Clinical and medical history characteristics of pregnant women with different cervical cytology results
Rosyuk E.A., Oboskalova T.A., Zornikov D.L., Ten A.R., Askerova M.G., Sevostyanova O.Yu., Soloviev D.V., Kudimov A.A., Bikbulatova E.R., Averchenkova E.A.
Objective: To determine the clinical and medical history characteristics of pregnant women with different cervical cytology results.
Materials and methods: This retrospective study included 349 patients aged 18–44 years (median=32,
Q25–Q75: 29–36). Group 1 included pregnant women without a history of cervical surgery and NILM cytology reports (n=136); group 2 included pregnant women with a history of cervical conization (before pregnancy) for obligate precancer and NILM cytology reports at the time of inclusion in the study (n=67); group 3 included pregnant patients with mild dysplasia (LSIL by cytology, n=63), and group 4 included pregnant patients with severe dysplasia (HSIL according to cytology, n=83). Statistical analysis and data visualization were performed using R version 4.4.0 (build 2024-04-24). The statistical significance of differences between categorical variables was assessed using two-tailed Fisher's exact test, and differences between continuous variables were assessed using the Kruskal-Wallis test. Differences were considered statistically significant at p<0.05.
Results: Pregnant women with HSIL cytology had a nicotine addiction rate of 44.6% (p<0.001), initiated sexual activity at ages 16–18 (p<0.001), a high abortion rate of 59% (p=0.005), and a high birth rate of 83.1% (p=0.016). They also had a high rate of gynecological diseases in general (65.1%, p=0.018) as well as sexually transmitted infections, HIV infections, and viral hepatitis C. Patients with NILM cytology had a higher rate of endometriosis (p=0.018) and ovarian lesions (p=0.037) than those with abnormal cytology. Women with a history of cervical conization were distinguished by the absence of allergic reactions compared to those in the other groups (p<0.001). There were no differences in the rates of extragenital diseases.
Conclusion: Distinct medical history characteristics were observed in patients, depending on the results of the cytological examination. All pregnant women exhibited low adherence to the use of contraceptive methods, a significant number of pregnancy terminations, and high parity.
Authors' contributions: Rosyuk E.A., Oboskalova T.A. – conception and design of the study; Zornikov D.L. – statistical analysis, editing of the manuscript; Soloviev D.V., Kudimov A.A., Bikbulatova E.R., Averchenkova E.A. – material collection; Rosyuk E.A., Ten A.R., Askerova M.G., Sevostyanova O.Yu. – drafting of the manuscript.
Conflicts of interest: The authors have no conflicts of interest to declare.
Funding: There was no funding for this study.
Ethical Approval: The study was reviewed and approved by the Research Ethics Committee of the Ural State Medical University, Ministry of Health of the Russian Federation.
Patient Consent for Publication: All patients provided informed consent for the publication of their data.
Authors' Data Sharing Statement: The data supporting the findings of this study are available upon request from the corresponding author after approval from the principal investigator.
For citation: Rosyuk E.A., Oboskalova T.A., Zornikov D.L., Ten A.R., Askerova M.G., Sevostyanova O.Yu., Soloviev D.V., Kudimov A.A., Bikbulatova E.R., Averchenkova E.A. Clinical and medical history characteristics of pregnant women with different cervical cytology results.
Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2025; (1): 73-81 (in Russian)
https://dx.doi.org/10.18565/aig.2024.226
Keywords
All women infected with highly oncogenic human papillomavirus (HPV) are at risk of cervical cancer, but this risk does not always translate into disease [1]. Pregnancy does not affect cervical cancer screening regimens; however, if a high risk of invasion is detected based on cytology and colposcopy, management of pregnant women with cervical intraepithelial neoplasia (CIN) involves several considerations [2]. A literature review by Larish A. and Long M.E. [3] indicated that CIN diagnosed during pregnancy tends to remain stable with frequent regression in the postpartum period, although this is not a universal phenomenon. Colposcopic examination during pregnancy can be challenging. Although a biopsy during pregnancy is subjectively associated with increased bleeding, it does not increase the risk of complications. However, diagnostic cervical curettage and accelerated treatment are not acceptable. The treatment of CIN II–III during pregnancy is not recommended. Excisional biopsy is performed during pregnancy when malignancy is suspected but cannot be confirmed by colposcopic biopsy or when biopsy results may affect oncologic treatment or pregnancy management. For the surveillance of high-grade lesions during pregnancy, HPV testing, cytology, and colposcopy with biopsies of worsening lesions are performed every 12–24 weeks from diagnosis until postpartum evaluation. The mode of delivery does not definitively affect the persistence of CIN in the postpartum period. Cytological and colposcopic examinations are performed in the postpartum period, based on which a decision is made regarding excision or conization of the cervix [3, 4]. Thus, the goal of perinatal management of patients with cervical disease is to improve outcomes for cervical cancer diagnosed during pregnancy as opposed to after delivery and to facilitate further evaluation and treatment of postpartum disease with smaller lesions. Invasive cervical procedures are often delayed until the postpartum period. These findings underscore the need for obstetrician-gynecologists to understand whether there are differences in the medical histories of pregnant patients with normal and abnormal cytology. This knowledge will help assess the degree of risk of disease progression, the need for invasive procedures during pregnancy, or the possibility of postponing them until the postpartum period, as a comprehensive profile is developed for pregnant patients with abnormal cytologic examination results.
