Clinical course, maternal and perinatal outcomes of 2019 novel coronavirus infectious disease (COVID-19) in pregnant women in Siberia and Far East
Aim. To assess the morbidity, clinical course, maternal and perinatal outcomes of COVID-19 in pregnant women in the Far Eastern and Siberian Federal Districts. Materials and methods. The latest information on COVID-19 in pregnant, parturient and puerperal women was analyzed. The data were presented by chief obstetricians-gynecologists of these Districts in the period from 11 March to 25 December 2020. Results. During the specified period, 8485 cases of COVID-19 were registered in pregnant, parturient and puerperal women. The rate of morbidity was 3 times higher among these women compared to the general population: 5933.2 versus 1960.8 per 100,000 people. In 27.4% of mothers, SARS-CoV-2 infection was asymptomatic; in 52.7% it was mild; in 16.6% – moderately severe, in 2.5% – severe and in 0.5% – very severe. Pregnant women were more often hospitalized and stayed in intensive care and anesthesiology units compared to patients in the general population (3.57% vs 2.24%, р<0.001), and invasive mechanical ventilation (IMV) was used less often (0.48% vs 1.05%, р<0.001). 27.97% (2373) of patients delivered their babies. Preterm delivery was in 18.3% of women, cesarean section – in 42.0%, operative vaginal delivery – in 0.2%. 12 mothers (0.14%) with COVID-19 died (mortality rate was 1.95% in the general population, р<0.001). Maternal mortality rate was 505.69 per 100,000 live births. Perinatal losses were registered in 37 cases (1.54%): stillbirths – 31 (1.29%), early neonatal mortality – 6 (0.25%). 148 (6.2%) cases of COVID-19(+) were detected in newborns. Conclusion. The incidence of COVID-19 in pregnant women in Siberia and Far East is higher than in general population, but the disease is characterized by lower demand for IMV and lower mortality rate. The rates of preterm delivery and cesarean section in patients with COVID-19 were higher than in the general population. Finding of the SARSCoV-2 RNA in newborns suggested vertical transmission of the infection.Belokrinitskaya T.E., Artymuk N.V., Filippov O.S., Frolova N.I.
Keywords
On the 11th of March, 2020, the World Health Organization announced the start of the novel coronavirus infection (NCI) COVID-19 pandemic. The disease caused by a new viral pathogen – severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has rapidly swept across the world and became a severe ordeal for healthcare system, economy and the lives of people in most countries. Due to rapid increase in the number of cases and the massive admission of patients with severe forms of respiratory pathology to hospitals, healthcare settings even in the developed countries were not ready to provide medical care. This led to high mortality in patients with COVID-19 in the first months of pandemic: 13.73% – in Great Britain, 15.2% – France, 13.02% – Italy, 11.64% – Belgium, at the same time the proportion of deaths in China, from where NCI spread, was 5.27%, in the USA – 3.02%, in Russia – 1.74% [1, 2].
Long-term observations have shown that pregnant women have an increased risk of respiratory viral infections conditioned by physiological restructuring of the immune system to maintain tolerance towards the allogeneic fetus, changes in the respiratory system (increased tidal volume per minute, decreased functional residual capacity and total lung capacity, decreased respiratory excursion), which are progressing during gestation [3].
During the previous pandemics of the current century caused by viruses A (H1N1), SARS, MERS, pregnant women also showed higher susceptibility to infectious agents and mortality rate among them was higher than in the general population. According to the large-scale study carried out in Russia during the 2009 swine flu epidemic caused by the A(H1N)1pdm09 virus, the rates of morbidity and mortality in pregnant women was 2.4 times higher than those in the population, and the incidence of pneumonia was 2.5 times higher [4]. According to foreign authors, the mortality rate in pregnant women with SARS-CoV was 18%, with MERS – 25%, with A (H1N1) – 5%; severe forms of the disease, requiring mechanical ventilation (MV) were found in 25%, 41%, 19% of cases, respectively [5].
