Сlinical characteristics of Syrian women with uterine leiomyoma
Alali O.M., Khaddam W.M., Churnosov M.I.
Objective: To analyze the clinical characteristics, risk factors, and impact on lifestyle of women with uterine leiomyomas (ULs) and compare these findings with a control group of healthy women.
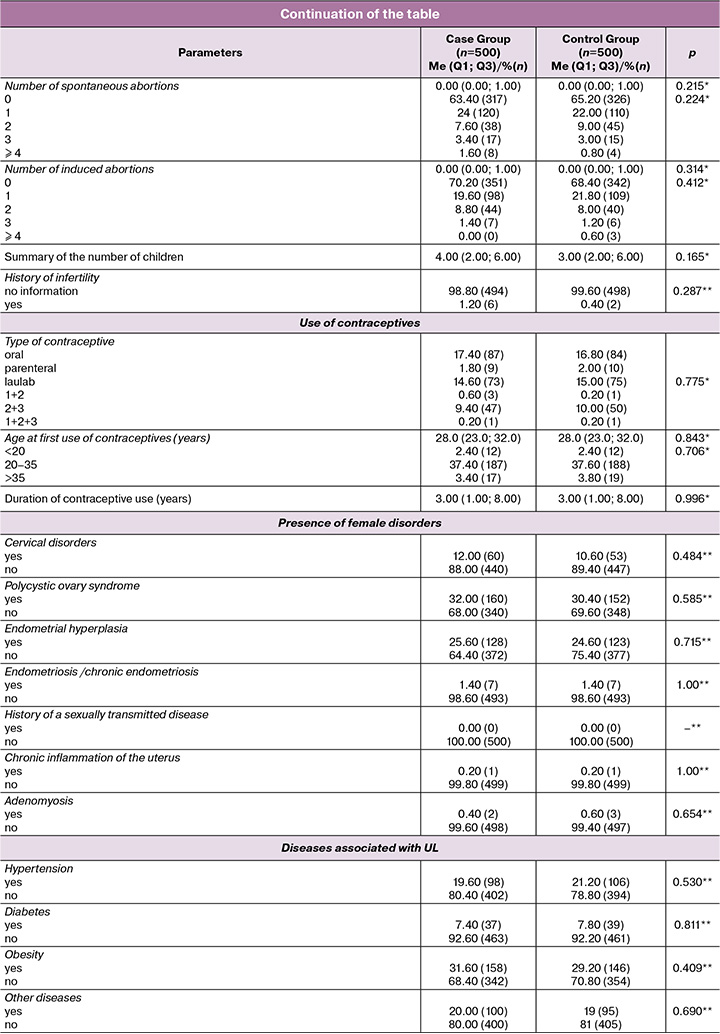
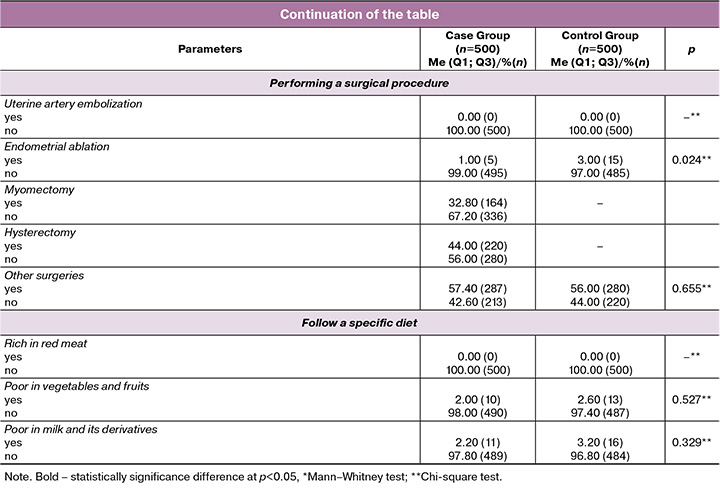
Materials and methods: Conducted from June 2023 to August 2024, the study included 1,000 Syrian women (500 patients with ULs and 500 controls) aged 22–83 from various cities. A questionnaire formed of 65 questions containing information about the clinical characteristics and risk factors for the development of uterine leiomyomas was used. Data was analyzed using Statistical Packages for Software Sciences (SPSS) version 30.