This study aimed to determine the clinical and medical history characteristics of pregnant women with different cervical cytology results.
Materials and methods
This study was conducted at the Ural State Medical University of the Ministry of Health of Russia and the Consultative and Diagnostic Outpatient Clinic of the Yekaterinburg Clinical Perinatal Center from 2023 to 2024. This retrospective study included 349 patients aged 18–44 years (median=32; Q25–Q75: 29–36). All patients were classified into the following groups based on the results of cytological examination.
Group 1 – Pregnant women with no history of cervical surgery who had an NILM cytology report (negative for intraepithelial lesion or malignancy) (n=136);
Group 2 – Pregnant women with a history of cervical conization (prior to pregnancy) for obligate precancer who had an NILM cytology report at the time of enrollment (n=67);
Group 3 – Pregnant patients with low-grade squamous intraepithelial lesion (LSIL) according to cytology (n=63);
Group 4 – Pregnant patients with high-grade squamous intraepithelial lesion (HSIL) according to cytology (n=83).
The inclusion criteria for the study were pregnancy, a cytological report in the first trimester of pregnancy, and age between 18 and 45 years. Exclusion criteria included abnormal cytology results other than LSIL and HSIL (e.g., ASC-US (atypical cells of undetermined significance), AGS-NOS (atypical glandular cells of undetermined significance).
Pregnant women with abnormal cytology were included in this study by using a continuous sampling method. The authors observed all patients in the cervical pathology office during the specified time period who met the above criteria. The group of pregnant women with an NILM cytology report and no history of cervical surgery included women who were observed in the Yekaterinburg Clinical Perinatal Center during the same time as those with abnormal cytology. Pregnant women under 18 years of age (13, 16, and 17 years) were not included in the study.
Statistical analysis
Statistical analysis and data visualization were performed using R version 4.4.0 (build 2024-04-24). The normality of the distribution was tested using the Shapiro–Wilk test. The median, along with the 0.25 and 0.75 percentiles, was used as a measure of central tendency. Proportions were compared using two-tailed Fisher’s exact test for categorical variables and Kruskal-Wallis test for continuous variables. Differences were considered statistically significant at p<0.05.
Results
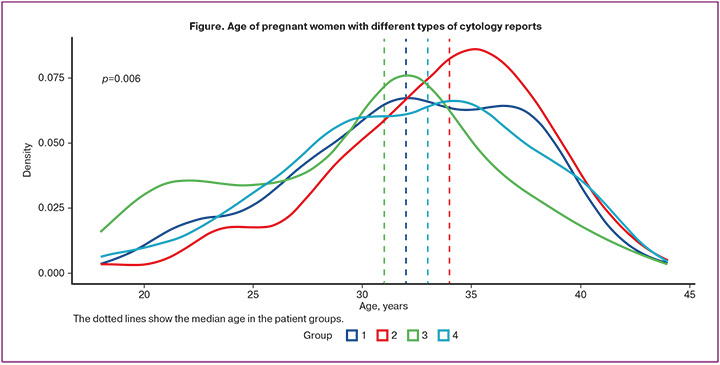
The mean age of patients in the study groups was as follows: 32 (28.8–37) years for group 1; 34 (31–37) years for group 2; 31 (26–33) years for group 3; and 33 (29–36) years for group 4 (Figure). Patients with a history of cervical conization were significantly older than women with LSIL cytology reports of 34 and 31 years, respectively (p2-3=0.003) (Table 1).