P. Dashraath et al. (2020) noted, that in pregnant women with SARS-CoV, kidney failure, sepsis, and disseminated intravascular coagulation syndrome was most common; they often required hospitalization in intensive care units; 40% of women required IMV compared to 13% among non-pregnant patients (p=0.07); the mortality rate in pregnant women was also significantly higher (p=0.01) [5]. According to the study of T. Ghi et al. (2020), which was published almost at the same time, pregnant women infected with SARS-CoV-2, on the contrary had severe forms of pneumonia and acute respiratory distress syndrome less frequently than non-pregnant women [6].
Based on the analysis of the available epidemiological data on the prevalence of NCI in pregnant women and the experience acquired during other pandemics, it is logical to assume that the course of COVID-19 in pregnant women, obstetric and perinatal outcomes may differ significantly in populations and ethnic groups, in countries with different levels of economic development, in different climatic and geographical zones, as well as in the districts of one country [1, 2, 4–8].
Currently, the course of the epidemic process caused by the SARSCoV-2 virus continues. The data on morbidity and mortality of the population in different ethnogeographic, age and medical-social groups are accumulated and systematized. The first results are summarized, the clinical, pathogenic and epidemic patterns are deduced.
The territory of the Russian Federation (RF) ranks first in the world (17.1 million square meters). Multiple ethnic subpopulations live in different climatic and geographical zones in the RF. The Far Eastern Federal District (FEFD) and the Siberian Federal District (SFD) cover 2/3 (66.1%) of the country’s territory. Both districts have similar population composition, climatic and economic characteristics.* Thus, it was entirely appropriate to trace the course and outcomes of NCI COVID-19 in pregnant women living in the most part of the territory of the country.
Aim of the study – to assess the incidence, clinical course, maternal and perinatal outcomes of NCI COVID-19 in pregnant women in the Far Eastern and Siberian Federal Districts.
Materials and methods
The latest information on the incidence of NCI COVID-19 and features of the course of the disease in pregnant, parturient and puerperal women was analyzed. The data were presented by chief obstetricians-gynecologists of the FEFD and SFD in the period from March 11 to December 25, 2020.
The SARS-CoV-2 virus was identified using PCR in nasopharyngeal material [7, 8]. Along with this, the frequency of testing the general population and pregnant women in both federal districts was comparable.
Statistical analysis
Qualitative data were presented in numbers (n) and percentages (%) (the number of patients with the symptom and the percentage of patients in the group). Mathematical analysis included descriptive statistics, analysis of contingency tables to calculate χ2 value and the achieved level of significance (p). The values were considered statistically significant at p≤0.05
Results and discussion
The total number of registered cases of NCI COVID-19 in the general population, in pregnant, parturient and puerperal women in the FEFD and SFD is shown in Table 1.
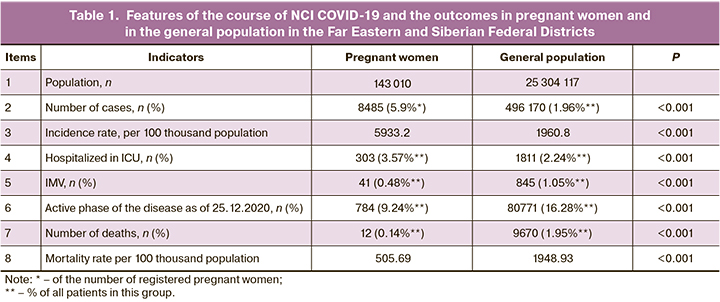
The incidence rate of NCI COVID-19 in the general population (25,304,117) in the FEFD and SFD as of December 25, 2020 was 1,960.8 per 100 thousand population: in the FEFD – 2,294.6 in the SFD – 1,801.7 per 100 thousand population. High number of patients actively sick with COVID-19 – 16.28% (80,771/496,170): 19.26% – in the FEFD and 14.47% – in the SFD (36,104/187,463 and 44,667/308,707, р=0.007); and of those who were hospitalized in ICUs – 2.24% (1,811/80,771) and had IMV – 1.05% (845/80,771) was the evidence of continuing activity of the epidemic process.
Mortality rate in the FEFD was 1.25%, in the SFD – 2.36%. Thus, the total mortality rate among the population in both federal districts due to NCI COVID-19 was 1.95%.
