The informative value of ultrasound examination of patients with intrauterine adhesions
Objective: To improve intrauterine adhesions (IUA) diagnosis accuracy and integrate three-dimensional echography into the algorithm for examining patients with IUA.Esipova I.A., Krasnova I.A., Breusenko V.G., Aksenova V.B., Timofeeva E.G.
Materials and methods: The study comprised 79 patients with suspected IUA. We analyzed various functions and modes of three-dimensional echography, including multiplanar reconstruction mode, Vocal, OmniView mode, frontal section (using HI, SRI CRI functions or Render Mode automatic versions, surface scanning mode with a combination of minimum/maximum intensity), ultrasound tomography mode. The examination was performed on the Canon Aplio 500 ultrasound system to assess the degree of obliteration and septal architectonics. The role of three-dimensional hydrohysteroscopy in navigation during endoscopic adhesiolysis was determined.
Results: Echographic criteria for assessing uterine cavity obliteration by three-dimensional echography were developed. Echographic features of the three-dimensional uterine model, including "muscular invagination" (frontal section, OmniView mode, ultrasound imaging), hourglass and discontinuous M-echo character (frontal
section, OmniView mode), allowed for a detailed evaluation of uterine cavity obliteration, its architectonics, and determine the intraoperative strategy for IUA destruction.
Conclusion: The developed three-dimensional criteria enabled developing a unified strategy to guide pre-surgical planning, reduce the risk of intraoperative complications and disease recurrence. To reduce the risk of uterine perforation and surgical trauma in patients with IUA, it was suggested to form a surgical team consisting of an endoscopy specialist and a diagnostic medical sonographer.
Keywords
Intrauterine adhesions (IUA) remain one of the challenging issues in gynecology. A meta-analysis has shown an increasing trend in the incidence of IUA [1–6]. This trend is associated with a growing number of operative deliveries and uterine surgery. The low efficacy of IUA treatment is related to delayed diagnosis in the asymptomatic early stages of the disease. Studies [2, 3, 5, 7] have shown that this factor complicates surgical correction and worsens the reproductive prognosis. Interventions in the later stages of the disease may increase the risk of surgical complications and recurrence. Hooker A.B. et al. (2021) [7]; Vancaillie T. et al. (2020) [8] note that before surgical treatment, the number of diagnosed IUAs with grade III–V endometrial cavity obliterations prevailed over the number of diagnosed grade I–II obliteration (European Society of Gynecological Endoscopy IUA classification). This, in its turn, worsens the prognosis of surgical restoration of the functional anatomical volume of the uterine cavity, endometrial recovery, and subsequent improvement of its functional activity.
Current literature data suggest a high informative value of three-dimensional echography in detecting changes in uterine cavity topography associated with such nosology as uterine fibroids, adenomyosis, and endometrial hyperplasia [9, 10]. However, the current literature lacks information related to three-dimensional imaging in diagnosing IUA [11, 12].
This study aimed to improve intrauterine adhesions diagnosis accuracy and integrate 3D echography into the algorithm for examining patients with IUA.
Materials and methods
We examined 79 patients with suspected IUA admitted to the gynecological department of City Clinical Hospital No.31 of Moscow Healthcare Department. The control group included 20 healthy women visiting the consultative department for a prophylactic examination. 3D ultrasound findings were analyzed in 57 patients with IUA and 22 patients with endometrial hypoplasia according to the final diagnosis.
The patients' age ranged from 24 to 45 years, averaging 31.5±2.4 years. The study inclusion criteria were age under 45 years and suspected IUA. The exclusion criteria were age over 46 years, a history of total or partial endometrial hysteroresectoscopy for various endometrial and myometrial diseases, reproductive system malignancy, and polycystic ovarian syndrome.
Sixty-four patients complained of various menstrual disorders. Amenorrhea, abnormal uterine bleeding, hypo menstrual syndrome, and algodysmenorrhea were diagnosed in 9, 19, 21, and 15 patients, respectively. Every third patient was concerned about fertility. Most patients had a history of pelvic surgery (Table 1).