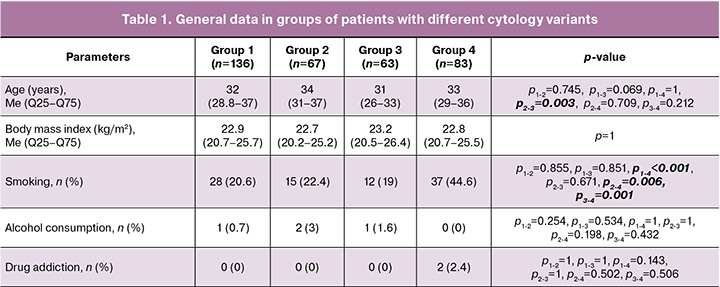
The body mass index of pregnant women at the time of registration did not demonstrate any statistically significant differences. Additionally, there were no statistically significant differences in the frequency of alcohol and drug use according to the medical history of the patients. However, a higher proportion of patients in group 4 were identified as having nicotine addiction: 37/83 (44.6%) (p1-4<0.001, p2-4=0.006, p3-4=0.001) (Table 1).
The mean age at menarche of patients in the study groups was 13 years. Women with abnormal cytology had a significantly lower age at the onset of sexual activity (p1-2=0.007, p1-3=0.029, p1-4<0.001, p3-4=0.033) (Table 2). In all groups, women did not use reliable contraception before pregnancy, with a frequency of 77.8 to 87.5%. Condoms were used at frequencies of 1/136 (0.7%), 0/67 (0%), 4/63 (6.3%), and 6/83 (7.2%), respectively, and there were statistically significant differences between the groups (p1-3=0.036, p1-4=0.013, p2-4=0.036). Combined oral contraceptives were used with a frequency of 17/136 (12.6%) in group 1, 7/67 (10.9%) in group 2, 12/63 (19%) in group 3 and 7/83 (8.4%) in group 4 (p>0.05) (Table 2). The structure of gynecological diseases in female patients of the studied groups included: menstrual cycle disorders – 13/136 (9.6%), 12/67 (18.5%), 5/63 (7.9%), 9/83 (10.8%), respectively (p˃0.05); endometriosis – 8/136 (5.9%), 6/67 (9.2%), 0/63 (0%) and 1/83 (1.2%) (statistically significant in women of group 2 compared to patients of groups 3 and 4); ovarian neoplasms – 12/136 (8.8%), 5/67 (7.7%), 0/63 (0%) and 3/83 (3.6%) (statistically significant differences in women of group 1 compared to patients of group 3, p=0.011); hyperplastic processes of the endometrium – 13/136 (9.6%), 5/67 (7.7%), 22/63 (34.9%) and 24/83 (28.9%) (statistically significant in women of groups 3 and 4 compared to patients of groups 1 and 2, p<0.001); inflammatory diseases of the pelvic organs – 5/136 (3.7%), 2/67 (3.1%), 2/63 (3.2%), 2/83 (2.4%) (p˃0.05); uterine leiomyoma – 11/136 (8.1%), 9/67 (13.8%), 8/63 (12.7%), 7/83 (8.4%) (p˃0.05); sexually transmitted infections – 5/136 (3.7%), 1/67 (1.5%), 8/63 (12.7%), 11/83 (13.3%) (statistically significantly more common in women of groups 3 and 4 compared to patients of groups 1 and 2), respectively (Table 2). In general, gynecological diseases occurred in patients in all four groups but at different frequencies. They were less common in group 1 (62/136, 45.6%) and in group 2 (36/67, 55.4%), and more common in group 3 (40/63, 63.5%) and in group 4 (54/83, 65.1%) (statistically significant differences between groups: p1-3=0.022, p1-4=0.005) (Table 2). Patients in all four groups had a history of pregnancy: group 1, 106/136 (78.5%); group 2, 44/67 (69.8%); group 3, 50/63 (79.4%); and group 4, 75/83 (90.4%); the highest number of pregnancies was noted in patients with HSIL cytology. The pregnancy termination rates at the request of women in groups 1, 2, and 3 were 52/136 (38.5%), 21/67 (33.3%) and 23/63 (36.5%), respectively. The high percentage of terminations of pregnancy in general is depressing, and in women with HSIL cytology, this figure was 49/83 (59%), which was statistically significantly higher than in women in other groups (p<0.003). The number of deliveries among the women included in the study was 93/136 (68.9%) in group 1, 38/67 (60.3%) in group 2, 47/63 (74.6%) in group 3, and 69/83 (83.1%) in group 4 (statistically significant differences between the groups: p1-4=0.025, p2-4=0.003). Pre-pregnancy infertility was predominantly experienced by women with NILM cytology: 15/136 (11%) in group 1, 12/67 (18.5%) in group 2, while in group 3 it was 5/63 (7.9%) in group 4 it and 2/83 (2.4%) (statistically significant differences between the groups: p1-4=0.02, p2-4=0.001). In this case, pregnancy occurred as a result of using various assisted reproductive technologies (ART) in 13/136 (9.6%) patients in group 1, 7/67 (10.8%) in group 2, 3/63 (4.8%) in group 3, and 2/83 (2.4%) in group 4 (p˃0.05). Miscarriage occurred with almost the same frequency in all four groups and amounted to 7.2 to 7.9% (p=1) (Table 2).
