Clinical and economic effectiveness of a placental alpha-microglobulin-1 test and that of the clinical diagnosis of premature rupture of membranes
The incidence of premature rupture of membranes (PROM) during full-term and preterm pregnancy is 10 and 40%, respectively. To clarify the diagnosis of PROM in clinical practice, tests are used, which have a high frequency of false-positive results, being accompanied by unreasonable economic costs. At the same time, new biochemical markers of high accuracy have been developed.Baev O.R., Tysyachnyi O.V., Klimov V.A., Balashov I.S.
Objective: to compare the clinical and economic efficacy of traditional clinical examination and a placental alpha-microglobulin-1 (PAMG-1) test in patients with a presumptive diagnosis of PROM.
Subjects and methods. The investigation enrolled 114 women with a presumptive diagnosis of PROM. A decision-making model was developed and the cost-effectiveness of traditional tactics and the PAMG-1 test were compared.
Results. The cost of a case with the traditional survey strategy was 16,700 rubles. That of the PAMG-1 test was 3,000 rubles. The average cost of a case when using the latter was 3,060 rubles. The average cost saving per patient was 13,640 rubles.
Conclusion. Compared with the traditional approach to diagnosing PROM, the use of the PAMG-1 test is more effective and cost-effective.
Keywords
Premature rupture of membranes (PROM) remains one of the most urgent problems of modern obstetrics. This condition occurs in full-term pregnancy in 10% of cases, in preterm pregnancy in 40% of cases [1]. Despite numerous studies on PROM, this problem still remains significant, especially in preterm pregnancy, due to high frequency of obstetric and neonatal complications and high costs for nursing preterm infants [2, 3].
Timely diagnosis of PROM is a key point for choosing further obstetric tactics, since a false positive diagnosis leads to unreasonable actions, such as unjustified hospitalization with subsequent delivery or surgical delivery, false negative diagnosis causes prolonged expected tactics with the risk of ascending infection and subsequent complications.
In routine practice, the patient’s history and clinical examination are used to diagnose the membranes rupture. Clinical diagnosis of PROM is established in the presence of amniotic fluid in the posterior vaginal fornix when examined in sterile mirrors as well as in the absence of membranes during vaginal examination (in case of patency of the cervical canal). However, it is often difficult to make a diagnosis if there is a small amount of amniotic fluid, a lateral rupture of the fetal membranes, especially in the presence of “immature” cervix. In this regard, in order to clarify the diagnosis of PROM, different tests are used, though many of them have a high frequency of false positive results [4].
One of the most commonly used methods in clinical practice is the arborization test. The idea of the test is to perform microscopy of a smear of contents from the posterior vaginal fornix. Since the drying of amniotic fluid is accompanied by crystallization of salts, a characteristic pattern is formed on the glass, the so called fern phenomenon. According to the literature, the sensitivity of this method is 51.4%, and the specificity is 70.8%, and up to 30% of false positive results are possible in the presence of fingerprints on the glass, cervical mucus, and blood as well as with insufficient amount of material taken for evaluation [5, 6, 7].
The second most commonly used test is to determine pH of the vaginal contents, nitrazine test. The presence of amniotic fluid in the vagina shifts pH from acidic to neutral which indicates a change in the color of the test. The sensitivity of this method is 90%, the specificity is 16%, and the frequency of false positive results is 17.4% and may be associated with a disturbance of the vaginal microflora, presence of blood, semen or antiseptics [5, 7].
Lack of uniform standard and low accuracy of the clinical diagnosis of routine laboratory tests determined the development of tests based on biochemical markers that can accurately detect the presence of amniotic fluid in the vagina. One of the most accurate tests is placental alpha-microglobulin-1 (PAMG-1). This protein is synthesized by the decidual membrane and its concentration in the amniotic fluid reaches 25,000 ng/ml, but when the content of PAMG-1 is only 5 ng/ml in the vaginal contents, the sensitivity of the test for determining amniotic fluid in the vagina is 99%, and the specificity is 87.5-100% [8]. The test for the diagnosis of PROM for PAMG-1 is a one-stage immunoassay with minimal invasiveness, which is not affected by the presence of sperm, urine, blood or an infectious-inflammatory reaction in the vagina [9]. Our previous study showed that the sensitivity and specificity of PAMG-1 test is 97.3% and 97.1%, while using a complex of routine methods (clinical examination, arborization and nitrazine tests) it is 68.5% and 74.3%, respectively [10]. However, the cost of test for PAMG-1 is much higher than routine one. The use of the PAMG-1 test does not require hospitalization and additional studies [11]. In reference to the above-mentioned facts, it is relevant to compare the clinical and economic effictiveness of using the traditional clinical approach to diagnosis of PROM and application of the test for determining PAMG-1.