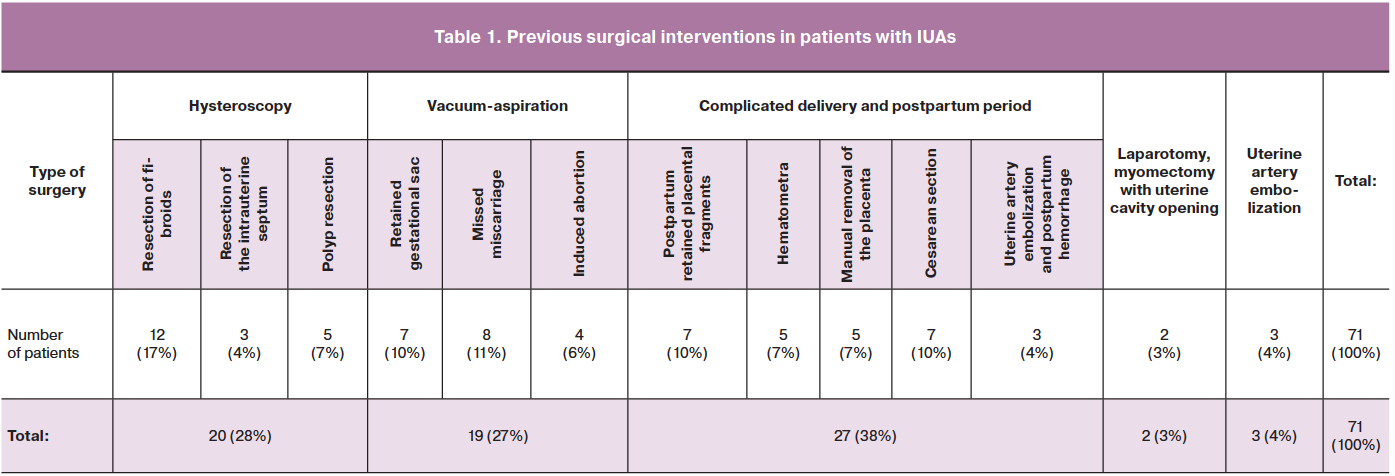
It is important to note that only 8/79 women had no prior history of pelvic surgery. A history of inflammatory predictors of IUA was identified in 27 patients: nine had acute salpingo-oophoritis, and 18 had endometritis, eight of them during the postpartum period.
Patients were examined according to a standard clinical and laboratory plan for the hospital admission. The ultrasound examination algorithm included four stages. At stage 1, patients on day 5–7 of the menstrual cycle, or irrespective of the cycle, underwent standard two-dimensional ultrasound screening (2DUS) with the targeted assessment of all available endometrial parameters. We supplemented this information with three-dimensional echography (3D ultrasound). An additional ultrasound on days 19–22 of the menstrual cycle was performed to assess the condition and volume of the endometrium if grade III–V obliteration of the uterine cavity was suspected. When obtaining a frontal plane (FP), we used image contrast enhancement (combination of image contrast settings (HI, SRI CRI or various automatic Render Mode options, surface scan mode with a combination of minimum/maximum intensity, and VCI function). To obtain adequate FP, we used the TUI mode (with slice thickness from 0.5 to 2.5 mm). To estimate the endometrial volume (Vend), we used an automatic calculation by using VOCAL software.
The next step was a minimally invasive procedure in the form of 2D/3D hysterosalpingography (HSG). We performed image inversion to obtain a contrast image and a clearer assessment of the uterine cavity deformity. Rough obliteration in the projection of the internal os may have been a technical limitation of uterine cavity contrasting. Contrasting of the cavity was performed with sterile saline using 5–7FR balloon catheters for HSG. The contrast was delivered using a Karl Storz Hamou Endomat Pump with preset speed and pressure parameters (V=50–100 ml/min, P=100–120 mmHg), with the possibility of adjustment. All images were saved for further offline processing. We interpreted the results of preoperative 2D and 3D ultrasound/ HSG based on the IUA classification system of the European Society for Gynecological Endoscopy [13, 14].
Stage 3: Intraoperative ultrasound navigation for intrauterine surgery. All pelvic ultrasound scans were performed using a Canon Aplio 500 Ultrasound Machin with an intracavitary 3D transducer. In the fourth stage, we evaluated the treatment effectiveness. All findings were compared with hysteroscopy results and IUA separation stages.
Results and discussion
The analysis of the ultrasound images showed that the presence of IUA can be suspected based on the standard two-dimensional echographic criteria (15).