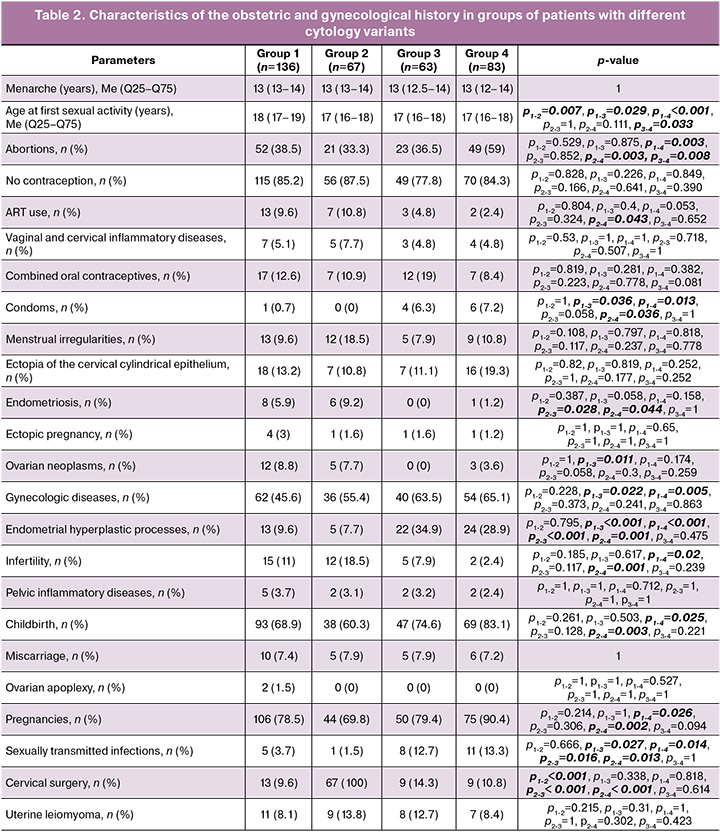
Cervical surgery before pregnancy (excision or conization of the cervix, ablative methods of treating the cervix) were performed in 67/67 (100%) patients in group 2; in other groups, they occurred with equal frequency: 13/136 (9.6%) in group 1, 9/63 (14.3%) in group 3, and 9/83 (10.8%) in group 4 (significant differences: p1-2<0.001, p2-3<0.001, p2-4<0.001). Ectopia of the cervical cylindrical epithelium was observed in 18/136 (13.2%) women in group 1, 7/67 (10.8%) in group 2, 7/63 (11.1%) in group 3, and 16/83 (19.3%) in group 4 (p˃0.05).