Results: Revealed significant differences between patients and controls in age at first menstruation (p=0.046), length of the menstrual cycle (p=0.016), duration of the menstrual bleeding (p=0.043), age at menopause (p<0.001), time elapsed since the last birth (p<0.001), and endometrial ablation (p=0.039). Regarding the characteristics of the Fibrous nodes, it indicated that submucosal fibroids were in only 6/500 (1.2%) women, while pedunculated was in 22/500 (4.4%) women, subserosal was in 227/500 (45.4%), and intramural was in 228/500 (45.6%).
Conclusion: This study demonstrated which clinical characteristics and risk factors for uterine leiomyomas were statistically significant in Syrian women. This may help determine the best techniques to diagnose and treat them well in order to prevent complications and reduce their impact on health-related quality of life.
Authors' contributions: Alali O.M., Khaddam W.M., Churnosov M.I. – conception and design of the study; Alali O.M. – data collection and analysis, manuscript drafting; Churnosov M.I. – manuscript editing.
Conflicts of interest: The authors have no conflicts of interest to declare.
Funding: There was no funding for this study.
Ethical Approval: The study was reviewed and approved by the Research Ethics Committee of the Belgorod State National Research University.
Patient Consent for Publication: All patients provided informed consent for the publication of their data.
Authors' Data Sharing Statement: The data supporting the findings of this study are available upon request from the corresponding author after approval from the principal investigator.
For citation: Alali O.M., Khaddam W.M., Churnosov M.I.
Сlinical characteristics of Syrian women with uterine leiomyoma.
Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2025; (7): 76-83 (in Russian)
https://dx.doi.org/10.18565/aig.2025.59
Keywords
Uterine leiomyomas (ULs) are the most frequent tumors of the female reproductive system [1]. They originate from the myometrium and are benign monoclonal uterine smooth muscle tumors [2]. By the time of menopause, more than 70% of women have ULs. With a lifetime prevalence of 30%_70% [2], they afflict 20%_40% of women of reproductive age [3], (they frequently regress after menopause). Uterine leiomyomas are a major cause of gynecologic morbidity, one of the most prevalent reasons for gynecologic hospitalizations, and the most common reason for hysterectomy in the United States [4], where are found in 75% of hysterectomy specimens [5]. The yearly cost of treating this condition in the United States is projected to be over $34 billion, which is higher than the cost of treating breast and colon cancers combined [6].
The clinical characteristics of ULs can include: menorrhagia, painful periods, lower backache or leg pain, constipation, discomfort or a feeling of fullness in the lower abdomen, especially in the case of large fibroid, frequent urination, etc. The symptoms are exacerbated by the position of fibroids within the uterus. According to their location, ULs are characterized as subserosal, intramural, submucosal, or pedunculated [7]. In a meta-analysis of many research on fibroids and infertility, submucosal fibroids were found to have a significant impact on all fertility outcomes and subserosal fibroids are thought to have a minor effect on fertility [7]. Fibroid may cause problems during pregnancy and labor, and they increase the chance of needing a cesarean delivery [8]. Uterine leiomyoma is a complicated condition caused by a number of demographic, dietary, and hormonal risk factors [9] as well as biological, epigenetic, and genetic causes [10], with the genetic component accounting for 40–50% [11] of the illness. The genetic foundation for the formation, development, and progression of ULs is now being studied by a considerable number of academics and researchers.
The prevalence of ULs has pronounced territorial features differences between ethnic groups and countries. Where in the Russian Federation was estimated to be around 70-71% over the age of 40 being affected [12]. In other countries, it varies, around 80% among African American women and around 70% among Caucasian women in the United States [13]. In Japan, was estimated to be around 37% [14]. Also, in India, was relatively higher 37.6% [15].