Evaluation of the incidence and clinical course of COVID-19 in pregnant, parturient and puerperal women in the Far East and Siberia at the end of 2020 clearly indicates the continuing activity of the epidemic process and the increased number of severe cases and adverse outcomes [9]. As of December 25, 2020, the percentage of women having an active form of the disease was 9.24% (784/8,485), which, however, was significantly lower than in the general population – 16.28% (80,771/496,170, р<0.001).
 During the first year of the pandemic, the SARS-CoV-2 virus was confirmed in 8485 pregnant, parturient and puerperal women (3267 in the FEFD and 5,218 in the SFD), which amounted to 5.9% of registered pregnant women and 1.71% of the total number of cases in the population. Thus, the incidence of SARS-CoV-2 in pregnant women was 3.0 times higher than in the general population: 5,933.2 versus 1,960.8 per 100 thousand population.
During the first year of the pandemic, the SARS-CoV-2 virus was confirmed in 8485 pregnant, parturient and puerperal women (3267 in the FEFD and 5,218 in the SFD), which amounted to 5.9% of registered pregnant women and 1.71% of the total number of cases in the population. Thus, the incidence of SARS-CoV-2 in pregnant women was 3.0 times higher than in the general population: 5,933.2 versus 1,960.8 per 100 thousand population.
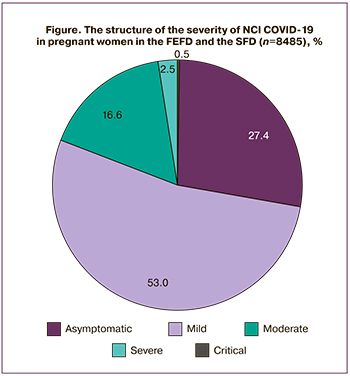
The severity of NCI COVID-19 in pregnant women in the SFD and the FEFD is presented on the Figure. In the studied cohort, 2,324 mothers (27.4%) infected with SARS-CoV-2 had no clinical symptoms of the disease. More than half of the patients had mild COVID-19 – 52.7% (4,471/8,485), while the least number of women had moderate (16.6%, 1,388/8,485), severe (2.5%, 210/8,485) and extremely severe course of the disease (0.5%, 39/8,485).
According to CDC (2020), among 461,825 women with confirmed NCI COVID-19, 409,462 (88.7%) women had the symptoms, and 52,363 (11.3%) women had asymptomatic course of the disease [10].
In the studied population, 3.57% (303/8,485) of pregnant, parturient and puerperal women, who were sick with COVID-19, underwent treatment in ICU; 0.48% (41/8,485) received IMV. Among pregnant women, there was higher percentage of those, who were hospitalized in ICU compared to the general population (3.57% (303/8,485) versus 2.24% (1,811/80,771), p<0.001), but less percentage of those, who received IMV (0.48% (41/8,485) versus 1.05% (845/80,771), p<0.001.
Available published data on the severity of COVID-19, the need for hospitalization in ICU and IMV are contradictory [11–14]. According to M. Knight et al. (2020), the frequency of hospitalizations of pregnant women with NCI COVID-19 in ICUs in the UK was several times higher and amounted to 10% [11]. A significantly higher percentage of pregnant women stayed in ICUs, both in China and in the USA [12, 13]. According to a meta-analysis (J. Juan et al., 2020), about 20% of mothers were hospitalized in intensive care units in China [12]. According to the CDC, 25.1% (5,424/21,573) of pregnant women with COVID-19 received treatment in ICUs, 22.4% required mechanical ventilation (4,825) in the United States [13]. The analysis of 10,996 COVID-19 cases among pregnant women in 15 countries (E.A. Figueiro-Filho et al., 2020) showed that there was a high risk of hospitalization in intensive care units (4.95%), and the need for IMV was significantly higher (35.87%) [14].
In the studied population, 6,112 (72.03%) women continued to carry their pregnancies at the end of 2020. Among 2,373 (27.97%) patients with confirmed SARS-CoV-2 infection, who gave birth during the analyzed period, 30 women had twin pregnancies and 2343 – single pregnancies. In our opinion, this indicator (about 30%) can be taken into account when predicting the number of deliveries in patients with NCI COVID-19 during pandemic.