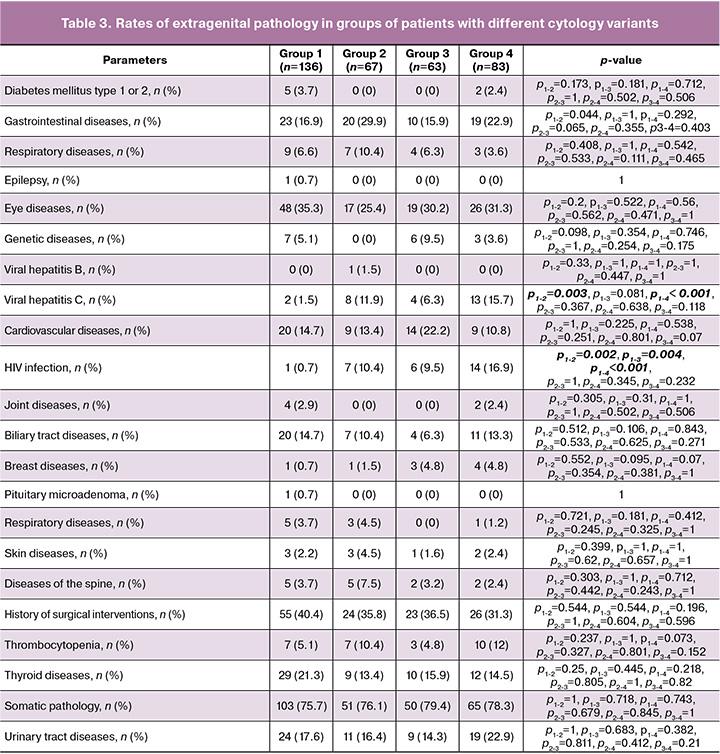
Statistically significant differences were observed in the detection rate of allergic reactions in pregnant women in the studied groups: group 1, 24/136 (17.6%); group 2, 0/67 (0%); group 3, 9/63 (14.3%); and group 4, 14/83 (16.9%) (p<0.001). No statistically significant differences were observed in the detection rates of most extragenital diseases. Their rates were 103/136 (75.7%) in group 1, 51/67 (76.1%) women in group 2, 50/63 (79.4%) patients in group 3 and 65/83 (78.3%) subjects from group 4 (p>0.05) (Table 3). In particular, no differences were observed in the detection rates of type 1 and 2 diabetes mellitus, gastrointestinal diseases, respiratory diseases, epilepsy, eye diseases, genetic diseases, cardiovascular diseases, joints, biliary tract, mammary gland, pituitary microadenoma, skin and spinal column diseases, blood diseases, thyroid gland, or urinary tract. Statistically significant differences were found in the prevalence of viral hepatitis C, including 2/136 (1.5%) in group 1, 7/67 (10.4%) in group 2, 6/63 (6.3%) in group 3, and 13/83 (15.7%) in group 4 (p1-2=0. 003, p1-4<0.001). Additionally, HIV infection was observed, in 1/136 (0.7%) patient in group 1, 7/67 (10.4%) in group 2, 6/63 (9.5%) in group 3, and 14/83 (16.9%) in group 4 (p1-2=0.002, p1-3=0.004, p1-4<0.001) (Table 3).
Discussion
Most pregnant women with abnormal cytology were over 30 years of age, and most patients with a history of conization were over 35 years of age (p2-3=0.003). Currently, the leading theory of the pathogenesis of cervical cancer involves a series of sequential changes in epithelial cells from HPV carriage to dysplastic changes: first, one-third of the epithelial thickness corresponds to CIN I or LSIL; then, two-thirds corresponds to CIN II or HSIL; and finally, changes in the entire thickness of the epithelium correspond to CIN III or HSIL. The pathogenesis of CIN development during pregnancy mirrors that in the absence of pregnancy [4]. In the present study, the age of the examined pregnant women generally aligned with this pathogenetic concept. Notably, the highest average age was observed in the group of patients who had previously undergone cervical conization (prior to pregnancy) for obligate precancer. Younger ages were noted in patients with HSIL, and even younger ages were found in patients with a normal cytological picture (Figure). Interestingly, the youngest patients were those with LSIL, which likely reflects a second peak in age at 21–22 years. This observation may indicate an earlier onset of HPV infection among the patients in recent years.
This study demonstrated that pregnant women with NILM, LSIL, and HSIL cytology exhibited notable differences. In particular, it reaffirmed the established facts that smoking and early onset of sexual activity contribute to the development of precancerous processes in the cervix [5]. Patients with HSIL were more likely to be nicotine-dependent (44.6%) than other groups of pregnant women, and the onset of sexual activity for women in this group often occurred between the ages of 16 and 18 years.
It is also possible to support the notion that condoms do not provide complete protection against HPV, as pregnant women with LSIL and HSIL cytology were significantly more frequently reported using barrier methods of contraception (6.3% and 7.2%, respectively) than patients in the first two groups (0.7% and 0%, respectively). Alternatively, the use of condoms may have been coupled with a greater number of sexual partners among women with abnormal cytology results [6].
It should also be noted that the pregnant women in all groups used unreliable methods of contraception or did not use contraception at all (from 77.8% to 87.5%). This may explain the high percentage of abortions across all four groups; the smallest proportion (33.3%) was found in group 3, while the largest proportion (59%) occurred in patients with a cytology conclusion of HSIL (p1-4=0.003, p2-4=0.003, p3-4=0.008). Additionally, these patients exhibited a significantly higher prevalence of a childbirth history (83.1%). This reinforces the understanding that trauma to the cervical tissue (including that caused by abortion and childbirth) can be an additional risk factor for the development of cervical precancer in the context of HPV persistence.