As for the Arab countries, the data on the incidence and prevalence of ULs, clinical characteristics and risk factors related to them are extremely limited and are only presented in small elections. Considering the results of the first systematic review of the prevalence of common gynecological conditions in Middle Eastern women, including ULs in 2021 by Mousa M. et al., the study and reporting quality were generally low for several reasons that were mentioned, as the hospital-based pooled prevalence of ULs for women was estimated at 28.2%, and 57.1% among women with heavy menstrual bleeding [16], which are on the high end of the estimated global prevalence 5–30% [17] and 37–59% [18], respectively. In Egypt, the prevalence of ULs was 47.5% within the age group 30-35 years [8], while ranged from 9.8% to 17.8% in the age group of 40–49 years, and about 25 % of them underwent hysterectomy due to ULs [19]. In Kingdom of Saudi Arabia, the prevalence of ULs in reproductive age at king Abdul-Aziz University Hospital with an incidence of 21.24%, which represents higher percentage than that of the previous study for five years 19.75% [20]. As for the clinical characteristics and risk factors of uterine leiomyomas in Syria, they have not been studied yet, so this will be the first study of its kind on Syrian women.
The aim of this study, which is the first of its kind in Syria, was to analyze clinical characteristics and risk factors of ULs, impact on lifestyle of the condition under investigation, and to compare these findings with those of a control group (healthy women).
Materials and methods
A questionnaire-based study was conducted in Syria from June 2023 to August 2024 across public and private hospitals in cities including Homs, Hama, Tartus, Latakia, and Damascus. Which include: Homs University Hospital, Alahli Private Hospital, Latakia University Hospital, Latakia Maternity and Children's Hospital, and Tartus Maternity and Children's Hospital.
The study involved 1,000 Syrian women (500 patients and 500 controls) aged 20 years or older. Patients were women with ULs, while controls were asymptomatic women without signs of benign reproductive organ diseases. Exclusion criteria included women under 20, non-Syrian descent, or those born outside Syria. Participants provided informed consent after explanation of the study purpose, and a 65-question questionnaire was formed of categorical questions as yes/no and MCQ translated into Arabic to be easy for the participants to understand, which used to assess clinical characteristics and risk factors. The questionnaire design was adapted from previously published studies with some modifications.
Statistical analysis
We estimated that a sample size was 500 patients and 500 controls. Statistical Packages for Software Sciences (SPSS) version 30.0.0.0(172), IBM Corporation has been used to perform all statistical analysis for this study. Shapiro–Wilk test was used to test normality of evaluated quantitative variables. For all indicators p Shapiro–Wilk was less than 0.001, meaning that their distribution differed from the normal distribution. Therefore, to characterize these quantitative indicators, we used the median and interquartile range Me (Q1; Q3), for comparative analysis, the Mann–Whitny test were used. For qualitative variables, the Chi-square test was employed to compare binary categorical variables between the case and control groups. For variables with three or more than categories, the Mann–Whitney test was used to compare the groups. Results were represented as numbers/all participants (percentages) for all qualitative parameters. P-value<0.05 was considered statistically significant.
Results
1000 participants were recruited in this study, 500 have or suffered from ULs and 500 controls, aged 22–83, with the majority in the 36–50 age group.
As for the characteristics of the fibroid nodes, the results showed that the range volume of these nodes was 14.7 cm3 (4; 144), and the range number of them was 1 (1; 3). Furthermore, the results indicated that submucosal fibroids were in only 6/500 (1.2%) women, while pedunculated was in 22/500 (4.4%) women, subserosal was in 227/500 (45.4%), and intramural was in 228/500 (45.6%). There were also women who had two types of fibroids together, which were subserosal and intramural 13/500 (2.6%).
The most common symptoms in women diagnosed with ULs were heavy menstrual bleeding 384/500 (76.8%), prolonged menstrual cycle 328/500 (65.6%), dysmenorrhea 338/500 (67.6%), abdominal pain 346/500 (69.2%), pelvic pain 331/500 (66.2%), back and leg pain 352/500 (70.4%), while some had difficulty urinating 139/500 (27.8%), frequent urination 200/500 (40%), constipation 167/500 (33.4%), and a few had premature birth 41/500 (8.2%), recurrent pregnancy loss 62/500 (12.4%), or complications during pregnancy 25/500 (5%), as shown in the table.
