кратковременному кровомазанию, симптом считался значимым только при продолжительности в течение, как минимум, двух дней.
В группе пациенток без кровомазания эндометриоз был диагностирован в 26% случаев (у 11 из 42 пациенток). Стоит отметить, что все случаи в этой группе были доказаны гистологически и относились к I стадии по классификации rAFS.
А в группе пациенток с предменструальным кровомазанием частота гистологически подтвержденного эндометриоза при лапароскопии составила 89% (34/38 пациенток) (р<0,0001). Более того, в 85% случаев наблюдалась II и более стадия эндометриоза по классификации rAFS (табл. 4).

По сравнению с такими симптомами, как дисменорея и диспареуния, предменструальное кровомазание являлось показателем с наивысшей положительной прогностической ценностью и показателем с отрицательной прогностической ценностью, практически сопоставимым с дисменорей (табл. 5). Из трех симптомов предменструальное кровомазание было самым точным в правильности выбора пациенток с эндометриозом: 81% точности по сравнению с 76% для дисменореи и 58% для диспареунии.
Одномерный регрессионный анализ показал, что предменструальное кровомазание не менее двух дней (OR 24; 95% CI, 6,9–83; р=0,001), дисменорея (OR 15,5; 95% CI, 4,3–43; р=0,001) и диспареуния (OR 3,2; 95% CI, 1,2–9,3; р=0,03) в значительной степени коррелировали с наличием эндометриоза во время лапароскопии. В множественной регрессии предменструальное кровомазание (OR 16; 95% CI, 3,9–65,4; р=0,001) и дисменорея (OR 8,63; 95% CI, 1,9–38,8; р=0,005) оставались значимыми показателями при гистологически подтвержденном эндометриозе.
Результаты исследования показывают значимую связь между предменструальным кровомазанием в течение, как минимум, 2 дней и диагностикой эндометриоза во время лапароскопии у пациенток с бесплодием. Интересным является тот факт, что этот симптом связан со II и более стадией болезни по классификации rAFS. Предменструальное кровомазание может указать на наличие или отсутствие эндометриоза с точностью до 81%.
A.C. Wentz [43] был первым, кто описал потенциальную связь предменструального кровомазания и эндометриоза. В обзоре [44] проводилась оценка связи между предменструальным кровомазанием и эндометриозом. Среди 1350 пациенток с бесплодием или обратившихся за коррекцией стерилизации, у 101 женщины (8%) отмечалось предменструальное кровомазание (как минимум, один день до менструации). Среди этих пациенток, у 83% (84 из 101) во время лапароскопии был диагностирован эндометриоз. Для сравнения, предменструальное кровомазание наблюдалось у 4% фертильных пациенток (3 из 70), которые обратились для коррекции трубной стерилизации. Если рассматривать принятую теорию ретроградной менструации, то маточные трубы необходимы для развития эндометриоза. Таким образом, когорта пациенток с трубной стерилизацией в анамнезе не является оптимальной группой для сравнения.
Анализ первичного бесплодия, тяжести дисменореи, наличия патологических образований в области заднего свода в качестве предикторов эндометриоза при бесплодии
К следующим предикторам эндометриоза при бесплодии можно отнести: первичное бесплодие, тяжесть дисменореи и наличие узелков в области крестцово-маточных связок/заднего свода. В исследовании K. Whitehill et al. [46] приняло участие 429 пациенток, которым проводилась лапароскопия по поводу бесплодия: в 168 случаев (39%) диагностирован эндометриоз, в 261 случае (61%) эндометриоза не было. При сравнении групп прогностическими показателями, связанными с эндометриозом, являлись: первичное бесплодие, возрастающая тяжесть дисменореи (отсутствие, легкая, умеренная, тяжелая), глубокая диспареуния, болезненность и наличие узелков в области крестцово-маточных связок/заднего свода влагалища, наличие у врача специализации по эндометриозу (табл. 6).