Researchers from China and Japan have published data indicating that a high number of pregnancies, abortions, various types of transformation zones, and other factors in the treatment of cervical pathology do not serve as risk factors that reduce the percentage of cure but rather as risk factors for the development of CIN [7]. In general, women with LSIL and HSIL cytology results had a higher prevalence of gynecologic diseases in their medical history (63.5% and 65.1 %, respectively). Among these diseases, a significant percentage of endometrial hyperplastic processes was observed in patients with abnormal cytology: 34.9% in pregnant women with LSIL and 28.9% in those with HSIL. In contrast, patients with NILM cytology results had rates of 9.6% in group 1 and 7.7% in group 2. Evidence suggests that the presence of a viral infection, which leads to abnormal cytology, provokes proliferation of the endometrium, resulting in chronic endometritis and endometrial hyperplasia [8].
Endometriosis was more frequently detected in pregnant women after cervical conization with NILM cytology (9.2%) and in patients with NILM cytology without cervical surgery (5.9%). In patients with HSIL cytology, endometriosis was noted in only 1.2% of cases, and none were observed in patients with LSIL. A study on the association between endometriosis and CIN conducted in Greece found that 70% of the patients with CIN also had endometriosis. A high prevalence of HPV and rare detection of CIN II and III have been reported in patients with endometriosis [9]. Although the pathophysiology and genetics of cervical dysplasia are well described, further studies are necessary to establish an association between endometriosis and gynecologic precancerous and malignant pathologies.
Ovarian neoplasms were diagnosed more frequently before pregnancy in women with NILM cytology, with a prevalence of 8.8% in patients who did not undergo cervical surgery and 7.7% in women who underwent cervical conization. Previous studies have shown that the expression of the p16 gene, which is used in the immunohistochemical assessment of CIN, is elevated in some ovarian serous carcinomas [10]. However, it is inappropriate to extrapolate these findings to the results obtained in this study, as patients in groups 1 and 2 had only benign ovarian neoplasms prior to pregnancy.
It is noteworthy that patients with NILM cytology reported higher rates of infertility: 11% in group 1 and 18.5% in group 2. In contrast, patients with abnormal cytology experienced infertility less frequently (7.9% and 2.4% for LSIL and HSIL, respectively). A prospective cohort study involving 9,586 women planning pregnancy in Denmark and the USA over 13 years of age found no association between CIN and fertility. Only in cases of CIN II–III was there a slight decrease in fertility observed during the two years following diagnosis (outpatient medical supervision period) [11].
Sexually transmitted infections were significantly more prevalent among patients with LSIL (12.7%) and HSIL (13.3%). Somatic pathology was not identified as a risk factor for the development of abnormal cytology, except for viral hepatitis C and HIV infection. In the group of women with HSIL cytology, these infections were found in 15.7% and 16.9% of patients, respectively. Among pregnant women who had undergone cervical conization, these infections occurred in 11.9% and 10.4% of patients, respectively. Patients with immunodeficiency, particularly when combined with sexually transmitted infections, show a higher prevalence of precancerous changes in the cervix than in the general population [12].
Interestingly, there was an absence of a history of allergic reactions in pregnant women following cervical conization (this group included women who underwent surgery for obligate precancer of the cervix, primarily CIN III), whereas the rate in the other groups ranged from 14.3% to 17.6%. This observation aligns with previous findings regarding the lower overall prevalence of allergies in patients with certain types of cancer [13]. This phenomenon may be attributed to the decreased reactivity of the immune system, which may concurrently increase the risk of infections and malignancies while reducing the risk of allergic reactions [14].
Conclusion
The clinical and medical history characteristics of pregnant women with HSIL cytology results include the onset of sexual activity at ages 16–18 years, a high prevalence of nicotine addiction, and a considerable number of abortions and births. They also exhibited a higher prevalence of sexually transmitted infections (caused by Chlamydia trachomatis, Mycoplasma genitalium, and Trichomonas vaginalis), viral hepatitis C, HIV infection, and gynecologic diseases, particularly endometrial hyperplastic processes. Pregnant women who have undergone cervical conization typically have no history of allergic reactions, along with a high prevalence of viral hepatitis C and HIV infection. Pregnant women with NILM cytology and no history of cervical surgery had a high prevalence of endometriosis, ovarian cysts, and infertility. Pregnant women with LSIL cytology are generally younger and have a higher prevalence of gynecologic diseases and sexually transmitted infections, although these rates are somewhat lower than those of pregnant women with HSIL. All the pregnant women had low contraceptive adherence, with a significant number of pregnancy terminations and high parity.