The objective of the study was to compare clinical and economic effectiveness of a traditional clinical examination and a test for determining PAMG-1 in patients with suspected PROM.
Materials and Methods
The study included 114 healthy pregnant women who were admitted to the National Medical Research Centre for Obstetrics, Gynecology and Perinatology, Moscow from January 1, 2018 to January 1, 2019. They complained of light liquid discharge from the genital tract which could be regarded as amniotic fluid.
The criteria for inclusion in the study were the presence of light liquid discharge from the genital tract supposing premature leakage of amniotic fluid, despite the lack of convincing clinical data indicating PROM, age from 18 to 40 years, spontaneous pregnancy between 22- 40 weeks, patient’s informed consent. The study was approved by the local ethics committee of the National Medical Research Center.
The exclusion criteria were clinically or laboratory-confirmed PROM, severe somatic pathology, complicated pregnancy, abnormalities of the uterus, fetal malformations, chorioamnionitis.
The women were taken a history, they underwent speculum examination, microbiological examination from the cervical canal (in preterm pregnancy), bimanual vaginal examination for the assessment of the integrity of the fetal membranes (in full term), aborization test (fern phenomenon) on two glasses, nitrazine test for determining pH of the vaginal fluid, test for determining vaginal secretions of placental alpha-microglobulin (AmniSure), ultrasound examination with identifying amniotic fluid index, full blood count, C-reactive protein, determining blood group and Rh factor (due to the possibility of delivery), urine analysis.
Due to the development of decision-making model, the costs and effectiveness of two approaches to the diagnosis and further management of patients were compared with an estimated diagnosis of PROM.
When creating the model, the following assumptions were made:
- For traditional examination strategy, the prognostic value of both positive and negative results for arborization test and nitrazine test do not make it possible to determine PROM with sufficient accuracy for use in real clinical practice. In this regard, all patients with suspected PROM undergo a complex of diagnostic tests, including laboratory and instrumental methods which may confirm the presence or absence of PROM; on the basis of this, the false positive and false negative results of the traditional strategy are not considered.
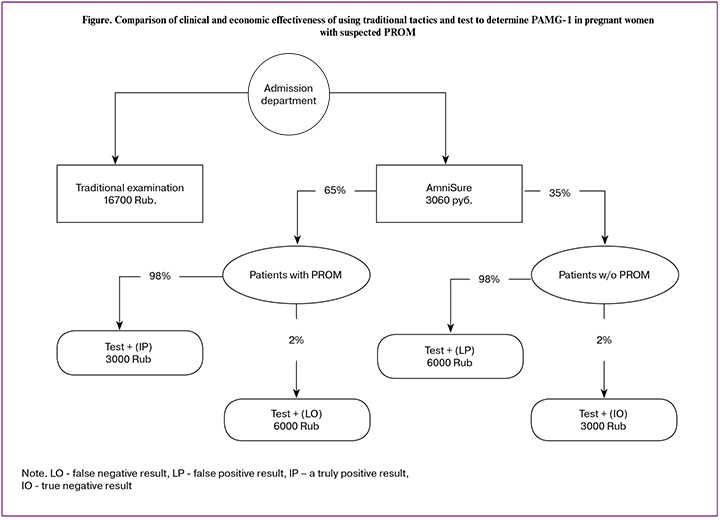
- Test for determining the presence of PAMG-1 is characterized by high prognostic value of both positive and negative results; according to the results of the test, decisions on patient management tactics can be made. Taking into account the literature data and preliminary results of our research, the share of false positive and false negative test results is considered to be 2%.