Pregnancy outcomes in mothers and neonates born to 8,485 women with confirmed SARS-CoV-2 infection are presented in Table 2.
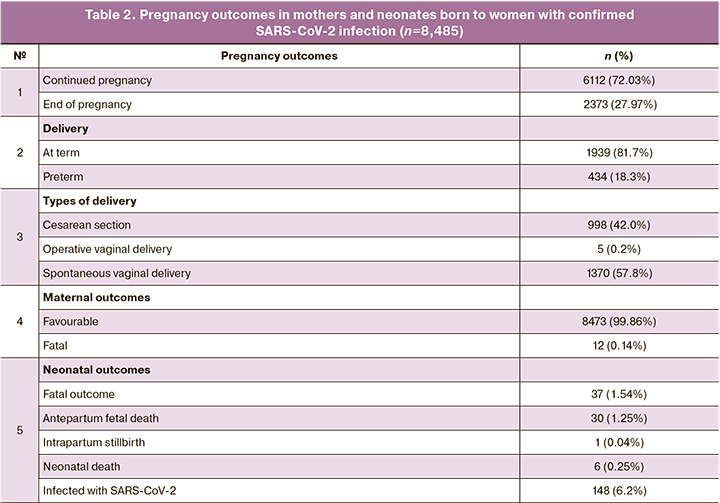
The majority of women delivered their babies at term – 81.7% (1,939/2,373), the percentage of preterm deliveries was 18.3% (434/2,373), which was significantly higher than in Russia – 6.1% (р<0.001) [15]. Most of foreign researchers conclude that COVID-19 is associated with an increased risk of preterm delivery. This may be explained both by the impact of the infectious disease and indications for preterm delivery due to maternal or fetal condition [4, 7, 13, 14, 16]. The meta-analysis by M. Jafari et al. (2021), which included 10,000 pregnant women (121 studies) with COVID-19 and 128,176 non-pregnant women (228 studies) showed that the rate of deliveries before 37 weeks of pregnancy in women with COVID-19 was 25.0%, and relative risk was 2.5 (95% CI: 1.5–3.5) [16]. According to K. Diriba et al. (2020) the percentage of preterm deliveries was 14.3% [17], according to E.A. Figueiro-Filho et al. (2020) it was 25.32% [14].
The results of our study showed that the rate of cesarean deliveries was 42.0% (998/2,373), operative vaginal deliveries (vacuum extraction, obstetrical forceps) – 0.2% (5/2,373). According to the official statistics of the Ministry of Health of the RF, in 2019 the rate of cesarean sections was 30.1%, vaccum extraction – 0.12%, obstetrical forceps – 0,005% [15]. M. Jafari et al. (2021) also showed that pregnant women with COVID-19 have cesarean delivery more often that women without COVID-19 – 48% (risk ratio (RR) = 3; 95% CI: 2–5) [16]. According to K. Diriba et al. (2020), the rate of cesarean sections in SARSCov-2-positive mothers, was higher and amounted to 56.9% [17]; P. Dubey et al. (2020) reported on higher percentage – 72% [18]. This fact is attributed to the increased frequency of critical maternal and fetal condition due to COVID-19. [7, 11, 13, 14, 16–18].
During the analyzed period, 12 (0.14%) patients died among pregnant, parturient and puerperal women (n=8,485). In 11 cases, the cause of death was viral and bacterial pneumonia with progressive respiratory and multiple organ failure, in one case – pulmonary embolism (severity index class 2). COVID-19 death rate in the general population was significantly higher – 1.95% (9,670/496,170, р<0.001). Maternal death rate was 505.69 per 100 thousand livebirths (12/2,372) or 0.51% of the number of patients with COVID-19, who have delivered their babies.
According to the results of the largest meta-analysis (M. Jafari et al., 2021), on the contrary, mortality rate among hospitalized pregnant women was higher and amounted to 11.3% (9.6–13.3), and among non-pregnant patients it was 6.4% (4.4–8.5) [16].