References
- Гарелик Т.М., Наумов И.А. Выявление медико-социальных факторов риска рака шейки матки и ухудшения репродуктивного здоровья. Современные проблемы гигиены, радиационной и экологической медицины. 2020; 10: 69-82. [Harelik T.M., Naumau I.A. Identification of medical-social risk factors of cervical cancer and deterioration of reproductive health. Modern Problems of Hygiene, Radiation and Environmental Medicine. 2020; (10): 69-82. (in Russian)].
- Росюк Е.А., Обоскалова Т.А., Емельянова Е.С., Буторина Н.В., Емельянова Т.Г., Глухов Е.Ю., Нефф Е.И., Якушев А.М. Влияние электроконизации шейки матки до зачатия на течение беременности и родов. Акушерство и гинекология. 2024; 6: 105-12. [Rosyuk E.A., Oboskalova T.A., Emelyanova E.S., Butorina N.V., Emelyanova T.G., Glukhov E.Yu., Neff E.I., Yakushev A.M. Effect of preconceptional cervical electroconizationon the course of pregnancy and childbirth. Obstetrics and Gynecology. 2024; (6): 105-12 (in Russian)]. https://dx.doi.org/10.18565/aig.2024.23.
- Larish A., Long M.E. Diagnosis and management of cervical squamous intraepithelial lesions in pregnancy and postpartum. Obstet. Gynecol. 2024; 144(3): 328-38. https://dx.doi.org/10.1097/AOG.0000000000005566.
- Министерство здравоохранения Российской Федерации. Клинические рекомендации. Цервикальная интраэпителиальная неоплазия, эрозия и эктропион шейки матки. 2020. 57с. [Ministry of Health of the Russian Federation. Clinical guidelines. Cervical intraepithelial neoplasia, erosion and ectropion of the cervix. 2020. 57p. (in Russian)].
- Росюк Е.А., Обоскалова Т.А., Верба Т.Е., Салимова И.В., Туреева А.В. Анализ структуры гинекологических заболеваний и объема оперативного вмешательства у пациенток кабинета патологии шейки матки и эндометрия в разных возрастных группах. Акушерство и гинекология. 2024; 5: 92-8. [Rosyuk E.A., Oboskalova T.A., Verba T.E., Salimova I.V., Tureeva A.V. Analysis of the structure of gynecological diseases and extent of surgery in patients of different age groups supervised in the cervical and endometrial pathology office. Obstetrics and Gynecology. 2024; (5): 92-8 (in Russian)]. https://dx.doi.org/10.18565/aig.2024.6.
- Orya E.E., Bello K.K., Sampson S., Envuladu E.A., Okagbue H.I. Varying behavioral differences and correlates of HPV infection among young adolescents in Benue state, Nigeria. BMC Public Health. 2024; 24(1): 1548. https://dx.doi.org/10.1186/s12889-024-19068-7.
- Chen L., Zhang Y., Liu L., Hayashi T., Cui N., Liu Y. Risk factors predicting pathological degradation after cervical excision in cervical intraepithelial neoplasia grade II P16-positive patients over 25 years old: a cross-sectional study. Transl. Cancer Res. 2023; 12(11): 3147-55. https://dx.doi.org/10.21037/tcr-23-1745.
- Зароченцева Н.В., Аршакян А.К., Титченко Ю.П., Меньшикова Н.С., Баринова И.В., Ушакова С.В. Применение препарата аллокина-альфа в комплексной терапии пациенток с хроническим эндометритом и привычным невынашиванием беременности. Российский вестник акушера-гинеколога. 2014; 14(4): 74‑80. [Zarochentseva N.V., Arshakian A.K., Titchenko Iu.P., Men'shikova N.S., Barinova I.V., Ushakova S.V. Use of allokine-alpha in the combination therapy of patients with chronic endometritis and recurrent miscarriage. Russian Bulletin of Obstetrician-Gynecologist. 2014; 14(4): 74-80. (in Russian)].
- Matalliotakis M., Matalliotaki C., Zervou M.I., Krithinakis K., Kalogiannidis I., Goulielmos G.N. Coexistence of cervical endometriosis with premalignant and malignant gynecological pathologies: report on a series of 27 cases. Women Health. 2021; 61(9): 896-901. https://dx.doi.org/10.1080/03630242.2021.1991073.