- In case of false positive test result for PAMG-1, the cost of the case was considered equal to the cost of the test and additional bed-day.
- In case of false-negative test for PAMG-1, the cost of the case was equal to the cost of two tests, since if PROM and negative test results are suspected, the test is repeated. Since the probability of two false-negative tests tends to zero, it is possible to use the cost of double application of the test as the necessary cost per patient.
- When assessing the cost of one case with the generally accepted methods, the number of necessary manipulations did not depend on the gestational age and associated pathology.
- Costs of patient management after the diagnosis of PROM are considered equal for both diagnostic strategies and were not taken into account in this work.
Statistical processing of the results was carried out using the statistical program “IBM SPSS Statistics 22 for Windows”. Since the results of PAMG-1 test are a binary value, the calculation of diagnostic criteria was carried out on the basis of the confusion matrix.
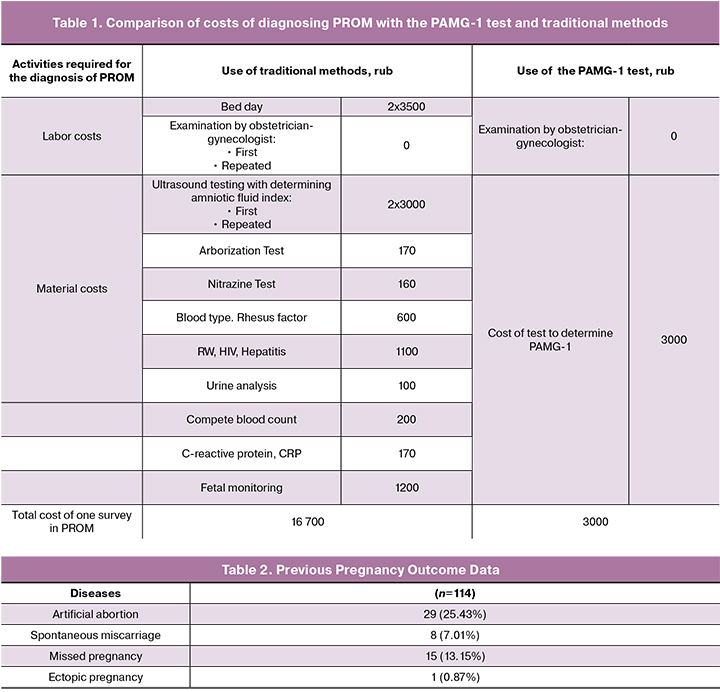
In order to assess the economic feasibility of using PAMG-1 test as a method of diagnosing PROM in the analysis, we took into account only the direct costs of diagnosing PROM. Costs were considered as the direct cost of medical services as well as the costs of hospital days and possible costs of PAMG-1 diagnostic test on the basis of outpatient department. It should be noted that during hospitalization in the maternity hospital, all patients underwent studies necessary for the diagnosis of PROM. The cost of all services was calculated as the commercial value for this type of medical service at the National Medical Research Center for Obstetrics, Gynecology and Perinatology, Moscow in 2019 (Table 1).
Results and Discussion
The average age of women included in the study was 29 (5.1) years. The average body mass index was 26.4 (3.1) kg/m2.
The analysis of frequency and structure of extra genital diseases showed that the diseases of extra genital organs (rhinitis, tonsillitis, sinusitis), cardiovascular system (vegetative vascular dystonia, mitral valve prolapse, varicose veins of the lower extremities), digestive system (gastritis, cholecystitis, peptic ulcer, pancreatitis), urinary system (cystitis, pyelonephritis, urolithiasis) were found in 11.4%, 19.2%, 16.6% and 14% of cases, respectively. The most common pathology was myopia (34.2%). It is important to note that somatic diseases in all cases had only initial manifestations or were mild, and there was not any exacerbation of the diseases during the study.
Analysis of gynecological history showed that menarche ranged from 9 to 20 years, and it averaged 13.2 (1.28) years. Benign cervix uteri diseases (ectopia) were most commonly found in about 43.85% of cases, while ovarian dysfunction, uterine myoma, ovarian cysts and infertility had a frequency of 6.14%, 5.26%, 8.77% and 7.89%, respectively.