In our opinion, significantly lower rates of severe forms of NCI and mortality among pregnant women in Russia can be explained, first, by the existing pregnancy monitoring system, which allows the timely identification of suspicion for COVID-19 or probable cases of the disease [7, 8]; secondly, by prevention measures for SARS-CoV-2 infection, which were used during the analyzed period. In the guidelines of the WHO and Centers for Disease Control and Prevention of leading professional societies of obstetricians and gynecologists in the world, the basic preventive measures for pregnant women in the ourbreak of pandemic include: wearing face masks, the use of antiseptics, social distancing and self-isolation [7, 8, 19, 20]. In addition to the anti-epidemic measures adopted in the world, the Temporary methodological recommendations for healthcare workers issued by the Ministry of Health of Russia on medical care for the COVID-19 patients, recommended intranasal administration of recombinant interferon-α for pregnant women as medication to prevent the disease [8]. Also, the influence of different approaches on statistical indicators when selecting pregnant women for hospitalization cannot be ruled out. In the Russian Federation, they are severe and moderate forms of the disease, as well as mild forms in the presence of risk factors [2].
As of December 25, 2020, perinatal mortality rate in mothers with confirmed COVID-19 in Siberia and Far East was 15.40 per mille (37/2,403, 1.54%). The highest rate of antenatal mortality was 12.48 per mille (30/2,403, 1.25%), intranatal losses – 0.42 per mille (1/2,403, 0.04%), early neonatal mortality – 2.50 per mille (6/2,372, 0.25%).
According to the conclusions in the latest large-scale studies published at the time of this study, the mortality rates in neonates born to mothers with NCI COVID-19 in other countries were slightly higher than those in the FEFD and the SFD, and amounted to 2.2% according to the results of the meta-analysis by K. Diriba et al. (2020), which included 1,316 pregnant women (39 studies) [17], and 4.2% according to the register of the World Association of Perinatal Medicine (WAPM-study) [21].
The results of our study are consistent with the data obtained in other countries regarding possible vertical transmission of SARSCoV-2 virus from mother to child [11, 12, 14, 16–18, 21]. Despite strict compliance with Temporary Methodological Recommendations on anti-epidemic measures during delivery and isolation of newborn infants from mothers, 148 SARSCoV-2-positive babies were born to 2,373 women (6.2%). Similar birth rates of babies positive for COVID-19 born to sick mothers – 8% (40–16%) were presented in meta-analysis conducted by M. Jafari et al. (2021 [16].
Conclusion
The incidence of COVID-19 in pregnant women in Siberia and Far East is higher than in the general population, but the disease is characterized by mild course with lower demand for IMV and low mortality rate. The rates of preterm delivery and cesarean section in patients with COVID-19 were higher than the average rate in the general population. Despite isolation of newborn infants from mothers, detection of the SARS-CoV-2 RNA in 148 newborns (6.2%) suggests vertical transmission of the infection.
References
- https://ourworldindata.org/excess-mortality-covid. Accessed 11.01.2021.
- https://www.worldometers.info/coronavirus. Accessed 11.01.2021.
- Артымук Н.В., Белокриницкая Т.Е. Клинические нормы. Акушерство и гинекология. Справочник для врачей. М.: ГЭОТАР-Медиа; 2018. 352 с. [Artymuk N.V., Belokrinitskaya T.E. Clinical norms. Obstetrics and Gynecology. Handbook for doctors. M.: GEOTAR-Media; 2018. 352 p. (in Russian)].
- Белокриницкая Т.Е., Шаповалов К.Г. Грипп и беременность. М.: ГЭОТАР-Медиа; 2015. 144 c. [Belokrinitskaya T.E., Shapovalov K.G. Influenza and Pregnancy. M.: GEOTAR-Media; 2015. 144 p. (in Russian)].
- Dashraath P., Wong J.L.J., Lim M.X.K., Lim L.M., Li S., Biswas A. et al. Coronavirus disease 2019 (COVID-19) pandemic and pregnancy. Am. J. Obstet. Gynecol. 2020; 222(6): 521-31. https://dx.doi.org/10.1016/j.ajog.2020.03.021.
- Ghi T., di Pasquo E., Mekinian A., Calza L., Frusca T. Sars-CoV-2 in pregnancy: Why is it better than expected? Eur. J. Obstet. Gynecol. Reprod. Biol. 2020; 252: 476-8. https://dx.doi.org/10.1016/j.ejogrb.2020.07.025.