Significant differences were observed in menstrual cycle characteristics between women with ULs and controls. Early menstruation (<12 years) was less common in the case group 5/500 (1%) compared to controls 20/500 (4%) (p=0.046). As for the length of the menstrual cycle, it was also statistically significant (p=0.016). In the case group, the range was 28 (27.5; 28), and in the control group, the range was 28 (28; 28). Menstrual duration also differed significantly (p=0.043), with fewer UL patients having cycles <5 days 102/500 (20.4%) compared to controls 293/500 (58.6%), while more UL patients had cycles lasting 5–7 days 382/500 (76.4%) versus controls 195/500 (39%), as shown in the table.
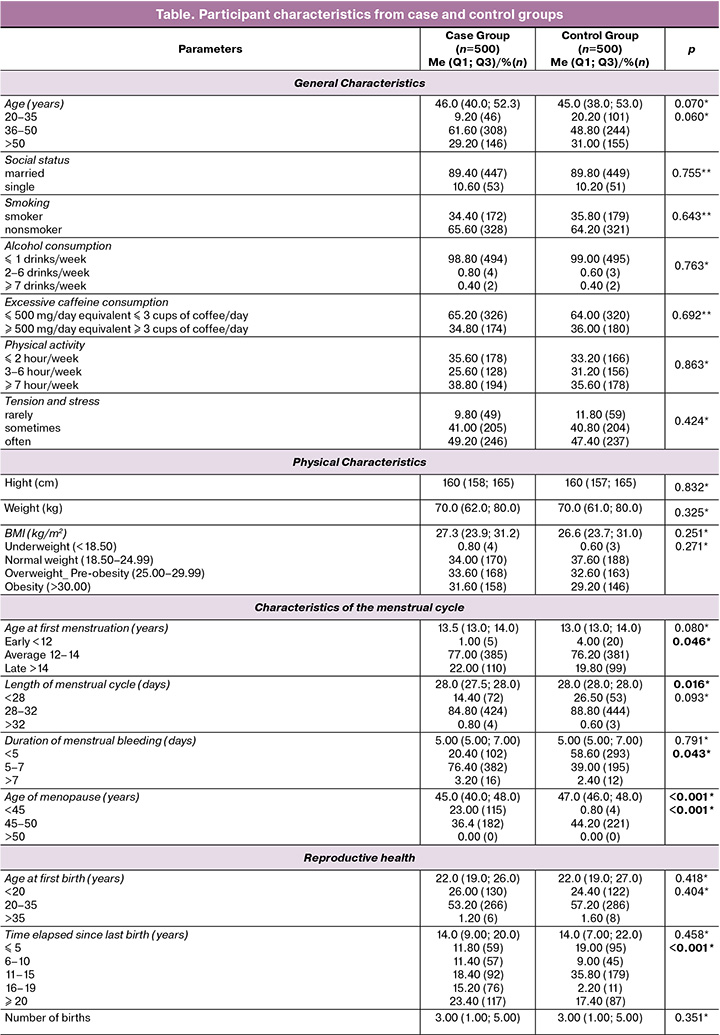
The age of menopause was statistically significant (p<0.001) lower in the case group 45 (40; 48) than in controls 47 (46; 48). The number of women in the case group 115/500 (23%) was greater than in controls 4/500 (0.8%) with a menopausal age of <45 years, while more controls experienced menopause between 45–50 years 221/500 (44.2%) than the case group 182/500 (36.4%), as shown in the table.
Regarding the reproductive health, it was also close between both groups through the answers of questions included in the questionnaire and shown in the table, except for the time elapsed since the last birth, which showed significant differences (p<0.001). In the categories <5 years, and 11–15 years, it was the percentage in the control group 95/500 (19%) and 179/500 (35.8%) was higher than in the case group 59/500 (11.8%) and 92/500 (18.4%), respectively. Conversely, within the following categories: 6–10 years, 16–19 years, and ≥20 years, the percentage in the case group 57/500 (11.4%), 76/500 (15.2%), and 117/500 (23.4%) was higher than in the control group 45/500 (9%), 11/500 (2.2%) and 87/500 (17.4%), respectively, as shown in the table. Regarding surgical procedures, only endometrial ablation was statistically significant (p=0.039), with a higher percentage in the control group 15/500 (3%) than in the case group 5/500 (1%), as shown in the table.
