Maternal mortality at the present stage of development of the healthcare system
Objective. To present trends in maternal mortality over 2014-2015, the pattern of causes and an analysis of the preventability of maternal losses.Frolova O.G., Shuvalova M.P., Guseva E.V., Ryabinkina I.N.
Material and methods. The official statistics on maternal mortality from the Russian Federal State Statistics Service and the Ministry of Health of Russia were used.
Results. In 2015, the number of maternal deaths declined to 10.6 per 100,000 live births from 11.9 in 2014. The reduction was registered in all federal districts, except the Siberian and the Crimean ones, which was due to bleeding of ectopic pregnancy, after an abortion.
Conclusion. To reduce maternal mortality is an important task not only of the healthcare system, but also the whole social service. Therefore, the analysis of the causes of maternal deaths in terms of the characteristics of the subjects of the Russian Federation can be the basis for the development of more effective measures to prevent deaths.
Keywords
Maternal mortality is an integrating indicator of the health of women of reproductive age and reflects the result of the interaction of economic, environmental, cultural, social, hygienic, medical and organizational factors on population.
Over the last 25 years, the worldwide maternal mortality rate has declined by 44%. This reduction in the pregnancy-related mortality over a quarter of a century can be viewed as substantial progress, says Dr. Flavia Bustreo, Assistant Director-General for Family, Women’s and Children’s Health. However, it is not an easy task to prevent the death of a woman while pregnant or within 42 days of termination of pregnancy [1].
Globally, there were an estimated 303 000 maternal deaths in 2015, yielding a maternal mortality rate of 12.0 per 100 000 live births in developed countries and 319.0 per 100 000 live births in developing countries (Ghana) [1].
Achieving the maternal mortality rate of less than 70 per 100 000 live births (for the period from 1990 to 2015) became possible with its average annual decline of 2.3%. From 2016, this figure should increase to 7.5% [1].
According to the Ministry of Health of Russia, there were 232 (11.9 per 100 000 live births) and 207 (10.7 per 100 000 live births) maternal deaths in 2014 and 2015, respectively [2, 3].
The Russian Federal State Statistical Service (Rosstat) reports only in-hospital maternal mortality while the data of the Ministry of Health of Russia reflect both in-hospital and out of hospital maternal mortality.
In 2014 and 2015, there were significant differences in maternal mortality in federal districts of Russia (table. 1).
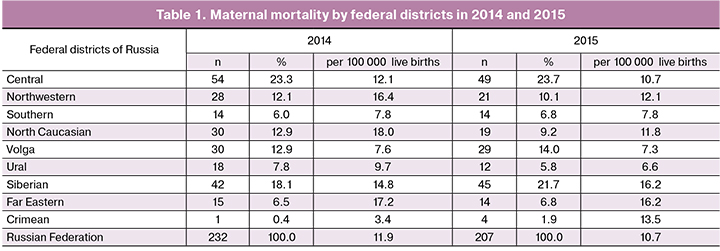
The lowest maternal mortality rates in 2014 were registered in Crimean (3.4 per 100 000 live births), Volga (7.6 per 100 000 live births), and Southern (7.8 per 100 000 live births) federal districts, while the highest rates were observed in North Caucasian (18.0 per 100 000 live births) and Far Eastern (17.2 per 100 000 live births) federal districts [2].
In 2014, no maternal deaths were registered in 17 out of 85 federal subjects of Russia (according to Rosstat, in 18). In 22 federal subjects of Russia (according to Rosstat, in 23), the maternal mortality rate was less than 10.0 per 100 000 live births, that is, it was close to the rates of economically developed countries. In 2015, no maternal deaths were registered in 20 federal subjects.
At the same time, 30 federal subjects of Russia did not attain their targets of reducing maternal mortality rates envisaged by the Road Maps in 2014.
Major causes of maternal mortality in 2014–2015 are presented in table 2.