Table 2 shows that the technique's sensitivity is relatively low, which is consistent with the available literature [16, 17]. When assessing the criteria "correspondence of M-echo to menstrual cycle phase" and "discontinuous nature of M-echo," the diagnosis of IUA was not confirmed by hysteroscopy in 22/79 patients; they were diagnosed with endometrial hypoplasia. In 3/8 patients with grade I and 4/11patients with grade II obliteration, single, thin, filmy synechiae were not detected by echography. Hysteroscopy showed single and multiple filmy adhesions in the middle third of the uterus (n=2), synechiae in the lower third of the uterine cavity (n=3), and at the ostia of the fallopian tubes (n=2). The use of office hysteroscopy as the 'gold standard in diagnosing IUA has long been discussed by specialists [18, 19]. This method allows real-time visualization of the uterine cavity, including uterine cavity architectonics, the course and nature of the septa, and the condition of the endometrium, but only in grade I–II obliteration. In these cases, intraoperative ultrasound navigation is often necessary due to the lack of topographic landmarks. However, more significant uterine cavity obliteration is a limitation for adequate examination due to the lack of complete insufflation of the cavity, which requires the use of standard hysteroscopic techniques.
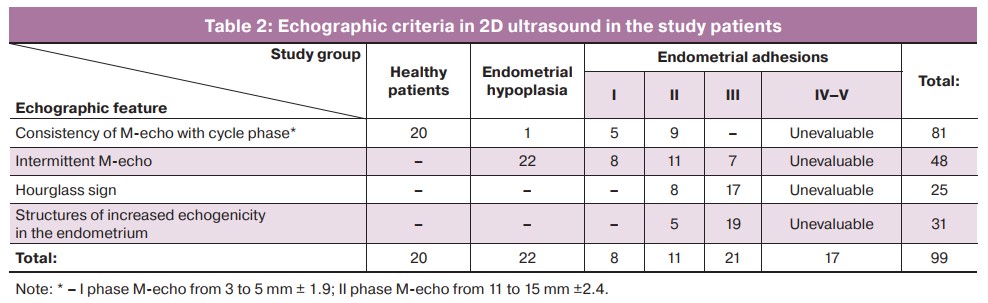
2D ultrasound allowed IUAs to be suspected based on the echographic criteria in 49 of 57 patients. However, 2D ultrasound did not provide complete information on the degree of obliteration, architectonics alterations, direction, and nature of the septa in every second patient with grade I–II and all patients with grade III obliteration. In patients with severe IUAs, 2D ultrasound data may suggest grade IV–V obliteration based on the inability to interpret the above echographic signs.
Using contrast-enhanced uterine cavity 2D ultrasound improved the sensitivity and specificity of the technique, which is in concordance with the findings of a group of researchers [16, 20] who reported that two-dimensional HGS, in comparison with hysteroscopy, had a high sensitivity (75–81%) and specificity (80%). However, this method does not provide information on the septa architectonics and the degree of uterine cavity obliteration, which does not reduce surgical risks.
The use of three-dimensional echography remains controversial due to the small number of studies [12, 21]. According to our data, three-dimensional imaging has a different range of extended echographic criteria based on additional options.
Obtaining a section in the frontal plane (FP) allowed us to assess the shape of the uterine cavity and its architectonics and visualize uterine cavity deformation through an echographic feature we termed as "muscular invagination" at the septal fixation points (n=15), stenosis at the ostia of the fallopian tubes (n=10), and obliteration at the middle and lower thirds of the cervical canal (n=5) and at the internal os (n=4). We obtained additional echographic findings that were not recorded in the longitudinal and transverse planes, namely, visualization of multidirectional septa of the lateral contralateral walls narrowing the uterine cavity with the assessment of their thickness and structure (n=15), lateral walls, and uterine fundus (n=12) (Fig. 1).