Among the participants of the study there were 64 primiparous women (56.1%) and 50 multiparous women (43.8%). The data on previous pregnancies are presented in Table 2.
A total of 101 women (88.6%) were admitted to hospital at full-term pregnancy and 13 women (11.4%) were hospitalized before 37 weeks gestation.
Among 114 admitted patients with complaints of fluid discharge from the vagina, PROM was confirmed in 75 (65.8%) women. In the remaining 39 (34.2%) women, the diagnosis of PROM was excluded by the determination of PAMG-1, and existing complaints were regarded as a mucous plug or clinical manifestations of vaginitis.
Thus, a third of the pregnant women who did not have convincing data for PROM and who were to be hospitalized, observed and examined additionally for clarifying the diagnosis, according to Order №572n dated from 2012, were examined in outpatient departments. The sensitivity of the method for determining PAMG-1 was 96%, specificity 97.4%. Moreover, the scope of the examination was limited by the use of the test to determine PAMG-1.
According to the results, the cost of the case with the traditional expected strategy for suspected PROM is 16,700 rubles. The cost of one PAMG-1 test is 3,000 rubles. As shown in the decision tree (Figure), the average cost of a case when using PAMG-1 test is 3,060 Rubles. Consequently, the average savings per patient admitted with suspected PROM is 13,640 Rubles. From 2018 to 2019, 198 patients (on average 18 people per month) were admitted to our Center with suspected PROM; in traditional tactics of managing patients they required hospitalization and clarification of the diagnosis using additional methods. The use of the PAMG-1 test at the prehospital stage allows doctors to save 13,640 * 198 = 2,700,720 rubles per year.
Conclusion
Thus, the use of test for determining PAMG-1 in comparison with the traditional approach to the diagnosis of PROM in pregnant women with suspected leakage of amniotic fluid proved to be more effective and economically feasible.
References
- Negara K.S., Prajawati N.L.L.C., Surya G.P., Suhendro S., Arijana K., Tunas K. Protein 53 (P53) expressions and apoptotic index of amniotic membrane cells in the premature rupture of membranes. Open Access Maced. J. Med. Sci. 2018; 6(11): 1986-92. https://doi.org/10.3889/oamjms.2018.465.
- Ocviyanti D., Wahono W.T. Risk factors for neonatal sepsis in pregnant women with premature rupture of the membrane. J Pregnancy. 2018; 2018: 4823404. https://doi.org/10.1155/2018/4823404. eCollection 2018.
- Ibishi V.A., Isjanovska R.D. Prelabour rupture of membranes: mode of delivery and outcome. Open Access Maced. J. Med. Sci. 2015; 3(2): 237-40. https://doi.org/10.3889/oamjms.2015.037.
- Gallot D. Diagnosis of rupture of fetal membranes: CNGOF Preterm Premature Rupture of Membranes Guidelines. Gynecol. Obstet. Fertil. Senol. 2018; 46(12): 1022-8. https://doi.org/10.1016/j.gofs.2018.10.014.
- Mariona F.G., Cabero L. Are we ready for a new look at the diagnosis of premature rupture of membranes? J. Matern. Fetal Neonatal Med. 2012; 25(4): 403-7. https://doi.org/10.3109/14767058.2011.581715.
- Lee S.M., Lee J., Seong H.S., Lee S.E., Park J.S., Romero R., Yoon B.H. The clinical significance of a positive Amnisure test in women with term labor with intact membranes. J. Matern Fetal Neonatal Med. 2009; 22(4): 305-10.
- Abdelazim I.A., Abdelrazak K.M., Al-Kadi M., Yehia A..H., Abdulkareem A.F. Fetal fibronectin (Quick Check fFN test) versus placental alpha microglobulin-1 (AmniSure test) for detection of premature rupture of fetal membranes. Arch. Gynecol. Obstet. 2014; 290(3): 457-64. https://doi.org/10.1007/s00404-014-3225-5.
- Di Renzo G.C., Roura L.C., Facchinetti F., Antsaklis A., Breborowicz G., Gratacos E. et al. Guidelines for the management of spontaneous preterm labor: identification of spontaneous preterm labor, diagnosis of preterm premature rupture of membranes, and preventive tools for preterm birth. J. Matern. Fetal Neonatal Med. 2011; 24(5): 659-67.