Discussion
The study found that the range volume of fibroid nodes was 14.7 cm3 (4; 144), which differs significantly from a study on Egyptian women by Fawzi M. et al.[21], where the average volume was 202.15±206.63. The range number of nodes was 1 (1; 3), with 394/500 (78.8%) of cases having single fibroid nodes and 106/500 (21.2%) having multiple nodes. This contrasts with study by Abbas H.Y. et al. on Saudi women [20] and Fawzi M. et al. on Egyptian women [21], where the distribution of single and multiple fibroids was nearly equal at around 50% each.
The study showed that only 6/500 (1.2%) of women had submucosal fibroids, while 22/500 (4.4%) had pedunculated fibroids, 227/500 (45.4%) had subserosal fibroids, and 228/500 (45.6%) had intramural fibroids. Additionally, 13/500 (2.6%) of women had both subserosal and intramural fibroids. These results differ from a study by Fawzi M. et al. [21], where 5% of fibroids were submucosal and 95% were intramural. The findings highlight differences in the distribution of fibroid nodes characteristics compared to other populations.
Significant differences were observed in menstrual cycle characteristics between women with ULs and controls, who had early menstruation (<12 years), consistent with early studies reported increased risk of fibroids with earlier age of menarche, before age 11 compared to women with menarche after age 13 varying from 25% to 48% [22]. On the contrary, many studies established an inverse relationship between age at menarche and the risk of developing UL [23]. In addition, Ponomarenko I. et al. found menarcheal age was not a primary risk factor of ULs in their Russian sample and that other factors may be of greater importance [2]. Menstrual cycle length and duration also showed significant differences. While the Terry K.L. et al. linked irregular and longer menstrual cycles to reduced UL risk [24], other studies found no such associations [25, 26].
The study found a statistically significant association between the age of menopause and ULs, with menopause delayed in the 45–50 years category compared to those under 45. While no studies have specifically examined late menopause as a risk factor for fibroids, it is suggested that later menopause may increase the likelihood of developing new fibroids [9, 26].
Regarding reproductive health, the time elapsed since the last birth was statistically significant, with the majority of UL patients having intervals >5 years, particularly ≥20 years. Previous studies suggest that longer intervals since the last birth increase UL risk [24, 27, 28], and a 20–50% lower UL risk in women with previous live births than nulliparous women [29].
Conclusion
This study demonstrated which clinical characteristics and risk factors for uterine leiomyomas were statistically significant in Syrian women. This may help determine the best techniques to diagnose and treat them well in order to prevent complications and reduce their impact on health-related quality of life.
References
- Peng J., Wang J., Shu Q., Luo Y., Wang S., Liu Z. Systematic review and meta-analysis of current evidence in uterine artery embolization vs myomectomy for symptomatic uterine fibroids. Sci. Rep. 2024; 14(1): 19252. https://dx.doi.org/10.1038/s41598-024-69754-0
- Ponomarenko I., Reshetnikov E., Polonikov A., Verzilina I., Sorokina I., Yermachenko A. et al. Candidate genes for age at menarche are associated with uterine leiomyoma. Front. Genet. 2021; 11: 512940. https://dx.doi.org/10.3389/fgene.2020.512940
- Stewart E.A., Cookson C.L., Gandolfo R.A., Schulze‐Rath R. Epidemiology of uterine fibroids: a systematic review. BJOG. 2017; 124(10): 1501-12. https://dx.doi.org/10.1111/1471-0528.14640
- Алали О.М., Чурносов М.И. Полногеномные исследования лейомиом матки. Акушерство и гинекология. 2023; 7: 28-38. [Alali O.M., Churnosov M.I. Genome-wide studies of uterine leiomyomas. Obstetrics and Gynecology. 2023; (7): 28-38 (in Russian)]. https://dx.doi.org/10.18565/aig.2023.156
- Li B., Wang F., Chen L., Tong H. Global epidemiological characteristics of uterine fibroids. Arch. Med. Sci. 2023; 19(6): 1802-10. https://dx.doi.org/10.5114/aoms/171786
- Alsudairi H.N., Alrasheed A.T., Dvornyk V. Estrogens and uterine fibroids: an integrated view. Research Results in Biomedicine. 2021; 7(2): 156-63. https://dx.doi.org/10.18413/2658-6533-2021-7-2-0-6
- Алали О.М., Чурносов М.И. Этиопатогенез миомы матки (обзор). Гинекология. 2023; 25(1): 22-30. [Alali O.M., Churnosov M.I. The etiopathogenesis of uterine leiomyomas: A review. Gynecology. 2023; 25(1): 22-30. (in English)]. https://dx.doi.org/10.26442/20795696.2023.1.201827
- Abd Alazeam M.M., Abd El-hak Farag R.E., Mohamady S.H. Raising middle-aged women awareness of uterine fibroid. IJCBS. 2023; 24(6):722-35.