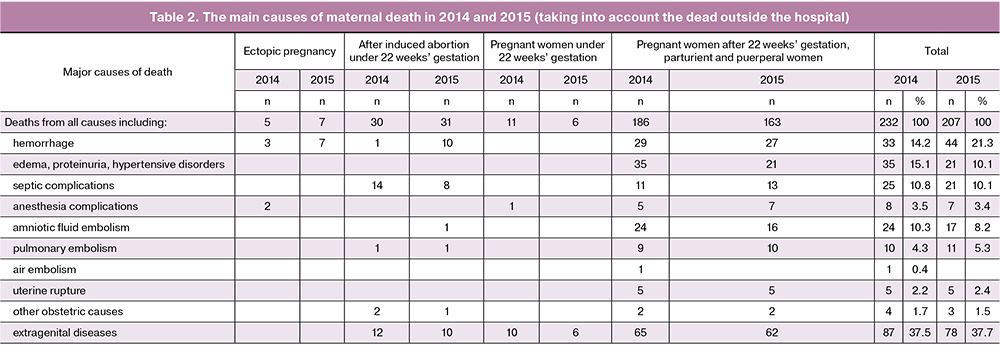
In 2014, extragenital diseases were the major cause of maternal mortality (n = 87; 37.5%). Most of the deaths occurred during and after childbirth (n = 65; 74.5%); 12 women (13.8%) died after induced abortion under 22 weeks’ gestation; 10 women (11.5%) died while pregnant under 22 weeks’ gestation.
The second leading cause of maternal deaths was in edema, proteinuria, and hypertensive disorders (n = 35; 15.1%); 33 (14.2%) women died from hemorrhage. Deaths due to obstetric hemorrhage included in-hospital deaths due to an ectopic pregnancy (n = 3), during childbirth and puerperium (n = 29), and one after an induced abortion.
Twenty-five maternal deaths (10.8%) occurred due to septic complications, including 14 deaths after an induced abortion before 22 weeks’ gestation and 11 deaths of parturient and puerperal women. Amniotic fluid embolism was the cause of death in 24 (10.3%) parturient and puerperal women. Ten maternal deaths (4.3%) occurred due to pulmonary embolism, including nine deaths during childbirth and puerperium, and one after induced abortion.
Uterine rupture during childbirth and puerperium was a cause of death in 5 women (2.2%).
In 2015, there were some changes in the structure of causes of maternal mortality. Of 207 maternal deaths, 163 (79.2%), 31 (15.0%), 7 (3.4%), and six occurred during childbirth and puerperium, after induced abortion, due to ectopic pregnancy, and during pregnancy before 22 weeks’ gestation, respectively [3].
The leading cause of maternal mortality were extragenital diseases (n = 78; 37.7%). Of them, 62 (81.8%), 6 (6.5%), and 10 (11.7%) deaths occurred during childbirth and puerperium, due to induced abortion, and during pregnancy before 22 weeks’ gestation, respectively.
There was an increase in mortality due to obstetric hemorrhage (n = 44; 21.4%) including 27 (61.4%), 10 (22.7%), and 7 (14.9%) deaths during childbirth and puerperium, and due to induced abortion and ectopic pregnancy, respectively.
The number of deaths from edema, proteinuria and hypertensive disorders and septic complications decreased making up 10.2% (n = 21) each.
Maternal mortality from amniotic fluid embolism also decreased to 17 deaths with most of them (16 out of 17) occurring during childbirth and puerperium. The number of deaths from uterine rupture has not changed. The number of deaths from complications of anesthesia decreased from 8 to 7.
The analysis of the preventability of maternal mortality is important to develop measures for their prevention. Expert analysis of the causes of maternal mortality in the subjects of the Russian Federation includes the assessment of the preventability of each death.
An analysis of preventable causes of maternal death is provided below. The analysis was conducted based on data from maternal death reporting cards (registration form No.003/u-MS).
In 2014, according to the Ministry of Health of Russia, 12.9%, 44.0%, and 43.1% of maternal deaths were attributed to preventable causes, conditionally preventable causes, and unavoidable causes, respectively.
The largest proportion of deaths (44.0%) was attributed to conditionally preventable causes including ectopic pregnancy (66.7%), edema, proteinuria, and hypertension disorders (68.6%), anesthesia complications (62.5%), uterine rupture (60%), and obstetric hemorrhage (50%). Among preventable causes (12.9% of the total) were an ectopic pregnancy (33.3%), other causes (50%), anesthesia complications (25.0%), obstetric hemorrhage (23.3%), sepsis and uterine rupture (20.2%). Unavoidable causes of maternal mortality included 100% of deaths from air embolism, 90%, 87.5%, 56.3%, and 26.7% of deaths from a pulmonary embolism, amniotic fluid embolism, extragenital diseases, and obstetric hemorrhage.