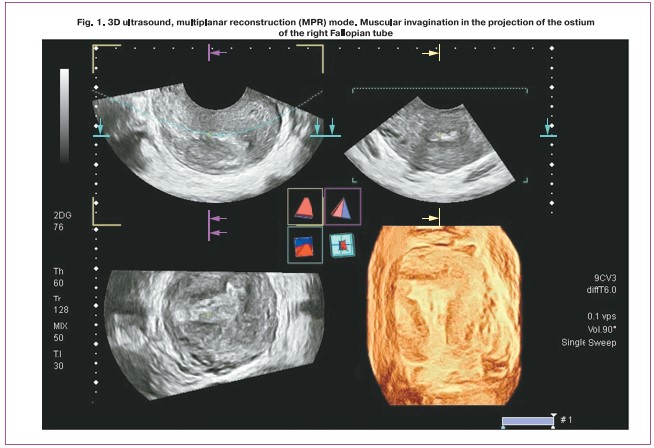
The MPR mode allowed us to obtain a three-dimensional virtual model of the uterine cavity due to the sequential processing of slices of three mutually perpendicular planes (Fig. 2).
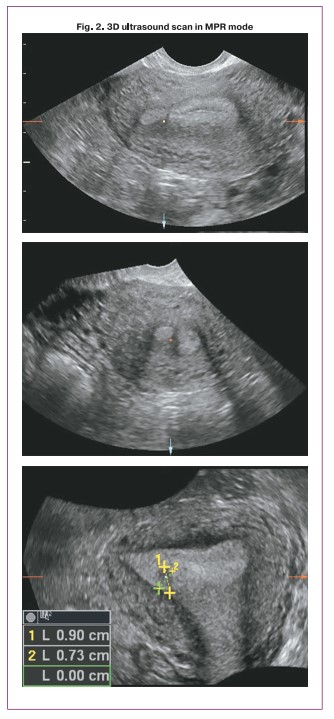
Excursion of the control mark in the scans of the three orthogonal projections provided information about the location of septa at the ostia of the fallopian tubes (n=8), isthmus (n=4), which were not diagnosed by 2D ultrasound.
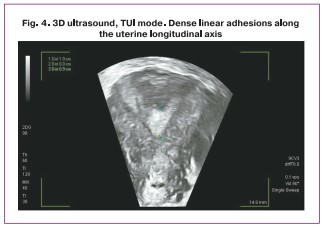
The TUI mode allows the acquisition of echograms at a predetermined step comparable in quality to MRI slices. Based on the findings, we assessed the level and extent of maximum cavity fusion along the uterine longitudinal axis in patients with grade III–IV obliteration (n=10) (Fig. 3).
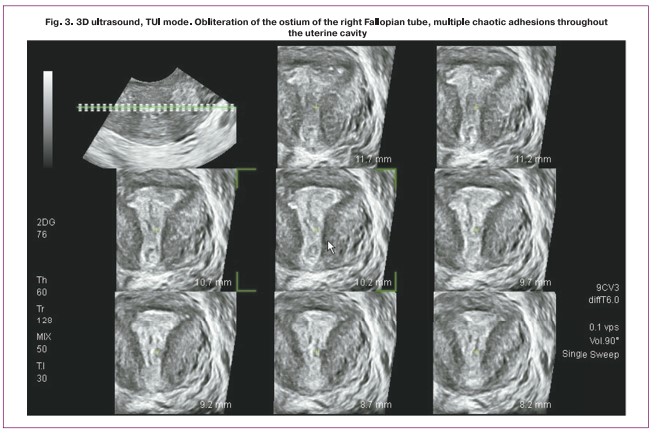
Importantly, these data determined the intraoperative navigation, direction, and depth of dissecting instrument advancement in patients with dense linear adhesions along the longitudinal axis (Fig. 4).
The Omni-view mode with automatic accelerated construction of FP along the polygonal navigation contour provides an actual 3D model of the cavity, modified by IUA, and more reliable differentiation of the degree of obliteration. This information is helpful for surgeons who are not skilled in the evaluation of ultrasound images (Fig. 5).
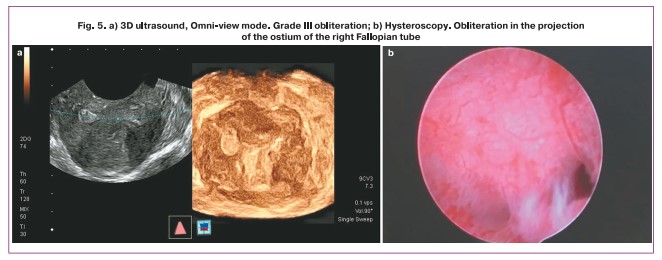
The reconstruction data allowed evaluation of the level and degree of obliteration. In patients with grades I and II of obliteration, the uterine cavity was triangular (n=19). The uterine cavity had a polygonal shape in 4 patients with grade III and 6 patients with grade IV obliteration. In remaining patients with grade IV obliteration and those with grade V obliteration, reconstruction of the uterine cavity proved impossible, as it was visualized by several fragmented, small-sized cavities.