- Pavone D., Clemenza S., Sorbi F., Fambrini M., Petraglia F. Epidemiology and risk factors of uterine fibroids. Best Pract. Res. Clin. Obstet. Gynaecol. 2018; 46: 3-11. https://dx.doi.org/10.1016/j.bpobgyn.2017.09.004
- Qin H., Lin Z., Vásquez E., Xu L. The association between chronic psychological stress and uterine fibroids risk: a meta‐analysis of observational studies. Stress Health. 2019; 35(5): 585-94. https://dx.doi.org/10.1002/smi.2895
- Meadows K.L., Andrews D.M., Xu Z., Carswell G.K., Laughlin S.K., Baird D.D. et al. Genome-wide analysis of loss of heterozygosity and copy number amplification in uterine leiomyomas using the 100K single nucleotide polymorphism array. Exp. Mol. Pathol. 2011; 91(1): 434-39. https://dx.doi.org/10.1016/j.yexmp.2011.03.007
- Ponomarenko M.S., Reshetnikov E.A., Churnosova M.M., Reshetnikova Y.N., Churnosov V.I., Ponomarenko I.V. Comorbidity and syntropy of benign proliferative diseases of the female reproductive system: non-genetic, genetic, and epigenetic factors (review). Research Results in Biomedicine. 2023; 9(4): 544-56. https://dx.doi.org/10.18413/2658-6533-2023-9-4-0-9
- Marsh E.E., Ekpo G.E., Cardozo E.R., Brocks M., Dune T., Cohen L.S. Racial differences in fibroid prevalence and ultrasound findings in asymptomatic young women (18–30 years old): a pilot study. Fertil. Steril. 2013; 99(7): 1951-7. https://dx.doi.org/10.1016/j.fertnstert.2013.02.017
- Nishiyama S., Saito M., Sato K., Kurishita M., Itasaka T., Shioda K. High recurrence rate of uterine fibroids on transvaginal ultrasound after abdominal myomectomy in Japanese women. Gynecol. Obstet. Invest. 2006; 61(3): 155-9. https://dx.doi.org/10.1159/000090628
- Munusamy M.M., Sheelaa W.G., Lakshmi V.P. Clinical presentation and prevalence of uterine fibroids: a 3-year study in 3-decade rural South Indian women. IJRCOG. 2017; 6(12): 5596-602. https://dx.doi.org/10.18203/2320-1770.ijrcog20175288
- Mousa M., Al-Jefout M., Alsafar H., Kirtley S., Lindgren C.M., Missmer S.A. et al. Prevalence of common gynecological conditions in the Middle East: systematic review and meta-analysis. Front. Reprod. Health. 2021; 3: 661360. https://dx.doi.org/10.3389/frph.2021.661360
- Stewart E.A., Laughlin-Tommaso S.K., Catherino W.H., Lalitkumar S., Gupta D., Vollenhoven B. Uterine fibroids. Nat. Rev. Dis. Primers. 2016; 2(1): 1-8. https://dx.doi.org/10.1038/nrdp.2016.43
- Zimmermann A., Bernuit D., Gerlinger C., Schaefers M., Geppert K. Prevalence, symptoms and management of uterine fibroids: an international internet-based survey of 21,746 women. BMC Women's Health. 2012; 12: 1-11. https://dx.doi.org/10.1186/1472-6874-12-6
- Ragvendra D.R., Meena L.V. Diseases of reproductive age. 2008; 147-9.