In 2015, mortality decreased to 207 maternal deaths (10.7 per 100 000 live births).
There has been a change in the preventability of maternal mortality. Regional expert commissions attributed 31 (15.0%), 86 (41.8%), and 89 (43.2%) deaths to preventable, conditionally preventable, and unavoidable causes, respectively.
Compared to 2014, the number of preventable deaths has somewhat increased, while the number of conditionally preventable deaths has decreased. The proportion of unavoidable deaths has not changed. Among the preventable deaths, the largest percentage falls on uterine rupture (60%) and ectopic pregnancy and anesthesia complications (57.1%) followed by other causes (33.3%), obstetric hemorrhage (27.0%), edema, proteinuria, and hypertensive disorders (28.6%).
The list of preventable causes remained unchanged (sepsis was not registered).
Among conditionally preventable deaths, the highest proportion was attributed to sepsis (66%), other causes (66.7%), edema, proteinuria, and hypertensive disorders (57.1%), obstetric hemorrhage (46.0%), ectopic pregnancy (42.9%), and extragenital diseases (41.6%).
The structure of unavoidable mortality has not changed and included 81.8%, 94.1%, and 55.8% of deaths from pulmonary embolism, amniotic fluid embolism, and extragenital diseases, respectively.
A relatively low percentage of unavoidability was observed among deaths from sepsis (28.6%), obstetric hemorrhage (27%), and uterine rupture (20.0%).
As seen from the above data, the analysis of the preventability of maternal mortality allows estimation of positive changes in the quality of obstetric care regarding major causes of maternal deaths and the need to introduce new preventive, diagnostic and treatment modalities aimed to reduce maternal mortality.
Thus, the problem of reducing maternal mortality can be solved. This is evidenced by the above statistical data. However, the system of measures to further reduce maternal mortality must take into account the level of socio-economic development of the country and regions, as well as the level, quality and availability of medical care.
References
1. Maternal mortality in the Russian Federation in 2014: Methodological letter of Ministry of Health of Russia. Moscow; 2015. (in Russian)
2. Trends in maternal mortality: 1990 to 2015: estimates by WHO, UNICEF, UNFPA, World Bank Group and the United Nations Population Division. [Electronic resource] Available at: http://data.unicef.org/corecode/uploads/ document6/ uploaded_pdfs/corecode/Trends-in-MMR-1990-2015_Full- report_243.pdf
3. Main indicators of obstetric service in the Russian Federation in 2015: Methodological letter of Ministry of Health of Russia. Moscow, 2016. (in Russian)
Received 20.05.2016
Accepted 27.05.2016
About the Authors
Frolova Olga G., MD, PhD, Professor, Consultant of Research Group, Research Center of Obstetrics, Gynecology, and Perinatology, Ministry of Health of Russia. 117997, Russia, Moscow, Ac. Oparina str. 4. Tel.: +74954386948. E-mail: o_frolova@oparina4.ruShuvalova Marina P., MD, PhD, Head of the Department of medical and social research of scientific and organizational support, Research Center of Obstetrics, Gynecology, and Perinatology, Ministry of Health of Russia. 117997, Russia, Moscow, Ac. Oparina str. 4. Tel.: +74954386948. E-mail: m_shuvalova@oparina4.ru
Guseva Elena V., MD, PhD, Deputy Director, Chief of Medical Care for Children and Services Delivery Department, Chief researcher of the Department of Pathology of Newborn, Ministry of Health of Russia
Ryabinkina Irina N., Junior researcher of the Department of Medical and Social Researches of the Scientific and Organizational Support Service, Research Center for Obstetrics, Gynecology and Perinatology, Ministry of Health of Russia. 117997, Russia, Moscow, Ac. Oparina str. 4. Tel.: +74954386948. E-mail: i_ryabinkina@oparina4.ru
For citations: Frolova O.G., Shuvalova M.P., Guseva E.V., Ryabinkina I.N. Maternal mortality at the present stage of development of the healthcare system. Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2016; (12): 121-4. (in Russian)
http://dx.doi.org/10.18565/aig.2016.12.121-4