- Методические рекомендации Минздрава России «Организация оказания медицинской помощи беременным, роженицам, родильницам и новорожденным при новой коронавирусной инфекции COVID-19». Версия 2 от 27.05.2020. 56с. Доступно по: https://rosminzdrav.ru/ministry/med_covid19 12.09.2020. Ссылка активна на 11.01.2021 [Organization of medical care for pregnant women, women in labor, women in labor and newborns with a new coronavirus infection COVID-19. Methodological recommendations. Ministry of Health of Russia. Version 2. 27.05.2020. 56 р. Available at: https://rosminzdrav.ru/ministry/med_covid19 12.09.2020. On 11.01.2021 (in Russian)].
- Временные методические рекомендации Минздрава России «Профилактика, диагностика и лечение новой коронавирусной инфекции (COVID-19)». Версия 9 от 26.10.2020. 236 с. Доступно по: https://static-0.minzdrav.gov.ru/system/attachments/attaches/000/052/550/original/МР_COVID-19_%28v9%29.pdf?1603788097. Ссылка активна на 11.01.2021. [Prevention, diagnosis and treatment of new coronavirus infection (COVID-19). The provisional guidelines. Ministry of Health of Russia. Version 9. 26.10.2020. 236 c. Aviable on: https://static-0.minzdrav.gov.ru/system/attachments/attaches/000/052/550/original/МР_COVID-19_%28v9%29.pdf?1603788097. On 11.01.2021 (in Russian)].
- Белокриницкая Т.Е., Артымук Н.В., Филиппов О.С., Шифман Е.М. Динамика эпидемического процесса и течение новой коронавирусной инфекции COVID-19 у беременных Дальневосточного и Сибирского федеральных округов. Гинекология. 2020; 22(5): 6-11. [Belokrinitskaya T.E., Artymuk N.V., Filippov O.S., Shifman E.M. Dynamics of the epidemic process and the course of the COVID-19 in pregnant women of the Far Eastern and Siberian Federal Districts. Ginekologiya/Gynecology. 2020; 22 (5): 6-11. (in Russian)].
- Zambrano L.D., Ellington S., Strid P., Galang R.R., Oduyebo T., Tong V.T. et al.; CDC COVID-19 Response Pregnancy and Infant Linked Outcomes Team. Update: Characteristics of symptomatic women of reproductive age with laboratory-confirmed SARS-CoV-2 infection by pregnancy status - United States, January 22 - October 3, 2020. MMWR Morb. Mortal Wkly Rep. 2020; 69(44): 1641-7. https://dx.doi.org/10.15585/mmwr.mm6944e3.
- Knight M., Bunch K., Vousden N., Morris E., Simpson N., Gale Ch. et al. Characteristics and outcomes of pregnant women admitted to hospital with confirmed infection in UK: National population based cohort study. BMJ. 2020; 369: m2107. https://dx.doi.org/10.1136/bmj.m2107.
- Juan J., Gil M.M., Rong Z., Zhang Y., Yang H., Poon L.C. Effect of coronavirus disease 2019 (COVID-19) on maternal, perinatal and neonatal outcome: systematic review. Ultrasound Obstet. Gynecol. 2020; 56(1): 15-27. https://dx.doi.org/10.1002/uog.22088.
- https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/special-populations/pregnancy-data-on-covid-19.html. Accessed 20.09.2020.
- Figueiro-Filho E.A., Yudin M., Farine D. COVID-19 during pregnancy: an overview of maternal characteristics, clinical symptoms, maternal and neonatal outcomes of 10,996 cases described in 15 countries. J. Perinat. Med. 2020; 48(9): 900-11. https://dx.doi.org/10.1515/jpm-2020-0364.