- Echebiri N.C., McDoom M.M., Pullen J.A., Aalto M.M., Patel N.N., Doyle N.M. Placental alpha-microglobulin-1 and combined traditional diagnostic test: a cost-benefit analysis. Am. J. Obstet. Gynecol. 2015; 212(1): 77. e1-10. https://doi.org/10.1016/j.ajog.2014.07.028.
- Баев О.Р., Васильченко О.Н., Румянцева В.П., Шахмаева А.Б., Козлова О.А. Точность диагностики преждевременного разрыва плодных оболочек и самостоятельное использование теста определения PAMG-1 беременной. Акушерство и гинекология. 2014; 3: 39-43. [Baev O.R., Vasil’chenko O.N., Rumyantseva V.P., Shakhmaeva A.B., Kozlova O.A. Accuracy of diagnosis of premature rupture of the fetal membranes and the independent use of the PAMG-1 test for pregnant. Akusherstvo i ginekologiya/Obstetrics and Gynecology. 2014; 3: 39-43. (In Russ.)]
- Болотских В.М., Захарова В.Ю., Кузьминых Т.У. Клинико-экономическое обоснование применения теста AmniSure® ROM в акушерской практике. Журнал акушерства и женских болезней. 2012; 61(4): 33-9. [Bolotskikh V.M., Zakharova V.Yu., Kuzminykh T.U. Clinical and economic rationale for using the AmniSure® ROM test in obstetric practice. Journal of Obstetrics and Women’s Diseases. 2012; 61 (4): 33-39. (InRuss.)]
Received 08.06.2019
Accepted 21.06.2019
About the Authors
Baev Oleg R., MD; Head, Maternity Department One, Academician V.I. Kulakov National Medical Research Center of Obstetrics, Gynecology, and Perinatology,Ministry of Health of Russia.
Address: 4, Academician Oparin Street, Build. 1, Moscow 117513, Russia. Postal Code. Tel.: +7 (495) 438-1188. E-mail: metod_obsgyn@hotmail.com.
Department of Obstetrics, Gynecology, and Reproductology, I.M. Sechenov First Moscow State Medical University (Sechenov University), Ministry of Health of Russia.
Tysyachnyi Oleg V., Cand. Med. Sci.; Researcher, Department of Innovative Technologies, Academician V.I. Kulakov National Medical Research Center
of Obstetrics, Gynecology, and Perinatology, Ministry of Health of Russia.
Address: 4, Academician Oparin St., Build. 1, Moscow 117513, Russia. Tel.: +7 (495) 438-1188. E-mail: olti23@mail.ru
Klimov Vladimir A., Cand. Med. Sci.; Head, Service for Organization of Medical Care and Information Service, Academician V.I. Kulakov National Medical Research Center
of Obstetrics, Gynecology, and Perinatology, Ministry of Health of Russia.
Address: 4, Academician Oparin St., Build. 1, Moscow 117513, Russia. Tel.: +7 (495) 438-1188. E-mail: olti23@mail.ru Cand. Med. Sci.; Head, Service for Organization
of Medical Care and Information service, Academician V.I. Kulakov National Medical Research Center of Obstetrics, Gynecology, and Perinatology,
Ministry of Health of Russia. Address: 4, Academician Oparin St., Build. 1, Moscow 117513, Russia. Tel.: +7 (495) 438-1188. E-mail: va_klimov@oparina4.ru
Balashov Ivan S., Junior Researcher Laboratory of Bioinformatics of the Academician V.I. Kulakov National Medical Research Center of Obstetrics, Gynecology, and Perinatology, Ministry of Health of Russia.
Address: Russia, Moscow, Akademika Oparin street, house 4, building 1. 117198. Phone +7(495)438-2090. Email: i_balashov@oparina4.ru
For citation: Baev O.R., Tysyachnyi O.V., Klimov V.A., Balashov I.S. Clinical and economic effectiveness of a placental alpha-microglobulin-1 test and that of the clinical diagnosis of premature rupture of membranes.
Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2019; (8): 71-6 (in Russian)
http://dx.doi.org/10.18565/aig.2019.8.71-76