Данные представленной работы совпадают с результатами ранее опубликованных исследований. L. Fedele et al. показали, что тяжесть дисменореи возрастает, а диспареуния и хроническая тазовая боль встречается чаще у пациенток с сочетанием бесплодия и эндометриоза, по сравнению с пациентками, которые страдают бесплодием без эндометриоза [24]. R. Mattoras et al. выяснили, что наличие узелков в заднем своде является ключевым индикатором эндометриоза при бесплодии [25]. Другие авторы. обнаружили связь между болезненностью и наличием узелков в области крестцово-маточных связок/заднего свода с эндометриозом у пациенток с бесплодием и тяжелой дисменореей [26].
Интересным является тот факт, что гинеколог со специализацией по эндометриозу чаще диагностирует эту патологию при лапароскопии. Обученные специалисты находят типичное и нетипичное проявление эндометриоза, что подтверждается при патогистологическом исследовании. Одним из объяснений этому является тот факт, что специалисты чаще распознают нетипичное проявление эндометриоидных очагов и удаляют их, а также иссекают большие поверхности брюшины, а не ограничиваются точечной биопсией. Ложноположительные диагнозы у врачей-специалистов в области диагностики и лечения эндометриоза встречаются редко.
Эндометриоз и воспаление
Помимо теории ретроградной менструации, этиопатогенез эндометриоза включает еще несколько теорий. Два состояния встречаются крайне часто: локальное и системное воспаление, которое стимулирует выработку брюшиной цитокинов, особенно интерлейкина 6 (ИЛ-6) и интерлейкина 8 (ИЛ-8) [46]. Было высказано предположение, что аутоиммунные механизмы могут играть важную роль в развитии бесплодия [47].
Биомаркеры эндометриоза
До настоящего времени большое количество исследований были направлены на оценку биомаркеров в качестве неинвазивной диагностики эндометриоза. Однако связь этих биомаркеров с бесплодием не оценивалась. Целью исследования N. Gica et al. [48] было определить связь между уровнем биомаркеров из периферической крови (сыворотка крови, без уточнения дня менструального цикла) с эндометриозом и бесплодием. СА-125 – это основной биомаркер, наряду с провоспалительными цитокинами, которые определяются при эндометриозе. Таким образом, была выдвинута гипотеза о том, что сочетание ИЛ-6 и ИЛ-8 с уровнем СА-125 может предсказать бесплодие у пациенток с эндометриозом точнее, чем только оценка СА-125 [46, 47].
Параллельно проводилось два исследования. В первом исследовании оценивался уровень СА-125 у 116 пациенток с эндометриозом и сохранением проходимости маточных труб, а во втором – уровень ИЛ-6 и ИЛ-8 у 36 пациенток. После применения всех критериев включения, в исследовании осталось 116 пациенток, которые были распределены по двум группам, в зависимости от фертильного статуса: фертильные и с бесплодием (как первичным, так и вторичным) [48].
В первом исследовании для классификации эндометриоза использовалась шкала Американской ассоциации по репродуктивной медицине (ASRM): I стадия – 15 пациенток (12,93%), II стадия – 57 пациенток (49,13%), III стадия – 30 пациенток (25,86%), IV стадия – 14 пациенток (12,06%). Достоверной разницы в показателях возраста между двумя группами отмечено не было. Достоверного влияния стадии эндометриоза на фертильность отмечено не было (р=0,83). В группе фертильных пациенток среднее значение СА-125 составило 31,43±19,98 с медианой 24; в группе пациенток с бесплодием – 45,99±30,37 с медианой 43,8. Распределение значений СА-125 в группе фертильных пациенток было непараметрическим (р=0,00<0,05) и параметрическим в группе пациенток с бесплодием. Разница в уровне СА-125 между группами была достоверной (р=0,00).