- Филиппов О.С., Гусева Е.В. Основные показатели деятельности акушерско-гинекологической службы в Российской Федерации в 2019 году. М.; 2020. 30 с. [Filippov O.S., Guseva E.V. Key performance indicators of the obstetric and gynecological service in the Russian Federation in 2019. Moscow, 2020. 30 p. (in Russian)]
- Jafari M., Pormohammad A., Sheikh Neshin S.A., Ghorbani S., Bose D., Alimohammadi S. et al. Clinical characteristics and outcomes of pregnant women with COVID-19 and comparison with control patients: A systematic review and meta-analysis. Rev. Med. Virol. 2021; Jan 2: e2208. https://dx.doi.org/10.1002/rmv.2208.
- Diriba K., Awulachew E., Getu E. The effect of coronavirus infection (SARS-CoV-2, MERS-CoV, and SARS-CoV) during pregnancy and the possibility of vertical maternal-fetal transmission: a systematic review and meta-analysis. Eur. J. Med. Res. 2020; 25(1): 39. https://dx.doi.org/10.1186/s40001-020-00439-w.
- Dubey P., Reddy S.Y., Manuel S., Dwivedi A.K. Maternal and neonatal characteristics and outcomes among COVID-19 infected women: An updated systematic review and meta-analysis. Eur. J. Obstet. Gynecol. Reprod. Biol. 2020; 252: 490-501. https://dx.doi.org/10.1016/j.ejogrb.2020.07.034.
- CDC Interim guidance for general population disaster shelters during the COVID-19 pandemic. Available at: https://www.cdc.gov/coronavirus/2019-ncov/downloads/Guidance-for-Gen-Pop-Disaster-Shelters-COVID19.pdf
- RCOG. Coronavirus (COVID-19) infection in pregnancy. Version 12: updated 14 October 2020.
- Di Mascio D., Sen C., Saccone G., Galindo A., Grünebaum A., Yoshimatsu J. et al. Risk factors associated with adverse fetal outcomes in pregnancies affected by Coronavirus disease 2019 (COVID-19): a secondary analysis of the WAPM study on COVID-19. J. Perinat. Med. 2020; 48(9): 950-8. https://dx.doi.org/10.1515/jpm-2020-0355.
Received 21.01.2021
Accepted 08.02.2021
About the Authors
Tatiana E. Belokrinitskaya, MD, PhD, Professor, Head of the Obstetrics and Gynecology Department, Chita State Medical Academy, Ministry of Health of Russia. Tel.: +7(3022)32-30-58. E-mail: tanbell24@mail.ru. ORCID: 0000-0002-5447-4223. 39a Gorky str., Chita, 672000, Russian Federation.Natalya V. Artymuk, MD, PhD, Professor, Head of the G.A. Ushakova Department of Obstetrics and Gynecology, Kemerovo State Medical University, Ministry of Health of Russia. Tel.: +7(3842)73-48-56. E-mail: artymuk@gmail.com. ORCID: 0000-0001-7014-6492.
22a Voroshilova str., Kemerovo, 650056, Russian Federation.
Oleg S. Filippov, MD, PhD, Professor, Professor of the Department of Obstetrics and Gynecology, A.I. Evdokimov Moscow State Medical and Dental University, Ministry of Health of Russia, Deputy Director of the Department of Medical Assistance to Children and Obstetrics Aid of the Ministry of Health of Russia. Tel.: +7(495) 609-67-00. E-mail: filippovolsem@yandex.ru. ORCID: 0000-0003-2654-1334. 3 Rakhmanovsky str., Moscow, 127994, Russian Federation.
Nataly I. Frolova, MD, PhD, Associate Professor of the Department of Obstetrics and Gynecology of the Pediatric Faculty, Faculty of Continuing Education and Professional Retraining, Chita State Medical Academy, Ministry of Health of Russia. Tel.: +7(3022)32-30-58. E-mail: taasyaa@mail.ru. ORCID: 0000-0002-7433-6012.
39a Gorky str., Chita, 672000, Russian Federation.
For citation: Belokrinitskaya T.E., Artymuk N.V., Filippov O.S., Frolova N.I. Clinical course, maternal and perinatal outcomes of 2019 novel coronavirus infectious disease (COVID-19) in pregnant women in Siberia and Far East
Akusherstvo i Ginekologiya/ Obstetrics and gynecology. 2021; 2: 48-54 (in Russian)
https://dx.doi.org/10.18565/aig.2021.2.48-54