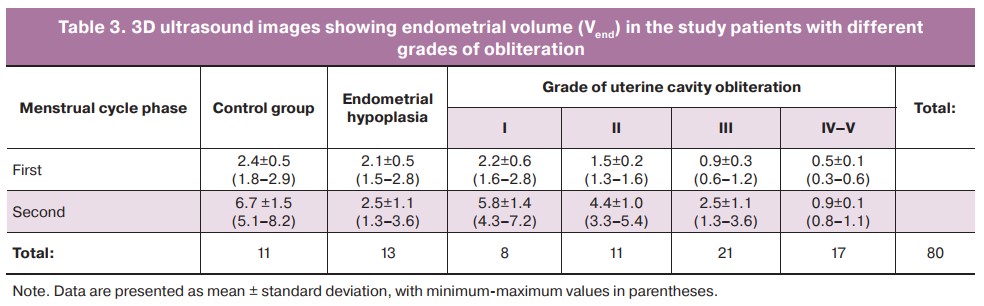
Assessment of the endometrial volume (Vend) by Vocal function reliably indicated a diffuse change in the functional endometrial layer in grade III–IV obliteration. In grade I–II obliteration, Vend corresponded to normal or reduced to the level of endometrial hypoplasia indicators, both in the secretion phase and in the proliferation phase. As seen in Table 3, Vend in grade I–II obliteration did not significantly differ from the normal values in the 1st phase of the menstrual cycle. No significant echographic differences in endometrial volume were found in patients with endometrial hypoplasia and grade I–II obliteration. In this case, we could only suspect the presence of uterine cavity obliteration by an altered Vend.
We also evaluated the advanced features of 2D/3D HSG, which improves diagnosis with an additional acoustic window to facilitate the assessment of the basal contour. We obtained other changes in the endometrium: the proliferation of the functional layer without obvious signs of septa. This feature was detected in 18/22 patients in the absence of IUAs and the lack of the functional layer in both cycle phases 1 and 2. In all patients with thin endometrium, hysteroscopy data confirmed the absence of IUAs.
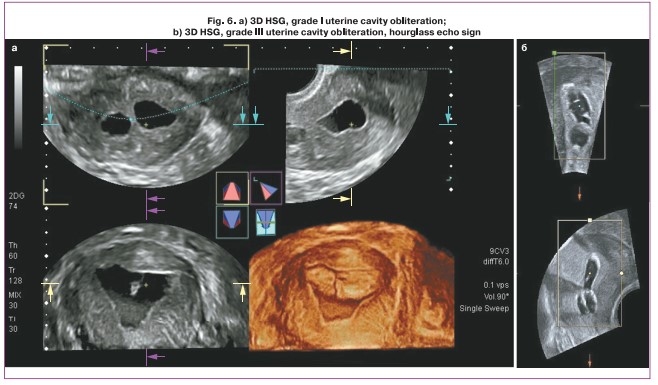
Dense IUAs were detected at septal fixation points measuring 2–3 mm, which did not exceed 1 mm in thickness and did not cause changes in the internal contour of the cavity. This feature was better visualized in FP. The intermittent nature of the M-echo repeated the hourglass feature due to the accumulation of contrast in the septum-bounded cavities and was presented more clearly in 3D HSG (Fig. 6).
A significant advantage of 2D/3D HSG is the visualization of multidirectional septa. Contrasting difficulties appeared only when the IUA was located in the lower third where the catheter could not be inserted. The advantages of HSG using an endomate include the ability to evaluate further technical options, such as automatic changes in speed and contrast delivery due to obliteration.
In patients with IUAs in the lower third and grade IV–V, automatic contrast delivery was impossible or was difficult due to an extensive scar deformity preventing adequate insufflation. In the absence of contrast delivery (grade IV–V), 3D ultrasound findings were used.
In patients with grade I–II obliteration, there was a decrease in the contrast delivery rate and a reduction in endometrial pressure. In some patients, insufflation of the uterine cavity was incomplete due to single coarse septa, which also did not provide a complete picture of the altered uterine cavity topography.