- Abbas H.Y., Awad I.A., Alharbi E., Alaameri H., Althubaiti S., Ashkar L. Prevalence and incidence of uterine fibroid at king Abdulaziz university hospital Saudi Arabia. Statistics. Clinical Medicine and Diagnostics. 2016; 6(3): 45-8. https://dx.doi.org/10.5923/j.cmd.20160603.01
- Fawzi M., ElMandouh S., Elbanna A.E., Narouz M.E., Habib M., Mahmoud S.S. et al. Preliminary insights into high-intensity focused ultrasound ablation for symptomatic uterine fibroids: a first look in Egypt. Egyptian Journal of Radiology and Nuclear Medicine. 2024; 55(1): 44. https://dx.doi.org/10.1186/s43055-024-01219-w
- Keizer A.L., Semmler A., Kok H.S., Kesteren P.J. van, Huirne J.A., Hehenkamp W.J. Modifiable prognostic factors in uterine fibroid development: a systematic review of literature. J. Obstet. and Gynaecol. 2024; 44(1): 2288225. https://dx.doi.org/10.1080/01443615.2023.2288225
- El Mawla Z., Berthe Y., Salameh P. Epidemiology of uterine fibroid disease in Lebanon: a case-control study. IJCR. 2023; 3(1): 245-57. https://dx.doi.org/10.38179/ijcr.v3i1.113
- Terry K.L., Vivo I. de, Hankinson S.E., Missmer S.A. Reproductive characteristics and risk of uterine leiomyomata. Fertil. Steril. 2010; 94(7): 2703-07. https://dx.doi.org/10.1016/j.fertnstert.2010.04.065
- Song S., Park S., Song B.M., Lee J.E., Cha C., Park H.Y. Risk of uterine leiomyomata with menstrual and reproductive factors in premenopausal women: Korea nurses’ health study. BMC Women's Health. 2023; 23(1): 305. https://dx.doi.org/10.1186/s12905-023-02447-4
- Muawad R., Dabbagh R., Sabr Y. Association of health and lifestyle factors with uterine fibroids among Saudi women: a case – control study. J. Taibah Univ. Med. Sci. 2022; 17(6): 1039-46. https://dx.doi.org/10.1016/j.jtumed.2022.06.005
- Пономаренко М.С., Решетников Е.А., Пономаренко И.В., Чурносов М.И. Факторы риска развития миомы матки. Акушерство и гинекология. 2024; 3: 20-7. [Ponomarenko M.S., Reshetnikov E.A., Ponomarenko I.V., Churnosov M.I. Risk factors for uterine fibroids. Obstetrics and Gynecology. 2024; (3): 20-7 (in Russian)]. https://dx.doi.org/10.18565/aig.2023.275
- Nwonuma C., Irokanulo E., Bamgboye F., Akinduko A., Okeniyi F., Eigbe C. Uterine fibroid: risk factors and therapeutic interventions. 2024 International Conference on Science, Engineering and Business for Driving Sustainable Development Goals (SEB4SDG), Omu-Aran, Nigeria, 2024: 1-10. https://dx.doi.org/10.1109/SEB4SDG60871.2024.10630388
- Shabahat, Ahmed A., Kiran, Sharif M.A. Prevalence and clinical characteristics of uterine fibroids in women of reproductive age in district hyderabad. The Research of Medical Science Review. 2025; 3(1): 635-47.
Received 05.03.2025
Accepted 17.06.2025
About the Authors
Ola Mohamad Alali, PhD student, Belgorod State National Research University, 85 Pobedy str., 308015, Belgorod, Russia, alali@bsuedu.ru,https://orcid.org/0000-0003-4370-6719
Walid Khaddam, Doctor of Microbiology, Homs University, Homs, Syria, wkhaddam@homs-univ.edu.sy, https://orcid.org./0000-0001-6771-2211
Mikhail I. Churnosov, Dr. Med. Sci., Professor, Head of the Department of Medical and Biological Disciplines, Belgorod National Research University, 85 Pobedy str.,
308015, Belgorod, Russia, churnosov@bsuedu.ru, https://orcid.org/ 0000-0003-1254-6134