- O'Neill C.J., McCluggage W.G. p16 expression in the female genital tract and its value in diagnosis. Adv. Anat. Pathol. 2006;13(1): 8-15. https://dx.doi.org/10.1097/01.pap.0000201828.92719.f3.
- Kristensen M.L., Waldstrøm M., Laursen A.S.D., Eriksen K., Ulrichsen S.P., Hatch E.E. et al. Cervical intraepithelial neoplasia and fecundability: a prospective cohort study. Hum. Reprod. 2024; 39(8): 1835-43. https://dx.doi.org/10.1093/humrep/deae139.
- Бебнева Т.Н., Дикке Г.Б. Алгоритм диагностики заболеваний шейки матки и ведения беременных женщин, инфицированных ВПЧ. Акушерство и гинекология. 2020; 12(Приложение): 22-5. [Bebneva T.N., Dicke G.B. Algorithm for the diagnosis of cervical diseases and management of pregnant women infected with HPV. Obstetrics and Gynecology. 2020; 12(Suppl.):22-5. (in Russian)].
- Kozłowska R., Bożek A., Jarząb J. Association between cancer and allergies. Allergy Asthma Clin. Immunol. 2016; 12: 39. https://dx.doi.org/10.1186/s13223-016-0147-8.
- Joost van Neerven J. Mucosal immunity: barriers, bugs, and balance. Wageningen University; 2014. Available at: https://edepot.wur.nl/330156.
Received 09.09.2024
Accepted 23.12.2024
About the Authors
Elena A. Rosyuk, PhD, Associate Professor at the Department of Obstetrics and Gynecology, Ural State Medical University, Ministry of Health of Russia, 620028, Russia, Yekaterinburg, Repin str., 3, +7(902)26-56-385, elenakdc@yandex.ru, https://orcid.org/0000-0003-1303-3955Tatyana A. Oboskalova, Dr. Med. Sci., Professor, Head of the Department of Obstetrics and Gynecology, Ural State Medical University, Ministry of Health of Russia,
620028, Russia, Yekaterinburg, Repin str., 3, +7(912)28-37-631, oboskalova.tat@yandex.ru, https://orcid.org/ 0000-0003-0711-7896
Danila L. Zornikov, PhD, Associate Professor, Head of the Laboratory of Genetic and Epigenetic Foundations for Predicting Disorders of Ontogenesis and Human Aging, Associate Professor at the Department of Medical Microbiology and Clinical Laboratory Diagnostics, Ural State Medical University, Ministry of Health of Russia,
620028, Russia, Yekaterinburg, Klyuchevskaya str., 17, +7(900)20-65-926, zornikovdl@yandex.ru, https://orcid.org/0000-0001-9132-215X
Angelika R. Ten, PhD, Teaching Assistant at the Department of Obstetrics and Gynecology with a Course of Medical Genetics, Ural State Medical University,
Ministry of Health of Russia, 620028, Russia, Yekaterinburg, Repin str., 3, +7(912)20-30-241, tenar79@mail.ru, https://orcid.org 0000-0002-6349-9756
Marina G. Askerova, PhD, Associate Professor, Department of Obstetrics and Gynecology with a Course in Medical Genetics, Ural State Medical University,
Ministry of Health of Russia, 620028, Russia, Yekaterinburg, Repin str., 3, mg.askerova@gmail.com
Olga Yu. Sevostyanova, Dr. Med. Sci., Professor, Department of Obstetrics and Gynecology with a Course of Medical Genetics, Ural State Medical University,
Ministry of Health of Russia, 620028, Russia, Yekaterinburg, Repin str., 3, olsyava@gmail.com, https://orcid.org/0000-0002-0828-0479
Denis V. Soloviev, student, Ural State Medical University, Ministry of Health of Russia, 620028, Russia, Yekaterinburg, Repin str., 3, +7(996)22-94-265, den.sol2011@gmail.com
Andrey A. Kudimov, student, Ural State Medical University, Ministry of Health of Russia, 620028, Russia, Yekaterinburg, Repin str., 3, +7(982)61-25-200,
es.tine.dorian@gmail.com
Elina R. Bikbulatova, student, Ural State Medical University, Ministry of Health of Russia, 620028, Russia, Yekaterinburg, Repin str., 3, +7(922)16-65-155,
bzema9471@gmail.com
Elizaveta A. Averchenkova, student, Ural State Medical University, Ministry of Health of Russia, 620028, Russia, Yekaterinburg, Repin str., 3, +7(992)00-88-962,
aviga-02@yandex.com