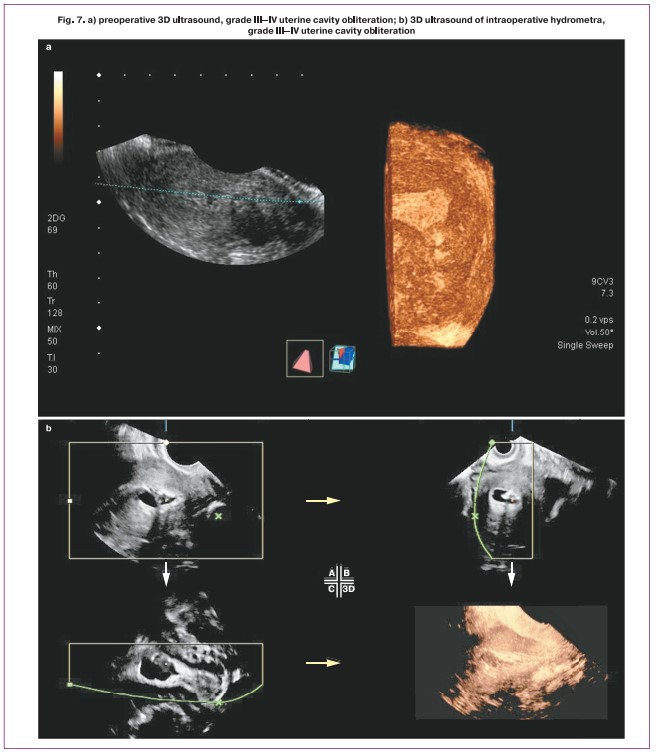
We believe that a trans-rectal scan should be performed during intrauterine surgery with ultrasound navigation [22]. Intraoperative hydrometra (partial or increasingly progressive) provides more comprehensive information about uterine cavity architectonics, considering the use of 3D ultrasound options.
Comparison of the hysteroscopy and 3D ultrasound visual range capabilities [18, 23] showed that 3D ultrasound provided the most comprehensive information on IUA architectonics, especially in grade III–IV obliteration. In contrast to the tunnel view of the cavity in hysteroscopy, the virtual volumetric visualization model of the uterine cavity in 3D ultrasound allowed the determination of topographic landmarks for safe surgical restoration of the normal uterine cavity topography (Fig. 7).
Conclusion
IUAs in reproductive-age women are nowadays associated not only with infection but also on an increased number of iatrogenic factors related to intrauterine surgery, including manual removal of placenta (7%), uterine artery embolization for postpartum hemorrhage (4%), transcervical resection of fibroids (17%), intrauterine septum (4%); intrauterine interventions for pregnancy, and others (68%). Surgical treatment to restore the normal uterine cavity topography and endometrial function requires a highly skilled surgeon because it is associated with a high risk of intraoperative complications, especially in grade III–V obliteration.
Pre- and intraoperative ultrasound examination supplemented by 3D ultrasound and 3D USG, and the identified echographic criteria of IUA, provide the most valuable information on the degree of uterine cavity obliteration and septal architectonics.
Including 3D echography and intraoperative navigation into the IUA diagnostic algorithm can reduce the surgical risks of uterine cavity reconstruction and allow assessment 0f the postoperative period to prevent adhesion recurrence.
Based on our findings, we consider it necessary to include a diagnostic medical sonographer in the surgical team to reduce the risks of perforation and surgical trauma during surgical adhesiolysis.
References
- Popov A.A., Manannikova T.N., Alieva A.S., Fedorov A.A., Bespalova A.G. Intrauterine synechiae: a century later. Russia Journal of Woman and Child Health. 2017; 12: 895-9. (in Russian).
- Khirieva P.M., Adamyan L.V., Martynov S.A. Modern methods of prevention and treatment of intrauterine synechiae (literature review). 2016; 18(5): 32-6. (in Russian).
- Makarenko T.A., Nikiforova D.E., Ulyanova I.O. Intrauterine synechiae: Features of surgical treatment and prevention of recurrence. Medical Council. 2018; 7: 147-51. (in Russian).