Во втором исследовании приняло участие 36 пациенток: 22 (61,11%) пациентки с бесплодием и 14 (38,88 %) – с сохраненной фертильностью. Значимых различий в возрасте отмечено не было. В обеих группах распределение было непараметрическим. Для оценки влияния стадии эндометриоза на статус фертильности использовался тест χ2. Он показал значимое влияние стадии эндометриоза на фертильность (χ2=23,19, р=0,00). Средний показатель ИЛ-6 (±SD) у фертильных пациенток составил 5,79±2,87 с медианой 6,01, а в группе пациенток с бесплодием – 91,88±107,74 с медианой 100. Статистический анализ ИЛ-6 и ИЛ-8 показал, что среднее значение ИЛ-6 (±SD) составило 38,38±87,86 с медианой 10,5. Среднее значение ИЛ-8 (±SD) составило 12,54±23,58 с медианой 1,1 в группе фертильных пациенток и 17,34±28,59 с медианой 3,53 – у пациенток с бесплодием. У пациенток с бесплодием наблюдалось значимое повышение уровня ИЛ-6, по сравнению с фертильной группой (р=0,00). Достоверной разницы в уровне ИЛ-8 между группами отмечено не было (р=0,06). Вероятность бесплодия у пациенток требовала анализа логистической регрессии: чувствительность составила 75%, а специфичность – 90%. Положительное прогностическое значение составило 85,71%, отрицательное прогностическое значение – 81,81%. После статистической оценки показателей СА-125, ИЛ-6 и ИЛ-8 выяснилось, что повышение уровня СА-125 является единственным показателем вероятной диагностики бесплодия при эндометриозе.
Предыдущие исследования показали, что уровни цитокинов и гликопротеинов тесно связаны с эндометриозом, а определение биомаркеров является неинвазивным тестом на эндометриоз [49]. СА-125 является периферическим биомаркером эндометриоза, который продуцируется эндометриальными и мезотелиальными клетками [11]. У пациенток с эндометриозом также повышается уровень ИЛ-6 и ИЛ-8 [50–53]. Однако литературные данные противоречивы. Другие исследователи свидетельствуют об одинаковых значениях интерлейкинов при эндометриозе и в контрольных группах [13, 54].
Посредством логистической регрессии оценивалась вероятность наличия бесплодия в зависимости от уровня СА-125. Показатель СА-125 был единственным подходящим под эту модель (р=0,01), и повышение указанного маркера связано с повышением вероятности диагностики бесплодия. Авторы сделали вывод, что повышение уровня СА-125 увеличивает риск бесплодия [48].
Статистический анализ второго исследования показал, что стадия эндометриоза оказывает значительное влияние на статус фертильности (χ2=23,19, р=0,00) [49]. Особенно выраженные стадии эндометриоза, даже необструктивного, приводят к формированию бесплодия через механизм, отличный от двусторонней обструкции маточных труб.
Три биомаркера эндометриоза являются неспецифическими протеинами воспаления, которые также повышаются при аутоиммунных заболеваниях, гепатите, сепсисе, воспалительных заболеваниях малого таза. Результаты исследования могут помочь выбрать перечень цитокинов для улучшения диагностики.
Заключение
Согласно изученным литературным данным, прогностическими факторами эндометриоза при бесплодии являются: предменструальное кровомазание, первичное бесплодие, ухудшение течения дисменореи, наличие узелков в области крестцово-маточных связок/заднего свода, возраст, продолжительность бесплодия, ИМТ, продолжительность менструального цикла, аборты в анамнезе, диспареуния, тазовая боль, семейный анамнез. Независимыми предиктивными факторами тяжелого эндометриоза являются: возраст, образование, продолжительность бесплодия, ИМТ, объем менструальной кровопотери, продолжительность менструации, диспареуния, тазовая боль, семейный анамнез. В отдельных исследованиях показана прогностическая роль СА-125 и ИЛ-6 у пациенток с бесплодием.
Нам представляется, что разработка специальных опросников и диагностических программ на основе клинических рекомендаций, позволит автоматизировать процесс сбора данных и их интерпретацию для своевременного выявления на дооперационном этапе пациенток с максимальным риском развития эндометриоза при бесплодии, которым в наибольшей степени показано проведение лапароскопии.