- Pulver A.Yu., Pulver N.A., Poltavtseva R.A. Reconstructive approaches to the treatment of secondary infertility. Obstetrics and Gynecology. 2021; 2: 32-8. (in Russian). https://dx.doi.org/10.18565/aig.2021.2.32-38.
- Konci R., Caminsky N., Tulandi T., Dahan M.H. Supplements to conventional treatment after hysteroscopic lysis of intrauterine adhesions: A systematic review. J. Obstet. Gynaecol. Can. 2020; 42(8): 984-1000. https://dx.doi.org/10.1016/j.jogc.2019.09.008.
- Bortoletto P., Keefe K.W., Unger E., Hariton E., Gargiulo A.R. Incidence and risk factors for intrauterine adhesions following myomectomy. J. Minim. Invasive Gynecol. 2020; 27(7, Suppl.): S112.
- Hooker A.B., de Leeuw R.A., Twisk J.W., Brölmann H.A., Huirne J.A. Reproductive performance of women with and without intrauterine adhesions following recurrent dilatation and curettage for miscarriage: long-term follow-up of a randomized controlled trial. Hum. Reprod. 2021; 36(1): 70-81. https://dx.doi.org/10.1093/humrep/deaa289.
- Vancaillie T., Chan K., Liu J., Deans R., Howard E. Asherman syndrome: Audit of a single-operator cohort of 423 cases. N. Z. J. Obstet. Gynaecol. 2020; 60(4): 574-8. https://dx.doi.org/10.1111/ajo.13182.
- Rasmussen C.K., Hansen E.S., Dueholm M. Two- and three-dimensional ultrasonographic features related to histopathology of the uterine endometrial-myometrial junctional zone. Acta Obstet. Gynecol. Scand. 2019; 98(2): 205-14. https://dx.doi.org/10.1111/aogs.13484.
-
Grigore M., Popovici R., Himiniuc L.M., Scripcariu I.S., Toma B.F., Grigore A.M. et al.
The added value of three-dimensional ultrasonography in uterine pathology. Exp. Ther. Med. 2021; 22(5): 1261. https://dx.doi.org/10.3892/etm.2021.10696.
- Ni J., Han B., Liang J., Wang F. Three-dimensional 3D ultrasound combined with power Doppler for the differential diagnosis of endometrial lesions among infertile women. Int. J. Gynaecol. Obstet. 2019; 145(2): 212-8. https://dx.doi.org/10.1002/ijgo.12787.
- Gazhonova V.E. Ultrasound diagnostics in gynecology. 3D. Guide. M.: MedPressInfo; 2003: 83-114. (in Russian).
- Wamsteker K. European Society for Hysteroscopy (ESH) Classification of IUA. 1995.
- Wamsteker K., De Block S.J. Diagnostic hysteroscopy: technique and documentation. In: Sutton C., Diamon M., eds. Endoscopic surgery for gynecologists. New York: Lippincott Williams & Wilkins Publishers; 1995: 263-76.
- Demidov V.N., Gus A.I. Echography of the pelvic organs in women. Issue IV. Pathology of the uterine cavity and endometrium. VMK: practical guide. М.: BINOM Publishing House; 2020: 48-68. (in Russian).
- Soares S.R., Barbosa dos Reis M.M.B., Carnargos A.F. Diagnostic accuracy of sonohysterography, transvaginal sonography, and hysterosalpingography in patients with uterine cavity diseases. Fertil. Steril. 2000; 73(2): 406-10. https://dx.doi.org/10.1016/s0015-0282(99)00532-4.
- Kresowik J.D., Syrop C.H., Van Voorhis B.J., Ryan G.L. Ultrasound is the optimal choice for guidance in difficult hysteroscopy. Ultrasound Obstet. Gynecol. 2012; 39(6): 715-8. https://dx.doi.org/10.1002/uog.11072.
- Bortsvadze Sh.N., Azhibladze T.A., Ishenko A.I. The value of office hysteroscopy in the diagnosis of the uterine factor of infertility and the treatment of such patients. Russian Bulletin of Obstetrician-Gynecologist. 2012; 5: 53-6. (in Russian).
- Kozachenko I.F., Arakelyan A.S., Smolnikova V.Yu., Adamyan L.V. The role of minimally invasive intrauterine interventions in improving the effectiveness of IVF programs. Obstetrics and gynecology. 2020; 9: 97-104. (in Russian). https://dx.doi.org/10.18565/aig.2020.9.97-104.
- Roma D.A., Ubeda B., Ubeda A., Monzón M., Rotger R., Ramos R., Palacio A. Diagnostic value of hysterosalpingography in the detection of intrauterine abnormalities: a comparison with hysteroscopy. AJR Am. J. Roentgenol. 2004; 183(5): 1405-9. https://dx.doi.org/10.2214/ajr.183.5.1831405.
-
Esipova I.А., Kappusheva L.M., Breusenko V.G., Lyafisheva D.M., Ovchinnikova A.V.,
Demidov A.V.
Ultrasound assessment of the uterine wall after hysteroscopic myomectomy of submucous uterine fibroids. Issues of gynecology, obstetrics and perinatology. 2020; 19(4): 5-21. (in Russian). https://dx.doi.org/10.20953/1726-1678-2020-4-5-21. - Svidinskaya E.A., Bortsvadze Sh.N. Ultrasound monitoring in the surgical treatment of intrauterine synechiae. Obstetrics and Gynecology. 2020; 4 (Suppl): 187-8. (in Russian).
- Magos A. Hysteroscopic treatment of Asherman’s syndrome. Reprod. Biomed. Online. 2002; 4(Suppl. 3): 46-51. https://dx.doi.org/10.1016/s1472-6483(12)60116-3.
Received 30.11.2021
Accepted 20.12.2021
About the Authors
Irina A. Esipova, PhD, Associate Professor at the Department of Obstetrics and Gynecology, Faculty of Pediatrics, Pirogov RNRMU, Ministry of Health of Russia, +7(916)345-17-88, esipova.ira@inbox.ru, https://orcid.org/0000-0002-2130-5431, 119415, Russia, Moscow, Lobachevskogo str., 42.Irina A. Krasnova, Dr. Med. Sci., Professor at the Department of Obstetrics and Gynecology, Faculty of Pediatrics, Pirogov RNRMU, Ministry of Health of Russia, +7(916)687-46-73, krasnovairina@mail.ru, https://orcid.org/0000-0002-6765-4127, 119415, Russia, Moscow, Lobachevskogo str., 42.
Valentina G. Breusenko, Dr. Med. Sci., Professor at the Department of Obstetrics and Gynecology, Faculty of Pediatrics, Pirogov RNRMU, Ministry of Health of Russia, +7(985)-725-00-32, breusenkovg@yandex.ru, https://orcid.org/0000-0001-6999-4654, 119415, Russia, Moscow, Lobachevskogo str., 42.
Viktoria B. Aksenova PhD, Department of Obstetrics and Gynecology, Faculty of Pediatrics, Pirogov RNRMU, Ministry of Health of Russia, +7(916)181-28-16, viktoriya-aksenova@yandex.ru, https://orcid.org/0000-0002-8193-7887, 117997, Russia, Moscow, Ostrovytianova str., 1.
Elena G. Timofeeva, Ph.D. student at the Department of Obstetrics and Gynecology, Faculty of Pediatrics, Pirogov RNRMU, Ministry of Health of Russia, +7(926)528-77-74, sonadormonroe@gmail.com, https://orcid.org/0000-0003-3316-3976, 119415, Russia, Moscow, Lobachevskogo str., 42.
Corresponding author: Elena G. Timofeeva, sonadormonroe@gmail.com
Authors' contributions: Esipova I.A. - material processing, manuscript drafting and editing; Krasnova I.A., Breusenko V.G., Esipova I.A. - conception and design of the study, manuscript drafting and editing; Aksenova V.B. - statistical analysis; Timofeeva E.G. - material collection and processing, review of the relevant literature.
Conflicts of interest: The authors have no conflicts of interest to declare.
Funding: There was no funding for this study.
Patient Consent for Publication: All patients provided informed consent for the publication of their data.
Authors' Data Sharing Statement: The data supporting the findings of this study are available on request from the corresponding author after approval from the principal investigator.
For citation: Esipova I.A., Krasnova I.A., Breusenko V.G., Aksenova V.B., Timofeeva E.G. The informative value of ultrasound examination ofpatients with intrauterine adhesions.
Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2022; 1:97-106 (in Russian)
https://dx.doi.org/10.18565/aig.2022.1.97-106